Fundamental Movement Skills and Accelerometer-Measured Physical Activity Levels during Early Childhood: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Study Selection Criteria
2.3. Search Strategy
2.4. Data Extraction and Synthesis
2.4.1. Locomotor, Object Control and PA Articles
2.4.2. Balance Articles
2.5. Study Quality Assessment
2.6. Analysis
3. Results
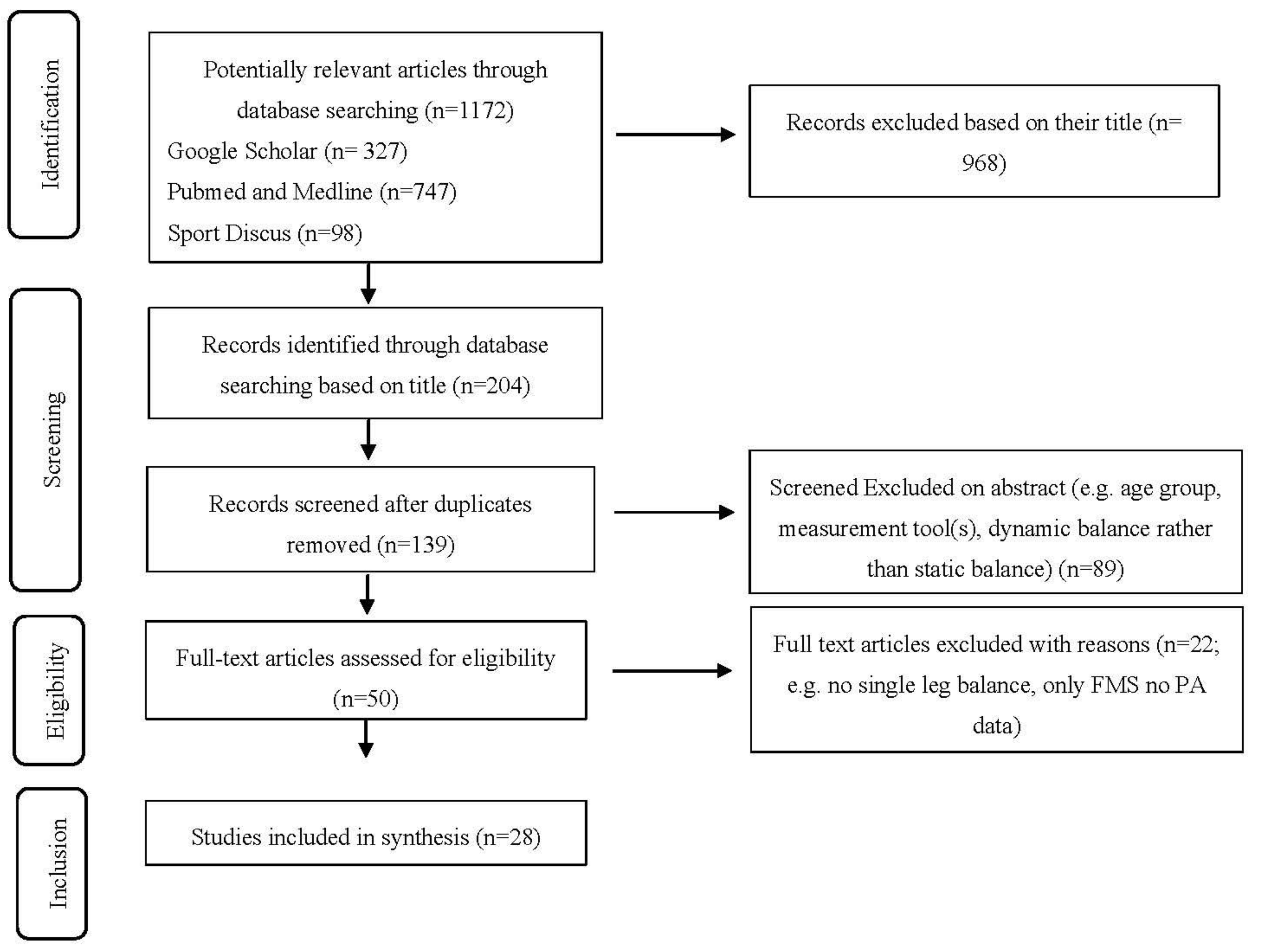
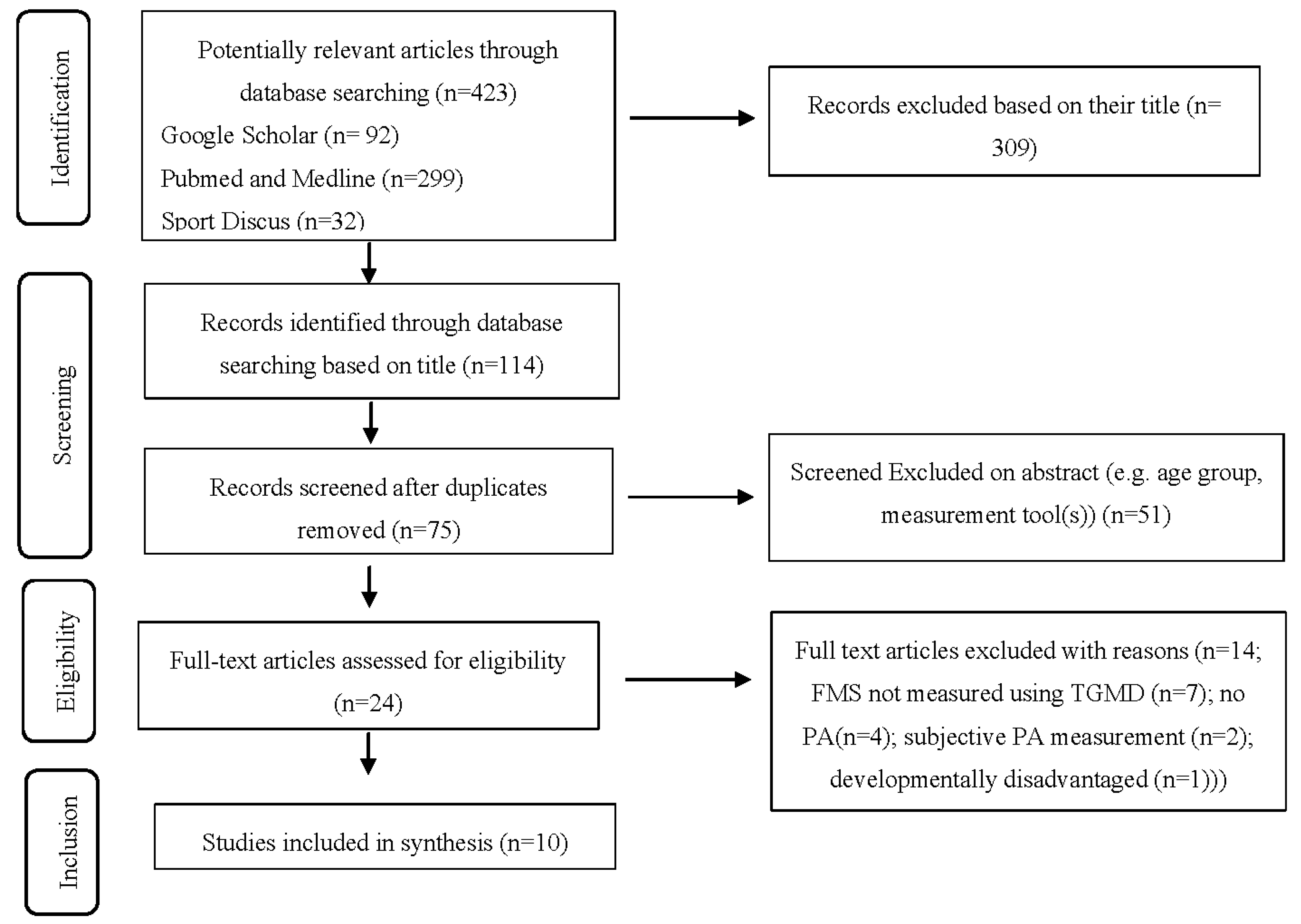
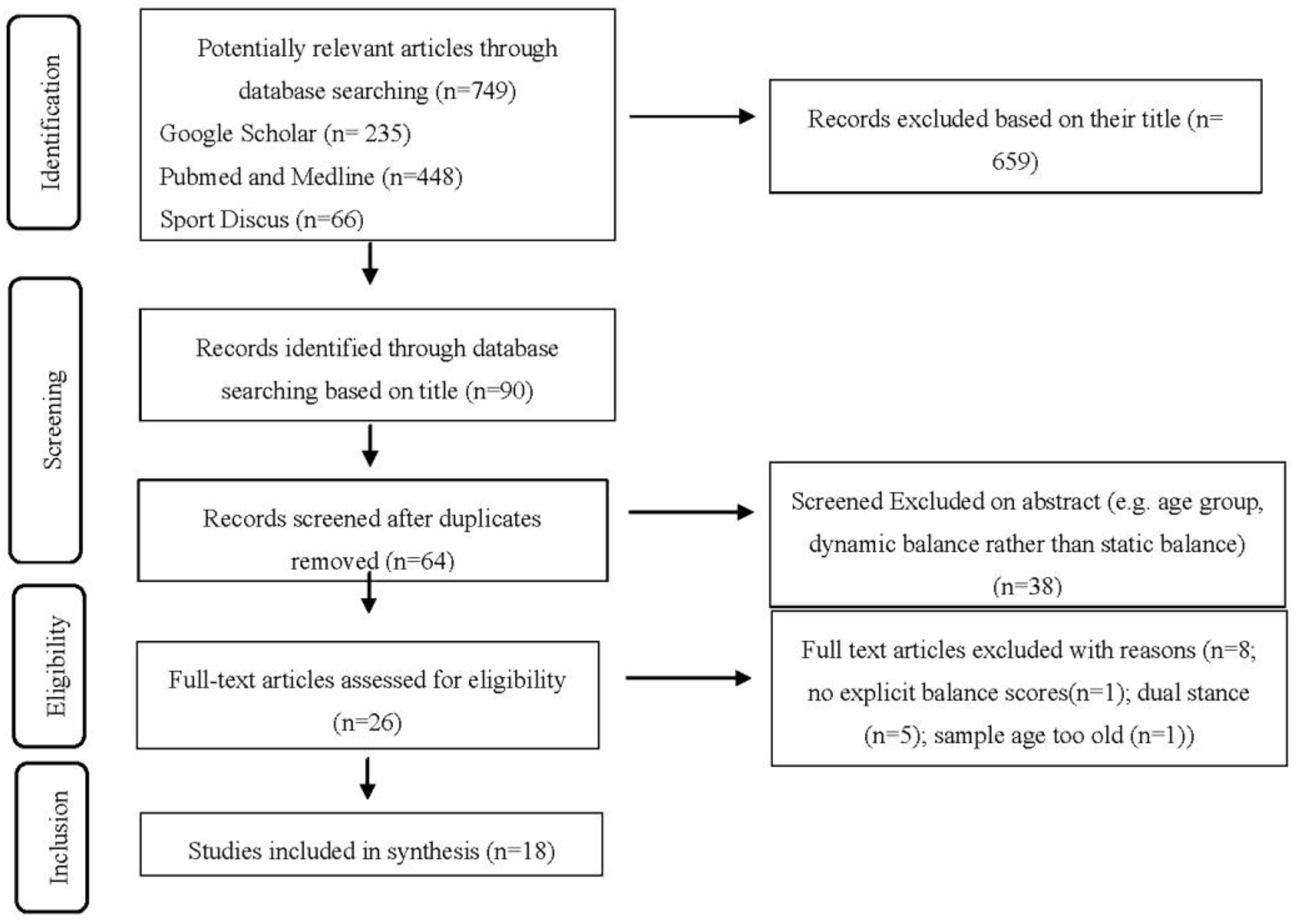
3.1. Study Selection
3.2. Origin and Participants
3.3. Study Quality Assessment
3.4. Locomotor and Object Control Proficiency
3.5. PA Levels
3.6. Balance Proficiency
| Author | Country | Setting | Sample Size | Mean Age (years) | Study Design | Outcome Measure(s) | Overall Findings—Relating to Baseline FMS and PA |
|---|---|---|---|---|---|---|---|
| Barnett et al. (2016) [44] | Australia | Home setting | 127 (59 boys, 68 girls) | 5 ± 0.1 | Observational cohort study | TGMD-2 (full), Accelerometry MVPA levels @ hip, ActiGraph GT1M |
|
| Cliff et al. (2009) [45] | Australia | Preschool | 46 (25 boys, 21 girls) | 4.3 ± 0.7 | Cross-sectional | TGMD-2 (full), Accelerometry MVPA levels @ hip, ActiGraph 7164 uniaxial |
|
| Duff et al. (2019) [47] | Ireland | Preschool | 141 (71 boys, 70 girls) | 3.9 ± 0.5 | Cross-sectional baseline | TGMD-2 and Victorian FMS manual- run, vertical jump, throw and catch Accelerometry ActiGraph GT3x and GT1m @ Hip (only preschool time) |
|
| Foweather et al. (2015) [50] | England | Preschool | 99 (52 boys, 47 girls) | 4.6 ± 0.5 | Cross-sectional observational | TGMD-2 scored with CMPS (total 138), Accelerometer ActiGraph GT3X@ waist |
|
| Jones et al. (2011) [48] | Australia | Preschool | 97 (no gender data) | 4.13 | Cluster randomised controlled trial | TGMD-2 (5 skills; Run, Jump, Hop Catch, Kick), MTI 7164 ActiGraph accelerometer @ right hip |
|
| Nilsen et al. (2020) [53] | Norway | Preschool | 376 (196 boys, 180 girls) | 4.7 ± 0.9 | Cross-sectional observational | TGMD-3 (partial), Accelerometer ActiGraph GT3X @ right hip |
|
| Palmer et al. (2018) [51] | USA | Preschool | 102 (63 boys, 39 girls) | 4.4 ± 0.43 | Randomised control trial | TGMD-3 (Full), Accelerometer ActiGraph GT3X@ waist |
|
| Roscoe et al. (2019) [49] | England | Preschool | 185 (99 boys, 86 girls) | 3.4 ± 0.5 | Cross-sectional observational | TGMD-2 (no underhand roll, added skip), Accelerometer- Geneactiv @wrist |
|
| Wasenius et al. (2018) [46] | Canada | Preschool | 215 (117 boys, 98 girls) | 3.65 ± 0.5 | Cluster randomised controlled trial | TGMD-2 (full), Accelerometer Actical, omnidirectional |
|
| Webster et al. (2019) [52] | USA | Childcare centres | 126 (58 boys, 68 girls) | 3.4 ± 0.5 | Observational cohort study | TGMD-3(full), Accelerometer ActiGraph GT3X @ right hip |
|
| Author | Country | Setting | Sample Size | Mean Age (years) | Study Design | Outcome Measure(s) for Single-Leg Balance | Overall Findings—Relating to Static Balance |
|---|---|---|---|---|---|---|---|
| Adamovic et al. (2015) [62] | Serbia | Testing at university | 54 (29 boys, 25 girls) | 5.24 ± 0.14 | Longitudinal observational | Standing on one foot for 20 s: score from 0–2. |
|
| Amelia et al. (2019) [63] | Indonesia | N/A | 30 (no gender data) | 5.5 | Non-equivalent control group | Standing on single leg (trial on each leg) for up to 30 s, measured in seconds. |
|
| An et al. (2009) [73] | Korea | Elementary school | 18 (no gender data available) | 5 | Cross-sectional observational | Single-limb standing test; 4 conditions; firm surface: eyes opened and closed, foam surface: eyes open and closed. Measured in seconds. |
|
| Cambier et al. (2001) [74] | Belgium | Primary School | 73 (no gender data available) | 4.5 | Cross-sectional observational | Unilateral stance test, 4 conditions; firm surface: eyes opened and closed, consecutively on the left then right foot, measured using centre of gravity sway velocity. |
|
| Condon and Cremin (2014) [75] | Ireland | Mainstream primary schools | 26 (11 boys, 15 girls) | 4.5 | Cross-sectional | Single-limb standing test; 3 conditions; firm surface: eyes opened and closed, foam surface: eyes open, measured in seconds. |
|
| De Oliveira et al. (2019) [64] | Australia | Primary School | 511 (257 boys, 254 girls) | 5.4 | Cluster randomised control trial | One-leg balance: MABC-2, measured in seconds. |
|
| Eshaghi et al. (2015) [72] | Iran | N/A | 20 (9 boys, 11 girls) | 6 | Cross-sectional observational | One-leg balance eyes open and closed on ground and repeated on balance beam from BOTMP-2, measured in seconds. |
|
| Fujinaga (2008) [65] | Japan | Kindergarten | 105 (51 boys, 54 girls) | 5 | Cross-sectional observational | One-leg standing test, measured by time, up to 120 s (seconds). |
|
| Guffey et al. (2016) [32] | USA | Hospital paediatric clinic and day care | 28 (no gender data) | 3.54 ± 0.84 | Cross-sectional observational | Paediatric Balance Scale component 9 (standing on one foot), scored 0–4. |
|
| Jiang et al. (2018) [34] | China | Public kindergarten | 60 (30 boys, 30 girls) | 4.5 | Cross-sectional observational | Tekscan foot pressure measurement system, one foot eyes open, held for 10 s. Measured by envelope area (area), path length (length), maximum displacement in anteroposterior (forward–back) and mediolateral direction (left–right) of the centre of pressure. |
|
| Jung et al. (2017) [66] | Korea | N/A | 11 (4 boys, 5 girls) | 5.8 ± 1.2 | Cross-sectional observational | One-leg standing test (OLST) non-dominant leg, measured in seconds. |
|
| Marin (2012) [67] | Romania | Kindergarten | 20 (9 boys, 11 girls) | 4.5 | Observational cohort study | The flamingo test for up to one minute, measured in seconds. |
|
| Moran et al. (2005) [68] | Brazil | Public school | 136 (62 boys, 74 girls) | 5 | Cross-sectional | Single-leg stance test for 10 s. |
|
| Latorre-Roman et al. (2017) [69] | Spain | Preschool | 3575 (1816 boys, 1759 girls) | 4.7 ± 0.93 | Cross-sectional observational | Stork balance stand test, up to one minute, measured in seconds. |
|
| Stankovic and Radenkovic (2012) [71] | Serbia | Preschool | 39 (26 boys, 13 girls) | 5.5 | Observational cohort study | Standing on one leg eyes open and standing on one leg eyes closed, measured in seconds. |
|
| Tan et al. (2019) [76] | Sinagpore | N/A | 23 (9 boys, 14 girls) | 6.32 ± 0.27 | Cross-sectional observational | One-leg balanc:- MABC-2, measured in seconds. Barefoot and shod conditions, up to 30 s tested. |
|
| Venetsanou and Kambas (2011) [35] | Greece | Public preschools | 283 (145 boys, 138 girls) | 5.15 ± 0.45 | Cross-sectional observational | BOTMP; standing on the preferred leg on the floor, standing on the preferred leg on a balance beam, standing on the preferred leg on a balance beam—eyes closed. Numerical point score. |
|
| Zumbrunn et al. (2012) [70] | USA | Test in laboratory | 15 (9 boys, 6 girls) | 6.17 ± 1.1 | Evaluation study | Stand on one foot for 5 s, COPsd A/P, COPsd M/L, COPsd Res, COPmax A/P, COPmax M/L, COParea, ARD, path velocity, COPvel A/P, COPvel M/L, ARF |
|
4. Discussion
4.1. Achievement
4.2. Measurement
4.3. Strengths and Limitations of the Current Study
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Section/Topic | # | Checklist Item | Reported on Page |
|---|---|---|---|
| TITLE | |||
| Title | 1 | Identify the report as a systematic review, meta-analysis, or both. | 1 |
| ABSTRACT | |||
| Structured summary | 2 | Provide a structured summary including, as applicable: background; objectives; data sources; study eligibility criteria, participants, and interventions; study appraisal and synthesis methods; results; limitations; conclusions and implications of key findings; systematic review registration number. | 1 |
| INTRODUCTION | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. | 1–3 |
| Objectives | 4 | Provide an explicit statement of questions being addressed with reference to participants, interventions, comparisons, outcomes, and study design (PICOS). | 3 |
| METHODS | |||
| Protocol and registration | 5 | Indicate if a review protocol exists, if and where it can be accessed (e.g., Web address), and, if available, provide registration information including registration number. | 3 |
| Eligibility criteria | 6 | Specify study characteristics (e.g., PICOS, length of follow-up) and report characteristics (e.g., years considered, language, publication status) used as criteria for eligibility, giving rationale. | 3–4 |
| Information sources | 7 | Describe all information sources (e.g., databases with dates of coverage, contact with study authors to identify additional studies) in the search and date last searched. | 4 |
| Search | 8 | Present full electronic search strategy for at least one database, including any limits used, such that it could be repeated. | 4 |
| Study selection | 9 | State the process for selecting studies (i.e., screening, eligibility, included in systematic review, and, if applicable, included in the meta-analysis). | 4, 6–8 figures |
| Data collection process | 10 | Describe method of data extraction from reports (e.g., piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators. | 4 |
| Data items | 11 | List and define all variables for which data were sought (e.g., PICOS, funding sources) and any assumptions and simplifications made. | 4–5 |
| Risk of bias in individual studies | 12 | Describe methods used for assessing risk of bias of individual studies (including specification of whether this was done at the study or outcome level), and how this information is to be used in any data synthesis. | 4 |
| Summary measures | 13 | State the principal summary measures (e.g., risk ratio, difference in means). | N/A |
| Synthesis of results | 14 | Describe the methods of handling data and combining results of studies, if done, including measures of consistency (e.g., I2) for each meta-analysis. | 5 |
| Risk of bias across studies | 15 | Specify any assessment of risk of bias that may affect the cumulative evidence (e.g., publication bias, selective reporting within studies). | N/A |
| Additional analyses | 16 | Describe methods of additional analyses (e.g., sensitivity or subgroup analyses, meta-regression), if done, indicating which were pre-specified. | N/A |
| RESULTS | |||
| Study selection | 17 | Give numbers of studies screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally with a flow diagram. | 9 |
| Study characteristics | 18 | For each study, present characteristics for which data were extracted (e.g., study size, PICOS, follow-up period) and provide the citations. | 9 |
| Risk of bias within studies | 19 | Present data on risk of bias of each study and, if available, any outcome level assessment (see item 12). | 9 |
| Results of individual studies | 20 | For all outcomes considered (benefits or harms), present, for each study: (a) simple summary data for each intervention group (b) effect estimates and confidence intervals, ideally with a forest plot. | 12–19 tables |
| Synthesis of results | 21 | Present results of each meta-analysis done, including confidence intervals and measures of consistency. | 9–11 |
| Risk of bias across studies | 22 | Present results of any assessment of risk of bias across studies (see Item 15). | N/A |
| Additional analysis | 23 | Give results of additional analyses, if done (e.g., sensitivity or subgroup analyses, meta-regression [see Item 16]). | N/A |
| DISCUSSION | |||
| Summary of evidence | 24 | Summarize the main findings including the strength of evidence for each main outcome; consider their relevance to key groups (e.g., healthcare providers, users, and policy makers). | 20–23 |
| Limitations | 25 | Discuss limitations at study and outcome level (e.g., risk of bias), and at review-level (e.g., incomplete retrieval of identified research, reporting bias). | 23–24 |
| Conclusions | 26 | Provide a general interpretation of the results in the context of other evidence, and implications for future research. | 24 |
| FUNDING | |||
| Funding | 27 | Describe sources of funding for the systematic review and other support (e.g., supply of data); role of funders for the systematic review. | N/A |
Appendix B
| Author and Year | Score |
|---|---|
| Barnett et al., 2016 [44] | 7 |
| Cliff et al., 2009 [45] | 7 |
| Duff et al., 2019 [47] | 7 |
| Foweather et al., 2015 [50] | 7 |
| Nilsen et al., 2020 [53] | 7 |
| Roscoe et al., 2019 [49] | 7 |
| Webster et al., 2019 [52] | 7 |
| Eshagi et al., 2015 [72] | 7 |
| Fujinaga 2008 [65] | 7 |
| Moran et al., 2005 [68] | 7 |
| Roman et al., 2017 [69] | 7 |
| Jones et al., 2011 [48] | 7 |
| De Oliveira et al., 2019 [64] | 7 |
| An et al., 2009 [73] | 6 |
| Jiang et al., 2018 [34] | 6 |
| Jung et al., 2017 [66] | 6 |
| Stankovic and Radenkovic 2012 [71] | 6 |
| Tan et al., 2019 [76] | 6 |
| Palmer et al., 2018 [51] | 6 |
| Marin 2012 [67] | 5 |
| Wasneius et al., 2017 [46] | 4 |
| Adamovic et al., 2016 [62] | 5 |
| Amelia et al., 2019 [63] | 5 |
| Cambier et al., 2001 [74] | 5 |
| Condon and Cremin 2014 [75] | 7 |
| Guffey et al., 2016 [32] | 7 |
| Vanetsanou and Kambas 2011 [35] | 7 |
| Zumbrunn et al., 2012 [70] | 6 |
References
- Carson, V.; Lee, E.-Y.; Hewitt, L.; Jennings, C.A.; Hunter, S.; Kuzik, N.; Stearns, J.A.; Unrau, S.P.; Poitras, V.J.; Gray, C.E.; et al. Systematic review of the relationships between physical activity and health indicators in the early years (0–4 years). BMC Public Health 2017, 17, 33–63. [Google Scholar] [CrossRef]
- Ebbeling, C.B.; Pawlak, D.B.; Ludwig, D.S. Childhood obesity: Public-health crisis, common sense cure. Lancet 2002, 360, 473–482. [Google Scholar] [CrossRef]
- Department for Health and Social Care. UK Chief Medical Officers’ Physical Activity Guidelines; 2019. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/832868/uk-chief-medical-officers-physical-activity-guidelines.pdf (accessed on 28 August 2020).
- Goldfield, G.S.; Harvey, A.; Grattan, K.P.; Adamo, K.B. Physical Activity Promotion in the Preschool Years: A Critical Period to Intervene. Int. J. Environ. Res. Public Health 2012, 9, 1326–1342. [Google Scholar] [CrossRef]
- The Department of Health. Australian 24-Hour Movement Guidelines for the Early Years (Birth to 5 years): An Integration of Physical Activity, Sedentary Behaviour, and Sleep; 2012. Available online: https://www1.health.gov.au/internet/main/publishing.nsf/Content/FCE78513DAC85E08CA257BF0001BAF95/$File/Birthto5years_24hrGuidelines_Brochure.pdf (accessed on 28 August 2020).
- World Health Organisation. Information Sheet: Global Recommendations on Physical Activity for Health 5–17 Years Old. 2011. Available online: https://www.who.int/dietphysicalactivity/publications/recommendations5_17years/en/ (accessed on 13 August 2020).
- Pate, R.R.; O’Neill, J.R.; Mitchell, J.A. Measurement of Physical Activity in Preschool Children. Med. Sci. Sports Exerc. 2010, 42, 508–512. [Google Scholar] [CrossRef] [PubMed]
- Loprinzi, P.D.; Cardinal, B.J. Measuring Children’s Physical Activity and Sedentary Behaviour. J. Exerc. Sci. Fit. 2011, 9, 15–23. [Google Scholar] [CrossRef]
- Penpraze, V.; Reilly, J.J.; MacLean, C.M.; Montgomery, C.; Kelly, L.A.; Paton, J.Y.; Aitchison, T.; Grant, S. Monitoring of Physical Activity in Young Children: How Much Is Enough? Pediatr. Exerc. Sci. 2006, 18, 483–491. [Google Scholar] [CrossRef]
- Bingham, D.D.; Costa, S.; Hinkley, T.; Shire, K.A.; Clemes, S.A.; Barberm, S.E. Physical Activity during the Early Years A Systematic Review of Correlates and Determinants. Am. J. Prev. Med. 2016, 51, 384–402. [Google Scholar] [CrossRef]
- Migueles, J.H.; Cadenas-Sanchez, C.; Tudor-Locke, C.; Löf, M.; Esteban-Cornejo, I.; Molina-Garcia, P.; Mora-Gonzalez, J.; Rodriguez-Ayllon, M.; Garcia-Marmol, E.; Ekelund, U.; et al. Comparability of published cut-points for the assessment of physical activity: Implications for data harmonization. Scand. J. Med. Sci. Sports 2018, 29, 566–574. [Google Scholar] [CrossRef]
- Gallahue, D.L.; Ozmun, J.C.; Goodway, J.D. Understanding Motor Development: Infants, Children, Adolescents, Adults, 7th ed.; McGraw-Hill: New York, NY, USA, 2011. [Google Scholar]
- Logan, S.W.; Ross, S.M.; Chee, K.; Stodden, D.F.; Robinson, L.E. Fundamental motor skills: A systematic review of terminology. J. Sports Sci. 2017, 36, 781–796. [Google Scholar] [CrossRef]
- D’Hondt, E.; Deforche, B.; De Bourdeaudhuij, I.; Lenoir, M. Relationship between Motor Skill and Body Mass Index in 5- to 10-Year-Old Children. Adapt. Phys. Act. Q. 2009, 26, 21–37. [Google Scholar] [CrossRef]
- Donath, L.; Faude, O.; Hagmann, S.; Roth, R.; Zahner, L. Fundamental movement skills in preschoolers: A randomized controlled trial targeting object control proficiency. Child Care Health Dev. 2015, 41, 1179–1187. [Google Scholar] [CrossRef] [PubMed]
- Gabbard, C.P. Life Long Motor Development, 7th ed.; Wolters Kluwer Health: Philadelphia, PA, USA, 2018. [Google Scholar]
- Verbecque, E.; da Costa, P.H.L.; Meyns, P.; Desloovere, K.; Vereeck, L.; Hallemans, A. Age-related changes in postural sway in pre-schoolers. Gait Posture 2016, 44, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Barnett, L.; Van Beurden, E.; Morgan, P.J.; Brooks, L.O.; Beard, J.R. Childhood Motor Skill Proficiency as a Predictor of Adolescent Physical Activity. J. Adolesc. Health 2009, 44, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Fisher, A.; Reilly, J.J.; Kelly, L.A.; Montgomery, C.; Williamson, A.; Paton, J.Y.; Grant, S. Fundamental Movement Skills and Habitual Physical Activity in Young Children. Med. Sci. Sports Exerc. 2005, 37, 684–688. [Google Scholar] [CrossRef]
- Ulrich, D.A. Test of Gross Motor Development, 2nd ed.; PRO-ED: Austin, TX, USA, 2000. [Google Scholar]
- Ulrich, D.A. Test of Gross Motor Development, 3nd ed.; PRO-ED: Austin, TX, USA, 2016. [Google Scholar]
- Klingberg, B.; Schranz, N.; Barnett, L.M.; Booth, V.; Ferrar, K. The feasibility of fundamental movement skill assessments for pre-school aged children. J. Sport Sci. 2019, 37, 378–386. [Google Scholar] [CrossRef]
- Eddy, L.H.; Bingham, D.D.; Crossley, K.L.; Shahid, N.F.; Ellingham-Khan, M.; Otteslev, A.; Figueredo, N.S.; Mon-Williams, M.; Hill, L.J.B. The validity and reliability of observational assessment tools available to measure fundamental movement skills in school-age children: A systematic review. PLoS ONE 2020, 15, e0237919. [Google Scholar] [CrossRef]
- Griffiths, A.; Toovey, R.; E Morgan, P.; Spittle, A.J. Psychometric properties of gross motor assessment tools for children: A systematic review. BMJ Open 2018, 8, e021734. [Google Scholar] [CrossRef]
- Robinson, L.E.; Stodden, D.F.; Barnett, L.M.; Lopes, V.P.; Logan, S.W.; Rodrigues, L.P.; D’Hondt, E. Motor Competence and its Effect on Positive Developmental Trajectories of Health. Sports Med. 2015, 45, 1273–1284. [Google Scholar] [CrossRef]
- Gallahue, D.L.; Donnelly, F.C. Developmental Physical Education for All Children, 4th ed.; Human Kinetics: Champaign, IL, USA, 2003. [Google Scholar]
- Xin, F.; Chen, S.; Clark, C.C.; Hong, J.-T.; Liu, Y.; Cai, Y. Relationship between Fundamental Movement Skills and Physical Activity in Preschool-aged Children: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 3566. [Google Scholar] [CrossRef]
- Henderson, S.E.; Sugden, D.A. Movement Assessment Battery for Children; The Psychological Corporation: Kent, WA, USA, 1992. [Google Scholar]
- Bruininks, R.H.; Bruininks, B.D. Bruininks-Oseretsky Test of Motor Proficiency: Manual; Pearson Assessments; AGS Publishing: Circle Pines, MN, USA, 2005. [Google Scholar]
- Franjoine, M.R.; Gunther, J.S.; Taylor, M.J. Pediatric Balance Scale: A Modified Version of the Berg Balance Scale for the School-Age Child with Mild to Moderate Motor Impairment. Pediatr. Phys. Ther. 2003, 15, 114–128. [Google Scholar] [CrossRef]
- Hardy, L.L.; King, L.; Farrell, L.; Macniven, R.; Howlett, S. Fundamental movement skills among Australian preschool children. J. Sci. Med. Sport 2010, 13, 503–508. [Google Scholar] [CrossRef]
- Guffey, K.; Regier, M.; Mancinelli, C.; Pergami, P. Gait parameters associated with balance in healthy 2–4 year-old children. Gait Posture 2016, 43, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Richardson, P.K.; Atwater, S.W.; Crowe, T.K.; Deitz, J.C. Performance of pre-schoolers on the paediatric clinical test of sensory interaction for balance. Am. J. Occup. Ther. 1992, 46, 793–800. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jiang, G.-P.; Jiao, X.-B.; Wu, S.-K.; Ji, Z.-Q.; Liu, W.-T.; Chen, X.; Wang, H.-H. Balance, Proprioception, and Gross Motor Development of Chinese Children Aged 3 to 6 Years. J. Mot. Behav. 2018, 50, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Venetsanou, F.; Kambas, A. The effects of age and gender on balance skills in preschool children. Facta Univ. Ser. Phys. Educ. Sport 2011, 9, 81–90. [Google Scholar]
- Chow, B.C.; Chan, L. Gross motor skills of Hong Kong preschool children. Asian J. Phys. Educ. Recreat. 2011, 17, 71–77. [Google Scholar]
- Krombholz, H. Physical Performance in Relation to Age, Sex, Birth Order, Social Class, and Sports Activities of Preschool Children. Percept. Mot. Ski. 2006, 102, 477–484. [Google Scholar] [CrossRef]
- Roncesvalles, M.N.C.; Woollacott, M.H.; Jensen, J.L. Development of Lower Extremity Kinetics for Balance Control in Infants and Young Children. J. Mot. Behav. 2001, 33, 180–192. [Google Scholar] [CrossRef]
- GOV.UK. School Starting Age; 2020. Available online: https://www.gov.uk/schools-admissions/school-starting-age (accessed on 28 August 2020).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Group PRISMA 2009 Flow Diagram. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Lonsdale, C.; Rosenkranz, R.R.; Peralta, L.R.; Bennie, A.; Fahey, P.; Lubans, D.R. A systematic review and meta-analysis of interventions designed to increase moderate-to-vigorous physical activity in school physical education lessons. Prev. Med. 2013, 56, 152–161. [Google Scholar] [CrossRef]
- Riley, J.J.; Hughes, A.; Janssen, X.; Martin, A.; Hesketh, K.; Livingstone, S.; Hill, C.; Kipping, R.; Draper, C.; Okely, A.; et al. Expert Working Group Working Paper, Under 5s. UK physical activity guidelines: Draft review and recommendations for the Under 5s; University of Bristol: Bristol, UK, 2018. [Google Scholar]
- Hong, Q.N.; Pluye, P.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; et al. Mixed Methods Appraisal Tool (MMAT), Version 2018; McGraw-Hill: New York, NY, USA, 2018. [Google Scholar]
- Barnett, L.M.; Salmon, J.; Hesketh, K.D. More active pre-school children have better motor competence at school starting age: An observational cohort study. BMC Public Health 2016, 16, 1068. [Google Scholar] [CrossRef] [PubMed]
- Cliff, D.P.; Okely, A.D.; Smith, L.M.; McKeen, K. Relationships between Fundamental Movement Skills and Objectively Measured Physical Activity in Preschool Children. Pediatr. Exerc. Sci. 2009, 21, 436–449. [Google Scholar] [CrossRef] [PubMed]
- Wasenius, N.S.; Grattan, K.P.; Harvey, A.L.; Naylor, P.-J.; Goldfield, G.S.; Adamo, K.B. The effect of a physical activity intervention on preschoolers’ fundamental motor skills—A cluster RCT. J. Sci. Med. Sport 2018, 21, 714–719. [Google Scholar] [CrossRef] [PubMed]
- Duff, C.; Issartel, J.; O’Brien, W.; Belton, S. Physical Activity and Fundamental Movement Skills of 3- to 5-Year-Old Children in Irish Preschool Services. J. Mot. Learn. Dev. 2019, 7, 354–373. [Google Scholar] [CrossRef]
- Jones, R.A.; Riethmuller, A.; Hesketh, K.; Trezise, J.; Batterham, M.; Okely, A.D. Promoting Fundamental Movement Skill Development and Physical Activity in Early Childhood Settings: A Cluster Randomized Controlled Trial. Pediatr. Exerc. Sci. 2011, 23, 600–615. [Google Scholar] [CrossRef]
- Roscoe, C.M.P.; James, R.S.; Duncan, M.J. Accelerometer-based physical activity levels, fundamental movement skills and weight status in British preschool children from a deprived area. Eur. J. Nucl. Med. Mol. Imaging 2019, 178, 1043–1052. [Google Scholar] [CrossRef]
- Foweather, L.; Knowles, Z.; Ridgers, N.D.; O’Dwyer, M.V.; Foulkes, J.D.; Stratton, G. Fundamental movement skills in relation to weekday and weekend physical activity in preschool children. J. Sci. Med. Sport 2015, 18, 691–696. [Google Scholar] [CrossRef]
- Palmer, K.K.; Chinn, K.M.; Robinson, L.E. The effect of the CHAMP intervention on fundamental motor skills and outdoor physical activity in pre-schoolers. J. Sport Health Sci. 2018, 8, 98–105. [Google Scholar] [CrossRef]
- Webster, E.K.; Martin, C.K.; Staiano, A.E. Fundamental motor skills, screen-time, and physical activity in pre-schoolers. J. Sport Health Sci. 2019, 8, 114–121. [Google Scholar] [CrossRef]
- Nilsen, A.K.O.; Anderssen, S.A.; Johannessen, K.; Aadland, K.N.; Ylvisaaker, E.; Loftesnes, J.M.; Aadland, E. Bi-directional prospective associations between objectively measured physical activity and fundamental motor skills in children: A two-year follow-up. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 1. [Google Scholar] [CrossRef]
- Roscoe, C.M.P.; James, R.S.; Duncan, M.J. Calibration of GENEActiv accelerometer wrist cut-points for the assessment of physical activity intensity of preschool aged children. Eur. J. Nucl. Med. Mol. Imaging 2017, 176, 1093–1098. [Google Scholar] [CrossRef] [PubMed]
- Evenson, K.R.; Catellier, D.J.; Gill, K.; Ondrak, K.S.; McMurray, R.G. Calibration of two objective measures of physical activity for children. J. Sports Sci. 2008, 26, 1557–1565. [Google Scholar] [CrossRef] [PubMed]
- Pate, R.R.; McIver, K.L.; Dowda, M.; Brown, W.H.; Addy, C. Directly Observed Physical Activity Levels in Preschool Children. J. Sch. Health 2008, 78, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Adolph, A.L.; Puyau, M.R.; Vohra, F.A.; Nicklas, T.A.; Zakeri, I.F.; Butte, N.F. Validation of Uniaxial and Triaxial Accelerometers for the Assessment of Physical Activity in Preschool Children. J. Phys. Act. Health 2012, 9, 944–953. [Google Scholar] [CrossRef] [PubMed]
- Sirard, J.R.; Trost, S.G.; Pfeiffer, K.A.; Dowda, M.; Pate, R.R. Calibration and Evaluation of an Objective Measure of Physical Activity in Preschool Children. J. Phys. Act. Health 2005, 2, 345–357. [Google Scholar] [CrossRef]
- Janssen, X.; Cliff, D.P.; Reilly, J.J.; Hinkley, T.; Jones, R.A.; Batterham, M.; Ekelund, U.; Brage, S.; Okely, A.D. Predictive Validity and Classification Accuracy of ActiGraph Energy Expenditure Equations and Cut-Points in Young Children. PLoS ONE 2013, 8, e79124. [Google Scholar] [CrossRef] [PubMed]
- Pate, R.R.; Almeida, M.J.; McIver, K.L.; Pfeiffer, K.A.; Dowda, M. Validation and Calibration of an Accelerometer in Preschool Children. Obesity 2006, 14, 2000–2006. [Google Scholar] [CrossRef]
- Reilly, J.J.; Coyle, J.; Kelly, L.; Burke, G.; Grant, S.; Paton, J.Y. An Objective Method for Measurement of Sedentary Behavior in 3- to 4-Year Olds. Obes. Res. 2003, 11, 1155–1158. [Google Scholar] [CrossRef]
- Adamović, T.; Kosanović, R.; Madić, D.; Ribarić-Jankes, K.; Sovilj, M.; Ðoković, S. Correlation between Balance Ability and Speech-Language Development in Children. Coll. Antropol. 2016, 39, 11–20. [Google Scholar]
- Amelia, H.; Hendratno, H.; Jannah, M. The Effect of Playing Bridge Beams on the Coordination and Balance of the Body of Early Childhood. Int. J. Educ. Vocat. Stud. 2019, 1, 72–74. [Google Scholar] [CrossRef]
- De Oliveira, J.; Rigoli, D.; Kane, R.; McLaren, S.; Goulardins, J.B.; Straker, L.L.; Dender, A.; Rooney, R.; Piek, J.P. Does ‘Animal Fun’ improve aiming and catching, and balance skills in young children? Res. Dev. Disabil. 2019, 84, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Fujinaga, H. Static standing balance as a component of motor fitness among the 5-year-old children. Int. J. Fit. 2008, 4, 67–74. [Google Scholar]
- Jung, H.-K.; Chung, E.; Lee, B.-H. A comparison of the balance and gait function between children with Down syndrome and typically developing children. J. Phys. Ther. Sci. 2017, 29, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Marin, F. Ascertaining Study on the Manifestation Level of the Ability to Balance at Children of 4–5 Years Rural Areas. Ovidius Univ. Ann. Ser. Phys. Educ. Sport/Sci. Mov. Health 2012, 12, 411–416. [Google Scholar]
- Moran, C.A.; De Carvalho, L.B.C.; Prado, L.B.; Prado, G.F.D. Sleep disorders and starting time to school impair balance in 5-year-old children. Arq. Neuro-Psiquiatria 2005, 63, 571–576. [Google Scholar] [CrossRef]
- Latorre-Román, P.Á.; López, D.M.; Fuentes, A.R.; García-Pinillos, F.M.; Fuentes, A.R.; García-Pinillos, F. Reference Values of Static Balance in Spanish Preschool Children. Percept. Mot. Ski. 2017, 124, 740–753. [Google Scholar] [CrossRef]
- Zumbrunn, T.; MacWilliams, B.A.; Johnson, B.A. Evaluation of a single leg stance balance test in children. Gait Posture 2011, 34, 174–177. [Google Scholar] [CrossRef]
- Stanković, M.; Radenković, O. The Status of Balance in Preschool Children Involved in Dance Program. RIK 2012, 40, 113–116. [Google Scholar]
- Eshaghi, Z.; Jafari, Z.; Jalaie, S. Static balance function in children with a history of preterm birth. Med. J. Islam. Repub. Iran 2015, 29, 310. [Google Scholar]
- An, M.-H.; Yi, C.; Jeon, H.-S.; Park, S.-Y. Age-related changes of single-limb standing balance in children with and without deafness. Int. J. Pediatr. Otorhinolaryngol. 2009, 73, 1539–1544. [Google Scholar] [CrossRef]
- Cambier, D.; Cools, A.; Danneels, L.; Witvrouw, E. Reference data for 4- and 5-year-old-children on the Balance Master: Values and clinical feasibility. Eur. J. Nucl. Med. Mol. Imaging 2001, 160, 317. [Google Scholar] [CrossRef] [PubMed]
- Condon, C.; Cremin, K. Static Balance Norms in Children. Physiother. Res. Int. 2014, 19, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.; Jernice, S. The balance control of young children under different shod conditions in a naturalistic environment. Gait Posture 2019, 68, 68–71. [Google Scholar] [CrossRef] [PubMed]
- Stodden, D.F.; Goodway, J.D.; Langendorfer, S.J.; Roberton, M.A.; Rudisill, M.E.; Garcia, C.; Garcia, L.E. A Developmental Perspective on the Role of Motor Skill Competence in Physical Activity: An Emergent Relationship. Quest 2008, 60, 290–306. [Google Scholar] [CrossRef]
- Jones, D.; Innerd, A.; Giles, E.L.; Azevedo, L.B. Association between fundamental motor skills and physical activity in the early years: A systematic review and meta-analysis. J. Sport Health Sci. 2020, 00, 1–11. [Google Scholar] [CrossRef]
- Roscoe, C.M.P.; James, R.S.; Duncan, M.J. Preschool staff and parents’ perceptions of preschool children’s physical activity and fundamental movement skills from an area of high deprivation: A qualitative study. Qual. Res. Sport Exerc. Health 2017, 9, 619–635. [Google Scholar] [CrossRef]
- McKenzie, T.L.; Sallis, J.F.; Broyles, S.L.; Zive, M.M.; Nader, P.R.; Berry, C.C.; Brennan, J.J. Childhood Movement Skills: Predictors of Physical Activity in Anglo American and Mexican American Adolescents? Res. Q. Exerc. Sport 2002, 73, 238–244. [Google Scholar] [CrossRef]
- Iivonen, S.; Sääkslahti, A. Preschool children’s fundamental motor skills: A review of significant determinants. Early Child Dev. Care 2014, 184, 1107–1126. [Google Scholar] [CrossRef]
- Duncan, M.J.; Roscoe, C.M.P.; Faghy, M.; Tallis, J.; Eyre, E.L.J. Estimating Physical Activity in Children Aged 8–11 Years Using Accelerometry: Contributions From Fundamental Movement Skills and Different Accelerometer Placements. Front. Physiol. 2019, 10, 242. [Google Scholar] [CrossRef]
- Canadian Society for Exercise Physiology. Canadian 24-Hour Movement Guidelines for the Early Years (0–4 Years): An Integration of Physical Activity, Sedentary Behaviour and Sleep. 2020. Available online: https://csepguidelines.ca/wp-content/themes/csep2017/pdf/PAR7972_24Hour_Guidelines_EY_En-4.pdf (accessed on 24 October 2020).
- Iacobucci, G. “Some exercise is good, more is better” say medical chiefs in new guidance. BMJ 2019, 366, l5470. [Google Scholar] [CrossRef]
- Gordon, E.S.; Tucker, P.; Burke, S.M.; Carron, A.V. Effectiveness of Physical Activity Interventions for Preschoolers: A Meta-Analysis. Res. Q. Exerc. Sport 2013, 84, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Hesketh, K.R.; McMinn, A.M.; Ekelund, U.; Sharp, S.J.; Collings, P.J.; Harvey, N.C.; Godfrey, K.M.; Inskip, H.; Cooper, C.; Van Sluijs, E. Objectively measured physical activity in four-year-old British children: A cross-sectional analysis of activity patterns segmented across the day. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 1. [Google Scholar] [CrossRef] [PubMed]
- Cools, W.; De Martelaer, K.; Samaey, C.; Andries, C. Fundamental movement skill performance of preschool children in relation to family context. J. Sports Sci. 2011, 29, 649–660. [Google Scholar] [CrossRef] [PubMed]
- Sport England. Active Lives Children and Young People Survey Academic Year 2018/19. 2019. Available online: https://sportengland-production-files.s3.eu-west-2.amazonaws.com/s3fs-public/2020-01/active-lives-children-survey-academic-year-18-19.pdf?cVMsdnpBoqROViY61iUjpQY6WcRyhtGs (accessed on 24 October 2020).
- Shape America. Shape of the Nation 2016. 2016. Available online: https://www.shapeamerica.org/uploads/pdfs/son/Shape-of-the-Nation-2016_web.pdf (accessed on 24 October 2020).
- Nguyen, S.; Häcker, A.-L.; Henderson, M.; Barnett, T.A.; Mathieu, M.; Pagani, L.S.; Bigras, J.-L. Physical Activity Programs with Post-Intervention Follow-Up in Children: A Comprehensive Review According to Categories of Intervention. Int. J. Environ. Res. Public Health 2016, 13, 664. [Google Scholar] [CrossRef]
- Department for Health and Social Care. UK Chief Medical Officers’ Physical Activity for Early Years; 2019. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/829882/1-physical-activity-for-early-years-birth-to-5.pdf (accessed on 26 October 2020).
- Schmalz, D.L.; Kerstetter, D.L. Girlie Girls and Manly Men: Chidren’s Stigma Consciousness of Gender in Sports and Physical Activities. J. Leis. Res. 2006, 38, 536–557. [Google Scholar] [CrossRef]
- Boyle, D.E.; Marshall, N.L.; Robeson, W. Gender at play—Fourth-grade girls and boys on the playground. Am. Behav. Sci. 2003, 46, 1326–1345. [Google Scholar] [CrossRef]
- Brown, T.; Lalor, A. The Movement Assessment Battery for Children—Second Edition (MABC-2): A Review and Critique. Phys. Occup. Ther. Pediatr. 2009, 29, 86–103. [Google Scholar] [CrossRef]
- Deitz, J.C.; Kartin, D.; Kopp, K. Review of the Bruininks-Oseretsky Test of Motor Proficiency, Second Edition (BOT-2). Phys. Occup. Ther. Pediatrics 2007, 27, 87–102. [Google Scholar] [CrossRef]
- Hulteen, R.M.; Barnett, L.M.; True, L.; Lander, N.; Cruz, B.D.P.; Lonsdale, C. Validity and reliability evidence for motor competence assessments in children and adolescents: A systematic review. J. Sports Sci. 2020, 38, 1717–1798. [Google Scholar] [CrossRef]
- The Australian Curriculum. Health and Physical Education. 2020. Available online: https://www.australiancurriculum.edu.au/f-10-curriculum/health-and-physical-education/ (accessed on 4 September 2020).
- SHAPE America. Guidelines for K-12 Online Physical Education. 2018. Available online: https://www.shapeamerica.org/uploads/pdfs/2020/guidelines/Online-PE-Guidance-Document.pdf (accessed on 4 September 2020).
- Department for Education. Physical Education Programmes of Study: Key Stages 1 and 2. National Curriculum in England; 2013. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/239040/PRIMARY_national_curriculum_-_Physical_education.pdf (accessed on 4 September 2020).
- Dobell, A.; Eyre, E.L.J.; Tallis, J.; Chinapaw, M.J.M.; Altenburg, T.M.; Duncan, M.J. Examining accelerometer validity for estimating physical activity in pre-schoolers during free-living activity. Scand. J. Med. Sci. Sports 2019, 29, 1618–1628. [Google Scholar] [CrossRef]
- Johansson, E.; Ekelund, U.; Nero, H.; Marcus, C.; Hagströmer, M. Calibration and cross-validation of a wrist-worn Actigraph in young preschoolers. Pediatr. Obes. 2014, 10, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Peach, D.; Van Hoomissen, J.; Callender, H.L. Exploring the ActiLife®filtration algorithm: Converting raw acceleration data to counts. Physiol. Meas. 2014, 35, 2359–2367. [Google Scholar] [CrossRef] [PubMed]
- Van Hees, V.T.; Thaler-Kall, K.; Wolf, K.-H.; Brønd, J.C.; Bonomi, A.; Schulze, M.; Vigl, M.; Morseth, B.; Hopstock, L.A.; Gorzelniak, L.; et al. Challenges and Opportunities for Harmonizing Research Methodology: Raw Accelerometry. Methods Inf. Med. 2016, 55, 525–532. [Google Scholar] [CrossRef] [PubMed]
- Karas, M.; Bai, J.; Strączkiewicz, M.; Harezlak, J.; Glynn, N.W.; Harris, T.; Zipunnikov, V.; Crainiceanu, C.; Urbanek, J.K. Accelerometry data in health research: Challenges and opportunities Review and examples. Stat. Biosci. 2018, 11, 210–237. [Google Scholar] [CrossRef]
- Konstabel, K.; Chopra, S.; Ojiambo, R.; Muñiz-Pardos, B.; Pitsiladfis, Y. Accelerometry-based Physical Activity Assessment for Children and Adolescents. In Instruments for Health Surveys in Children and Adolescents; Bammann, K., Lissner, L., Piegeot, I., Ahrens, W., Eds.; Springer: London, UK; Cham, Switzerland, 2019; pp. 135–173. [Google Scholar]
- Crotti, M.; Foweather, L.; Rudd, J.R.; Hurter, L.; Schwarz, S.; Boddy, L.M. Development of raw acceleration cut-points for wrist and hip accelerometers to assess sedentary behaviour and physical activity in 5–7-year-old children. J. Sports Sci. 2020, 38, 1036–1045. [Google Scholar] [CrossRef]
- Duncan, M.J.; Eyre, E.L.J.; Cox, V.; Roscoe, C.M.P.; Faghy, M.A.; Tallis, J.; Dobell, A. Cross-validation of Actigraph derived accelerometer cut-points for assessment of sedentary behaviour and physical activity in children aged 8–11 years. Acta Paediatr. 2020, 109, 1825–1830. [Google Scholar] [CrossRef]
- Hagenbuchner, M.; Cliff, D.P.; Trost, S.G.; Van Tuc, N.; Peoples, G.E. Prediction of activity type in preschool children using machine learning techniques. J. Sci. Med. Sport 2014, 18, 426–431. [Google Scholar] [CrossRef]
- Bakrania, K.; Yates, T.; Rowlands, A.V.; Esliger, D.W.; Bunnewell, S.; Sanders, J.; Davies, M.; Khunti, K.; Edwardson, C.L. Intensity Thresholds on Raw Acceleration Data: Euclidean Norm Minus One (ENMO) and Mean Amplitude Deviation (MAD) Approaches. PLoS ONE 2016, 11, e0164045. [Google Scholar] [CrossRef]
- Rowlands, A.V.; Rennie, K.; Kozarski, R.; Stanley, R.M.; Eston, R.; Parfitt, G.; Olds, T. Children’s Physical Activity Assessed with Wrist- and Hip-Worn Accelerometers. Med. Sci. Sports Exerc. 2014, 46, 2308–2316. [Google Scholar] [CrossRef]
- Fairclough, S.J.; Noonan, R.; Rowlands, A.V.; Van Hees, V.; Knowles, Z.; Boddy, L.M. Wear Compliance and Activity in Children Wearing Wrist- and Hip-Mounted Accelerometers. Med. Sci. Sports Exerc. 2016, 48, 245–253. [Google Scholar] [CrossRef]
- Oliver, M.; Schofield, G.M.; Kolt, G.S. Physical Activity in pre-schooler: Understanding Prevalence and Measurement Issues. Sports Med. 2007, 37, 1045–1070. [Google Scholar] [CrossRef] [PubMed]
- Gallahue, D.; Cleland-Donnelly, F. Developmental Physical Education for All Children, 5th ed.; Human Kinetics: Champaign, IL, USA, 2007. [Google Scholar]
- Newell, K.M. Motor Development in Children: Aspects of Coordination and Control. In Constraints on the Development of Coordination; Wade, M.G., Whiting, H.T.A., Eds.; Martinus Nijhoff: Dordrecht, The Netherlands, 1986; pp. 341–360. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dobell, A.; Pringle, A.; Faghy, M.A.; Roscoe, C.M.P. Fundamental Movement Skills and Accelerometer-Measured Physical Activity Levels during Early Childhood: A Systematic Review. Children 2020, 7, 224. https://doi.org/10.3390/children7110224
Dobell A, Pringle A, Faghy MA, Roscoe CMP. Fundamental Movement Skills and Accelerometer-Measured Physical Activity Levels during Early Childhood: A Systematic Review. Children. 2020; 7(11):224. https://doi.org/10.3390/children7110224
Chicago/Turabian StyleDobell, Alexandra, Andy Pringle, Mark A. Faghy, and Clare M. P. Roscoe. 2020. "Fundamental Movement Skills and Accelerometer-Measured Physical Activity Levels during Early Childhood: A Systematic Review" Children 7, no. 11: 224. https://doi.org/10.3390/children7110224
APA StyleDobell, A., Pringle, A., Faghy, M. A., & Roscoe, C. M. P. (2020). Fundamental Movement Skills and Accelerometer-Measured Physical Activity Levels during Early Childhood: A Systematic Review. Children, 7(11), 224. https://doi.org/10.3390/children7110224








