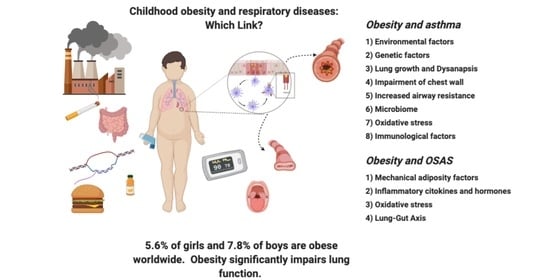
Childhood Obesity and Respiratory Diseases: Which Link?
Abstract
1. Introduction
2. Obesity and Asthma
2.1. Obesity and Asthma: Pathogenesis
2.1.1. Environmental Factors
2.1.2. Genetics
2.1.3. Lung Growth
2.1.4. Lung Function
2.1.5. Mechanical and Inflammatory Mechanisms
2.1.6. Oxidative Stress
2.1.7. Microbiome
2.2. Treatment
3. Obesity and OSAS
3.1. Obesity and OSAS: Diagnosis
3.2. Obesity and OSAS: A Bidirectional Causality
4. Obesity and COVID 19
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Noncommunicable Diseases: Childhood Overweight and Obesity. Available online: https://www.who.int/news-room/q-a-detail/noncommunicable-diseases-childhood-overweight-and-obesity (accessed on 29 December 2020).
- Llewellyn, A.; Simmonds, M.C.; Owen, C.G.; Woolacott, N. Childhood obesity as a predictor of morbidity in adulthood: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 56–67. [Google Scholar] [CrossRef]
- Hales, C.M.; Fryar, C.D.; Carroll, M.D.; Freedman, D.S.; Ogden, C.L. Trends in Obesity and Severe Obesity Prevalence in US Youth and Adults by Sex and Age, 2007–2008 to 2015–2016. JAMA 2018, 319, 1723–1725. [Google Scholar] [CrossRef] [PubMed]
- Global Nutrition Report Shining a Light to Spur Action on Nutrition 2018. World Health Organization. Available online: https://www.who.int/nutrition/globalnutritionreport/2018_Global_Nutrition_Report.pdf (accessed on 30 December 2020).
- Bentham, J.; Di Cesare, M.; Bilano, V.; Bixby, H.; Zhou, B.; Stevens, G.A.; Riley, L.M.; Taddei, C.; Hajifathalian, K.; Lu, Y.; et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- Valerio, G.; Maffeis, C.; Saggese, G.; Ambruzzi, M.A.; Balsamo, A.; Bellone, S.; Bergamini, M.; Bernasconi, S.; Bona, G.; Calcaterra, V.; et al. Diagnosis, treatment and prevention of pediatric obesity: Consensus position statement of the Italian Society for Pediatric Endocrinology and Diabetology and the Italian Society of Pediatrics. Ital. J. Pediatr. 2018, 44, 1–21. [Google Scholar] [CrossRef]
- Ayer, J.; Charakida, M.; Deanfield, J.E.; Celermajer, D.S. Lifetime risk: Childhood obesity and cardiovascular risk. Eur. Heart J. 2015, 36, 1371–1376. [Google Scholar] [CrossRef] [PubMed]
- Pulgaron, E.R.; Delamater, A.M. Obesity and Type 2 Diabetes in Children: Epidemiology and Treatment. Curr. Diabetes Rep. 2014, 14, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Di Bonito, P.; Pacifico, L.; Chiesa, C.; Valerio, G.; Miraglia del Giudice, E.; Maffeis, C.; Morandi, A.; Invitti, C.; Licenziati, M.R.; Loche, S.; et al. Impaired fasting glucose and impaired glucose tolerance in children and adolescents with overweight/obesity. J. Endocrinol. Investig. 2017, 40, 409–416. [Google Scholar] [CrossRef]
- Casavalle, P.L.; Lifshitz, F.; Romano, L.S.; Pandolfo, M.; Caamaño, A.; Boyer, P.M.; Rodríguez, P.N.; Friedman, S.M. Prevalence of dyslipidemia and metabolic syndrome risk factor in overweight and obese children. Pediatr. Endocrinol. Rev. 2014, 12, 213–223. [Google Scholar]
- Vajro, P.; Lenta, S.; Socha, P.; Dhawan, A.; McKiernan, P.; Baumann, U.; Durmaz, O.; Lacaille, F.; McLin, V.; Nobili, V. Diagnosis of Nonalcoholic Fatty Liver Disease in Children and Adolescents. J. Pediatr. Gastroenterol. Nutr. 2012, 54, 700–713. [Google Scholar] [CrossRef] [PubMed]
- Savino, A.; Pelliccia, P.; Chiarelli, F.; Mohn, A. Obesity-Related Renal Injury in Childhood. Horm. Res. Paediatr. 2010, 73, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Chan, G.; Chen, C.T. Musculoskeletal effects of obesity. Curr. Opin. Pediatr. 2009, 21, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Cardinale, F.; Ciprandi, G.; Barberi, S.; Bernardini, R.; Caffarelli, C.; Calvani, M.; Cavagni, G.; Galli, E.; Minasi, D.; Del Giudice, M.M.; et al. Consensus statement of the Italian society of pediatric allergy and immunology for the pragmatic management of children and adolescents with allergic or immunological diseases during the COVID-19 pandemic. Ital. J. Pediatr. 2020, 46, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Dixon, A.E.; Peters, U. The effect of obesity on lung function. Expert Rev. Respir. Med. 2018, 12, 755–767. [Google Scholar] [CrossRef] [PubMed]
- Lang, J.E.; Bunnell, H.T.; Hossain, J.; Wysocki, T.; Lima, J.J.; Finkel, T.H.; Bacharier, L.; Dempsey, A.; Sarzynski, L.; Test, M.; et al. Being Overweight or Obese and the Development of Asthma. Pediatrics 2018, 142, e20182119. [Google Scholar] [CrossRef]
- Chen, Y.C.; Dong, G.H.; Lin, K.C.; Lee, Y.L. Gender difference of childhood overweight and obesity in predicting the risk of incident asthma: A systematic review and meta-analysis. Obes. Rev. 2012, 14, 222–231. [Google Scholar] [CrossRef]
- Santamaría, F.; Montella, S.; Pietrobelli, A. Obesity and pulmonary disease: Unanswered questions. Obes. Rev. 2012, 13, 822–833. [Google Scholar] [CrossRef]
- Taytard, J.; Dubern, B.; Aubertin, G. Prise de poids chez l’enfant: Quels risques respiratoires ? Rev. Mal. Respir. 2019, 36, 1139–1147. [Google Scholar] [CrossRef] [PubMed]
- Hannon, T.S.; Rofey, D.L.; Ryan, C.M.; Clapper, D.A.; Chakravorty, S.; Arslanian, S.A. Relationships among Obstructive Sleep Apnea, Anthropometric Measures, and Neurocognitive Functioning in Adolescents with Severe Obesity. J. Pediatr. 2012, 160, 732–735. [Google Scholar] [CrossRef]
- Leone, N.; Courbon, D.; Thomas, F.; Bean, K.; Jego, B.; Leynaert, B.; Guize, L.; Zureik, M. Lung Function Impairment and the Metabolic Syndrome: The Critical Role of Abdominal Obesity. In Proceedings of the American Thoracic Society 2009 International Conference, San Diego, CA, USA, 15–20 May 2009; Volume 179, pp. 509–516. [Google Scholar] [CrossRef]
- Suratt, B.T.; Ubags, N.D.J.; Rastogi, D.; Tantisira, K.G.; Marsland, B.J.; Petrache, I.; Allen, J.B.; Bates, J.H.T.; Holguin, F.; McCormack, M.C.; et al. An Official American Thoracic Society Workshop Report: Obesity and Metabolism. An Emerging Frontier in Lung Health and Disease. Ann. Am. Thorac. Soc. 2017, 14, 1050–1059. [Google Scholar] [CrossRef] [PubMed]
- Forno, E.; Han, Y.-Y.; Mullen, J.; Celedón, J.C. Overweight, Obesity, and Lung Function in Children and Adults—A Meta-analysis. J. Allergy Clin. Immunol. Pract. 2018, 6, 570–581.e10. [Google Scholar] [CrossRef]
- Forno, E.; Celedón, J.C. The effect of obesity, weight gain, and weight loss on asthma inception and control. Curr. Opin. Allergy Clin. Immunol. 2017, 17, 123–130. [Google Scholar] [CrossRef]
- Weinmayr, G.; Forastiere, F.; Büchele, G.; Jaensch, A.; Strachan, D.P.; Nagel, G.; the ISAAC Phase Two Study Group. Overweight/Obesity and Respiratory and Allergic Disease in Children: International Study of Asthma and Allergies in Childhood (ISAAC) Phase Two. PLoS ONE 2014, 9, e113996. [Google Scholar] [CrossRef]
- Mebrahtu, T.F.; Feltbower, R.G.; Greenwood, D.C.; Parslow, R.C. Childhood body mass index and wheezing disorders: A systematic review and meta-analysis. Pediatr. Allergy Immunol. 2015, 26, 62–72. [Google Scholar] [CrossRef]
- Granell, R.; Henderson, A.J.; Evans, D.M.; Smith, G.D.; Ness, A.R.; Lewis, S.; Palmer, T.M.; Sterne, J.A.C. Effects of BMI, Fat Mass, and Lean Mass on Asthma in Childhood: A Mendelian Randomization Study. PLoS Med. 2014, 11, e1001669. [Google Scholar] [CrossRef] [PubMed]
- Peters, U.; Dixon, A.E.; Forno, E. Obesity and asthma. J. Allergy Clin. Immunol. 2018, 141, 1169–1179. [Google Scholar] [CrossRef] [PubMed]
- Beuther, D.A.; Sutherland, E.R. Overweight, obesity, and incident asthma: A meta-analysis of prospective epidemiologic studies. Am. J. Respir. Crit. Care Med. 2007, 175, 661–666. [Google Scholar] [CrossRef] [PubMed]
- Contreras, Z.A.; Chen, Z.; Roumeliotaki, T.; Annesi-Maesano, I.; Baïz, N.; von Berg, A.; Bergström, A.; Crozier, S.; Duijts, L.; Ekström, S.; et al. Does early onset asthma increase childhood obesity risk? A pooled analysis of 16 European cohorts. Eur. Respir. J. 2018, 52. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, Z.; Berhane, K.; Urman, R.; Chatzi, V.L.; Breton, C.; Gilliland, F.D. The Dynamic Relationship Between Asthma and Obesity in Schoolchildren. Am. J. Epidemiol. 2020, 189, 583–591. [Google Scholar] [CrossRef]
- Jones, S.E.; Merkle, S.L.; Fulton, J.E.; Wheeler, L.S.; Mannino, D.M. Relationship between asthma, overweight, and physical activity among U.S. high school students. J. Community Health 2006, 31, 469–478. [Google Scholar] [CrossRef]
- Vangeepuram, N.; McGovern, K.J.; Teitelbaum, S.; Galvez, M.P.; Pinney, S.M.; Biro, F.M.; Kushi, L.H.; Wolff, M.S. Asthma and physical activity in multiracial girls from three US sites. J. Asthma 2013, 51, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Holguin, F.; Bleecker, E.R.; Busse, W.W.; Calhoun, W.J.; Castro, M.; Erzurum, S.C.; Fitzpatrick, A.M.; Gaston, B.; Israel, E.; Jarjour, N.N.; et al. Obesity and asthma: An association modified by age of asthma onset. J. Allergy Clin. Immunol. 2011, 127, 1486–1493.e2. [Google Scholar] [CrossRef] [PubMed]
- Lang, J.E.; Hossain, J.; Smith, K.; Lima, J.J. Asthma Severity, Exacerbation Risk, and Controller Treatment Burden in Underweight and Obese Children. J. Asthma 2012, 49, 456–463. [Google Scholar] [CrossRef]
- Ahmadizar, F.; Vijverberg, S.J.; Arets, H.G.; De Boer, A.; Lang, J.E.; Kattan, M.; Palmer, C.N.; Mukhopadhyay, S.; Turner, S.; Der Zee, A.H.M.-V. Childhood obesity in relation to poor asthma control and exacerbation: A meta-analysis. Eur. Respir. J. 2016, 48, 1063–1073. [Google Scholar] [CrossRef] [PubMed]
- Forno, E.; Lescher, R.; Strunk, R.; Weiss, S.; Fuhlbrigge, A.; Celedón, J.C. Decreased response to inhaled steroids in overweight and obese asthmatic children. J. Allergy Clin. Immunol. 2011, 127, 741–749. [Google Scholar] [CrossRef] [PubMed]
- Lang, J.E. Obesity and asthma in children: Current and future therapeutic options. Pediatr. Drugs 2014, 16, 179–188. [Google Scholar] [CrossRef]
- McGarry, M.E.; Castellanos, E.; Thakur, N.; Oh, S.S.; Eng, C.; Davis, A.; Meade, K.; LeNoir, M.A.; Avila, P.C.; Farber, H.J.; et al. Obesity and Bronchodilator Response in Black and Hispanic Children and Adolescents With Asthma. Chest 2015, 147, 1591–1598. [Google Scholar] [CrossRef]
- Black, M.H.; Zhou, H.; Takayanagi, M.; Jacobsen, S.J.; Koebnick, C. Increased Asthma Risk and Asthma-Related Health Care Complications Associated With Childhood Obesity. Am. J. Epidemiol. 2013, 178, 1120–1128. [Google Scholar] [CrossRef]
- Aragona, E.; El-Magbri, E.; Wang, J.; Scheckelhoff, T.; Scheckelhoff, T.; Hyacinthe, A.; Nair, S.; Khan, A.; Nino, G.; Pillai, D.K. Impact of Obesity on Clinical Outcomes in Urban Children Hospitalized for Status Asthmaticus. Hosp. Pediatr. 2016, 6, 211–218. [Google Scholar] [CrossRef]
- Okubo, Y.; Nochioka, K.; Hataya, H.; Sakakibara, H.; Terakawa, T.; Testa, M. Burden of Obesity on Pediatric Inpatients with Acute Asthma Exacerbation in the United States. J. Allergy Clin. Immunol. Pract. 2016, 4, 1227–1231. [Google Scholar] [CrossRef]
- Dhana, K.; Haines, J.; Liu, G.; Zhang, C.; Wang, X.; E Field, A.; E Chavarro, J.; Sun, Q. Association between maternal adherence to healthy lifestyle practices and risk of obesity in offspring: Results from two prospective cohort studies of mother-child pairs in the United States. BMJ 2018, 362, k2486. [Google Scholar] [CrossRef]
- Kim, J.S.; Alderete, T.L.; Chen, Z.; Lurmann, F.; Rappaport, E.; Habre, R.; Berhane, K.; Gilliland, F.D. Longitudinal associations of in utero and early life near-roadway air pollution with trajectories of childhood body mass index. Environ. Health 2018, 17, 1–10. [Google Scholar] [CrossRef]
- Buteau, S.; Doucet, M.; Tétreault, L.-F.; Gamache, P.; Fournier, M.; Brand, A.; Kosatsky, T.; Smargiassi, A. A population-based birth cohort study of the association between childhood-onset asthma and exposure to industrial air pollutant emissions. Environ. Int. 2018, 121, 23–30. [Google Scholar] [CrossRef]
- Burke, H.; Leonardi-Bee, J.; Hashim, A.; Pine-Abata, H.; Chen, Y.; Cook, D.G.; Britton, J.R.; McKeever, T.M. Prenatal and Passive Smoke Exposure and Incidence of Asthma and Wheeze: Systematic Review and Meta-analysis. Pediatrics 2012, 129, 735–744. [Google Scholar] [CrossRef] [PubMed]
- Mastrorilli, C.; Posa, D.; Cipriani, F.; Caffarelli, C. Asthma and allergic rhinitis in childhood: What’s new. Pediatr. Allergy Immunol. 2016, 27, 795–803. [Google Scholar] [CrossRef] [PubMed]
- Wood, L.G.; Garg, M.L.; Gibson, P.G. A high-fat challenge increases airway inflammation and impairs bronchodilator recovery in asthma. J. Allergy Clin. Immunol. 2011, 127, 1133–1140. [Google Scholar] [CrossRef]
- Kuo, N.-W.; Tung, K.-Y.; Tsai, C.-H.; Chen, Y.-C.; Lee, Y.L. β3-Adrenergic receptor gene modifies the association between childhood obesity and asthma. J. Allergy Clin. Immunol. 2014, 134, 731–733.e3. [Google Scholar] [CrossRef]
- Murphy, A.; Tantisira, K.G.; Soto-Quirós, M.E.; Avila, L.; Klanderman, B.J.; Lake, S.; Weiss, S.T.; Celedón, J.C. PRKCA: A Positional Candidate Gene for Body Mass Index and Asthma. Am. J. Hum. Genet. 2009, 85, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Murk, W.; Dewan, A.T. Genome-Wide Gene by Environment Interaction Analysis Identifies Common SNPs at 17q21.2 that Are Associated with Increased Body Mass Index Only among Asthmatics. PLoS ONE 2015, 10, e0144114. [Google Scholar] [CrossRef] [PubMed]
- Rastogi, D.; Suzuki, M.; Greally, J.M. Differential epigenome-wide DNA methylation patterns in childhood obesity-associated asthma. Sci. Rep. 2013, 3, srep02164. [Google Scholar] [CrossRef]
- Hallstrand, T.S.; Fischer, M.E.; Wurfel, M.M.; Afari, N.; Buchwald, D.; Goldberg, J. Genetic pleiotropy between asthma and obesity in a community-based sample of twins. J. Allergy Clin. Immunol. 2005, 116, 1235–1241. [Google Scholar] [CrossRef][Green Version]
- Ahangari, F.; Sood, A.; Ma, B.; Takyar, S.; Schuyler, M.; Qualls, C.; Cruz, C.S.D.; Chupp, G.L.; Lee, C.G.; Elias, J.A. Chitinase 3–like-1 Regulates Both Visceral Fat Accumulation and Asthma-like Th2 Inflammation. Am. J. Respir. Crit. Care Med. 2015, 191, 746–757. [Google Scholar] [CrossRef] [PubMed]
- Pellegrino, R.; Viegi, G.; Brusasco, V.; Crapo, R.O.; Burgos, F.; Casaburi, R.; Coates, A.; Van Der Grinten, C.P.M.; Gustafsson, P.; Hankinson, J.; et al. Interpretative strategies for lung function tests. Eur. Respir. J. 2005, 26, 948–968. [Google Scholar] [CrossRef]
- Jones, M.H.; Roncada, C.; Fernandes, M.T.C.; Heinzmann-Filho, J.P.; Icaza, E.E.S.; Mattiello, R.; Pitrez, P.M.C.; Pinto, L.A.; Stein, R.T. Asthma and Obesity in Children Are Independently Associated with Airway Dysanapsis. Front. Pediatr. 2017, 5, 270. [Google Scholar] [CrossRef] [PubMed]
- Forno, E.; Weiner, D.J.; Mullen, J.; Sawicki, G.; Kurland, G.; Han, Y.Y.; Cloutier, M.M.; Canino, G.; Weiss, S.T.; Litonjua, A.A.; et al. Obesity and Airway Dysanapsis in Children with and without Asthma. Am. J. Respir. Crit. Care Med. 2016, 195, 314–323. [Google Scholar] [CrossRef] [PubMed]
- Strunk, R.C.; Colvin, R.; Bacharier, L.B.; Fuhlbrigge, A.L.; Forno, E.; Arbelaez, A.M.; Tantisira, K.G.; Williams, P.; Lasley, M.V.; Chinn, T.; et al. Airway Obstruction Worsens in Young Adults with Asthma Who Become Obese. J. Allergy Clin. Immunol. Pract. 2015, 3, 765–771.e2. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.L.; Nzekwu, M.-M.U. The Effects of Body Mass Index on Lung Volumes. Chest 2006, 130, 827–833. [Google Scholar] [CrossRef]
- Gibeon, D.; Batuwita, K.; Osmond, M.; Heaney, L.G.; Brightling, C.E.; Niven, R.; Mansur, A.; Chaudhuri, R.; Bucknall, C.E.; Rowe, A.; et al. Obesity-associated severe asthma represents a distinct clinical phenotype analysis of the british thoracic society diffi cult asthma registry patient cohort according to bmi. Chest 2013, 143, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Pellegrino, R.; Gobbi, A.; Antonelli, A.; Torchio, R.; Gulotta, C.; Pellegrino, G.M.; Dellacà, R.; Hyatt, R.E.; Brusasco, V. Ventilation heterogeneity in obesity. J. Appl. Physiol. 2014, 116, 1175–1181. [Google Scholar] [CrossRef] [PubMed]
- Steier, J.; Lunt, A.; Hart, N.; I Polkey, M.; Moxham, J. Observational study of the effect of obesity on lung volumes. Thorax 2014, 69, 752–759. [Google Scholar] [CrossRef] [PubMed]
- Davidson, W.J.; Mackenzie-Rife, K.A.; Witmans, M.B.; Montgomery, M.D.; Ball, G.D.; Egbogah, S.; Eves, N.D. Obesity negatively impacts lung function in children and adolescents. Pediatr. Pulmonol. 2014, 49, 1003–1010. [Google Scholar] [CrossRef] [PubMed]
- Tantisira, K.G.; A Litonjua, A.; Weiss, S.T.; Fuhlbrigge, A.L. Association of body mass with pulmonary function in the Childhood Asthma Management Program (CAMP). Thorax 2003, 58, 1036–1041. [Google Scholar] [CrossRef]
- Ulger, Z.; Demir, E.; Tanaç, R.; Gökşen, D.; Gülen, F.; Darcan, S.; Can, D.; Coker, M. The effect of childhood obesity on respiratory function tests and airway hyperresponsiveness. Turk. J. Pediatr. 2006, 48, 43–50. [Google Scholar]
- Spathopoulos, D.; Paraskakis, E.; Trypsianis, G.; Tsalkidis, A.; Arvanitidou, V.; Emporiadou, M.; Bouros, D.; Chatzimichael, A. The effect of obesity on pulmonary lung function of school aged children in Greece. Pediatr. Pulmonol. 2009, 44, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Baek, H.-S.; Kim, Y.-D.; Shin, J.-H.; Kim, J.-H.; Oh, J.-W.; Lee, H.-B. Serum leptin and adiponectin levels correlate with exercise-induced bronchoconstriction in children with asthma. Ann. Allergy Asthma Immunol. 2011, 107, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Shore, S.A. Obesity and asthma: Possible mechanisms. J. Allergy Clin. Immunol. 2008, 121, 1087–1093. [Google Scholar] [CrossRef]
- Litonjua, A.A.; Sparrow, D.; Celedon, J.C.; DeMolles, D.; Weiss, S.T. Association of body mass index with the development of methacholine airway hyperresponsiveness in men: The Normative Aging Study. Thorax 2002, 57, 581–585. [Google Scholar] [CrossRef] [PubMed]
- Sposato, B.; Scalese, M.; Migliorini, M.G.; Riccardi, M.P.; Balducci, M.T.; Petruzzelli, L.; Scala, R. Obesity can influence children’s and adolescents’ airway hyperresponsiveness differently. Multidiscip. Respir. Med. 2013, 8, 60. [Google Scholar] [CrossRef] [PubMed]
- Benedetti, F.J.; Bosa, V.L.; Giesta, J.M.; Fischer, G.B. Anthropometric indicators of general and central obesity in the prediction of asthma in adolescents; central obesity in asthma. Nutr. Hosp. 2015, 32, 2540–2548. [Google Scholar] [CrossRef]
- Sideleva, O.; Suratt, B.T.; Black, K.E.; Tharp, W.G.; Pratley, R.E.; Forgione, P.; Dienz, O.; Irvin, C.G.; Dixon, A.E. Obesity and asthma: An inflammatory disease of adipose tissue not the airway. Am. J. Respir. Crit. Care Med. 2012, 186, 598–605. [Google Scholar] [CrossRef] [PubMed]
- Periyalil, H.A.; Wood, L.G.; Wright, T.A.; Karihaloo, C.; Starkey, M.R.; Miu, A.S.; Baines, K.J.; Hansbro, P.M.; Gibson, P.G. Obese asthmatics are characterized by altered adipose tissue macrophage activation. Clin. Exp. Allergy 2018, 48, 641–649. [Google Scholar] [CrossRef] [PubMed]
- Torday, J.S.; E Sunday, M.; Wang, L.; Torres, E. Leptin mediates the parathyroid hormone-related protein paracrine stimulation of fetal lung maturation. Am. J. Physiol. Cell. Mol. Physiol. 2002, 282, L405–L410. [Google Scholar] [CrossRef]
- Han, W.; Li, J.; Tang, H.; Sun, L. Treatment of obese asthma in a mouse model by simvastatin is associated with improving dyslipidemia and decreasing leptin level. Biochem. Biophys. Res. Commun. 2017, 484, 396–402. [Google Scholar] [CrossRef]
- Scott, H.A.; Gibson, P.G.; Garg, M.L.; Upham, J.W.; Wood, L.G. Sex hormones and systemic inflammation are modulators of the obese-asthma phenotype. Allergy 2016, 71, 1037–1047. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.C.; McGrath, K.W.; A Hawkins, G.; Hastie, A.T.; Levy, B.D.; Israel, E.; Phillips, B.R.; Mauger, D.T.; A Comhair, S.; Erzurum, S.C.; et al. Plasma interleukin-6 concentrations, metabolic dysfunction, and asthma severity: A cross-sectional analysis of two cohorts. Lancet Respir. Med. 2016, 4, 574–584. [Google Scholar] [CrossRef]
- Rastogi, D.; Canfield, S.M.; Andrade, A.; Isasi, C.R.; Hall, C.B.; Rubinstein, A.; Arens, R. Obesity-associated asthma in children a distinct entity. Chest 2012, 141, 895–905. [Google Scholar] [CrossRef] [PubMed]
- Lugogo, N.; Francisco, D.; Addison, K.J.; Manne, A.; Pederson, W.; Ingram, J.L.; Green, C.L.; Suratt, B.T.; Lee, J.J.; Sunday, M.E.; et al. Obese asthmatic patients have decreased surfactant protein A levels: Mechanisms and implications. J. Allergy Clin. Immunol. 2018, 141, 918–926.e3. [Google Scholar] [CrossRef] [PubMed]
- Caffarelli, C.; Calcinai, E.; Rinaldi, L.; Dascola, C.P.; Terracciano, L.; Corradi, M. Hydrogen Peroxide in Exhaled Breath Condensate in Asthmatic Children during Acute Exacerbation and after Treatment. Respiration 2012, 84, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Novosad, S.; Khan, S.; Wolfe, B.; Khan, A. Role of Obesity in Asthma Control, the Obesity-Asthma Phenotype. J. Allergy 2013, 2013, 1–9. [Google Scholar] [CrossRef]
- Grasemann, H.; Holguin, F. Oxidative stress and obesity-related asthma. Paediatr. Respir. Rev. 2020. [Google Scholar] [CrossRef] [PubMed]
- Caffarelli, C.; Cardinale, F.; Povesi-Dascola, C.; Dodi, I.; Mastrorilli, V.; Ricci, G. Use of probiotics in pediatric infectious diseases. Expert Rev. Anti-Infect. Ther. 2015, 13, 1517–1535. [Google Scholar] [CrossRef]
- Cho, Y.; Shore, S.A. Obesity, Asthma, and the Microbiome. Physiology 2016, 31, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Shore, S.A.; Cho, Y. Obesity and Asthma: Microbiome–Metabolome Interactions. Am. J. Respir. Cell Mol. Biol. 2016, 54, 609–617. [Google Scholar] [CrossRef] [PubMed]
- Kamada, N.; Núñez, G. Role of the Gut Microbiota in the Development and Function of Lymphoid Cells. J. Immunol. 2013, 190, 1389–1395. [Google Scholar] [CrossRef]
- Ivanov, I.I.; Atarashi, K.; Manel, N.; Brodie, E.L.; Shima, T.; Karaoz, U.; Wei, D.; Goldfarb, K.C.; Santee, C.A.; Lynch, S.V.; et al. Induction of Intestinal Th17 Cells by Segmented Filamentous Bacteria. Cell 2009, 139, 485–498. [Google Scholar] [CrossRef] [PubMed]
- Kamada, N.; Seo, S.-U.; Chen, G.Y.; Núñez, G. Role of the gut microbiota in immunity and inflammatory disease. Nat. Rev. Immunol. 2013, 13, 321–335. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.Y.; Lee, H.J.; Chang, Y.-J.; Pichavant, M.; Shore, S.A.; Fitzgerald, K.A.; Iwakura, Y.; Israel, E.; Bolger, K.; Faul, J.; et al. Interleukin-17–producing innate lymphoid cells and the NLRP3 inflammasome facilitate obesity-associated airway hyperreactivity. Nat. Med. 2014, 20, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Dixon, A.E.; Pratley, R.E.; Forgione, P.M.; Kaminsky, D.A.; Whittaker-Leclair, L.A.; Griffes, L.A.; Garudathri, J.; Raymond, D.; Poynter, M.E.; Bunn, J.Y.; et al. Effects of obesity and bariatric surgery on airway hyperresponsiveness, asthma control, and inflammation. J. Allergy Clin. Immunol. 2011, 128, 508–515.e2. [Google Scholar] [CrossRef]
- Jensen, M.E.; Gibson, P.G.; Collins, C.E.; Hilton, J.M.; Wood, L.G. Diet-induced weight loss in obese children with asthma: A randomized controlled trial. Clin. Exp. Allergy 2013, 43, 775–784. [Google Scholar] [CrossRef]
- Van Leeuwen, J.C.; Hoogstrate, M.; Duiverman, E.J.; Thio, B.J. Effects of dietary induced weight loss on exercise-induced bronchoconstriction in overweight and obese children. Pediatr. Pulmonol. 2014, 49, 1155–1161. [Google Scholar] [CrossRef]
- Willeboordse, M.; Van De Kant, K.D.G.; Tan, F.E.S.; Mulkens, S.; Schellings, J.; Crijns, Y.; Van Der Ploeg, L.; Van Schayck, C.P.; Dompeling, E. A Multifactorial Weight Reduction Programme for Children with Overweight and Asthma: A Randomized Controlled Trial. PLoS ONE 2016, 11, e0157158. [Google Scholar] [CrossRef]
- Lang, J.E.; Hossain, J.; Holbrook, J.T.; Teague, W.G.; Gold, B.D.; A Wise, R.; Lima, J.J. Gastro-oesophageal reflux and worse asthma control in obese children: A case of symptom misattribution? Thorax 2016, 71, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Telenga, E.D.; Tideman, S.W.; Kerstjens, H.A.M.; Hacken, N.H.T.T.; Timens, W.; Postma, D.S.; Berge, M.V.D. Obesity in asthma: More neutrophilic inflammation as a possible explanation for a reduced treatment response. Allergy 2012, 67, 1060–1068. [Google Scholar] [CrossRef] [PubMed]
- Wong, E.H.C.; Porter, J.D.; Edwards, M.R.; Johnston, S.L. The role of macrolides in asthma: Current evidence and future directions. Lancet Respir. Med. 2014, 2, 657–670. [Google Scholar] [CrossRef]
- Peppard, P.E.; Young, T.; Palta, M.; Dempsey, J.; Skatrud, J. Longitudinal Study of Moderate Weight Change and Sleep-Disordered Breathing. JAMA 2000, 284, 3015–3021. [Google Scholar] [CrossRef] [PubMed]
- Mallory, G.B.; Fiser, D.H.; Jackson, R. Sleep-associated breathing disorders in morbidly obese children and adolescents. J. Pediatr. 1989, 115, 892–897. [Google Scholar] [CrossRef]
- Silvestri, J.M.; Weese-Mayer, D.E.; Bass, M.T.; Kenny, A.S.; Hauptman, S.A.; Pearsall, S.M. Polysomnography in obese children with a history of sleep-associated breathing disorders. Pediatr. Pulmonol. 1993, 16, 124–129. [Google Scholar] [CrossRef] [PubMed]
- Elidemir, O.; Maciejewski, S.R.; Oermann, C.M. Obstructive sleep apnea syndrome in obese Singapore children. Pediatr. Pulmonol. 2000, 29, 284–290. [Google Scholar] [CrossRef]
- Marcus, C.L.; Curtis, S.; Koerner, C.B.; Joffe, A.; Serwint, J.R.; Loughlin, G.M. Evaluation of pulmonary function and polysomnography in obese children and adolescents. Pediatr. Pulmonol. 1996, 21, 176–183. [Google Scholar] [CrossRef]
- Verhulst, S.L.; Van Gaal, L.; De Backer, W.; Desager, K. The prevalence, anatomical correlates and treatment of sleep-disordered breathing in obese children and adolescents. Sleep Med. Rev. 2008, 12, 339–346. [Google Scholar] [CrossRef]
- Verhulst, S.L.; Aerts, L.; Jacobs, S.; Schrauwen, N.; Haentjens, D.; Claes, R.; Vaerenberg, H.; Van Gaal, L.F.; De Backer, W.A.; Desager, K.N. Sleep-Disordered Breathing, Obesity, and Airway Inflammation in Children and Adolescents. Chest 2008, 134, 1169–1175. [Google Scholar] [CrossRef] [PubMed]
- Kohler, M.J.; Heuvel, C.J.V.D. Is there a clear link between overweight/obesity and sleep disordered breathing in children? Sleep Med. Rev. 2008, 12, 347–361. [Google Scholar] [CrossRef]
- Kohler, M.J.; Thormaehlen, S.; Kennedy, J.D.; Pamula, Y.; Heuvel, C.J.V.D.; Lushington, K.; Martin, A.J. Differences in the Association Between Obesity and Obstructive Sleep Apnea Among Children and Adolescents. J. Clin. Sleep Med. 2009, 5, 506–511. [Google Scholar] [CrossRef] [PubMed]
- Wing, Y.K.; Hui, S.H.; Pak, W.M.; Ho, C.K.; Cheung, A.; Li, A.M.; Fok, T.F. A controlled study of sleep related disordered breathing in obese children. Arch. Dis. Child. 2003, 88, 1043–1047. [Google Scholar] [CrossRef]
- O’Brien, L.M.; Gozal, D. Autonomic Dysfunction in Children with Sleep-Disordered Breathing. Sleep 2005, 28, 747–752. [Google Scholar] [CrossRef] [PubMed]
- Berry, R.B.; Budhiraja, R.; Gottlieb, D.J.; Gozal, D.; Iber, C.; Kapur, V.K.; Marcus, C.L.; Mehra, R.; Parthasarathy, S.; Quan, S.F.; et al. Rules for Scoring Respiratory Events in Sleep: Update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J. Clin. Sleep Med. 2012, 8, 597–619. [Google Scholar] [CrossRef]
- Schechter, M.S. Technical report: Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 2002, 109, e69. [Google Scholar] [CrossRef] [PubMed]
- Nixon, G.M.; Kermack, F.A.S.; Davis, B.G.M.; Manoukian, J.J.; Brown, K.A.; Brouillette, R.T. Planning Adenotonsillectomy in Children With Obstructive Sleep Apnea: The Role of Overnight Oximetry. Pediatrics 2003, 113, e19–e25. [Google Scholar] [CrossRef] [PubMed]
- Marcus, C.L.; Brooks, L.J.; Draper, K.A.; Gozal, D.; Halbower, A.C.; Jones, J.; Schechter, M.S.; Sheldon, S.H.; Spruyt, K.; Ward, S.D.; et al. Diagnosis and Management of Childhood Obstructive Sleep Apnea Syndrome. Pediatrics 2012, 130, 576–584. [Google Scholar] [CrossRef] [PubMed]
- Paruthi, S.; Rosen, C.L.; Wang, R.; Weng, J.; Marcus, C.L.; Chervin, R.D.; Stanley, J.J.; Katz, E.S.; Amin, R.; Redline, S. End-Tidal Carbon Dioxide Measurement during Pediatric Polysomnography: Signal Quality, Association with Apnea Severity, and Prediction of Neurobehavioral Outcomes. Sleep 2015, 38, 1719–1726. [Google Scholar] [CrossRef] [PubMed]
- Maniscalco, M.; Zedda, A.; Faraone, S.; Carratù, P.; Sofia, M. Evaluation of a transcutaneous carbon dioxide monitor in severe obesity. Intensive Care Med. 2008, 34, 1340–1344. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, B.; Norman, M.; Sullivan, C.E.; Waters, K.A. TcCO 2 changes correlate with partial obstruction in children suspected of sleep disordered breathing. Pediatr. Pulmonol. 2020, 55, 2773–2781. [Google Scholar] [CrossRef] [PubMed]
- Don, D.; Osterbauer, B.; Nour, S.; Matar, M.; Do, R.M.; Bushman, G. Transcutaneous CO 2 Monitoring in Children Undergoing Tonsillectomy for Sleep Disordered Breathing. Laryngoscope 2020. [Google Scholar] [CrossRef] [PubMed]
- Kuvat, N.; Tanriverdi, H.; Armutcu, F. The relationship between obstructive sleep apnea syndrome and obesity: A new perspective on the pathogenesis in terms of organ crosstalk. Clin. Respir. J. 2020, 14, 595–604. [Google Scholar] [CrossRef] [PubMed]
- Unnikrishnan, D.; Jun, J.; Polotsky, V. Inflammation in sleep apnea: An update. Rev. Endocr. Metab. Disord. 2015, 16, 25–34. [Google Scholar] [CrossRef]
- Pillar, G.; Shehadeh, N. Abdominal Fat and Sleep Apnea: The chicken or the egg? Diabetes Care 2008, 31, S303–S309. [Google Scholar] [CrossRef] [PubMed]
- Rasche, K.; Keller, T.; Hader, C.; Leidag, M.; Prinz, C. Impact of Obstructive Sleep Apnoea on Type 2 Diabetes and Vice Versa. Eur. Endocrinol. 2010, 9, 107–109. [Google Scholar] [CrossRef]
- Tauman, R.; Gozal, D. Obesity and obstructive sleep apnea in children. Paediatr. Respir. Rev. 2006, 7, 247–259. [Google Scholar] [CrossRef] [PubMed]
- Naimark, A.; Cherniack, R.M. Compliance of the respiratory system and its components in health and obesity. J. Appl. Physiol. 1960, 15, 377–382. [Google Scholar] [CrossRef]
- Imayama, I.; Prasad, B. Role of Leptin in Obstructive Sleep Apnea. Ann. Am. Thorac. Soc. 2017, 14, 1607–1621. [Google Scholar] [CrossRef] [PubMed]
- Öztürk, L.; Unal, M.; Tamer, L.; Celikoglu, F. The Association of the Severity of Obstructive Sleep Apnea With Plasma Leptin Levels. Arch. Otolaryngol.-Head Neck Surg. 2003, 129, 538–540. [Google Scholar] [CrossRef] [PubMed]
- Blüher, M. Adipose Tissue Dysfunction in Obesity. Exp. Clin. Endocrinol. Diabetes 2009, 117, 241–250. [Google Scholar] [CrossRef]
- Bleau, C.; Karelis, A.D.; St-Pierre, D.H.; Lamontagne, L. Crosstalk between intestinal microbiota, adipose tissue and skeletal muscle as an early event in systemic low-grade inflammation and the development of obesity and diabetes. Diabetes/Metab. Res. Rev. 2015, 31, 545–561. [Google Scholar] [CrossRef] [PubMed]
- Xu, T.; Lin, Y.; Sun, S.; Zhang, Q. Changes in four plasma adipokines before and after sleep in OSAS patients. Clin. Respir. J. 2016, 11, 968–974. [Google Scholar] [CrossRef] [PubMed]
- Lavie, L. Obstructive sleep apnoea syndrome—An oxidative stress disorder. Sleep Med. Rev. 2003, 7, 35–51. [Google Scholar] [CrossRef] [PubMed]
- Manna, P.; Jain, S.K. Obesity, Oxidative Stress, Adipose Tissue Dysfunction, and the Associated Health Risks: Causes and Therapeutic Strategies. Metab. Syndr. Relat. Disord. 2015, 13, 423–444. [Google Scholar] [CrossRef] [PubMed]
- Eisele, H.-J.; Markart, P.; Schulz, R. Obstructive Sleep Apnea, Oxidative Stress, and Cardiovascular Disease: Evidence from Human Studies. Oxidative Med. Cell. Longev. 2015, 2015, 1–9. [Google Scholar] [CrossRef]
- Uygur, F.; Tanriverdi, H.; Can, M.; Ornek, T.; Erboy, F.; Altinsoy, B.; Atalay, F.; Damar, M.; Kokturk, F.; Tor, M. The Impact of Obstructive Sleep Apnoea and Nasal Continuous Positive Airway Pressure on Circulating Ischaemia-Modified Albumin Concentrations. Mediat. Inflamm. 2016, 2016, 1–7. [Google Scholar] [CrossRef][Green Version]
- Bhattacharjee, R.; Kim, J.; Kheirandish-Gozal, L.; Gozal, D. Obesity and obstructive sleep apnea syndrome in children: A tale of inflammatory cascades. Pediatr. Pulmonol. 2010, 46, 313–323. [Google Scholar] [CrossRef] [PubMed]
- Kurt, O.K.; Yildiz, N. The importance of laboratory parameters in patients with obstructive sleep apnea syndrome. Blood Coagul. Fibrinolysis 2013, 24, 371–374. [Google Scholar] [CrossRef]
- Akyol, S.; Çörtük, M.; Baykan, A.O.; Kiraz, K.; Börekçi, A.; Şeker, T.; Gür, M.; Çayli, M. Mean platelet volume is associated with disease severity in patients with obstructive sleep apnea syndrome. Clinics 2015, 70, 481–485. [Google Scholar] [CrossRef]
- Chang, W.-D.; Tseng, C.-H.; Tsou, Y.-A. Mean platelet volume levels in children with sleep-disordered breathing: A meta-analysis. BMC Pediatr. 2020, 20, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Ji, X.; Wang, Q.; Li, J.Z. New insight into inter-organ crosstalk contributing to the pathogenesis of non-alcoholic fatty liver disease (NAFLD). Protein Cell 2018, 9, 164–177. [Google Scholar] [CrossRef]
- Farré, N.; Farré, R.; Gozal, D. Sleep Apnea Morbidity. Chest 2018, 154, 754–759. [Google Scholar] [CrossRef] [PubMed]
- Budden, K.F.; Gellatly, S.L.; Wood, D.L.A.; Cooper, M.A.; Morrison, M.; Hugenholtz, P.; Hansbro, P.M. Emerging pathogenic links between microbiota and the gut–lung axis. Nat. Rev. Microbiol. 2017, 15, 55–63. [Google Scholar] [CrossRef]
- Anand, S.; Mande, S.S. Diet, Microbiota and Gut-Lung Connection. Front. Microbiol. 2018, 9, 2147. [Google Scholar] [CrossRef]
- Durgan, D.J.; Ganesh, B.P.; Cope, J.L.; Ajami, N.J.; Phillips, S.C.; Petrosino, J.F.; Hollister, E.B.; Bryan, R.M. Role of the Gut Microbiome in Obstructive Sleep Apnea–Induced Hypertension. Hypertension 2016, 67, 469–474. [Google Scholar] [CrossRef]
- Delzenne, N.M.; Neyrinck, A.M.; Bäckhed, F.; Cani, P. Targeting gut microbiota in obesity: Effects of prebiotics and probiotics. Nat. Rev. Endocrinol. 2011, 7, 639–646. [Google Scholar] [CrossRef]
- Dobrosielski, D.A.; Papandreou, C.; Patil, S.P.; Salas-Salvadó, J. Diet and exercise in the management of obstructive sleep apnoea and cardiovascular disease risk. Eur. Respir. Rev. 2017, 26, 160110. [Google Scholar] [CrossRef]
- Schwartz, A.R.; Patil, S.P.; Laffan, A.M.; Polotsky, V.; Schneider, H.; Smith, P.L. Obesity and Obstructive Sleep Apnea: Pathogenic Mechanisms and Therapeutic Approaches. Proc. Am. Thorac. Soc. 2008, 5, 185–192. [Google Scholar] [CrossRef]
- Kapur, V.K.; Auckley, D.H.; Chowdhuri, S.; Kuhlmann, D.C.; Mehra, R.; Ramar, K.; Harrod, C.G. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2017, 13, 479–504. [Google Scholar] [CrossRef]
- Gileles-Hillel, A.; Kheirandish-Gozal, L.; Gozal, A.G.-H.L.K.-G.D. Biological plausibility linking sleep apnoea and metabolic dysfunction. Nat. Rev. Endocrinol. 2016, 12, 290–298. [Google Scholar] [CrossRef]
- Shah, N.; Roux, F. The Relationship of Obesity and Obstructive Sleep Apnea. Clin. Chest Med. 2009, 30, 455–465. [Google Scholar] [CrossRef]
- Gulotta, G.; Iannella, G.; Vicini, C.; Polimeni, A.; Greco, A.; De Vincentiis, M.; Visconti, I.C.; Meccariello, G.; Cammaroto, G.; De Vito, A.; et al. Risk Factors for Obstructive Sleep Apnea Syndrome in Children: State of the Art. Int. J. Environ. Res. Public Health 2019, 16, 3235. [Google Scholar] [CrossRef] [PubMed]
- Andersen, I.G.; Holm, J.-C.; Homøe, P. Impact of weight-loss management on children and adolescents with obesity and obstructive sleep apnea. Int. J. Pediatr. Otorhinolaryngol. 2019, 123, 57–62. [Google Scholar] [CrossRef]
- Nogueira-De-Almeida, C.A.; Del Ciampo, L.A.; Ferraz, I.S.; Del Ciampo, I.R.; Contini, A.A.; Ued, F.D.V. COVID-19 and obesity in childhood and adolescence: A clinical review. J. Pediatr. 2020, 96, 546–558. [Google Scholar] [CrossRef]
| Obesity and Asthma |
|---|
Environmental factors:
Oxidative stress Immunological factors
|
| Obesity and OSAS |
|---|
Mechanical adiposity factors
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
di Palmo, E.; Filice, E.; Cavallo, A.; Caffarelli, C.; Maltoni, G.; Miniaci, A.; Ricci, G.; Pession, A. Childhood Obesity and Respiratory Diseases: Which Link? Children 2021, 8, 177. https://doi.org/10.3390/children8030177
di Palmo E, Filice E, Cavallo A, Caffarelli C, Maltoni G, Miniaci A, Ricci G, Pession A. Childhood Obesity and Respiratory Diseases: Which Link? Children. 2021; 8(3):177. https://doi.org/10.3390/children8030177
Chicago/Turabian Styledi Palmo, Emanuela, Emanuele Filice, Alessandra Cavallo, Carlo Caffarelli, Giulio Maltoni, Angela Miniaci, Giampaolo Ricci, and Andrea Pession. 2021. "Childhood Obesity and Respiratory Diseases: Which Link?" Children 8, no. 3: 177. https://doi.org/10.3390/children8030177
APA Styledi Palmo, E., Filice, E., Cavallo, A., Caffarelli, C., Maltoni, G., Miniaci, A., Ricci, G., & Pession, A. (2021). Childhood Obesity and Respiratory Diseases: Which Link? Children, 8(3), 177. https://doi.org/10.3390/children8030177