Viral and Bacterial Etiology of Common Respiratory Infections in Children in Sub-Saharan Africa: A Systematic Review
Abstract
1. Introduction
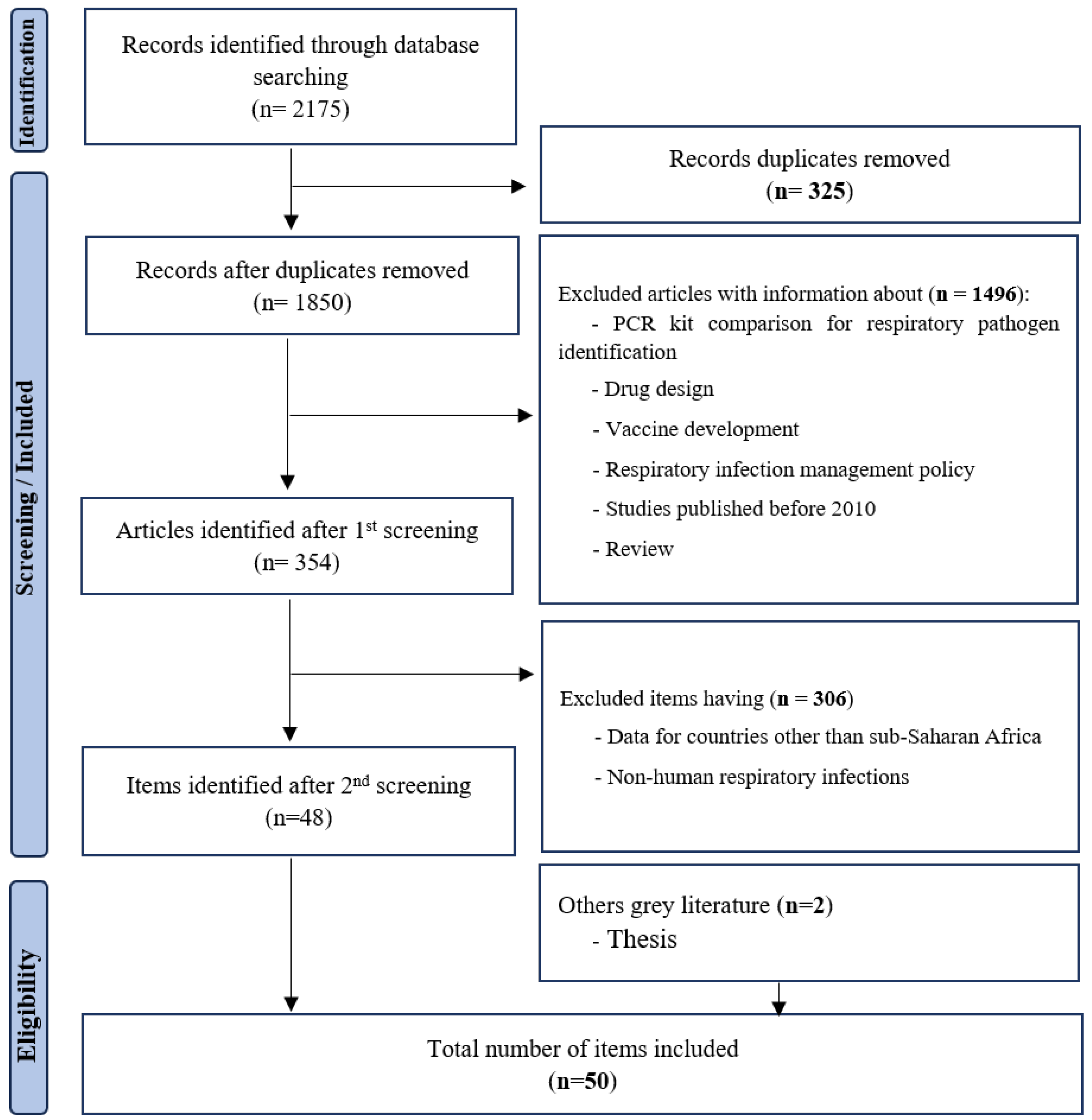
2. Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Inclusion Criteria
2.4. Exclusion Criteria
2.5. Data Extraction
2.6. Data Summary
3. Results
3.1. Literature Review
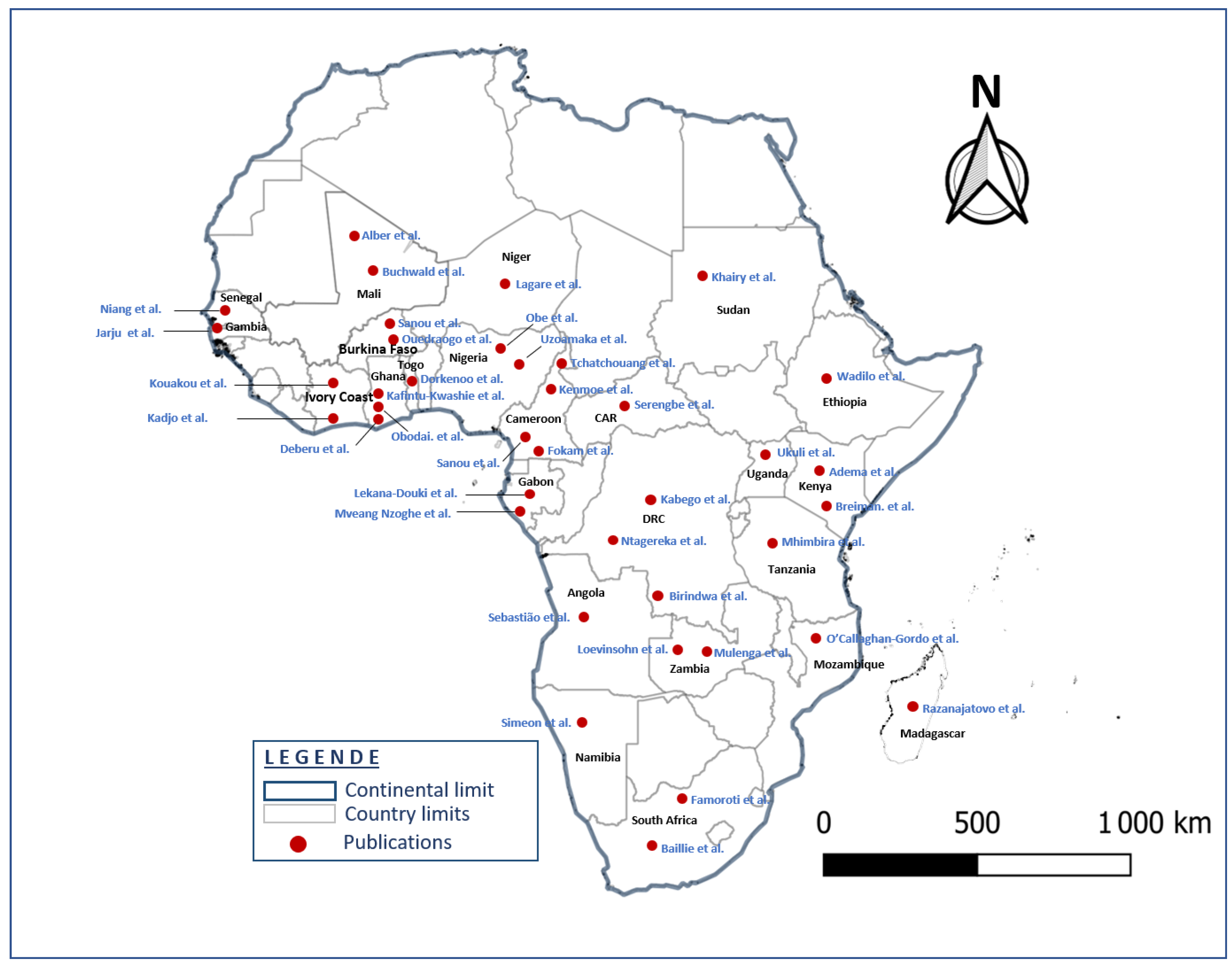
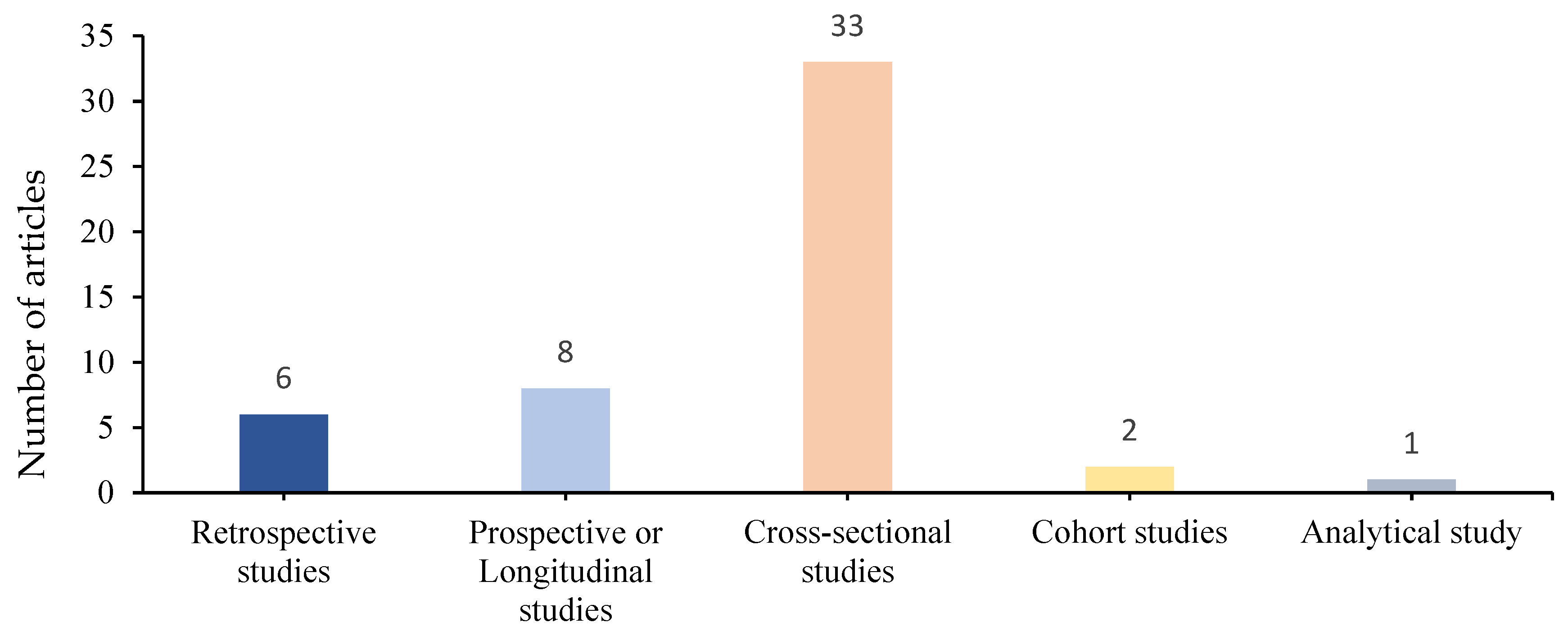
3.2. Features of Included Studies
3.3. Etiology of Pathogens Detected
4. Discussion
5. Conclusions
6. Study Limits
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Zhang, S.; Zhang, W.; Tang, Y.W. Molecular diagnosis of viral respiratory infections. Curr. Infect. Dis. Rep. 2011, 13, 149–158. [Google Scholar] [CrossRef]
- Obando-Pacheco, P.; Justicia-Grande, A.J.; Rivero-Calle, I.; Rodríguez-Tenreiro, C.; Sly, P.; Ramilo, O.; Mejías, A.; Baraldi, E.; Papadopoulos, N.; Nair, H.; et al. Respiratory syncytial virus seasonality: A global overview. J. Infect. Dis. 2018, 217, 1356–1364. [Google Scholar] [CrossRef] [PubMed]
- Jarju, S.; Greenhalgh, K.; Wathuo, M.; Banda, M.; Camara, B.; Mendy, S.; Sowe, G.; Dahaba, P.; Jammeh, L.; Bajinka, Y.; et al. Viral etiology, clinical features and antibiotic use in children <5 years of age in The Gambia presenting with influenza-like illness. Pediatr. Infect. Dis. J. 2020, 39, 925–930. [Google Scholar] [CrossRef] [PubMed]
- Bardsley, M.; Morbey, R.A.; Hughes, H.E.; Beck, C.R.; Watson, C.H.; Zhao, H.; Ellis, J.; Smith, G.; Elliot, A. Epidemiology of respiratory syncytial virus in children younger than 5 years in England during the COVID-19 pandemic, measured by laboratory, clinical, and syndromic surveillance: A retrospective observational study. Lancet Infect. Dis. 2023, 23, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Ouédraogo, S.; Traoré, B.; Nene Bi, Z.A.B.; Yonli, F.T.; Kima, D.; Bonané, P.; Congo, L.; Ouédraogo Traoré, R.; Yé, D.; Marguet, C.; et al. Viral etiology of respiratory tract infections in children at the pediatric hospital in Ouagadougou (Burkina Faso). PLoS ONE 2014, 9, e110435. [Google Scholar] [CrossRef]
- Sanou, A.M.; Cissé, A.; Millogo, T.; Sagna, T.; Tialla, D.; Williams, T.; Nzussouo, T.; Tarnagda, Z. Systematic review of articles on etiologies of acute respiratory infections in children aged less than five years in sub-Saharan Africa, 2000–2015. EC Microbiol. 2016, 6, 556–571. [Google Scholar]
- Sonego, M.; Pellegrin, M.C.; Becker, G.; Lazzerini, M. Risk factors for mortality from acute lower respiratory infections (ALRI) in children under five years of age in low and middle-income countries: A systematic review and meta-analysis of observational studies. PLoS ONE 2015, 10, e0116380. [Google Scholar] [CrossRef]
- Gadsby, N.J.; McHugh, M.P.; Russell, C.D.; Mark, H.; Morris, A.C.; Laurenson, I.F.; Hill, A.T.; Templeton, K.E. Development of two real-time multiplex PCR assays for the detection and quantification of eight key bacterial pathogens in lower respiratory tract infections. Clin. Microbiol. Infect. 2015, 21, 788.e1–788.e13. [Google Scholar] [CrossRef]
- Ayar, G.; Sahin, S.; Yazici, M.U.; Parlakay, A.Ö.; Tezer, H. RSV pneumonia in the pediatric intensive care unit. J. Pediatr. Inf. 2014, 8, 12–17. [Google Scholar] [CrossRef]
- Dube, F.S.; Kaba, M.; Robberts, F.J.; Ah Tow, L.; Lubbe, S.; Zar, H.J.; Nicol, M.P. Respiratory microbes present in the nasopharynx of children hospitalized with suspected pulmonary tuberculosis in Cape Town, South Africa. BMC Infect. Dis. 2016, 16, 597. [Google Scholar] [CrossRef]
- Deberu, O.; Nkrumah, B.; Sylverken, A.A.; Sambian, D.; Acheampong, G.; Amuasi, J.; Stebleson, A.; Agboyie, D.; Yenbaree, M.; Mensah, S.; et al. Common bacteria in sputum or gastric lavage of patients presenting with signs and symptoms of lower respiratory tract infections. Pan Afr. Med. J. 2021, 38, 383. [Google Scholar] [CrossRef] [PubMed]
- Yassine, H.M.; Sohail, M.U.; Younes, N.; Nasrallah, G.K. Systematic Review of the Respiratory Syncytial Virus (RSV) Prevalence, Genotype Distribution, and Seasonality in Children from the Middle East and North Africa (MENA) Region. Microorganisms 2020, 8, 713. [Google Scholar] [CrossRef] [PubMed]
- Haddad-Boubaker, S.; Mefteh, K.; Mejri, C.; Bouaffsoun, A.; El Moussi, A.; Boutiba, I.; Mnuf, K.; Slim, A.; Kechrid, A.; Smaoui, H. High genotypic diversity of Rhinoviruses obtained from Tunisian children with severe acute respiratory infection. J. Infect. Dev. Ctries. 2021, 15, 726–735. [Google Scholar] [CrossRef] [PubMed]
- Lagare, A.; Maïnassara, H.B.; Issaka, B.; Sidiki, A.; Tempia, S. Viral and bacterial etiology of severe acute respiratory illness among children <5 years of age without influenza in Niger. BMC Infect. Dis. 2015, 15, 515. [Google Scholar] [CrossRef]
- Gessner, B.D.; Shindo, N.; Briand, S. Seasonal influenza epidemiology in sub-Saharan Africa: A systematic review. Lancet Infect. Dis. 2011, 11, 223–235. [Google Scholar] [CrossRef]
- Wikipédia, L’encyclopédie Libre. Afrique. Available online: http://fr.wikipedia.org/w/index.php?title=Afrique&oldid=207325236 (accessed on 28 August 2023).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Tchatchouang, S.; Nzouankeu, A.; Kenmoe, S.; Ngando, L.; Penlap, V.; Fonkoua, M.C.; Pefura-Yone, E.; Njouom, R. Bacterial aetiologies of lower respiratory tract infections among adults in Yaoundé, Cameroon. BioMed Res. Int. 2019, 2019, 4834396. [Google Scholar] [CrossRef]
- Lagare, A.; Ousmane, S.; Dano, I.D.; Issaka, B.; Issa, I.; Mainassara, H.B.; Testa, J.; Tempia, S.; Mamadou, S. Molecular detection of respiratory pathogens among children aged younger than 5 years hospitalized with febrile acute respiratory infections: A prospective hospital-based observational study in Niamey, Niger. Health Sci. Rep. 2019, 2, e137. [Google Scholar] [CrossRef]
- Birindwa, A.M.; Kasereka, J.K.; Gonzales-Siles, L.; Geravandi, S.; Mwilo, M.; Tudiakwile, L.K.; Mwinja, N.; Muhigirwa, B.; Kashosi, T.; Manegabe, J.; et al. Bacteria and viruses in the upper respiratory tract of Congolese children with radiologically confirmed pneumonia. BMC Infect. Dis. 2021, 21, 837. [Google Scholar] [CrossRef]
- Mhimbira, F.; Hiza, H.; Mbuba, E.; Hella, J.; Kamwela, L.; Sasamalo, M.; Ticlla, T.; Said, K.; Mhalu, G.; Chiryamkubi, M.; et al. Prevalence and clinical significance of respiratory viruses and bacteria detected in tuberculosis patients compared to household contact controls in Tanzania: A cohort study. Clin. Microbiol. Infect. 2018, 25, 107.e1–107.e7. [Google Scholar] [CrossRef]
- Razanajatovo, N.H.; Guillebaud, J.; Harimanana, A.; Rajatonirina, S.; Ratsima, E.H.; Andrianirina, Z.Z.; Rakotoariniaina, H.; Andriatahina, T.; Orelle, A.; Ratovoson, R.; et al. Epidemiology of severe acute respiratory infections from hospital-based surveillance in Madagascar, November 2010 to July 2013. PLoS ONE 2018, 13, e0205124. [Google Scholar] [CrossRef]
- Lekana-Douki, S.E.; Mouinga-Ondémé, A.; Nkoghe, D.; Drosten, C.; Drexler, J.F.; Kazanji, M.; Leroy, E.M. Early introduction and delayed dissemination of pandemic influenza, Gabon. Emerg. Infect. Dis. 2013, 19, 644–647. [Google Scholar] [CrossRef]
- Lekana-Douki, S.E.; Nkoghe, D.; Drosten, C.; Ngoungou, E.B.; Drexler, J.F.; Leroy, E.M. Viral etiology and seasonality of influenza-like illness in Gabon, March 2010 to June 2011. BMC Infect. Dis. 2014, 14, 373. [Google Scholar] [CrossRef]
- Breiman, R.F.; Cosmas, L.; Njenga, M.K.; Williamson, J.; Mott, J.A.; Katz, M.A.; Erdman, D.; Schneider, E.; Oberste, M.S.; Neatherlin, J.; et al. Severe acute respiratory infection in children in a densely populated urban slum in Kenya, 2007–2011. BMC Infect. Dis. 2015, 15, 95. [Google Scholar] [CrossRef]
- Bobossi Serengbe, G.; Gody, J.C.; Fioboy, R.; Nakoune, E. Étiologie virale des infections respiratoires aiguës de l’enfant à Bangui. Arch. Pediatr. 2015, 22, 324–325. [Google Scholar] [CrossRef]
- Kenmoe, S.; Tchendjou, P.; Vernet, M.A.; Moyo-Tetang, S.; Mossus, T.; Njankouo-Ripa, M.; Kenne, A.; Beng, V.P.; Vabret, A.; Njouom, R. Viral etiology of severe acute respiratory infections in hospitalized children in Cameroon, 2011–2013. Influenza Other Respir. Viruses 2016, 10, 386–393. [Google Scholar] [CrossRef] [PubMed]
- Uzoamaka, M.; Ngozi, O.; Johnbull, O.S.; Martin, O. Bacterial etiology of lower respiratory tract infections and their antimicrobial susceptibility. Am. J. Med. Sci. 2017, 354, 471–475. [Google Scholar] [CrossRef] [PubMed]
- Niang, M.N.; Diop, N.S.; Fall, A.; Kiori, D.E.; Sarr, F.D.; Sy, S.; Goudiaby, D.; Barry, M.A.; Fall, M.; Dia, N. Respiratory viruses in patients with influenza-like illness in Senegal: Focus on human respiratory adenoviruses. PLoS ONE 2017, 12, e0174287. [Google Scholar] [CrossRef] [PubMed]
- Famoroti, T.; Sibanda, W.; Ndung’u, T. Prevalence and seasonality of common viral respiratory pathogens, including Cytomegalovirus in children, between 0–5 years of age in KwaZulu-Natal, an HIV endemic province in South Africa. BMC Pediatr. 2018, 18, 240. [Google Scholar] [CrossRef]
- Kadjo, H.A.; Adjogoua, E.; Dia, N.; Adagba, M.; Abdoulaye, O.; Daniel, S.; Kouakou, B.; Ngolo, D.C.; Coulibaly, D.; Ndahwouh, T.N.; et al. Detection of non-influenza viruses in acute respiratory infections in children under five-year-old in Cote d’Ivoire (January–December 2013). Afr. J. Infect. Dis. 2018, 12, 78–88. [Google Scholar] [CrossRef]
- Sanou, A.M.; Wandaogo, S.C.M.; Poda, A.; Tamini, L.; Kyere, A.E.; Sagna, T.; Ouedraogo, M.S.; Pauly, M.; Hübschen, J.M.; Muller, C.P.; et al. Epidemiology and molecular characterization of influenza viruses in Burkina Faso, sub-Saharan Africa. Influenza Other Respir. Viruses 2018, 12, 490–496. [Google Scholar] [CrossRef]
- Obodai, E.; Odoom, J.K.; Adiku, T.; Goka, B.; Wolff, T.; Biere, B.; Schweiger, B.; Reiche, J. The significance of human respiratory syncytial virus (HRSV) in children from Ghana with acute lower respiratory tract infection: A molecular epidemiological analysis, 2006 and 2013–2014. PLoS ONE 2018, 13, e0203788. [Google Scholar] [CrossRef]
- Lekana-Douki, S.E.; Behillil, S.; Enouf, V.; Leroy, E.M.; Berthet, N. Detection of human bocavirus-1 in both nasal and stool specimens from children under 5 years old with influenza-like illnesses or diarrhea in Gabon. BMC Res. Notes 2018, 11, 495. [Google Scholar] [CrossRef] [PubMed]
- Kabego, L.; Balol’Ebwami, S.; Kasengi, J.B.; Miyanga, S.; Bahati, Y.L.; Kambale, R.; de Beer, C. Human respiratory syncytial virus: Proportion, viral co-infections and risk factors for lower respiratory tract infections in children under 5 years of age at a general hospital in the Democratic Republic of Congo. J. Med. Microbiol. 2018, 67, 514–522. [Google Scholar] [CrossRef] [PubMed]
- Kenmoe, S.; Vernet, M.A.; Le Goff, J.; Penlap, V.B.; Vabret, A.; Njouom, R. Molecular characterization of human adenovirus associated with acute respiratory infections in Cameroon from 2011 to 2014. Virol. J. 2018, 15, 153. [Google Scholar] [CrossRef] [PubMed]
- Adema, I.W.; Kamau, E.; Nyiro, J.U.; Otieno, G.P.; Lewa, C.; Munywoki, P.K.; Nokes, D.J. Surveillance of respiratory viruses among children attending a primary school in rural coastal Kenya. Wellcome Open Res. 2020, 5, 63. [Google Scholar] [CrossRef]
- Buchwald, A.G.; Tamboura, B.; Tennant, S.M.; Haidara, F.C.; Coulibaly, F.; Doumbia, M.; Diallo, F.; Keita, A.M.; Sow, S.O.; Kotloff, K.L.; et al. Epidemiology, risk factors, and outcomes of respiratory syncytial virus infections in newborns in Bamako, Mali. Clin. Infect. Dis. 2020, 70, 59–66. [Google Scholar] [CrossRef]
- Obe, O.A.; Mutiu, B.W.; Amoo, A. Respiratory Syncytial Virus Infection among Children in Lagos, Nigeria. J. Clin. Immunol. Microbiol. 2021, 2, 1–11. [Google Scholar] [CrossRef]
- Kouakou, V.; Kadjo, H.; Oulo, N.A.; N’guessan, F.D.; N’Douba, A. Surveillance of Respiratory Syncytial Virus in Children Aged 0–5 years in Côte d’Ivoire. Am. J. BioScience 2021, 9, 185. [Google Scholar] [CrossRef]
- Kenmoe, S.; Sadeuh-Mba, S.A.; Vernet, M.A.; Beng, V.P.; Vabret, A.; Njouom, R. Molecular epidemiology of Enteroviruses and Rhinoviruses in patients with acute respiratory infections in Yaounde, Cameroon. Influenza Other Respir. Viruses 2021, 15, 641–650. [Google Scholar] [CrossRef]
- Ntagereka, P.B.; Basengere, R.A.; Baharanyi, T.C.; Kashosi, T.M.; Buhendwa, J.-P.C.; Bisimwa, P.B.; Kusinza, A.B.; Mugumaarhahama, Y.; Shukuru, D.W.; Patrick, S.B.; et al. Molecular evidence of coinfection with acute respiratory viruses and high proportion of SARS-CoV-2 among patients presenting flu-like illness in Bukavu city, Democratic Republic of Congo. Can. J. Infect. Dis. Med. Microbiol. 2022, 2022, 1553266. [Google Scholar] [CrossRef]
- Kafintu-Kwashie, A.A.; Nii-Trebi, N.I.; Obodai, E.; Neizer, M.; Adiku, T.K.; Odoom, J.K. Molecular epidemiological surveillance of viral agents of acute lower respiratory tract infections in children in Accra, Ghana. BMC Pediatr. 2022, 22, 364. [Google Scholar] [CrossRef]
- Kolawole, O.; Oguntoye, M.; Dam, T.; Chunara, R. Etiology of respiratory tract infections in the community and clinic in Ilorin, Nigeria. BMC Res. Notes 2017, 10, 712. [Google Scholar] [CrossRef]
- Ukuli, Q.A.; Erima, B.; Mubiru, A.; Atim, G.; Tugume, T.; Kibuuka, H.; Mworozi, E.; Ducatez, M.F.; Wabwire-Mangen, F.; Byarugaba, D.K. Molecular characterisation of human adenoviruses associated with respiratory infections in Uganda. BMC Infect. Dis. 2023, 23, 435. [Google Scholar] [CrossRef] [PubMed]
- Feikin, D.R.; Njenga, M.K.; Bigogo, G.; Aura, B.; Aol, G.; Audi, A.; Jagero, G.; Muluare, P.O.; Gikunju, S.; Nderitu, L.; et al. Etiology and Incidence of viral and bacterial acute respiratory illness among older children and adults in rural western Kenya, 2007–2010. PLoS ONE 2012, 7, e43656. [Google Scholar] [CrossRef] [PubMed]
- Fokam, J.; Takou, D.; Nka, A.D.; Ka’e, A.C.; Yagai, B.; Chenwi, C.A.; Semengue, E.N.J.; Beloumou, G.A.; Ndjeyep, S.C.D.; Abba, A.; et al. Epidemiological, virological and clinical features of SARS-CoV-2 among individuals during the first wave in Cameroon: Baseline analysis for the EDCTP PERFECT-Study RIA2020EF-3000. J. Public Health Afr. 2022, 13, 2142. [Google Scholar] [CrossRef] [PubMed]
- Dorkenoo, A.M.; Gbeasor-Komlanvi, F.A.; Gbada, K.; Zida-Compaore, W.I.C.; Teou, D.; Konu, Y.R.; Lack, F.; Sadio, A.J.; Tchankoni, M.K.; Dagnra, A.C.; et al. Prevalence of malaria and COVID-19 in febrile patients in Lomé, Togo in 2020. Acta Parasitol. 2022, 67, 1335–1342. [Google Scholar] [CrossRef] [PubMed]
- Alber, D.; Haidara, F.C.; Luoma, J.; Adubra, L.; Ashorn, P.; Ashorn, U.; Badji, H.; Cloutman-Green, E.; Diallo, F.; Ihamuotila, R.; et al. SARS-CoV-2 infection and antibody seroprevalence in routine surveillance patients, healthcare workers and general population in Kita region, Mali: An observational study 2020–2021. BMJ Open 2022, 12, e060367. [Google Scholar] [CrossRef]
- Khairy, A.; Elhussein, N.; Elbadri, O.; Mohamed, S.; Malik, E.M. Epidemiology of COVID-19 among Children and Adolescents in Sudan 2020–2021. Epidemiologia 2023, 4, 247–254. [Google Scholar] [CrossRef]
- Mulenga, L.B.; Hines, J.Z.; Fwoloshi, S.; Chirwa, L.; Siwingwa, M.; Yingst, S.; Wolkon, A.; Barradas, D.T.; Favaloro, J.; Zulu, J.E.; et al. Prevalence of SARS-CoV-2 in six districts in Zambia in July, 2020: A cross-sectional cluster sample survey. Lancet Glob. Health 2021, 9, e773–e781. [Google Scholar] [CrossRef]
- Wadilo, F.; Feleke, A.; Gebre, M.; Mihret, W.; Seyoum, T.; Melaku, K.; Howe, R.; Mulu, A.; Mihret, A. Viral etiologies of lower respiratory tract infections in children <5 years of age in Addis Ababa, Ethiopia: A prospective case–control study. Virol. J. 2023, 20, 163. [Google Scholar]
- Baillie, V.L.; Moore, D.P.; Mathunjwa, A.; Baggett, H.C.; Brooks, A.; Feikin, D.R.; Hammitt, L.L.; Howie, S.R.; Knoll, M.D.; Kotloff, K.L.; et al. Epidemiology of the rhinovirus (RV) in African and Southeast Asian children: A case-control pneumonia etiology study. Viruses 2021, 13, 1249. [Google Scholar] [CrossRef]
- Simusika, P.; Bateman, A.C.; Theo, A.; Kwenda, G.; Mfula, C.; Chentulo, E.; Monze, M. Identification of viral and bacterial pathogens from hospitalized children with severe acute respiratory illness in Lusaka, Zambia, 2011–2012: A cross-sectional study. BMC Infect. Dis. 2015, 15, 52. [Google Scholar] [CrossRef] [PubMed]
- Loevinsohn, G.; Hardick, J.; Sinywimaanzi, P.; Fenstermacher, K.Z.J.; Shaw-Saliba, K.; Monze, M.; Gaydos, C.A.; Rothman, R.E.; Pekosz, A.; Thuma, P.E.; et al. Respiratory pathogen diversity and co-infections in rural Zambia. Int. J. Infect. Dis. 2021, 102, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Yugbaré, S.O.O.; Ouédraogo, R.; Nenebi, A.; Traoré, B.; Congo, L.; Yonli, F.; Kima, D.; Bonané, P.; Yé, D.; Plantier, J.C.; et al. Infections à virus respiratoire syncytial (VRS) au CHU pédiatrique Charles de Gaulle de Ouagadougou, Burkina Faso. Bull. Soc. Pathol. Exot. 2016, 109, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Kenmoe, S. Prévalence et Diversité Génétique des Virus Respiratoires au Cameroun. 2017. Available online: http://www.theses.fr/2017NORMC417/document (accessed on 9 September 2025).
- Sanou, A.M. Epidemiology and Molecular Characterization of Viruses and Bacteria Detected in Acute Respiratory Infections in Children under Five in Burkina Faso. Master’s Thesis, Université Nazi BONI, Bobo-Dioulasso, Burkina Faso, 2018. Available online: https://bibliovirtuelle.u-naziboni.bf/biblio/opac_css/docnume/UFR-SJPEG/IDR-2018-SAN-EPI.pdf (accessed on 13 December 2017).
- O’Callaghan-Gordo, C.; Bassat, Q.; Morais, L.; Díez-Padrisa, N.; Machevo, S.; Nhampossa, T.; Nhalungo, D.; Sanz, S.; Quintó, L.; Alonso, P.L.; et al. Etiology and epidemiology of viral pneumonia among hospitalized children in rural Mozambique: A malaria endemic area with high prevalence of human immunodeficiency virus. Pediatr. Infect. Dis. J. 2011, 30, 39–44. [Google Scholar] [CrossRef]
- Jones, A.H.; Ampofo, W.; Akuffo, R.; Doman, B.; Duplessis, C.; Amankwa, J.A.; Sarpong, C.; Sagoe, K.; Agbenohevi, P.; Puplampu, N.; et al. Sentinel surveillance for influenza among severe acute respiratory infection and acute febrile illness inpatients at three hospitals in Ghana. Influenza Other Respir. Viruses 2016, 10, 367–374. [Google Scholar] [CrossRef]
- Simeon, P.; Godman, B.; Kalemeera, F. Antibiotics’ susceptibility patterns of bacterial isolates causing lower respiratory tract infections in ICU patients at referral hospitals in Namibia. Hosp. Pract. 2021, 49, 356–363. [Google Scholar] [CrossRef]
- Nzoghe, A.M.; Padzys, G.S.; Siawaya, A.C.M.; Yattara, M.K.; Leboueny, M.; Houechenou, R.M.A.; Bongho, E.C.; Mba-Mezemze, C.; Ndjindji, O.M.; Biteghe-Bi-Essone, J.C.; et al. Dynamic and features of SARS-CoV-2 infection in Gabon. Sci. Rep. 2021, 11, 9672. [Google Scholar]
- Sebastião, C.S.; Parimbelli, P.; Mendes, M.; Sacomboio, E.; Morais, J.; de Vasconcelos, J.N.; Brito, M. Prevalence and Risk Factors of SARS-CoV-2 Infection among Parturients and Newborns from Luanda, Angola. Pathogens 2021, 10, 1494. [Google Scholar] [CrossRef]
- Anjorin, A.A.; Abioye, A.I.; Asowata, O.E.; Soipe, A.; Kazeem, M.I.; Adesanya, I.O.; Raji, M.A.; Adesanya, M.; Oke, F.A.; Lawal, F.J.; et al. Comorbidities and the COVID-19 pandemic dynamics in Africa. Trop. Med. Int. Health 2021, 26, 2–13. [Google Scholar] [CrossRef]
- Omran, A.; Awad, H.; Ibrahim, M.; El-Sharkawy, S.; Elfiky, S.; Rezk, A.R. Lung Ultrasound and Neutrophil Lymphocyte Ratio in Early Diagnosis and Differentiation between Viral and Bacterial Pneumonia in Young Children. Children 2022, 9, 1457. [Google Scholar] [CrossRef]
- Buonacera, A.; Stancanelli, B.; Colaci, M.; Malatino, L. Neutrophil to Lymphocyte Ratio: An Emerging Marker of the Relationships between the Immune System and Diseases. Int. J. Mol. Sci 2022, 23, 3636. [Google Scholar] [CrossRef]
- de Jager, C.P.; Wever, P.C.; Gemen, E.F.; Kusters, R.; van Gageldonk-Lafeber, A.B.; van der Poll, T.; Laheij, R.J. The Neutrophil-Lymphocyte Count Ratio in Patients with Community-Acquired Pneumonia. PLoS ONE 2012, 7, e46561. [Google Scholar] [CrossRef]
- Cataudella, E.; Giraffa, C.M.; Di Marca, S.; Pulvirenti, A.; Alaimo, S.; Pisano, M.; Terranova, V.; Corriere, T.; Ronsisvalle, M.L.; Di Quattro, R.; et al. Neutrophil-To-Lymphocyte Ratio: An Emerging Marker Predicting Prognosis in Elderly Adults with Community-Acquired Pneumonia. J. Am. Geriatr. Soc. 2017, 65, 1796–1801. [Google Scholar] [CrossRef] [PubMed]
- Nair, H.; Simões, E.A.; Rudan, I.; Gessner, B.D.; Azziz-Baumgartner, E.; Zhang, J.S.F.; Feikin, D.R.; Mackenzie, G.A.; Moiïsi, J.C.; Roca, A.; et al. Global and regional burden of hospital admissions for severe acute lower respiratory infections in young children in 2010: A systematic analysis. Lancet 2013, 381, 1380–1390. [Google Scholar] [CrossRef] [PubMed]
- Naz, R.; Gul, A.; Javed, U.; Urooj, A.; Amin, S.; Fatima, Z. Etiology of acute viral respiratory infections common in Pakistan: A review. Rev. Med. Virol. 2019, 29, e2024. [Google Scholar] [CrossRef] [PubMed]
- Borchers, A.T.; Chang, C.; Gershwin, M.E.; Gershwin, L.J. Respiratory syncytial virus—A comprehensive review. Clin. Rev. Allergy Immunol. 2013, 45, 331–379. [Google Scholar] [CrossRef]
- Zhang, N.; Wang, L.; Deng, X.; Liang, R.; Su, M.; He, C.; Hu, L.; Su, Y.; Ren, J.; Yu, F.; et al. Recent advances in the detection of respiratory virus infection in humans. J. Med. Virol. 2020, 92, 408–417. [Google Scholar] [CrossRef]
- Van der Zalm, M.M.; Uiterwaal, C.S.; Wilbrink, B.; Koopman, M.; Verheij, T.J.; van der Ent, C.K. The influence of neonatal lung function on rhinovirus-associated wheeze. Am. J. Respir. Crit. Care Med. 2011, 183, 262–267. [Google Scholar] [CrossRef]
- Zhu, X.; Ge, Y.; Wu, T.; Zhao, K.; Chen, Y.; Wu, B.; Zhu, F.; Zhu, B.; Cui, L. Co-infection with respiratory pathogens among COVID-2019 cases. Virus Res. 2020, 285, 198005. [Google Scholar] [CrossRef]
- Musuuza, J.S.; Watson, L.; Parmasad, V.; Putman-Buehler, N.; Christensen, L.; Safdar, N. Proportion and outcomes of co-infection and superinfection with SARS-CoV-2 and other pathogens: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0251170. [Google Scholar] [CrossRef]
- Lansbury, L.; Lim, B.; Baskaran, V.; Lim, W.S. Co-infections in people with COVID-19: A systematic review and meta-analysis. J. Infect. 2020, 81, 266–275. [Google Scholar] [CrossRef]
- Davis, B.; Rothrock, A.N.; Swetland, S.; Andris, H.; Davis, P.; Rothrock, S.G. Viral and atypical respiratory co-infections in COVID-19: A systematic review and meta-analysis. J. Am. Coll. Emerg. Physicians Open 2020, 1, 533–548. [Google Scholar] [CrossRef]
- World Health Organization (WHO). World Health Statistics. Available online: https://www.who.int/data/gho/publications/world-health-statistics (accessed on 3 October 2023).
| References | Collection Period | Year of Publication | Study Country | Age Range | Study Objective | Zone/Sample Size | Study Framework | Type of Sampling | Diagnostic Methods | Proportion of Pathogens | Type of Study |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lekana -Douki et al. [23] | 2009–2011 | 2013 | Gabon | No limit | To report the results of a large surveillance study for pH1N1 in Gabon during a 2-year period, July 2009–June 2011 | Urban/966 | Health care centers The regional hospitals | Nasal | RT-PCR | Flu A (61%); Flu B (39%) | Cross-sectional/Prospective |
| Lekana- Douki et al. [24] | 2010–2011 | 2014 | Gabon | No limit | To determine the prevalence, etiology and seasonality of viral respiratory tract infections | (Urban)/1041 | Health care centers The regional hospitals | Nasopharyngeal | One-step multiplex real-time RT-PCR | HAdV (17.5%), HPIV 1–4 (16.8%), EV (14.7%), HRSV (13.5%), and Flu A (11.9%) | Cross-sectional |
| Ouédraogo et al. [5] | 2010–2011 | 2014 | Burkina Faso | <3 years | To identify the respiratory viruses, present in children admitted to or consulting at the pediatric hospital in Ouagadougou | (Urban)/209 | Charles de Gaulle pediatric hospital | Nasopharyngeal | One-step multiplex real-time RT-PCR | HRV (59.1%); EV (25.5%); HRSV (16.1%); HMPV (9.4%) | Prospective |
| Breiman et al. [25] | 2007–2011 | 2015 | Kenya | <5 years | To analyze data from our population-based infectious disease surveillance (PBIDS) site in Kibera, an urban slum in Nairobi | 2592 | Community (Households) | Blood Naso/Oro-pharyngeal | Hemoculture RT-qPCR | HRV/EV (42%); HRSV (25%); HAdV (20%); HMPV (13.7%), Flu A (10.8%); Salmonella typhi (1.6%); Streptococcus pneumoniae (1%); Staphylococcus aureus (1.7%) | Cross-sectional |
| Serenbe et al. [26] | 2013 | 2015 | Central African Republic | <5 years | To determine the contribution of viruses to respiratory infections in children under five. | 361 | Referral hospital Outlying pediatric centers | Nasopharyngeal | RT-qPCR Multiplex RT-PCR | HRV (47.5%); FluA/B (26.6%); HPIV-3(9.3%); HRSV (5.8%); EV (4.3%); HAdV (2.9%); HBoV (1.4%); HCoV (1.4%) | Cross-sectional |
| Kenmoe et al. [27] | 2011–2013 | 2016 | Cameroon | ≤15 | To investigate the viral etiology and seasonality of SARI in hospitalized children in Yaoundé, Cameroon | (Urban)/347 | Hospital (pediatric service) | Nasopharyngeal | Multiplex PCR RT-PCR | HRSV (13.2%), HAdV (27.3%), HboV (10.6%), Flu A/B (9.8%); HPIV (6.6%); HCoV (5.7%); HMPV (2.3%); HRV/EV (11.5%) | Prospective |
| Uzoamaka et al. [28] | 2014–2016 | 2017 | Nigeria | No limit | To determine the current trends of bacterial etiology of LRTIs among the patients that attended the University of Nigeria Teaching Hospital (UNTH), and their antimicrobial susceptibility profile with special interest in pan drug resistance | (Peri-urban) /954 | Hospital | Expectoration | Culture (MacConkey agar, blood agar, chocolate agar) | Klebsiella pneumonia (49.9%); Klebsiella spp./Pseudomonas aeruginosa, (1.4%) | Cross-sectional |
| Niang et al. [29] | 2012–2015 | 2017 | Senegal | No limit | To investigate the epidemiologic and viral molecular features of HAdVs circulating in Senegal after 4 consecutive years of sentinel surveillance of influenza like illness cases | (Urban) /6381 | Hospital | Naso/Oro-pharyngeal | Two-step multiplex real-time RT-PCR | HAdV (30.8%); FluA/B (53.1%); HRV (30%); Ev (18.5%); HRSV (13.5%) | Cross-sectional/ Prospective |
| Famoroti et al. [30] | 2011–2015 | 2018 | South Africa | 0–5 years | To determine the most common viral pathogens associated with ARTI among children between 0 and 5 years of age in KwaZulu-Natal | (Urban) /2172 | Hospital (pediatric service) | Expectoration /Nasopharyngeal | Multiplex PCR | HRSV (32.1%), HAdV (21.8%), HRV (15.4%), FluA swl (5.1%) | Retrospective |
| Kadjo et al. [31] | 2013 | 2018 | Ivory Coast | <5 years | To describe the epidemiological, clinical, and virological pattern of ARI that tested negative for influenza virus, in children under five years old | (Urban) /1340 | Hospital (pediatric service) | Nasopharyngeal | RT-PCR | HRV (31.92%), HRSV (24.4%), HPIV (20.5%), HCoV 229E (12.05%) | Cross-sectional |
| Sanou et al. [32] | 2014–2015 | 2018 | Burkina Faso | <5 years | To assess the prevalence and seasonal occurrence of influenza viruses in children with ILI and severe acute respiratory infection (SARI) | (Urban) /924 | Healthcare centers | Nasopharyngeal | RT-PCR | Flu A/B (15.1%), A(H3N2) (69.1%) A(H1N1) pdm09 (30.9%) | Cross-sectional |
| Obodai et al. [33] | 2006, 2013–2014 | 2018 | Ghana | <5 years | To assess HRSV diagnostics and/or surveillance in affected age groups in the future and to the molecular understanding of the HRSV circulation in Ghana, Africa | (Urban) /552 | Hospital (pediatric service) | Nasopharyngeal | RT-PCR | HRSV (23%) | Cross-sectional |
| Lekana-Douki et al. [34] | 2018 | 2018 | Gabon | <5 years | To evaluate the prevalence and the HBoV genotype in children under 5 years old with ILI or diarrhea in Gabon | (Urban) /810 | Health centers | Nasopharyngeal | RT-PCR | HBoV (4.4%) | Retrospective |
| Kabego et al. [35] | 2016 | 2018 | Democratic Republic of the Congo | <5 years | To determine the prevalence of human respiratory syncytial virus (HRSV) acute respiratory infection (ARI) in children under the age of 5 years at the Provincial General Hospital of Bukavu (PGHB), and to analyze factors associated with the risk of ARI being diagnosed as lower respiratory tract infection (LRTI) | (Urban) /146 | General Hospital | Nasopharyngeal | Multiplex RT-PCR | HRSV (21.2%); HRV (16.4%); HPIV-3 (16.6%) and HAdV (4.79%). | Cross-sectional, analytical/Prospective |
| Mhimbira et al. [21] | 2013–2015 | 2018 | Tanzania | No limit | To describe the prevalence of respiratory pathogens in TB patients and household contact controls, and the clinical significance of respiratory pathogens in TB patients | (Urban) /972 | Community (Households) | Nasopharyngeal | Multiplex RT-PCR | HRV (9.3%); Influenza A (3.1%); HRSV A (1.9%); H. influenzae (26.1%); S. pneumoniae (21.5%) | Prospective cohort |
| Kenmoe et al. [36] | 2011–2014 | 2018 | Cameroon | <15 years | To document the different types of HAdV circulating in Cameroon in children with acute respiratory infections | (Urban) /811 | Hospital (pediatric service) | Nasopharyngeal | RT-PCR | HAdV (27.12%) | Cross-sectional |
| Razanajatovo et al. [22] | 2010–2013 | 2018 | Madagascar | No limit | To identify etiologies and describe clinical features of SARI-associated hospitalization in Madagascar | (Urban) /876 | Hospital- based | Nasopharyngeal, Expectorations Blood | Multiplex RT-PCR Cytobacteriologic testing | HRSV (37.7%); FluA (18.4%); HRV (13.5%; HAdV (8.3%); S. Pneumoniae (50.3%); H. Influenzae b (21.4%); Klebsiella (4.6%) | Prospective |
| Tchatchouang et al. [18] | 2019 | 2019 | Cameroon | No limit | To identify the respiratory bacteria of patients presenting with symptoms and clinical signs of LRTI at a referral center for respiratory diseases in Yaoundé, Cameroon | (Urban) /141 | Hospital (Pneumology department) | Branco-alveolar lavage (BAV) | Bacterial Culture | S. pneumoniae/H. infuenzae (14.2%); K. pneumoniae (9.2%); S. aureus, (7.1%) | Prospective |
| Adema et al. [37] | 2017–2018 | 2020 | Kenya | <20 years | To advance understanding of the nature of spread of respiratory viruses | (Urban) /781 | Community (School) | Nasopharyngeal | Multiplex RT-PCR | HRV (16.7%); HPIV (2.7%); HCoV (229E, NL63, OC43) (2.0%); HAdV (0.9%); HRSV (0.6%) | Longitudinal/ Cohort |
| Jarju et al. [3] | 2018–2019 | 2020 | Gambia | <5 years | To determine the viral etiology, seasonality, clinical features and associated AMU | (Urban) /805 | Hospital (Medical Research Council Unit) | Nasopharyngeal | Multiplex RT-PCR | HRV (36.7%); Flu A (7.0%); Flu B (1.4%); HRSV (14.7%); HMPV (7.2%); HPIV (13.2%); HCoV (229E, OC43 or NL63) (7.8%) | Prospective |
| Buchwald et al. [38] | 2011–2013 | 2020 | Mali | <2 years | To provide the first estimates of RSV incidence in Mali | (Urban) /1333 | Community (Households) | Naso/Oro-pharyngeal | RT-PCR | HRSV (37%) | Cohort |
| Obe et al. [39] | 2021 | 2021 | Nigeria | <5 years | To determine molecular prevalence of RSV among under five children admitted with ALRTTIs in a tertiary hospital and identify the risk factors associated with the acquisition of RSV-ALRTIs | (Urban) /200 | Hospital (pediatric service) | Nasopharyngeal | RT-PCR | HRSV (22.5%) | Cross-sectional |
| Deberu et al. [11] | 2018–2019 | 2021 | –Ghana | No limit | To identify the presence of pathogens in sputum of suspected tuberculosis cases and their antimicrobial resistance patterns | (Urban) /264 | Public Health Laboratory | Expectoration | Culture (MacConkey agar, blood agar, chocolate agar) | Klebsiella spp. (28%); M. tuberculosis (6.5%); Pseudomonas spp. (15.2%) | Retrospective |
| Kouakou et al. [40] | 2021 | 2021 | Ivory Coast | ≤5 years | To provide general knowledge on the epidemiology of the virus, its seasonality and the signs associated with RSV in children aged 0 to 5 years in Côte d’Ivoire | (Urban/rural)/5648 | Hospitals University (CHU) Regional Hospitals (CHR), General Hospitals (HG) Community Urban Health Unit | Nasopharyngeal | RT-qPCR | HRSV (10%) | Cross-sectional/descriptive |
| Kenmoe et al. [41] | 2011–2014 | 2021 | Cameroon | No limit | To report the occurrence and phylogenetic relatedness of EVs and RVs detected in samples from patients of all ages suffering from ARI in Cameroon based on the sequences of the VP4/VP2 genomic region | (Urban) /974 | Health centers | Nasopharyngeal | RT-PCR | HRV/EV (16.4%) | Cross-sectional |
| Birindwa et al. [20] | 2015–2017 | 2021 | Democratic Republic of the Congo | ≤5 years | To describe clinical characteristics and risk factors and to determine the occurrence of bacteria and viruses in the nasopharynx of hospitalized children with pneumonia in the Eastern DR Congo | (Urban) /2322 | Hospital | Nasopharyngeal | Multiplex RT-PCR assay Culture | H. influenzae (54%); S. pneumoniae (96%); HRV (73%); EV (17%); HRSV (7%); | Cross-sectional |
| Ntagereka et al. [42] | 2021 | 2022 | Democratic Republic of the Congo | No limit | To investigate the prevalence of SARSCoV-2, influenza A and B, and other acute respiratory viruses among local patients with flu-like symptoms | (Urban) /1352 | Hospital, Health Center. | Oro-pharyngeal | RT-PCR | SARS-CoV-2 (13.9%), Flu A (5.6%), Flu B (0.9%) | Cross-sectional |
| Kafintu- Kwashie et al. [43] | 2015–2016 | 2022 | Ghana | <5 years | To investigate and genotype respiratory syncytial virus and human metapneumovirus in children presenting with ALRTI infections at the Princess Marie Louis Children’s Hospital in Accra, Ghana | (Urban) /188 | Hospital | Nasopharyngeal | Two-step RT-PCR | HRSV (11.4); HMPV (1.7%); | Cross-sectional |
| Kolawole et al. [44] | 2017 | 2017 | Nigeria | <14 years | To investigate if clinical cases may describe the entire picture of ARI among children in Nigeria | (Urban) /91 | Community Hospital | Nasopharyngeal | PCR | HcoV OC43 (13.3%); HcoV 229E/NL63 (12.5%) | Cross-sectional |
| Ukuli et al. [45] | 2008–2016 | 2023 | Uganda | No limit | To identify and characterize new and re-emerging adenoviruses, which is important in the prevention and control of disease outbreaks as it would aid in predicting and preparing for future disease occurrences | 2298 | Hospital | Nasopharyngeal | PCR | HAdV (9.8%) | Retrospective |
| Feikin et al. [46] | 2007–2010 | 2012 | Kenya | No limit | To report bacterial and viral etiologies of ARI by age group, hospitalization status, HIV infection status and season. We also provide incidence by etiology, adjusted for healthcare seeking and presence of pathogens in asymptomatic controls | (Rural) /3046 | Community Hospital | Naso/Oro-pharyngeal Blood Urine | RT-qPCR Culture | HRV/EV (33%); Flu A (22%); S. pneumoniae (3%); Salmonella sp. (3%) | Cross-sectional |
| Fokam et al. [47] | 2020–2021 | 2022 | Cameroon | No limit | To conduct a study in a large number of individuals tested for the presence of SARS-CoV-2 by PCR during the first epidemiological wave, to shed more light on the epidemiological, virological and clinical characteristics of COVID-19 in Cameroon | Urban/14119 | Center for research | Nasopharyngeal | RT-PCR | SARS-CoV-2 (12.7%) | Cross-sectional |
| Dorkenoo et al. [48] | 2020 | 2022 | Togo | No limit | To estimate the prevalence of malaria and COVID-19 in febrile patients in Lomé | Urban/243 | Community health center of Legbassito; Hospital of Bè; Centre Hospitalier Universitaire Campus | Nasopharyngeal | GeneXpert | SARS-CoV-2 (7.4%) | Cross-sectional |
| Alber et al. [49] | 2020–2021 | 2022 | Mali | No limit | To estimate the degree of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) transmission among health care workers (HCWs) and the general population in a West African setting | Urban/2392 | Referral and community health center | Oro-pharyngeal | RT-PCR | SARS-CoV-2 (2.8%) | Cohort |
| Khairy et al. [50] | 2020–2021 | 2023 | Sudan | <19 years | To describe the epidemiology of COVID-19 in children and adolescents in Sudan during 2020–2021 | Urban/3150 | Not indicated | Nasopharyngeal | PCR | SARS-CoV-2 (44%) | Cross-sectional |
| Mulenga et al. [51] | 2020 | 2021 | Zambia | No limit | To estimate SARS-CoV-2 prevalence in six districts of Zambia in July 2020, using a population-based household survey | Urban/2848 | Households | Nasopharyngeal | RT-PCR | SARS-CoV-2 (7.6%) | Cross-sectional |
| References | Collection Period | Year of Publication | Study Country | Age Range | Study Objective | Zone/Sample Size | Study Framework | Type of Sampling | Diagnostic Methods | Proportion of Pathogens | Type of Study |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lagare et al. [14] | 2010–2012 | 2015 | Niger | <5 years | To document the prevalence of selected viral and bacterial infections among children <5 years of age hospitalized with severe acute respiratory illness (SARI) | (Urban)/160 | Hospital | Nasopharyngeal | One-step multiplex RT-PCR | HRSV (35%); HRV (29%); HPIV (24%); S. pneumoniae (56%); H. inflenzae (12%) | Retrospective |
| Lagare et al. [19] | 2015 | 2019 | Niger | <5 years | To describe viral and bacterial infections among children aged younger than 5 years hospitalized with febrile ARI at two hospitals in Niamey, Niger’s capital city, and the reported clinical procedures. | (Urban)/638 | Hospital | Expectoration /Nasopharyngeal | RT-qPCR | HRSV (23.3%), HPIV (12.2%), HRV (9.4%), HAdV (9.4%), Flu A (8.1%)/S. pneumoniae (39%), S. aureus (12.2%), H. influenzae B (2.5%) | Prospective |
| Wadilo et al. [52] | 2019–2022 | 2023 | Ethiopia | <5 years | To estimate the contribution of respiratory viruses to LRTIs among hospitalized children younger than 5 years. | (Urban)/420 | Hospital | Naso/Oro-pharyngeal | RT-qPCR | HRSVA/B (30.5%); HRV (18.6%); HBoV (16.2%); HMPV (23.3%); SARS-CoV-2 (0.47%) | Prospective case–control |
| Baillie et al. [53] | 2011–2014 | 2021 | South Africa | ≤5 years | To focus on the clinical epidemiology of RV infection, overall and by site, and its interactions with other respiratory pathogens in children 1–59 months of age hospitalized with pneumonia and in community controls. | (Urban)/4232 | Hospital | Naso/Oro-pharyngeal | RT-PCR | HRV (21%) | Cross-sectional |
| Simusika et al. [54] | 2011–2012 | 2015 | Zambia | <5 years | To detect upper respiratory pathogens in specimens that were previously laboratory-confirmed influenza negative, to investigate the relative frequency of isolation, seasonality, and clinical diagnosis of various pathogens identified from SARI patients | (Urban)/496 | Hospital | Naso/Oro-pharyngeal | Singleplex and multiplex rRT-PCR | HRV (19.2%); HADV (16.8%); HRSV (15.2%); HMPV (4.7%); S. pneumoniae (54.8%); M. catarrhalis (46.2%); H. influenzae (40.7%) | Cross-sectional |
| Loevinsohn et al. [55] | 2018–2019 | 2021 | Zambia | No limit | To describe the diversity of pathogens in the nasopharynx among patients with respiratory infections presenting for care in rural Zambia and the prognostic implications of co-infection. | (Rural)/671 | Hospital | Nasopharyngeal | RT-PCR (GeneXpert) | Flu A (12.7%); Flu B (6.4%); HRSV (4.4%); HRV (26.13%); HPIV (2.08%) HMPV (1.01%); HCoV (6.27%); HAdV (2.63%); Bordetella pertussis (0.19%) | Cross-sectional |
| Ouédraogo et al. [56] | 2010–2011 | 2016 | Burkina Faso | <5 years | To investigate the prevalence of RSV viral infections in infants suffering from respiratory infections and hospitalized in the city of Ouagadougou, and to evaluate the clinical characteristics associated with the identification of RSV. | (Urban)/209 | Hospital | Nasopharyngeal | RT-PCR | HRSV (16.2%) | Cross-sectional |
| Kenmoe [57] | 2011–2014 | 2017 | Cameroon | <15 years | To determine the etiology of ARI in children hospitalized in Yaoundé, Cameroon, and to genetically characterize the HRSV and HMPV strains detected. | (Urban)/822 | Hospital | Nasopharyngeal | PCR/RT-PCR | HRSV (9%); HMPV (3.9%); HAdV (28.5%); Flu A/B (21.4%); HRV/EV (15.5%); HBoV (9.4%); HCoV (8.2%); HPIV (6.2%) | Descriptive and cross-sectional |
| Sanou [58] | 2014–2015 | 2018 | Burkina Faso | <5 years | To study the epidemiology and genetic diversity of viruses and bacteria involved in acute respiratory infections in children under five in Burkina Faso. | (Urban)/584 | Hospital | Nasopharyngeal | PCR | HRV (29.8%); HRSV (13%); HAdV (9.8%); HBoV (8.2%); HPIV (7.8%); HMPV (6.2%); HCoV (3.1%); Flu A/B (12.3%); Flu C (2.9%) | Cross-sectional |
| O’Callaghan-Gordo et al. [59] | 2006–2007 | 2011 | Mozambique | <5 years | To present surveillance data on the epidemiology of several respiratory viruses associated with clinical pneumonia in children <5 years admitted to a rural hospital in Mozambique, a malaria-endemic area with high HIV prevalence | (Rural)/394 | hospital-based | Nasopharyngeal Aspirate | Multiplex RT-PCR | HRV (41%); HAdV (21%); HRSV (11%); HMPV (8%); Flu A/B (8%); HPIV (7%); EV (4%) | Cross-sectional |
| Jones et al. [60] | 2010–2013 | 2016 | Ghana | <5 years | To concurrently conduct surveillance for severe acute respiratory infection and acute febrile illness (AFI) in three referral hospitals in Ghana to compare influenza-related epidemiologic data from the two syndrome-based surveillance platforms. | (Urban)/1273 | Hospital | Naso/Oro-pharyngeal | RT-PCR | Flu A (55%); H1N1 (26%); H3N2 (29%); FluB (45%) | Cross-sectional |
| Simeon et al. [61] | 2017–2018 | 2021 | Namibia | <5 years | To formulate cumulative antibiograms for Intensive Care Units (ICUs) of referral hospitals in Namibia to guide future antibiotic use | (Urban)/976 | Hospital | Expectoration | Culture | K. pneumoniae (8.8%), Enterobacter sp. (22.2%); P. aeruginosa (37.5%) | Retrospective Analytical Cross-sectional |
| Mveang Nzoghe et al. [62] | 2020 | 2021 | Gabon | No limit | To Analyze and understand the dynamics of SARS-CoV-2 infection in this unique setting may help other countries in the fight against the COVID-19 pandemic. | Urban/3464 | Not indicated | Naso/Oro-pharyngeal and blood | RT-PCR | SARS-CoV-2 (17.2%) | Retrospective |
| Sebastião et al. [63] | 2021 | 2021 | Angola | No limit | To study the prevalence of SARS-CoV-2 in parturients and the risk factors that may be related to SARS-CoV-2 transmission to newborns in Luanda, the capital city of Angola. | Urban/3633 | Hospital | Nasopharyngeal | RT-PCR | SARS-CoV-2 (0.4%) | Cross-sectional |
| Proportion (%) | Number of Studies | Number of Countries | |
|---|---|---|---|
| Virus | |||
| Human Respiratory Syncytial Virus | 0.6–59 | 28 | 18 |
| Human rhinovirus | 7.5–73 | 24 | 14 |
| Influenza virus A/B | 0.9–69 | 19 | 13 |
| Human adenovirus | 0.9–30.8 | 17 | 13 |
| Human Parainfluenza virus | 2–24 | 13 | 10 |
| HCoV (NL63, OC43, 229E, HKU-1) | 1.4–13.9 | 10 | 8 |
| Human Enterovirus | 2.9–25.5 | 11 | 7 |
| Human metapneumovirus | 1–23.3 | 11 | 7 |
| SARS-CoV-2 | 0.4–44 | 9 | 9 |
| Human bocavirus | 1.4–16.2 | 6 | 5 |
| Bacteria | |||
| Streptococcus pneumoniae | 1–96 | 8 | 9 |
| Haemophilus influenzae type b | 2.5–54 | 7 | 6 |
| Klebsiella pneumoniae | 1.4–49.9 | 6 | 5 |
| Staphylococcus aureus | 1.7–12.2 | 2 | 3 |
| Pseudomonas aeruginosa | 1.4–37.5 | 3 | 3 |
| Salmonella typhi | 1.6–3 | 2 | 1 |
| Mycobacterium tuberculosis | 0–6.5 | 1 | 1 |
| M. catarrhalis | 0–46.2 | 1 | 1 |
| B. Pertussis | 0–0.1 | 1 | 1 |
| Enterobacter sp. | 22.2 | 1 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Demboux Lyelet, J.E.; Mayengue, P.I.; Koukouikila-Koussounda, F.; Leroy, E.M.; Becquart, P.; Niama, F.R. Viral and Bacterial Etiology of Common Respiratory Infections in Children in Sub-Saharan Africa: A Systematic Review. Children 2025, 12, 1212. https://doi.org/10.3390/children12091212
Demboux Lyelet JE, Mayengue PI, Koukouikila-Koussounda F, Leroy EM, Becquart P, Niama FR. Viral and Bacterial Etiology of Common Respiratory Infections in Children in Sub-Saharan Africa: A Systematic Review. Children. 2025; 12(9):1212. https://doi.org/10.3390/children12091212
Chicago/Turabian StyleDemboux Lyelet, Jordy Exaucé, Pembe Issamou Mayengue, Félix Koukouikila-Koussounda, Eric M. Leroy, Pierre Becquart, and Fabien Roch Niama. 2025. "Viral and Bacterial Etiology of Common Respiratory Infections in Children in Sub-Saharan Africa: A Systematic Review" Children 12, no. 9: 1212. https://doi.org/10.3390/children12091212
APA StyleDemboux Lyelet, J. E., Mayengue, P. I., Koukouikila-Koussounda, F., Leroy, E. M., Becquart, P., & Niama, F. R. (2025). Viral and Bacterial Etiology of Common Respiratory Infections in Children in Sub-Saharan Africa: A Systematic Review. Children, 12(9), 1212. https://doi.org/10.3390/children12091212






