A Case of Prenatally Diagnosed Uhl’s Anomaly with Absent Pulmonary Valve Leaflets and Dysplastic Tricuspid Valve
Abstract
1. Introduction
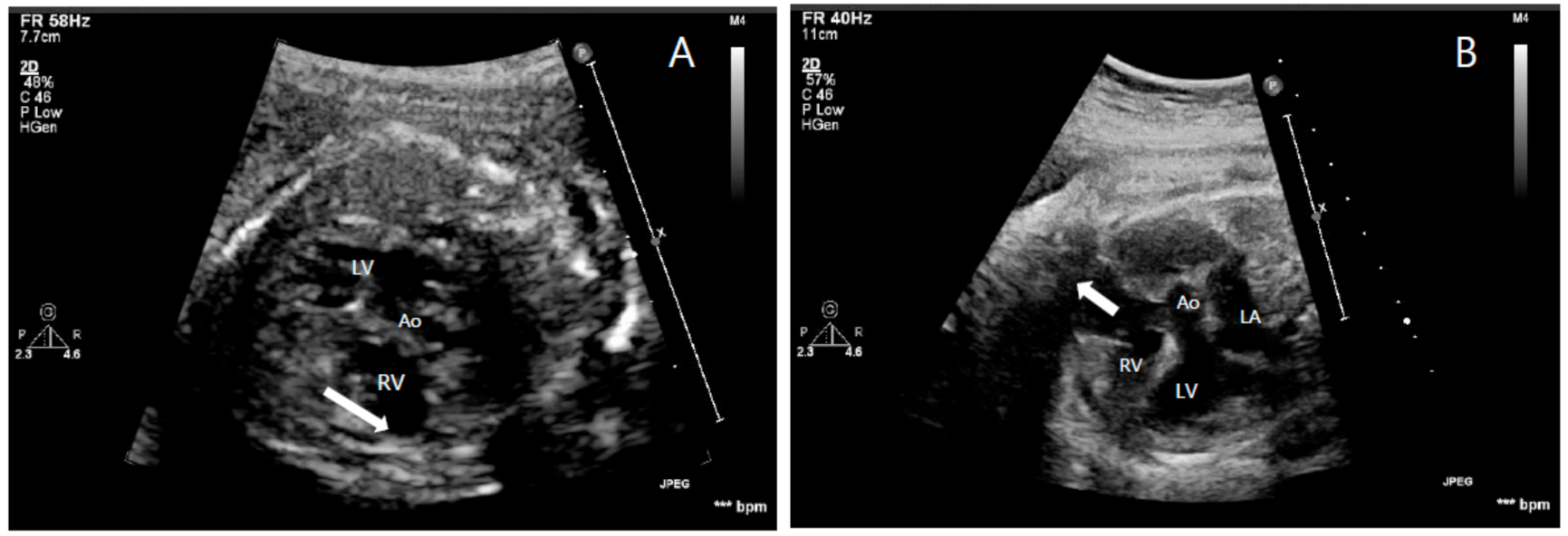
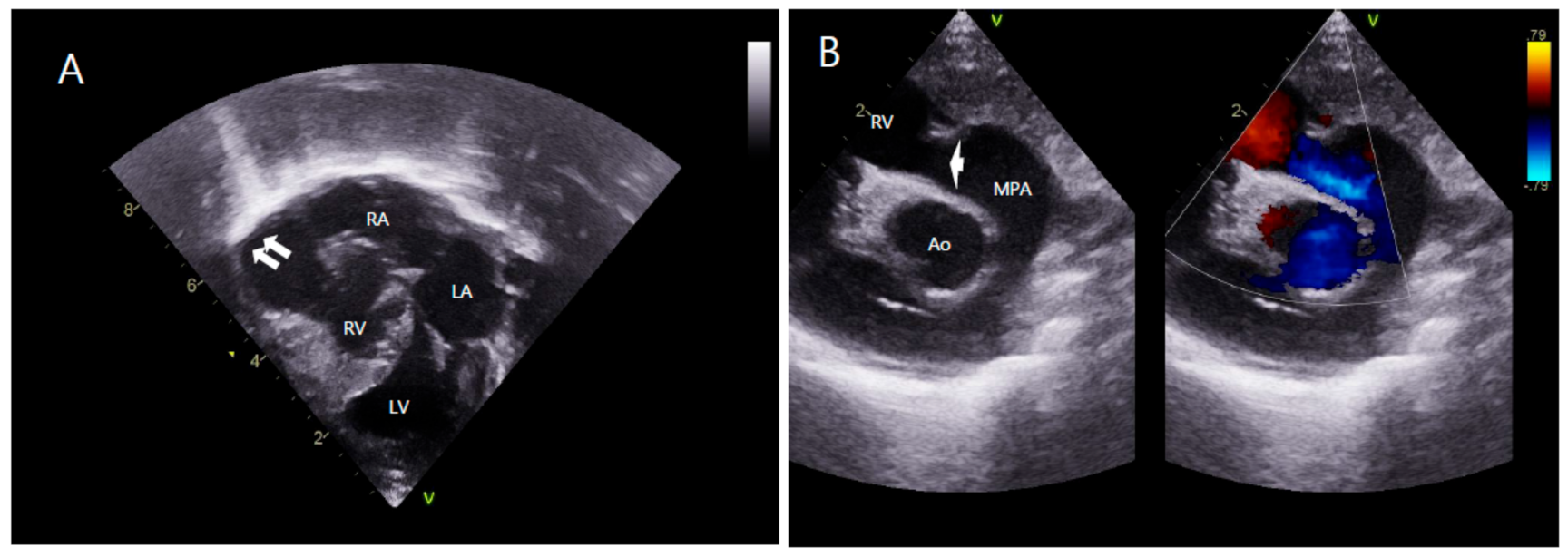
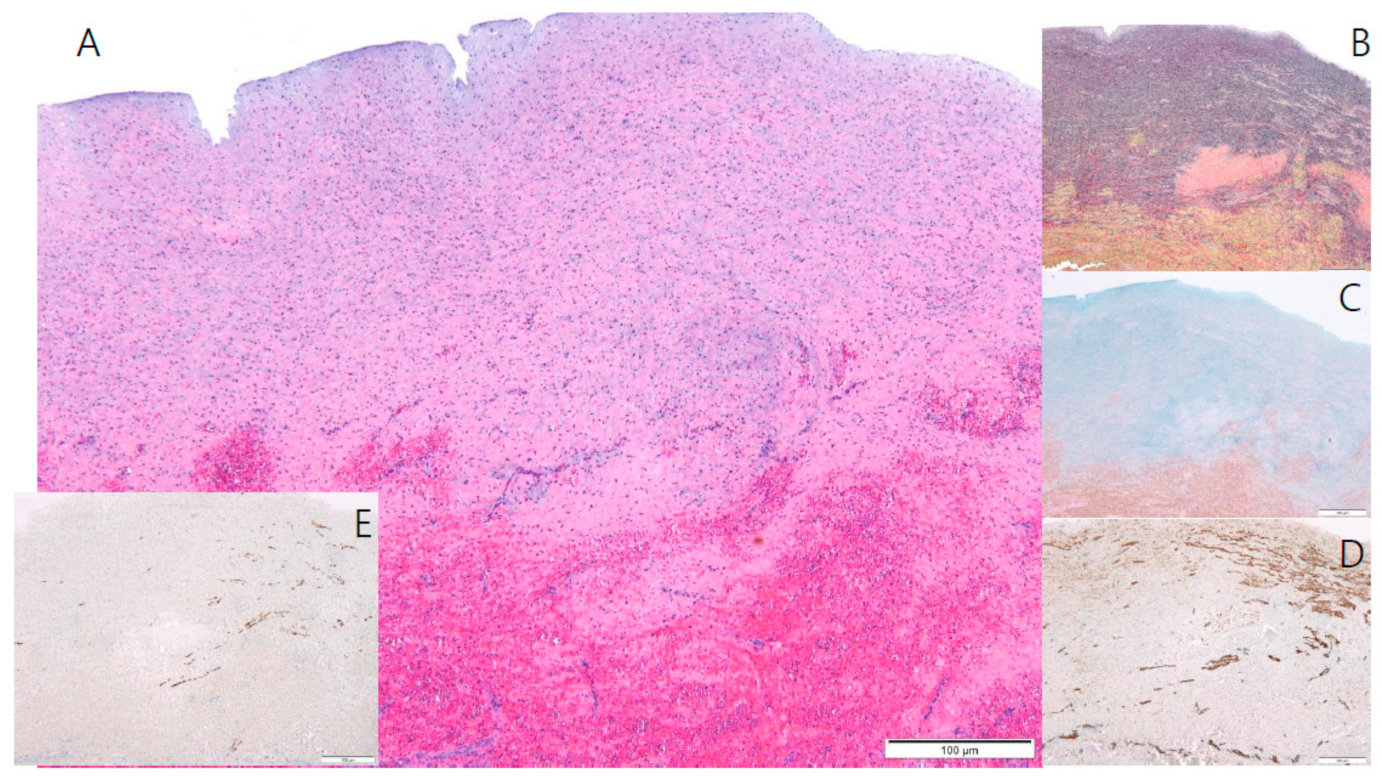
2. Case Report
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Uhl, H.S. A previously undescribed congenital malformation of the heart: Almost total absence of the myocardium of the right ventricle. Bull. Johns Hopkins Hosp. 1952, 91, 197–209. [Google Scholar]
- Uhl, H.S. Uhl’s anomaly revisited. Circulation 1996, 93, 1483–1484. [Google Scholar] [CrossRef]
- Van der Palen, R.L.; van der Wal, A.C.; Robles de Medina, P.G.; Blom, N.A.; Clur, S.A. Uhl’s anomaly: Clinical spectrum and pathophysiology. Int. J. Cardiol. 2016, 209, 118–121. [Google Scholar] [CrossRef]
- Osler, W.M. The Principles and Practice of Medicine, 6th ed.; D. Appleton: New York, NY, USA, 1905; p. 280. [Google Scholar]
- Gerlis, L.M.; Schmidt-Ott, S.C.; Ho, S.Y.; Anderson, R.A. Dysplastic conditions of the right ventricular myocardium: Uhl’s anomaly vs arrhythmogenic right ventricular dysplasia. Br. Heart J. 1993, 69, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Mihos, C.G.; Larrauri-Reyes, M.; Yucel, E.; Santana, O. Clinical presentation and echocardiographic characteristics of Uhl’s anomaly. Echocardiography 2017, 34, 299–302. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.F.; Mohammed, T.L.; Griffith, B.P.; White, C.S. CT of Uhl’s anomaly in an adult. Int. J. Cardiovasc. Imaging 2005, 21, 663–666. [Google Scholar] [CrossRef] [PubMed]
- Feucht, M.; Christ, B.; Wilting, J. VEGF induces cardiovascular malformation and embryonic lethality. Am. J. Pathol. 1997, 151, 1407–1416. [Google Scholar] [PubMed]
- Greer, M.L.; MacDonald, C.; Adatia, I. MRI of Uhl’s anomaly. Circulation 2000, 101, e230–e232. [Google Scholar] [CrossRef] [PubMed]
- Kilinc, M.; Akademir, I.; Sivasli, E. A case of Uhl’s anomaly presenting with severe right heart failure. Acta Cardiol. 2000, 55, 367–369. [Google Scholar] [CrossRef] [PubMed]
- Cammalleri, V.; Forcina, M.; Pugliese, L.; Romeo, F.; Floris, R.; Chiochi, M. Uhl anomaly in asymptomatic adult woman. Circ. Cardiovasc. Imaging 2019, 12, e008277. [Google Scholar] [CrossRef] [PubMed]
- Otmani, A.; Leborgne, L.; Renard, C.; Bakkour, H.; Quenum, S.; Tribouilloy, C.; Rey, J.L. Images in cardiovascular medicine. Electrocardiogram, Echocardiography, and Magnetic resonance imaging characteristics in Uhl’s disease. Circulation 2007, 115, e11–e12. [Google Scholar] [CrossRef]
- Taksande, A.; Gautami, V. Uhl’s anomaly with absent tricuspid valve in an infant. J. Cardiovasc. Echogr. 2015, 25, 90–92. [Google Scholar] [CrossRef] [PubMed]
- Azhari, N.; Assaqqat, M.; Bulbul, Z. Successful surgical repair of Uhl’s anomaly. Cardiol. Young 2002, 12, 192–195. [Google Scholar] [CrossRef] [PubMed]
- Yoshii, S.; Suzuki, S.; Hosaka, S.; Osawa, H.; Takahashi, W.; Takizawa, K.; Abraham, S.J.K.; Tada, Y.; Sugiyama, H.; Tan, T.; et al. A case of Uhl anomaly treated with one and a half ventricle repair combined with partial right ventriculectomy in infancy. J. Thorac. Cardiovasc. Surg. 2001, 122, 1026–1028. [Google Scholar] [CrossRef][Green Version]
- Ikari, N.M.; Azeka, E.; Aiello, V.D.; Atik, E.; Barbero-Marcial, M.; Ebaid, M. Uhl’s anomaly. Differential diagnosis and indications for cardiac transplantation in an infant. Arq. Bras. Cardiol. 2001, 77, 69–76. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, T.; Ko, H.; Byun, J.-H.; Lee, H.D.; Kim, H.; Choi, K.; Na, J.-Y. A Case of Prenatally Diagnosed Uhl’s Anomaly with Absent Pulmonary Valve Leaflets and Dysplastic Tricuspid Valve. Children 2021, 8, 190. https://doi.org/10.3390/children8030190
Kim T, Ko H, Byun J-H, Lee HD, Kim H, Choi K, Na J-Y. A Case of Prenatally Diagnosed Uhl’s Anomaly with Absent Pulmonary Valve Leaflets and Dysplastic Tricuspid Valve. Children. 2021; 8(3):190. https://doi.org/10.3390/children8030190
Chicago/Turabian StyleKim, Taehong, Hoon Ko, Joung-Hee Byun, Hyoung Doo Lee, Hyungtae Kim, Kwangho Choi, and Joo-Young Na. 2021. "A Case of Prenatally Diagnosed Uhl’s Anomaly with Absent Pulmonary Valve Leaflets and Dysplastic Tricuspid Valve" Children 8, no. 3: 190. https://doi.org/10.3390/children8030190
APA StyleKim, T., Ko, H., Byun, J.-H., Lee, H. D., Kim, H., Choi, K., & Na, J.-Y. (2021). A Case of Prenatally Diagnosed Uhl’s Anomaly with Absent Pulmonary Valve Leaflets and Dysplastic Tricuspid Valve. Children, 8(3), 190. https://doi.org/10.3390/children8030190





