Abstract
Background: Eating disorders are more common among adolescents and young adults. An increase in the rates of these disorders has been reported during the last years. Meanwhile, vegetarianism is becoming more popular in these age groups. The purpose of the present paper is to evaluate the association between eating disorders and vegetarian diets in adolescents and young adults. Methods: Systematic review of related articles published in PubMed, PsycInfo and Google Scholar up to 30 May 2019. Results: A total of 20 studies (14,391 subjects) were deemed eligible for this systematic review. The majority of the studies reported significant correlations between vegetarianism and eating disorders. However, due to the cross-sectional design, a causal link between eating disorders and vegetarian status cannot be established. Conclusions: Vegetarianism seems to be associated with eating disorders. Longitudinal studies are needed to establish temporal patterns between vegetarianism and the emergence of disordered eating.
1. Introduction
A vegetarian diet excludes meat, seafood and products containing both, but may include eggs and dairy [1]. Vegan diet is an extreme express of vegetarianism, excluding all animal products, namely everything based on animal origin such as additive fats [2]. Lately, there is an increasing movement toward vegetarian diets in different population groups, including adolescents (11–21 years) and young adults (up to 24 years), either due to personal initiative, ethical reasons or social factors [3]. In the United States, it has been estimated that 32% of adolescents between 8 and 18 years declare to have at least one vegetarian meal per week, while 4% of this age group is reported to completely follow vegetarian diet [3]. Concerning adults (>18 years) in the United States, the relevant rates are smaller, as 3.3% of them are recorded as vegetarians, half of them being vegans [3].
Elimination of animal products from the daily diet could potentially affect health especially that of adolescents whose development has not been yet complete. Although there is a correlation between vegetarian diet and health-related benefits, for instance regarding the decreased risk of cardiovascular disease [4,5], there is a large controversy about the effects of vegan diet on mental health [6].
Eating disorders (anorexia nervosa, bulimia nervosa and Eating Disorder Not Otherwise Specified—SCID [7]) are usually associated with restricted diets and are more commonly observed in adolescents and young adults. Vegetarianism has been increasingly considered as a way of weight control, as the diet is based in reduced animal fats [7]. In cases of eating disorders, the disorder itself leads to exclusion or restriction of specific products and different confounders and causes should be examined. According to the available literature, 45 to 54% of adolescents and young adults with anorexia nervosa followed some form of a vegetarian diet, especially females [7,8]. Additionally, in some cases (about 6%), patients have reported that they were vegetarians several years prior to the onset of their eating disorder [7]. It has been suggested that, when subjects with a suspected or diagnosed eating disorder follow a vegetarian diet, health care professionals should worry that this behavior may be used as a socially acceptable way to legitimize food avoidance [7] and avoid certain eating situations [8].
In light of the above, the aim of this systematic review was to investigate the correlation between vegetarian and vegan diets and eating disorders in adolescents and young adults.
2. Materials and Methods
2.1. Literature Search Strategy
A systematic literature search was performed on 30 May 2019 in three different databases (PubMeD, PsycInfo and Google Scholar). For the search, various terms were combined, namely vegetarian OR vegan OR vegans OR veganism OR vegetarian OR vegetarianism OR semi-vegetarian OR flexitarian OR lacto-ovo-vegetarian OR lacto-vegetarian OR lactovegetarian OR ovo-vegetarian OR fruitarian OR flexitarian, with “adolescents” OR “teenagers” OR “young adults” OR puberty OR youth OR “young adult” OR “young adults” OR “young adulthood” and anorexia OR bulimia OR “eating disorder”. The reference lists of eligible papers and relevant reviews were also meticulously searched in order to include further studies reporting on vegan diet and eating disorders.
2.2. Inclusion Criteria
The eligibility criteria were based on the PICOS (Participants, Intervention, Comparison, Outcomes, Study design) acronym. Articles eligible to be included in this review were required to meet the following criteria:
- Studies had to report on adolescents or young adults (up to 30 years of age) who follow vegetarian or vegan diet. Studies could be purely based on adolescents and young adults or include a subgroup of young adults with admixture of older individuals. At any case, the results of these two subcategories of studies were presented separately.
- Studies had to provide data about the correlation between vegetarian/vegan diet and eating disorders.
- Any strategy to diagnose eating disorders was deemed eligible.
- Prospective cohorts/cross-sectional/case-control studies were included.
- The article was written in English language.
- There was no restriction in publication year.
2.3. Exclusion Criteria
Articles meeting the following criteria were excluded from the review:
- Case reports
- Review articles and medical hypotheses
- Animal studies
- Papers referring to subjects with low-meat consumption (i.e., not vegetarians).
- Studies not declaring age groups
All article abstracts were screened by authors working in pairs in a blinded fashion. Those found not complying with the inclusion criteria were removed and any controversies were dealt with consensus in a meeting, in which the abstracts were reviewed.
2.4. Quality Assessment of Included Studies
All studies were rated with the Newcastle–Ottawa scale, adapted for assessing the quality of non-randomized cross-sectional studies. This scale allocates a maximum of 10 stars evaluating selection (representativeness, sample size, nonrespondents and ascertainment of exposure), comparability and outcome (assessment, statistical test) [9].
2.5. Data Collection Process
Data were extracted from each study in a structured coding scheme using Excel and included type of study, population size, gender and age distribution, population type (exclusively adolescents or young adults or a mix of them), confounders, definitions of eating habits, definitions of eating disorders and bias assessment. Data were retrieved by authors in pairs and team consensus was ensured.
2.6. Compliance with Ethics Guidelines
This article is based on previously conducted studies. The study is performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [10].
3. Results
Study Characteristics
The literature search produced a total of 1271 results, after removal of duplicates; of them 1235 were deemed irrelevant from title and abstract, whereas 36 were evaluated in full-text. Among the latter, 16 were excluded due to various reasons and ultimately, a total of 20 studies (14.391 subjects) published between 1986 and 2019 were included in the present systematic review [7,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. The PRISMA flowchart describing the successive steps in the selection of studies is presented in Figure 1. The general characteristics of the studies are presented in Table 1. Table 1 also presents the summary findings of the quality assessment (risk of bias) for the included studies; in the majority, the quality of studies was rated as low.
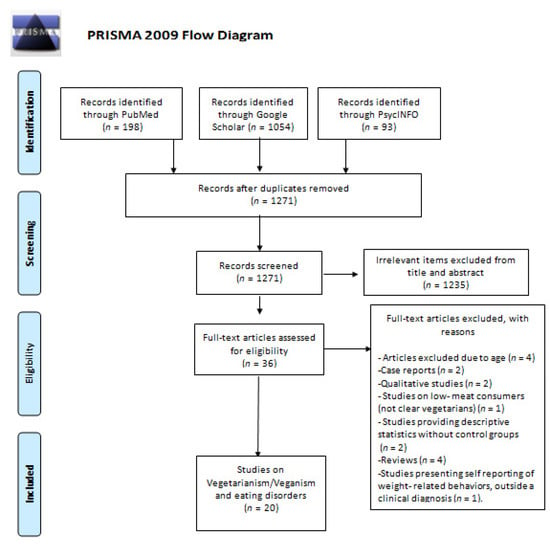
Figure 1.
Successive steps in the selection of studies—PRISMA Flow Diagram.

Table 1.
Characteristics of included studies. Upper panels present studies encompassing exclusively on adolescents and young adults; middle panels present studies on youth, but with admixture with older individuals; lower panels present studies on prognosis/features of eating disorders.
The majority of included studies reported a positive association between vegetarianism/veganism and eating disorders. Specifically, Bardone-Cone et al. observed that individuals with a history of eating disorder were more likely to have ever followed a vegetarian diet compared to healthy controls [7]; similarly, Zuromski et al. recorded a higher prevalence of vegetarianism amongst women with clinical diagnosis of eating pathology [16]. Likewise, in a questionnaire survey by McLean et al., female students with vegetarian dietary restraints were more likely to have a history of eating disorders [19]. In a representative community survey, Michalak et al. confirmed the association between vegetarianism and eating disorders [17]. Accordingly, a positive association between being a vegetarian and diagnosis [13] or indication (according to EAT-26 [12,15,20,21] and EAT-40 scores) [14] of an eating disorder has been reported by other researchers.
Barrack et al. observed that, despite a correlation in the univariate analysis, the association between vegetarian status and eating disorder examination scores did not persist at the multivariate analysis [18]. Notably, Timko et al. reported a trend linking semi-vegetarianism with highest levels of restraint [11].
On the other hand, a correlation between vegetarianism and eating disorders was not documented in a few studies [26,28,29], whereas an inverse association between veganism and pathological attitudes towards food was reported [27].
Regarding prognosis and features of eating disorders (lower panels of Table 1), Kadambari et al. [22] showed that vegetarian anorectics were more frequently abstainers, hyperactive, consumed large quantities of non-calorific fluid and presented higher fear of fatness versus non vegetarian anorectics. In a retrospective study, O’ Connor et al. found that, as a rule, the avoidance of red meat did not predate anorexia nervosa [23]. Hansson et al. discovered that vegetarianism was more frequently present in recovered or current patients with anorexia nervosa [24]. Interestingly, Yackobovitch-Gavan et al. showed that vegetarianism (past and present) correlated with non-remission of anorexia nervosa [25].
4. Discussion
The present systematic review is an effort to investigate the association between different types of vegetarian diet and eating disorders in adolescents and young adults. As the literature research revealed, there seems to be a correlation between vegetarianism and the presence of eating disorders [7,12,13,14,15,16,19,21] and particularly anorexia nervosa [22,23,24]. Especially for adolescents, vegetarianism and unhealthy and extreme behaviors on weight control are reported to be interconnected [13]. Females seem to be more prompt to such associations [16,17,19,20]. However, there were also studies reporting no correlation between eating disorders and vegetarianism [26,28,29].
Commenting on potential causal associations, numerous individuals with disordered eating habits and a history of vegetarianism report that the adoption of a vegetarian diet followed their disorder [7,8,17,23,30]. It seems therefore that, in a patient with an eating disorder and vegetarianism, there is a high likelihood that vegetarianism could represent a mode of restriction in eating habits, as a part of their eating disorder pathology. Perpetuation of pathology cannot be ruled out, in a vicious circle where restriction begets restriction. At any case, there is need for future prospective studies to shed light onto the aspect of temporality that is corollary for the establishment of any etiological associations.
Individuals with eating disorders might become vegetarians as a means to control weight, as a strategy of food avoidance, but also for non-weight reasons [7]. From an eating disorders perspective, subjects who are prompt to follow vegetarianism for mainly non-weight reasons (e.g., ethics, religion) could at first seem less alarming than subjects with weight-loss motives [13,18,19] and body shape worries [12], however bias in reporting the actual reasons is a concern. Specifically, in view of the stigma of eating disorders, the disclosed reason for following vegetarianism may sometimes be hard to identify in clinical practice. For a patient with an eating disorder, declaring to be a vegetarian for animal rights reasons would seem more socially acceptable and less uncomfortable than the explicit disclosure of weight loss as a motive. Social acceptability bias in this instance would denote that an eating disorder patient would purportedly prioritize animal rights/ethics when in reality the behavior could be driven by a desire to restrict.
The prevalence of reasons underlying choices of vegetarianism differ between studies. Klopp et al. [14] highlighted health/nutrition (37.5%) as the most common reason for vegetarianism, followed by weight control (18.8%) and animal ethics (14.6%). However, Bas et al. reported another context, with the most common reason being taste preferences (58.1%), followed by healthier diet (19.4%) and weight control only in 9.6% of the sample [12]. Other mechanisms have also been postulated, such as that the life experience of a mental health disorder may “sensitize” the patient towards the suffering of other beings and animals (thus eliciting vegetarianism or veganism), whereas presence of common variables underlying both vegetarianism and eating disorders (such as perfectionism, high levels of responsibility, social values) may provide another alternative explanation [17]. On the other hand, being vegetarian has been associated with positive qualities, including morality, empathy and being self-sacrificial for the greater good [31]. Concerning motivations, veganism is an entity distinct from vegetarianism, as it reflects a self-defining way of life, putting in practice ethical and moral beliefs that strongly oppose processes of treating animals in the food and animal products industry [29].
Regarding subgroups in the spectrum of semi-vegetarianism, vegetarianism and veganism, Timko et al. highlighted that semi-vegetarians had a trend towards a more restrained eating pattern [11]. Further studies are needed to differentiate between vegans, vegetarians, and semi-vegetarians.
In view of the association between vegetarianism and eating disorders, individuals who adopt a vegetarian diet should be closely examined regarding their general eating attitudes/behaviors by clinicians, to evaluate the presence of extreme weight control attitudes [13,18,19] and eating disorder chronicity [7,23,32].
The findings of the present systematic review can be inscribed into a wider perspective, regarding adverse aspects of vegetarianism in terms of mental health. A meta-analysis on 17.809 individuals, published in 2020, highlighted that vegan or vegetarian diets were associated with a higher risk of depression but with lower anxiety scores, although the synthesized studies were of low quality [33]. However, another meta-analysis, also published in 2020, indicated that there was no association between consumption of a vegetarian diet and depression or anxiety [34]. Such complex interplays between vegetarianism, eating disorders and depression would seem addressing in future studies. Eating pathology has been longitudinally associated with depression in a meta-analysis of 42 studies, that highlighted the need to identify factors that are etiological to the development of both conditions [35]. The debate regarding vegetarian diets and any effects upon mental health remains vivid and open.
Our results should be interpreted with some caution given the limitations of the synthesized studies. Firstly, most studies were of a cross-sectional design, thus cannot clarify if there is a causal relationship between vegetarianism and disorder eating. Secondly, quality ratings were low, as evidences by the Newcastle-Ottawa scale. The majority of studies were based on population-based samples, except for a few ones on clinical samples compared versus other groups [7,16,22,23,24,25]. Furthermore, a great variety of questionnaires was used. Other limitations include the lack of differentiation of eating disorder diagnoses, the scarcity of subgroup data about bulimia the small sample size in some studies, the variability in the definition of vegetarianism, and the lack of a validated measure for assessing aspects of vegetarianism or veganism. Although there was no limitation about the cultures on which studies were based, the fact that only studies in English were included in this systematic review may have actually limited synthesized evidence mainly into countries with a Western culture and lifestyle. There was paucity of data regarding subgroups of vegetarian diets, such as flexitarian, lacto-ovo-vegetarian, lacto-vegetarian, ovo-vegetarian, fruitarian and flexitarian diets that might exhibit distinct features.
5. Conclusions
In conclusion, this systematic review highlights a potential association between vegetarianism and eating disorders. Future research should focus on multi-center prospective studies in order to shed light on temporal patterns in the relationship between vegetarianism and disordered eating, although such studies would be practically demanding.
Author Contributions
Conceptualization, T.N.S. and A.T.; methodology, M.-E.C., A.L., C.-M.Y., T.P., T.N.S., A.T.; investigation, M.-E.C., A.L. and C.-M.Y.; writing—original draft preparation, M.-E.C., A.L., C.-M.Y. and E.P.; writing—review and editing, E.V., S.M., F.B., T.P., T.N.S., A.T.; visualization, E.V., S.M., F.B. and E.P.; supervision, A.T. and T.N.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
Data is contained within the article.
Acknowledgments
The authors would like to thank Georgios Koulouris, Maria Kallithraka-Moschochoritou, for their help in accessing PsycInfo database and during the initial reference management of items yielded by the search algorithm.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Melina, V.; Craig, W.; Levin, S. Position of the Academy of Nutrition and Dietetics: Vegetarian Diets. J. Acad. Nutr. Diet. 2016, 116, 1970–1980. [Google Scholar] [CrossRef]
- Appleby, P.N.; Key, T.J. The long-term health of vegetarians and vegans. Proc. Nutr. Soc. 2016, 75, 287–293. [Google Scholar] [CrossRef]
- Segovia-Siapco, G.; Burkholder-Cooley, N.; Haddad Tabrizi, S.; Sabate, J. Beyond Meat: A Comparison of the Dietary Intakes of Vegetarian and Non-vegetarian Adolescents. Front. Nutr. 2019, 6, 86. [Google Scholar] [CrossRef]
- Craig, W.J.; Mangels, A.R. American Dietetic Association. Position of the American Dietetic Association: Vegetarian diets. J. Am. Diet. Assoc. 2009, 109, 1266–1282. [Google Scholar]
- Key, T.J.; Fraser, G.E.; Thorogood, M.; Appleby, P.N.; Beral, V.; Reeves, G.; Burr, M.L.; Chang-Claude, J.; Frentzel-Beyme, R.; Kuzma, J.W.; et al. Mortality in vegetarians and nonvegetarians: Detailed findings from a collaborative analysis of 5 prospective studies. Am. J. Clin. Nutr. 1999, 70, 516S–524S. [Google Scholar] [CrossRef]
- Beezhold, B.; Radnitz, C.; Rinne, A.; DiMatteo, J. Vegans report less stress and anxiety than omnivores. Nutr. Neurosci. 2015, 18, 289–296. [Google Scholar] [CrossRef]
- Bardone-Cone, A.M.; Fitzsimmons-Craft, E.E.; Harney, M.B.; Maldonado, C.R.; Lawson, M.A.; Smith, R.; Robinson, D.P. The inter-relationships between vegetarianism and eating disorders among females. J. Acad. Nutr. Diet. 2012, 112, 1247–1252. [Google Scholar] [CrossRef]
- Gilbody, S.M.; Kirk, S.F.; Hill, A.J. Vegetarianism in young women: Another means of weight control? Int. J. Eat. Disord. 1999, 26, 87–90. [Google Scholar] [CrossRef]
- Modesti, P.A.; Reboldi, G.; Cappuccio, F.P.; Agyemang, C.; Remuzzi, G.; Rapi, S.; Perruolo, E.; Parati, G.; ESH Working Group on CV Risk in Low Resource Settings. Panethnic Differences in Blood Pressure in Europe: A Systematic Review and Meta-Analysis. PLoS ONE 2016, 25, e0147601. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Timko, C.A.; Hormes, J.M.; Chubski, J. Will the real vegetarian please stand up? An investigation of dietary restraint and eating disorder symptoms in vegetarians versus non-vegetarians. Appetite 2012, 58, 982–990. [Google Scholar] [CrossRef] [PubMed]
- Bas, M.; Karabudak, E.; Kiziltan, G. Vegetarianism and eating disorders: Association between eating attitudes and other psychological factors among Turkish adolescents. Appetite 2005, 44, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Perry, C.L.; McGuire, M.T.; Neumark-Sztainer, D.; Story, M. Characteristics of vegetarian adolescents in a multiethnic urban population. J. Adolesc. Health 2001, 29, 406–416. [Google Scholar] [CrossRef]
- Klopp, S.A.; Heiss, C.J.; Smith, H.S. Self-reported vegetarianism may be a marker for college women at risk for disordered eating. J. Am. Diet. Assoc. 2003, 103, 745–747. [Google Scholar] [CrossRef]
- Trautmann, J.; Rau, S.I.; Wilson, M.A.; Walters, C. Vegetarian students in their first year of college: Are they at risk for restrictive or disordered eating behaviors? Veg. Stud. 2008, 42, 2. [Google Scholar]
- Zuromski, K.L.; Witte, T.K.; Smith, A.R.; Goodwin, N.; Bodell, L.P.; Bartlett, M.; Siegfried, N. Increased prevalence of vegetarianism among women with eating pathology. Eat. Behav. 2015, 19, 24–27. [Google Scholar] [CrossRef]
- Michalak, J.; Zhang, X.C.; Jacobi, F. Vegetarian diet and mental disorders: Results from a representative community survey. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 67. [Google Scholar] [CrossRef]
- Barrack, M.T.; West, J.; Christopher, M.; Pham-Vera, A.M. Disordered Eating Among a Diverse Sample of First-Year College Students. J. Am. Coll. Nutr. 2019, 38, 141–148. [Google Scholar] [CrossRef]
- McLean, J.A.; Barr, S.I. Cognitive dietary restraint is associated with eating behaviors, lifestyle practices, personality characteristics and menstrual 79 irregularity in college women. Appetite 2003, 40, 185–192. [Google Scholar] [CrossRef]
- Fatima, W.; Ahmad, L.M. Prevalence of disordered eating attitudes among adolescent girls in Arar City, Kingdom of Saudi Arabia. Health Psychol. Res. 2018, 6, 7444. [Google Scholar] [CrossRef]
- Lindeman, M.; Stark, K.; Latvala, K. Vegetarianism and Eating-Disordered Thinking. Eat. Disord. 2000, 8, 157–165. [Google Scholar] [CrossRef]
- Kadambari, R.; Cowers, S.; Crisp, A. Some correlates of vegetarianism in anorexia nervosa. Int. J. Eat. Disord. 1986, 5, 539–544. [Google Scholar] [CrossRef]
- O’Connor, M.A.; Touyz, S.W.; Dunn, S.M.; Beumont, P.J. Vegetarianism in anorexia nervosa? A review of 116 consecutive cases. Med. J. Aust. 1987, 147, 540–542. [Google Scholar] [CrossRef] [PubMed]
- Hansson, L.M.; Bjorck, C.; Birgegard, A.; Clinton, D. How do eating disorder patients eat after treatment? Dietary habits and eating behaviour three years after entering treatment. Eat. Weight Disord. 2011, 16, e1–e8. [Google Scholar] [CrossRef] [PubMed]
- Yackobovitch-Gavan, M.; Golan, M.; Valevski, A.; Kreitler, S.; Bachar, E.; Lieblich, A.; Mitrani, E.; Weizman, A.; Stein, D. An integrative quantitative model of factors influencing the course of anorexia nervosa over time. Int. J. Eat. Disord. 2009, 42, 306–317. [Google Scholar] [CrossRef]
- Fatima, W.F.R.; Suhail, N. Subclinical eating disorders and association with vegetarianism in female students of Saudi Arabia: A cross-sectional stud. J. Nurs. Health Sci. 2018, 7, 2320. [Google Scholar]
- Heiss, S.; Coffino, J.A.; Hormes, J.M. Eating and health behaviors in vegans compared to omnivores: Dispelling common myths. Appetite 2017, 118, 129–135. [Google Scholar] [CrossRef]
- Fisak, B., Jr.; Peterson, R.D.; Tantleff-Dunn, S.; Molnar, J.M. Challenging previous conceptions of vegetarianism and eating disorders. Eat. Weight Disord. 2006, 11, 195–200. [Google Scholar] [CrossRef]
- Norwood, R.; Cruwys, T.; Chachay, V.S.; Sheffield, J. The psychological characteristics of people consuming vegetarian, vegan, paleo, gluten free and weight loss dietary patterns. Obes. Sci. Pract. 2019, 5, 148–158. [Google Scholar] [CrossRef]
- Sullivan, V.; Damani, S. Vegetarianism and eating disorders—Partners in crime? Eur. Eat. Disord. Rev. 2000, 8, 263–266. [Google Scholar] [CrossRef]
- Fox, N.; Ward, K.J. You are what you eat? Vegetarianism, health and identity. Soc. Sci. Med. 2008, 66, 2585–2595. [Google Scholar] [CrossRef] [PubMed]
- Bakan, R.; Birmingham, C.L.; Aeberhardt, L.; Goldner, E.M. Dietary zinc intake of vegetarian and nonvegetarian patients with anorexia nervosa. Int. J. Eat. Disord. 1993, 13, 229–233. [Google Scholar] [CrossRef]
- Iguacel, I.; Huybrechts, I.; Moreno, L.A.; Michels, N. Vegetarianism and veganism compared with mental health and cognitive outcomes: A systematic review and meta-analysis. Nutr. Rev. 2020, 1, nuaa030. [Google Scholar] [CrossRef] [PubMed]
- Askari, M.; Daneshzad, E.; Darooghegi Mofrad, M.; Bellissimo, N.; Suitor, K.; Azadbakht, L. Vegetarian diet and the risk of depression, anxiety, and stress symptoms: A systematic review and meta-analysis of observational studies. Crit. Rev. Food Sci. Nutr. 2020, 4, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Puccio, F.; Fuller-Tyszkiewicz, M.; Ong, D.; Krug, I. A systematic review and meta-analysis on the longitudinal relationship between eating pathology and depression. Int. J. Eat. Disord. 2016, 49, 439–454. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).