Pediatric Septic Arthritis of the Knee Due to a Multi-Sensitive Streptococcus pyogenes Strain Responsive to Clindamycin—A Case Report
Abstract
1. Introduction
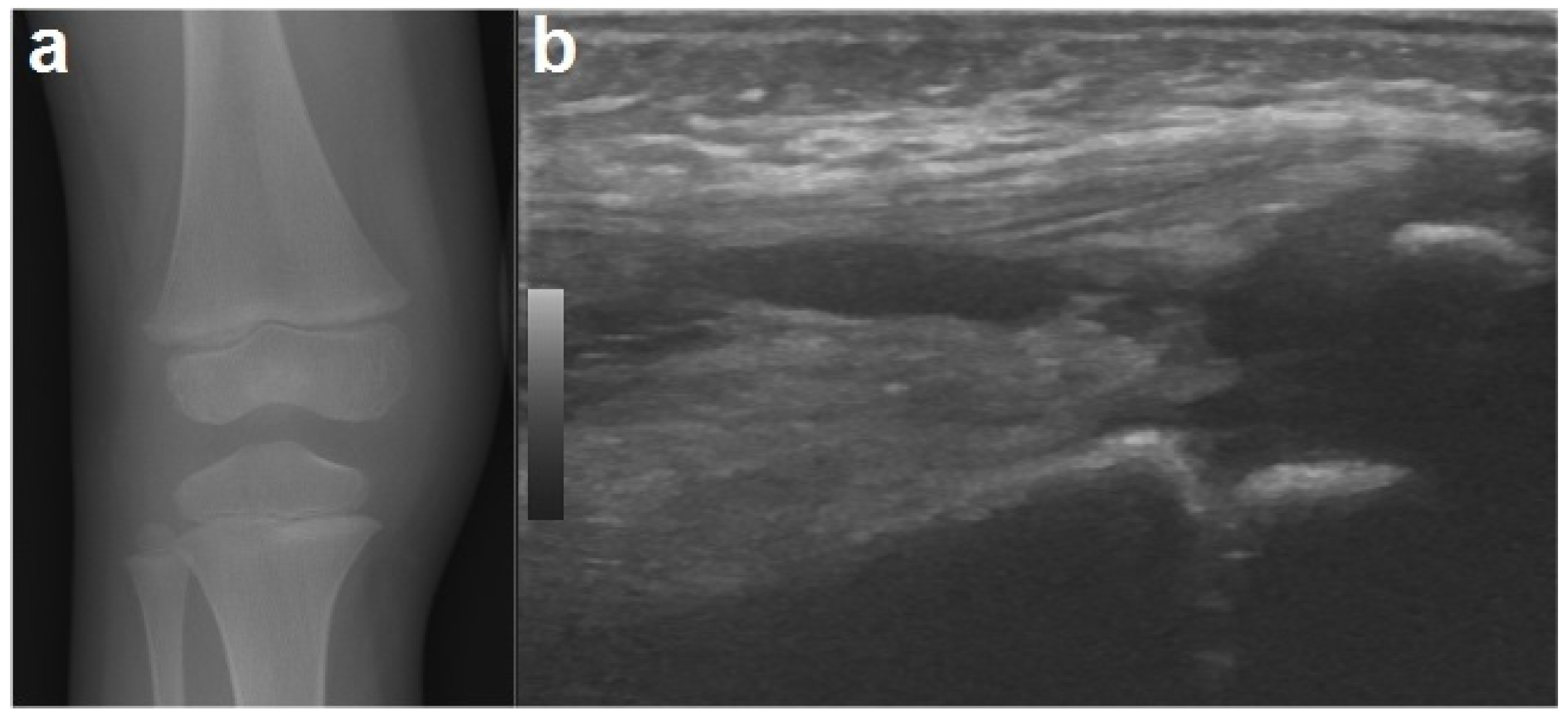
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- García-Arias, M.; Balsa, A.; Mola, E.M. Septic arthritis. Best Pract. Res. Clin. Rheumatol. 2011, 25, 407–421. [Google Scholar] [CrossRef] [PubMed]
- Lavy, C.B.; Peek, A.C.; Manjolo, G. The incidence of septic arthritis in Malawian children. Int. Orthop. 2005, 29, 195–196. [Google Scholar] [CrossRef] [PubMed]
- Swarup, I.; Meza, B.C.; Weltsch, D.; Jina, A.A.; Lawrence, J.T.; Baldwin, K.D. Septic arthritis of the knee in children: A critical analysis review. JBJS Rev. 2020, 8, e0069. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.N.; Sanghera, T.; Mangwani, J.; Paterson, J.M.; Ramachandran, M. The management of septic arthritis in children: Systematic review of the English language literature. J. Bone Jt. Surg. Br. 2009, 91, 1127–1133. [Google Scholar] [CrossRef] [PubMed]
- Gigante, A.; Coppa, V.; Marinelli, M.; Giampaolini, N.; Falcioni, D.; Specchia, N. Acute osteomyelitis and septic arthritis in children: A systematic review of systematic reviews. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 145–158. [Google Scholar] [CrossRef] [PubMed]
- Al Saadi, M.M.; Al Zamil, F.A.; Bokhary, N.A.; Al Shamsan, L.A.; Al Alola, S.A.; Al Eissa, Y.S. Acute septic arthritis in children. Pediatr. Int. 2009, 51, 377–380. [Google Scholar] [CrossRef] [PubMed]
- Bariteau, J.T.; Waryasz, G.R.; McDonnell, M.; Fischer, S.A.; Hayda, R.A.; Born, C.T. Fungal osteomyelitis and septic arthritis. J. Am. Acad. Orthop. Surg. 2014, 22, 390–401. [Google Scholar] [CrossRef]
- Shirtliff, M.E.; Mader, J.T. Acute septic arthritis. Clin. Microbiol. Rev. 2002, 15, 527–544. [Google Scholar] [CrossRef] [PubMed]
- Pääkkönen, M.; Peltola, H. Management of a child with suspected acute septic arthritis. Arch. Dis. Child. 2012, 97, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Arnold, J.C.; Bradley, J.S. Osteoarticular infections in children. Infect. Dis. Clin. N. Am. 2015, 29, 557–574. [Google Scholar] [CrossRef]
- Williams, N.; Cooper, C.; Cundy, P. Kingella kingae septic arthritis in children: Recognising an elusive pathogen. J. Child. Orthop. 2014, 8, 91–95. [Google Scholar] [CrossRef]
- Bernstein, D.T.; Haruno, L.S.; Daram, S.; Dawson, J.R.; Zhang, W.; Rosenfeld, S.B. Patient factors associated with methicillin-resistant staphylococcus aureus septic arthritis in children. Orthopedics 2018, 41, e277–e282. [Google Scholar] [CrossRef]
- Moumile, K.; Merckx, J.; Glorion, C.; Pouliquen, J.C.; Berche, P.; Ferroni, A. Bacterial aetiology of acute osteoarticular infections in children. Acta Paediatr. 2005, 94, 419–422. [Google Scholar] [CrossRef]
- Goergens, E.D.; McEvoy, A.; Watson, M.; Barrett, I.R. Acute osteomyelitis and septic arthritis in children. Paediatr. Child. Health. 2005, 41, 59–62. [Google Scholar] [CrossRef]
- Moro-Lago, I.; Talavera, G.; Moraleda, L.; González-Morán, G. Clinical presentation and treatment of septic arthritis in children. Rev. Española de Cirugía Ortopédica y Traumatol. 2017, 61, 170–175. [Google Scholar] [CrossRef] [PubMed]
- Kocher, M.S.; Zurakowski, D.; Kasser, J.R. Differentiating between septic arthritis and transient synovitis of the hip in children: An evidence-based clinical prediction algorithm. J. Bone Jt. Surg. 1999, 81, 1662–1670. [Google Scholar] [CrossRef]
- Caird, M.S.; Flynn, J.M.; Leung, Y.L.; Millman, J.E.; Joann, G.D.; Dormans, J.P. Factors distinguishing septic arthritis from transient synovitis of the hip in children. A prospective study. J. Bone Jt. Surg. 2006, 88, 1251–1257. [Google Scholar] [CrossRef]
- Obey, M.R.; Minaie, A.; Schipper, J.A.; Hosseinzadeh, P. Pediatric septic arthritis of the knee: Predictors of septic hip do not apply. J. Pediatr. Orthop. 2019, 39, e769–e772. [Google Scholar] [CrossRef]
- Saavedra-Lozano, J.; Falup-Pecurariu, O.; Faust, S.N.; Girschick, H.; Hartwig, N.; Kaplan, S.; Lorrot, M.; Mantadakis, E.; Peltola, H.; Rojo, P.; et al. Bone and Joint Infections. Pediatr. Infect. Dis. J. 2017, 36, 788–799. [Google Scholar] [CrossRef]
- Calvo, C.; Núñez, E.; Camacho, M.; Clemente, D.; Fernández-Cooke, E.; Alcobendas, R.; Mayol, L.; Soler-Palacin, P.; Oscoz, M.; Saavedra-Lozano, J. Epidemiology and management of acute, uncomplicated septic arthritis and osteomyelitis: Spanish multicenter study. Pediatr. Infect. Dis. J. 2016, 35, 1288–1293. [Google Scholar] [CrossRef]
- Autore, G.; Bernardi, L.; Esposito, S. Update on Acute Bone and Joint Infections in Paediatrics: A Narrative Review on the Most Recent Evidence-Based Recommendations and Appropriate Antinfective Therapy. Antibiotics 2020, 6, 486. [Google Scholar] [CrossRef] [PubMed]
- Pääkkönen, M. Septic arthritis in children: Diagnosis and treatment. Pediatric Health Med. Ther. 2017, 8, 65–68. [Google Scholar] [CrossRef]
- Yagupsky, P. Microbiological diagnosis of skeletal system infections in children. Curr. Pediatr. Rev. 2019, 15, 154–163. [Google Scholar] [CrossRef] [PubMed]
- Manz, N.; Krieg, A.H.; Heininger, U.; Ritz, N. Evaluation of the current use of imaging modalities and pathogen detection in children with acute osteomyelitis and septic arthritis. Eur. J. Pediatr. 2018, 177, 1071–1080. [Google Scholar] [CrossRef] [PubMed]
- McGillicuddy, D.C.; Shah, K.H.; Friedberg, R.P.; Nathanson, L.A.; Edlow, J.A. How sensitive is the synovial fluid white blood cell count in diagnosing septic arthritis? Am. J. Emerg. Med. 2007, 25, 749–752. [Google Scholar] [CrossRef] [PubMed]
- Lyon, R.M.; Evanich, J.D. Culture-negative septic arthritis in children. J. Pediatr. Orthop. 1999, 19, 655–659. [Google Scholar] [CrossRef]
- Christian, S.; Kraas, J.; Conway, W.F. Musculoskeletal infections. Semin. Roentgenol. 2007, 42, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Wall, C.; Donnan, L. Septic arthritis in children. Aust. Fam. Physician. 2015, 44, 213–215. [Google Scholar]
- Agarwal, A.; Aggarwal, A.N. Bone and joint infections in children: Septic arthritis. Indian J. Pediatr. 2016, 83, 825–833. [Google Scholar] [CrossRef]
- Yokoyama, K.; Yamamoto, Y.; Ukai, T.; Ebihara, G.; Watanabe, M. A patient with pediatric septic arthritis of the hip complicated with osteomyelitis responds to clindamycin. Tokai J. Exp. Clin. Med. 2019, 44, 113–117. [Google Scholar] [PubMed]
- Jagodzinski, N.A.; Kanwar, P.; Graham, K.; Bache, C.E. Prospective evaluation of a shortened regimen of treatment for acute osteomyelitis and septic arthritis in children. J. Pediatr. Orthop. 2009, 29, 518–525. [Google Scholar] [CrossRef]
- Lavy, C.B.; Thyoka, M. For how long should antibiotics be given in acute paediatric septic arthritis? A prospective audit of 96 cases. Trop. Doct. 2007, 37, 195–197. [Google Scholar] [CrossRef]
- Peltola, H.; Pääkkönen, M.; Kallio, P.; Kallio, M.J.T.; Osteomyelitis-Septic Arthritis (OMSA) Study Group. Prospective, randomized trial of 10 days versus 30 days of antimicrobial treatment, including a short-term course of parenteral therapy, for childhood septic arthritis. Clin. Infect. Dis. 2009, 48, 1201–1210. [Google Scholar] [CrossRef] [PubMed]
- Ross, J.J. Septic arthritis of native joints. Infect. Dis. Clin. N. Am. 2017, 31, 203–218. [Google Scholar] [CrossRef]
- Branson, J.; Vallejo, J.G.; Flores, A.R.; Hulten, K.G.; Mason, E.O.; Kaplan, S.L.; McNeil, J.C. The contemporary microbiology and rates of concomitant osteomyelitis in acute septic arthritis. Pediatr. Infect. Dis. J. 2017, 36, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Bynum, D.K., Jr.; Nunley, J.A.; Goldner, J.L.; Martinez, S. Pyogenic arthritis: Emphasis on the need for surgical drainage of the infected joint. South. Med. J. 1982, 75, 1232–1235, 1238. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, N.I.; Epps, H.R. Pediatric septic arthritis. Orthop. Clin. N. Am. 2017, 48, 209–216. [Google Scholar] [CrossRef]
- Givon, U.; Liberman, B.; Schindler, A.; Blankstein, A.; Ganel, A. Treatment of septic arthritis of the hip joint by repeated ultrasound-guided aspirations. J. Pediatr. Orthop. 2004, 24, 266–270. [Google Scholar] [CrossRef] [PubMed]


| Antimicrobial Agent | Antibiotic Susceptibility |
|---|---|
| Amoxicillin | Sensitive |
| Amoxiclav | Sensitive |
| Ampicillin | Sensitive |
| Azithromycin | Sensitive |
| Cefaclor | Sensitive |
| Clarithromycin | Sensitive |
| Clindamycin | Sensitive |
| Erythromycin | Sensitive |
| Levofloxacin | Sensitive |
| Penicillin | Sensitive |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Pietro, G.M.; Borzani, I.M.; Aleo, S.; Bosis, S.; Marchisio, P.; Tagliabue, C. Pediatric Septic Arthritis of the Knee Due to a Multi-Sensitive Streptococcus pyogenes Strain Responsive to Clindamycin—A Case Report. Children 2021, 8, 189. https://doi.org/10.3390/children8030189
Di Pietro GM, Borzani IM, Aleo S, Bosis S, Marchisio P, Tagliabue C. Pediatric Septic Arthritis of the Knee Due to a Multi-Sensitive Streptococcus pyogenes Strain Responsive to Clindamycin—A Case Report. Children. 2021; 8(3):189. https://doi.org/10.3390/children8030189
Chicago/Turabian StyleDi Pietro, Giada Maria, Irene Maria Borzani, Sebastiano Aleo, Samantha Bosis, Paola Marchisio, and Claudia Tagliabue. 2021. "Pediatric Septic Arthritis of the Knee Due to a Multi-Sensitive Streptococcus pyogenes Strain Responsive to Clindamycin—A Case Report" Children 8, no. 3: 189. https://doi.org/10.3390/children8030189
APA StyleDi Pietro, G. M., Borzani, I. M., Aleo, S., Bosis, S., Marchisio, P., & Tagliabue, C. (2021). Pediatric Septic Arthritis of the Knee Due to a Multi-Sensitive Streptococcus pyogenes Strain Responsive to Clindamycin—A Case Report. Children, 8(3), 189. https://doi.org/10.3390/children8030189






