Bilateral Wilms Tumor: A Surgical Perspective
Abstract
1. Introduction
2. Biology and Genetics
2.1. Nephrogenic Rests and Nephroblastomatosis
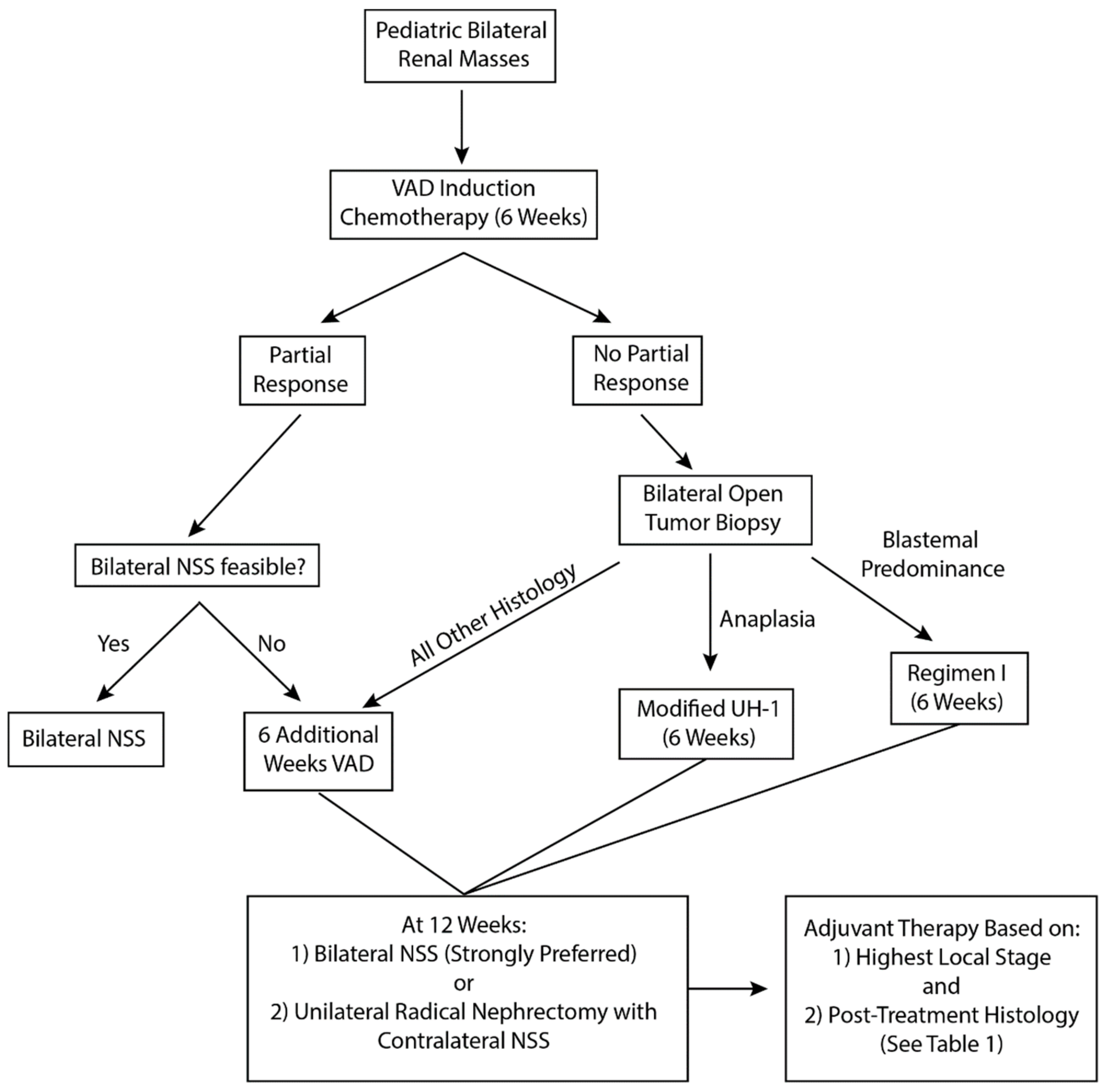
2.2. Diagnosis and Neoadjuvant Therapy
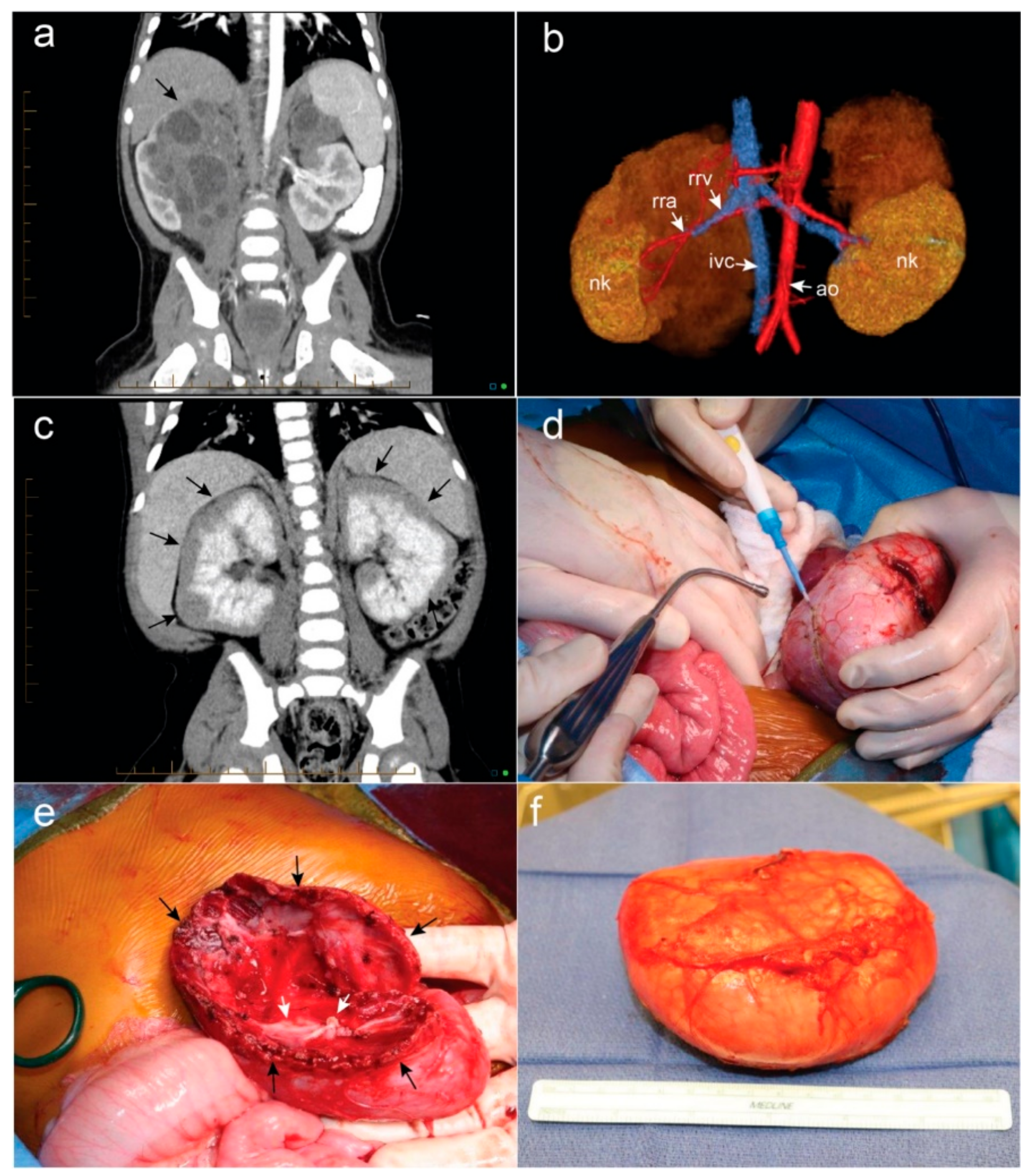
2.3. Surgical Management
2.4. Standardized Documentation of Nephron-Sparing Surgery
2.5. Difficult Surgical Scenarios
2.5.1. Positive Margins
2.5.2. Local Relapse
2.5.3. Diffuse Anaplasia
2.5.4. Repeat Nephron-Sparing Surgery
2.6. Long-Term Follow-Up/Renal Outcomes
2.7. Renal Transplantation for Bilateral Wilms Tumor
3. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Davidoff, A.M. Wilms tumor. Adv. Pediatr. 2012, 59, 247–267. [Google Scholar] [CrossRef] [PubMed]
- Charlton, J.; Irtan, S.; Bergeron, C.; Pritchard-Jones, K. Bilateral Wilms tumour: A review of clinical and molecular features. Expert Rev. Mol. Med. 2017, 19, e8. [Google Scholar] [CrossRef] [PubMed]
- Breslow, N.E.; Norris, R.; Norkool, P.A.; Kang, T.; Beckwith, J.B.; Perlman, E.J.; Ritchey, M.L.; Green, D.M.; Nichols, K.E.; National Wilms Tumor Study Group. Characteristics and outcomes of children with the wilms tumor-aniridia syndrome: A report from the national Wilms tumor study group. J. Clin. Oncol. 2003, 21, 4579–4585. [Google Scholar] [CrossRef] [PubMed]
- Pelletier, J.; Bruening, W.; Kashtan, C.E.; Mauer, S.M.; Manivel, J.C.; Striegel, J.E.; Houghton, D.C.; Junien, C.; Habib, R.; Fouser, L.; et al. Germline mutations in the Wilms’ tumor suppressor gene are associated with abnormal urogenital development in denys-drash syndrome. Cell 1991, 67, 437–447. [Google Scholar] [CrossRef]
- Porteus, M.H.; Narkool, P.; Neuberg, D.; Guthrie, K.; Breslow, N.; Green, D.M.; Diller, L. Characteristics and outcome of children with beckwith-wiedemann syndrome and Wilms’ tumor: A report from the national wilms tumor study group. J. Clin. Oncol. 2000, 18, 2026–2031. [Google Scholar] [CrossRef] [PubMed]
- Huff, V. Wilms tumor genetics. Am. J. Med. Genet. 1998, 79, 260–267. [Google Scholar] [CrossRef]
- Interiano, R.B.; Delos Santos, N.; Huang, S.; Srivastava, D.K.; Robison, L.L.; Hudson, M.M.; Green, D.M.; Davidoff, A.M. Renal function in survivors of nonsyndromic Wilms tumor treated with unilateral radical nephrectomy. Cancer 2015, 121, 2449–2456. [Google Scholar] [CrossRef] [PubMed]
- Cozzi, D.A.; Zani, A. Nephron-sparing surgery in children with primary renal tumor: Indications and results. Semin. Pediatr. Surg. 2006, 15, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Davidoff, A.M.; Giel, D.W.; Jones, D.P.; Jenkins, J.J.; Krasin, M.J.; Hoffer, F.A.; Williams, M.A.; Dome, J.S. The feasibility and outcome of nephron-sparing surgery for children with bilateral wilms tumor. The st jude children’s research hospital experience: 1999–2006. Cancer 2008, 112, 2060–2070. [Google Scholar] [CrossRef] [PubMed]
- Breslow, N.E.; Collins, A.J.; Ritchey, M.L.; Grigoriev, Y.A.; Peterson, S.M.; Green, D.M. End stage renal disease in patients with Wilms tumor: Results from the national wilms tumor study group and the united states renal data system. J. Urol. 2005, 174, 1972–1975. [Google Scholar] [CrossRef] [PubMed]
- Ehrlich, P.; Chi, Y.Y.; Chintagumpala, M.M.; Hoffer, F.A.; Perlman, E.J.; Kalapurakal, J.A.; Warwick, A.; Shamberger, R.C.; Khanna, G.; Hamilton, T.E.; et al. Results of the first prospective multi-institutional treatment study in children with bilateral Wilms tumor (aren0534): A report from the children’s oncology group. Ann. Surg. 2017, 266, 470–478. [Google Scholar] [CrossRef] [PubMed]
- Shamberger, R.C.; Haase, G.M.; Argani, P.; Perlman, E.J.; Cotton, C.A.; Takashima, J.; Green, D.M.; Ritchey, M.L. Bilateral Wilms’ tumors with progressive or nonresponsive disease. J. Pediatr. Surg. 2006, 41, 652–657. [Google Scholar] [CrossRef] [PubMed]
- Vujanic, G.M.; Apps, J.R.; Moroz, V.; Ceroni, F.; Williams, R.D.; Sebire, N.J.; Pritchard-Jones, K. Nephrogenic rests in Wilms tumors treated with preoperative chemotherapy: The UK SIOP Wilms tumor 2001 trial experience. Pediatr. Blood Cancer 2017, 64, e26547. [Google Scholar] [CrossRef] [PubMed]
- Pritchard-Jones, K.; Fleming, S.; Davidson, D.; Bickmore, W.; Porteous, D.; Gosden, C.; Bard, J.; Buckler, A.; Pelletier, J.; Housman, D.; et al. The candidate Wilms’ tumour gene is involved in genitourinary development. Nature 1990, 346, 194–197. [Google Scholar] [CrossRef] [PubMed]
- Compton, D.A.; Weil, M.M.; Jones, C.; Riccardi, V.M.; Strong, L.C.; Saunders, G.F. Long range physical map of the wilms’ tumor-aniridia region on human chromosome 11. Cell 1988, 55, 827–836. [Google Scholar] [CrossRef]
- Pelletier, J.; Bruening, W.; Li, F.P.; Haber, D.A.; Glaser, T.; Housman, D.E. WT1 mutations contribute to abnormal genital system-development and hereditary Wilms-tumor. Nature 1991, 353, 431–434. [Google Scholar] [CrossRef] [PubMed]
- Huff, V. Wilms’ tumours: About tumour suppressor genes, an oncogene and a chameleon gene. Nat. Rev. Cancer 2011, 11, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.; Fletcher, J.; McCahon, E.; Catchpoole, D.; Zhang, G.Y.; Wang, Y.M.; Algar, E.M.; Alexander, S.I. Bilateral Wilms tumor and early presentation in pediatric patients is associated with the truncation of the Wilms tumor 1 protein. J. Pediatr. 2013, 163, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Koesters, R.; Niggli, F.; von Knebel Doeberitz, M.; Stallmach, T. Nuclear accumulation of beta-catenin protein in Wilms’ tumours. J. Pathol. 2003, 199, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Maiti, S.; Alam, R.; Amos, C.I.; Huff, V. Frequent association of beta-catenin and WT1 mutations in Wilms tumors. Cancer Res. 2000, 60, 6288–6292. [Google Scholar] [PubMed]
- Royer-Pokora, B.; Beier, M.; Brandt, A.; Duhme, C.; Busch, M.; de Torres, C.; Royer, H.D.; Mora, J. Chemotherapy and terminal skeletal muscle differentiation in WT1-mutant Wilms tumors. Cancer Med. 2018, 7, 1359–1368. [Google Scholar] [CrossRef] [PubMed]
- Green, D.M.; Breslow, N.E.; Beckwith, J.B.; Norkool, P. Screening of children with hemihypertrophy, aniridia, and beckwith-wiedemann syndrome in patients with Wilms tumor: A report from the national wilms tumor study. Med. Pediatr. Oncol. 1993, 21, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Mussa, A.; Molinatto, C.; Baldassarre, G.; Riberi, E.; Russo, S.; Larizza, L.; Riccio, A.; Ferrero, G.B. Cancer risk in beckwith-wiedemann syndrome: A systematic review and meta-analysis outlining a novel (EPI)genotype specific histotype targeted screening protocol. J. Pediatr. 2016, 176, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Scott, R.H.; Douglas, J.; Baskcomb, L.; Huxter, N.; Barker, K.; Hanks, S.; Craft, A.; Gerrard, M.; Kohler, J.A.; Levitt, G.A.; et al. Constitutional 11p15 abnormalities, including heritable imprinting center mutations, cause nonsyndromic Wilms tumor. Nat. Genet. 2008, 40, 1329–1334. [Google Scholar] [CrossRef] [PubMed]
- Brioude, F.; Kalish, J.M.; Mussa, A.; Foster, A.C.; Bliek, J.; Ferrero, G.B.; Boonen, S.E.; Cole, T.; Baker, R.; Bertoletti, M.; et al. Expert consensus document: Clinical and molecular diagnosis, screening and management of beckwith-wiedemann syndrome: An international consensus statement. Nat. Rev. Endocrinol. 2018, 14, 229–249. [Google Scholar] [CrossRef] [PubMed]
- Lange, J.; Peterson, S.M.; Takashima, J.R.; Grigoriev, Y.; Ritchey, M.L.; Shamberger, R.C.; Beckwith, J.B.; Perlman, E.; Green, D.M.; Breslow, N.E. Risk factors for end stage renal disease in non-WT1-syndromic wilms tumor. J. Urol. 2011, 186, 378–386. [Google Scholar] [CrossRef] [PubMed]
- Stabouli, S.; Printza, N.; Dotis, J.; Matis, A.; Koliouskas, D.; Gombakis, N.; Papachristou, F. Perilobar nephroblastomatosis: Natural history and management. Case Rep. Pediatr. 2014, 2014, 756819. [Google Scholar] [CrossRef] [PubMed]
- Furtwangler, R.; Schmolze, M.; Graber, S.; Leuschner, I.; Amann, G.; Schenk, J.P.; Niggli, F.; Kager, L.; von Schweinitz, D.; Graf, N. Pretreatment for bilateral nephroblastomatosis is an independent risk factor for progressive disease in patients with stage V nephroblastoma. Klin. Padiatr. 2014, 226, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Perlman, E.J.; Faria, P.; Soares, A.; Hoffer, F.; Sredni, S.; Ritchey, M.; Shamberger, R.C.; Green, D.; Beckwith, J.B.; National Wilms Tumor Study Group. Hyperplastic perilobar nephroblastomatosis: Long-term survival of 52 patients. Pediatr. Blood Cancer 2006, 46, 203–221. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, T.E.; Ritchey, M.L.; Haase, G.M.; Argani, P.; Peterson, S.M.; Anderson, J.R.; Green, D.M.; Shamberger, R.C. The management of synchronous bilateral Wilms tumor: A report from the national wilms tumor study group. Ann. Surg. 2011, 253, 1004–1010. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, T.E.; Green, D.M.; Perlman, E.J.; Argani, P.; Grundy, P.; Ritchey, M.L.; Shamberger, R.C. Bilateral Wilms’ tumor with anaplasia: Lessons from the national Wilms’ tumor study. J. Pediatr. Surg. 2006, 41, 1641–1644. [Google Scholar] [CrossRef] [PubMed]
- Davidoff, A.M.; Interiano, R.B.; Wynn, L.; Delos Santos, N.; Dome, J.S.; Green, D.M.; Brennan, R.C.; McCarville, M.B.; Krasin, M.J.; Kieran, K.; et al. Overall survival and renal function of patients with synchronous bilateral Wilms tumor undergoing surgery at a single institution. Ann. Surg. 2015, 262, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Kieran, K.; Davidoff, A.M. Nephron-sparing surgery for bilateral Wilms tumor. Pediatr. Surg. Int. 2015, 31, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, J.; Szavay, P.; Seitz, G.; Handgretinger, R.; Schafer, J.F.; Warmann, S.W. Nephron sparing surgery for synchronous bilateral nephroblastoma involving the renal Hilus. J. Urol. 2011, 186, 1430–1436. [Google Scholar] [CrossRef] [PubMed]
- Giron-Vallejo, O.; Garcia-Calderon, D.; Ruiz-Pruneda, R.; Cabello-Laureano, R.; Domenech-Abellan, E.; Fuster-Soler, J.L.; Ruiz-Jimenez, J.I. Three-dimensional printed model of bilateral Wilms tumor: A useful tool for planning nephron sparing surgery. Pediatr. Blood Cancer 2018, 65, e26894. [Google Scholar] [CrossRef] [PubMed]
- Millar, A.J.; Davidson, A.; Rode, H.; Numanoglu, A.; Hartley, P.S.; Desai, F. Nephron-sparing surgery for bilateral Wilms’ tumours: A single-centre experience with 23 cases. Afr. J. Paediatr. Surg. 2011, 8, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Dome, J.S.; Graf, N.; Geller, J.I.; Fernandez, C.V.; Mullen, E.A.; Spreafico, F.; Van den Heuvel-Eibrink, M.; Pritchard-Jones, K. Advances in Wilms tumor treatment and biology: Progress through international collaboration. J. Clin. Oncol. 2015, 33, 2999–3007. [Google Scholar] [CrossRef] [PubMed]
- Godzinski, J.; Graf, N.; Audry, G. Current concepts in surgery for Wilms tumor—The risk and function-adapted strategy. Eur. J. Pediatr. Surg. 2014, 24, 457–460. [Google Scholar] [PubMed]
- Kieran, K.; Williams, M.A.; Dome, J.S.; McGregor, L.M.; Krasin, M.J.; Davidoff, A.M. Margin status and tumor recurrence after nephron-sparing surgery for bilateral Wilms tumor. J. Pediatr. Surg. 2013, 48, 1481–1485. [Google Scholar] [CrossRef] [PubMed]
- Shamberger, R.C.; Guthrie, K.A.; Ritchey, M.L.; Haase, G.M.; Takashima, J.; Beckwith, J.B.; D’Angio, G.J.; Green, D.M.; Breslow, N.E. Surgery-related factors and local recurrence of Wilms tumor in national Wilms tumor study 4. Ann. Surg. 1999, 229, 292–297. [Google Scholar] [CrossRef] [PubMed]
- Dome, J.S.; Liu, T.; Krasin, M.; Lott, L.; Shearer, P.; Daw, N.C.; Billups, C.A.; Wilimas, J.A. Improved survival for patients with recurrent wilms tumor: The experience at St. Jude children’s research hospital. J. Pediatr. Hematol. Oncol. 2002, 24, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Kieran, K.; Williams, M.A.; McGregor, L.M.; Dome, J.S.; Krasin, M.J.; Davidoff, A.M. Repeat nephron-sparing surgery for children with bilateral Wilms tumor. J. Pediatr. Surg. 2014, 49, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Ooms, A.H.; Gadd, S.; Gerhard, D.S.; Smith, M.A.; Guidry Auvil, J.M.; Meerzaman, D.; Chen, Q.R.; Hsu, C.H.; Yan, C.; Nguyen, C.; et al. Significance of TP53 mutation in wilms tumors with diffuse anaplasia: A report from the children’s oncology group. Clin. Cancer Res. 2016, 22, 5582–5591. [Google Scholar] [CrossRef] [PubMed]
- Interiano, R.B.; McCarville, M.B.; Santos, N.D.; Mao, S.; Wu, J.; Dome, J.S.; Kieran, K.; Williams, M.A.; Brennan, R.C.; Krasin, M.J.; et al. Comprehensive renal function evaluation in patients treated for synchronous bilateral Wilms tumor. J. Pediatr. Surg. 2017, 52, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Kist-van Holthe, J.E.; Ho, P.L.; Stablein, D.; Harmon, W.E.; Baum, M.A. Outcome of renal transplantation for Wilms’ tumor and denys-drash syndrome: A report of the north American pediatric renal transplant cooperative study. Pediatr. Transplant. 2005, 9, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Grigoriev, Y.; Lange, J.; Peterson, S.M.; Takashima, J.R.; Ritchey, M.L.; Ko, D.; Feusner, J.H.; Shamberger, R.C.; Green, D.M.; Breslow, N.E. Treatments and outcomes for end-stage renal disease following Wilms tumor. Pediatr. Nephrol. 2012, 27, 1325–1333. [Google Scholar] [CrossRef] [PubMed]
| Histology | Stage | Adjuvant Regimen |
|---|---|---|
| Completely necrotic | I–II | EE-4A |
| Intermediate risk | I | EE-4A |
| Intermediate risk | II | DD-4A |
| Intermediate risk | III–IV | DD-4A + XRT |
| Blastemal predominant | I | DD-4A |
| Diffuse anaplasia | I | DD-4A + XRT |
| Completely necrotic | III–IV | DD-4A + XRT |
| Focal anaplasia | I–III | DD-4A + XRT |
| Blastemal predominant | II | Regimen I |
| Blastemal predominant | III–IV | Regimen I + XRT |
| Focal anaplasia | IV | Revised UH-1 + XRT |
| Diffuse anaplasia | II–IV | Revised UH-1 + XRT |
| Reporting Component Format: NSS(X)-SRM(n)-PRM(n)-RRP(n%) | Description |
|---|---|
| 1. Surgical Technique | |
| a. NSS(A)—partial nephrectomy | Resection of the tumor with a rim of normal renal parenchyma |
| b. NSS(B)—enucleation (marginal resection) | Resection of the tumor without a rim of normal renal parenchyma |
| 2. Surgical Resection Margin (SRM) | Surgeon’s impression of resection margin |
| a. Intact pseudo-capsule = (0) | |
| b. Doubt intact pseudo-capsule = (1) | |
| c. Definite tumor breach = (2) | |
| 3. Pathological Resection Margin (PRM) | Microscopic resection margin on permanent pathology |
| a. Rim of normal renal parenchyma on resection margin (=0) | Exception for nephroblastomatosis |
| b. Intact pseudo-capsule along resection margin (=1) | |
| c. Tumor breach (=2) | |
| 4. Remaining Renal Parenchyma (RRP) = (n%) | Surgeon’s assessment of the percentage of remaining normal renal parenchyma |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murphy, A.J.; Davidoff, A.M. Bilateral Wilms Tumor: A Surgical Perspective. Children 2018, 5, 134. https://doi.org/10.3390/children5100134
Murphy AJ, Davidoff AM. Bilateral Wilms Tumor: A Surgical Perspective. Children. 2018; 5(10):134. https://doi.org/10.3390/children5100134
Chicago/Turabian StyleMurphy, Andrew J., and Andrew M. Davidoff. 2018. "Bilateral Wilms Tumor: A Surgical Perspective" Children 5, no. 10: 134. https://doi.org/10.3390/children5100134
APA StyleMurphy, A. J., & Davidoff, A. M. (2018). Bilateral Wilms Tumor: A Surgical Perspective. Children, 5(10), 134. https://doi.org/10.3390/children5100134





