From Alginate to Pixel: Comparing the Effect of Two Dental Impression Methods on Children’s Anxiety
Abstract
1. Introduction
- 1.
- Higher levels of anxiety, reflected by greater increases in HR and more significant decreases in SpO2, will be detected during alginate impressions.
- 2.
- The use of intraoral scanning will result in greater stability in HR and SpO2.
- 3.
- From a physiological standpoint, intraoral scanning will be the less anxiety-inducing technique.
2. Materials and Methods
2.1. Study Sample and Setting
2.2. Ethical Considerations
2.3. Data Collection
2.4. Study Protocol
2.4.1. Baseline Phase
2.4.2. Oral Cavity Impression Phase
2.4.3. Conventional Technique (Alginate)
2.4.4. Digital Technique (Intraoral Scanner)
2.4.5. Interval Phase
2.5. Statistical Analysis
3. Results
3.1. Graphical Analysis of Physiological Responses
3.2. Descriptive Analysis
3.2.1. Heart Rate (HR)
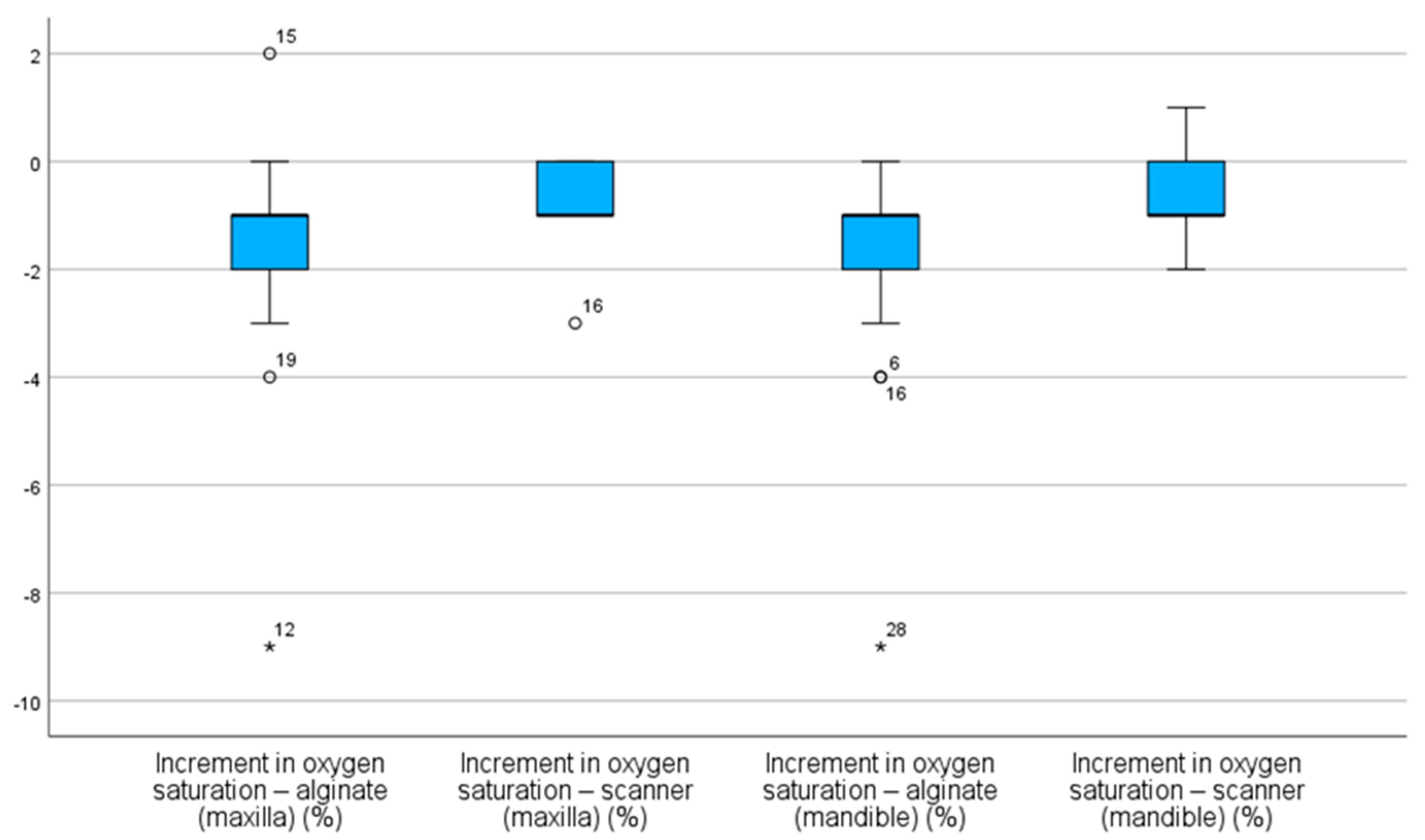
3.2.2. Oxygen Saturation (SpO2)
3.3. InferentialAnalysis
3.3.1. Heart Rate (HR)
3.3.2. Oxygen Saturation (SpO2)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HR | Heart rate |
| SpO2 | Oxygen saturation |
| bpm | Beats per minute |
| FC INCR | Heart rate saturation increment |
| INCR SpO2 | Oxygen saturation increment |
References
- Zhang, C.; Qin, D.; Shen, L.; Ji, P.; Wang, J. Does Audiovisual Distraction Reduce Dental Anxiety in Children under Local Anesthesia? A Systematic Review and Meta-analysis. Oral Dis. 2019, 25, 416–424. [Google Scholar] [CrossRef] [PubMed]
- Aziz, S.Z.; Jafar, Z.J. The Efficacy of Little Lovely Dentist and Tell Show Do in Alleviating Dental Anxiety in Iraqi Children: A Randomized Clinical Trial. J. Int. Soc. Prev. Community Dent. 2023, 13, 388–393. [Google Scholar] [CrossRef] [PubMed]
- Özmen, E.E.; Taşdemir, İ. Evaluation of the Effect of Dental Anxiety on Vital Signs in the Order of Third Molar Extraction. BMC Oral Health 2024, 24, 841. [Google Scholar] [CrossRef] [PubMed]
- Ghaffar, R.S.A.; Sheikh, M.; Kidwai, M.; Sanaullah, A.; Salman, M.; Ilyas, A.; Ahmed, N.; Lal, A. Impact of High-Speed Handpiece Noise-Induced Dental Anxiety on Heart Rate: Analyzing Experienced and Non-Experienced Patients—A Comparative Study. BMC Oral Health 2024, 24, 265. [Google Scholar] [CrossRef]
- Sun, I.G.; Chu, C.H.; Lo, E.C.M.; Duangthip, D. Global Prevalence of Early Childhood Dental Fear and Anxiety: A Systematic Review and Meta-Analysis. J. Dent. 2024, 142, 104841. [Google Scholar] [CrossRef]
- Karaca, S.; Sirinoglu Capan, B. The Effect of Sequential Dental Visits on Dental Anxiety Levels of Paediatric Patients. Eur. J. Paediatr. Dent. 2023, 24, 277–280. [Google Scholar] [CrossRef]
- Navit, S. Effectiveness and Comparison of Various Audio Distraction Aids in Management of Anxious Dental Paediatric Patients. J. Clin. Diagn. Res. 2015, 9, ZC05-9. [Google Scholar] [CrossRef]
- Anthonappa, R.P.; Ashley, P.F.; Bonetti, D.L.; Lombardo, G.; Riley, P. Non-Pharmacological Interventions for Managing Dental Anxiety in Children. Cochrane Database Syst. Rev. 2017, 24, 1151. [Google Scholar] [CrossRef]
- Zhang, D.; Li, S.; Zhang, R. Effects of Dental Anxiety and Anesthesia on Vital Signs during Tooth Extraction. BMC Oral Health 2024, 24, 632. [Google Scholar] [CrossRef]
- Kilinç, G.; Akay, A.; Eden, E.; Sevinç, N.; Ellidokuz, H. Evaluation of Children’s Dental Anxiety Levels at a Kindergarten and at a Dental Clinic. Braz. Oral Res. 2016, 30, e72. [Google Scholar] [CrossRef]
- Barbosa, N.B.; Rodrigues, B.R.; Madalena, I.R.; De Menezes, F.C.H.; Lepri, C.P.; De Oliveira, M.B.C.R.; Campos, M.G.D.; Oliveira, M.A.H.D.M. Effect of the Case for Carpule as a Visual Passive Distraction Tool on Dental Fear and Anxiety: A Pilot Study. Int. J. Environ. Res. Public. Health 2023, 20, 1793. [Google Scholar] [CrossRef] [PubMed]
- Yan, X.; Yan, Y.; Cao, M.; Xie, W.; O’Connor, S.; Lee, J.J.; Ho, M.-H. Effectiveness of Virtual Reality Distraction Interventions to Reduce Dental Anxiety in Paediatric Patients: A Systematic Review and Meta-Analysis. J. Dent. 2023, 132, 104455. [Google Scholar] [CrossRef]
- Babaji, P.; Chauhan, P.P.; Rathod, V.; Mhatre, S.; Paul, U.; Guram, G. Evaluation of Child Preference for Dentist Attire and Usage of Camouflage Syringe in Reduction of Anxiety. Eur. J. Dent. 2017, 11, 531–536. [Google Scholar] [CrossRef] [PubMed]
- Yon, M.J.Y.; Chen, K.J.; Gao, S.S.; Duangthip, D.; Lo, E.C.M.; Chu, C.H. Dental Fear and Anxiety of Kindergarten Children in Hong Kong: A Cross-Sectional Study. Int. J. Environ. Res. Public. Health 2020, 17, 2827. [Google Scholar] [CrossRef] [PubMed]
- Murad, M.; Ingle, N.; Assery, M. Evaluating Factors Associated with Fear and Anxiety to Dental Treatment—A Systematic Review. J. Fam. Med. Prim. Care 2020, 9, 4530. [Google Scholar] [CrossRef]
- Bagher, S.M.; Felemban, O.M.; Alsabbagh, G.A.; Aljuaid, N.A. The Effect of Using a Camouflaged Dental Syringe on Children’s Anxiety and Behavioral Pain. Cureus 2023, 15, e50023. [Google Scholar] [CrossRef]
- Kalra, N.; Sabherwal, P.; Tyagi, R.; Khatri, A.; Srivastava, S. Relationship between Subjective and Objective Measures of Anticipatory Anxiety Prior to Extraction Procedures in 8- to 12-Year-Old Children. J. Dent. Anesth. Pain Med. 2021, 21, 119. [Google Scholar] [CrossRef]
- Alghareeb, Z.; Alhaji, K.; Alhaddad, B.; Gaffar, B. Assessment of Dental Anxiety and Hemodynamic Changes during Different Dental Procedures: A Report from Eastern Saudi Arabia. Eur. J. Dent. 2022, 16, 833–840. [Google Scholar] [CrossRef]
- Dantas, M.V.M.; Nesso, B.; Mituuti, D.S.; Gabrielli, M.A.C. Assessment of Patient’s Anxiety and Expectation Associated with Hemodynamic Changes during Surgical Procedure under Local Anesthesia. Rev. Odontol. UNESP 2017, 46, 299–306. [Google Scholar] [CrossRef]
- Salma, R.G.; Abu-Naim, H.; Ahmad, O.; Akelah, D.; Salem, Y.; Midoun, E. Vital Signs Changes during Different Dental Procedures: A Prospective Longitudinal Cross-over Clinical Trial. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2019, 127, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Debs, N.; Aboujaoude, S. Effectiveness of Intellectual Distraction on Gagging and Anxiety Management in Children: A Prospective Clinical Study. J. Int. Soc. Prev. Community Dent. 2017, 7, 315. [Google Scholar] [CrossRef] [PubMed]
- Glisic, O.; Hoejbjerre, L.; Sonnesen, L. A Comparison of Patient Experience, Chair-Side Time, Accuracy of Dental Arch Measurements and Costs of Acquisition of Dental Models. Angle Orthod. 2019, 89, 868–875. [Google Scholar] [CrossRef]
- Gandhi, M.; Lakade, L.; Kunte, S.; Patel, A.; Shah, P.; Chaudhary, S. Effect of Virtual Reality and Musical Earplug Temporal Tap Technique in Reduction of Gag Reflex in Pediatric Patients. Int. J. Clin. Pediatr. Dent. 2024, 17, 981–986. [Google Scholar] [CrossRef]
- Dixit, U.B.; Moorthy, L. The Use of Interactive Distraction Technique to Manage Gagging during Impression Taking in Children: A Single-Blind, Randomised Controlled Trial. Eur. Arch. Paediatr. Dent. 2021, 22, 219–225. [Google Scholar] [CrossRef]
- Yilmaz, H.; Aydin, M.N. Digital versus Conventional Impression Method in Children: Comfort, Preference and Time. Int. J. Paediatr. Dent. 2019, 29, 728–735. [Google Scholar] [CrossRef]
- Mangano, A.; Beretta, M.; Luongo, G.; Mangano, C.; Mangano, F. Conventional vs. Digital Impressions: Acceptability, Treatment Comfort and Stress Among Young Orthodontic Patients. Open Dent. J. 2018, 12, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Christopoulou, I.; Kaklamanos, E.G.; Makrygiannakis, M.A.; Bitsanis, I.; Perlea, P.; Tsolakis, A.I. Intraoral Scanners in Orthodontics: A Critical Review. Int. J. Environ. Res. Public. Health 2022, 19, 1407. [Google Scholar] [CrossRef]
- Patel, C.; Barot, G.N.; Patel, M.C.; Nath, K.J.; Patel, S.P.; Patel, D.K. Accuracy and Comfort in Digital and Conventional Impression in Pediatric Dental Patients: A Randomized Comparative Study. Cureus 2025, 17, e76882. [Google Scholar] [CrossRef] [PubMed]
- Bosoni, C.; Nieri, M.; Franceschi, D.; Souki, B.Q.; Franchi, L.; Giuntini, V. Comparison between Digital and Conventional Impression Techniques in Children on Preference, Time and Comfort: A Crossover Randomized Controlled Trial. Orthod. Craniofac. Res. 2023, 26, 585–590. [Google Scholar] [CrossRef]
- Zarbakhsh, A.; Jalalian, E.; Samiei, N.; Mahgoli, M.H.; Kaseb Ghane, H. Accuracy of Digital Impression Taking Using Intraoral Scanner Versus the Conventional Technique. Front. Dent. 2021, 18, 6. [Google Scholar] [CrossRef]
- Burhardt, L.; Livas, C.; Kerdijk, W.; Van Der Meer, W.J.; Ren, Y. Treatment Comfort, Time Perception, and Preference for Conventional and Digital Impression Techniques: A Comparative Study in Young Patients. Am. J. Orthod. Dentofacial Orthop. 2016, 150, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Serrano-Velasco, D.; Martín-Vacas, A.; Cintora-López, P.; Paz-Cortés, M.M.; Aragoneses, J.M. Comparative Analysis of the Comfort of Children and Adolescents in Digital and Conventional Full-Arch Impression Methods: A Crossover Randomized Trial. Children 2024, 11, 190. [Google Scholar] [CrossRef] [PubMed]
- Grisolia, B.M.; Dos Santos, A.P.P.; Dhyppolito, I.M.; Buchanan, H.; Hill, K.; Oliveira, B.H. Prevalence of Dental Anxiety in Children and Adolescents Globally: A Systematic Review with Meta-analyses. Int. J. Paediatr. Dent. 2021, 31, 168–183. [Google Scholar] [CrossRef]
- Al-Khotani, A.; Bello, L.A.; Christidis, N. Effects of Audiovisual Distraction on Children’s Behaviour during Dental Treatment: A Randomized Controlled Clinical Trial. Acta Odontol. Scand. 2016, 74, 494–501. [Google Scholar] [CrossRef]
- Nuvvula, S.; Alahari, S.; Kamatham, R.; Challa, R.R. Effect of Audiovisual Distraction with 3D Video Glasses on Dental Anxiety of Children Experiencing Administration of Local Analgesia: A Randomised Clinical Trial. Eur. Arch. Paediatr. Dent. 2015, 16, 43–50. [Google Scholar] [CrossRef]
- Agarwal, N. Effectiveness of Two Topical Anaesthetic Agents Used along with Audio Visual Aids in Paediatric Dental Patients. J. Clin. Diagn. Res. 2017, 11, ZC80–ZC83. [Google Scholar] [CrossRef]
- Albanchez-González, M.I.; Brinkmann, J.C.-B.; Peláez-Rico, J.; López-Suárez, C.; Rodríguez-Alonso, V.; Suárez-García, M.J. Accuracy of Digital Dental Implants Impression Taking with Intraoral Scanners Compared with Conventional Impression Techniques: A Systematic Review of In Vitro Studies. Int. J. Environ. Res. Public. Health 2022, 19, 2026. [Google Scholar] [CrossRef]
- Malik, J.; Rodriguez, J.; Weisbloom, M.; Petridis, H. Comparison of Accuracy Between a Conventional and Two Digital Intraoral Impression Techniques. Int. J. Prosthodont. 2018, 31, 107–113. [Google Scholar] [CrossRef]
- Jeddy, N.; Nithya, S.; Radhika, T.; Jeddy, N. Dental Anxiety and Influencing Factors: A Cross-Sectional Questionnaire-Based Survey. Indian J. Dent. Res. 2018, 29, 10. [Google Scholar] [CrossRef]
- Beena, J.P. Dental Subscale of Children′s Fear Survey Schedule and Dental Caries Prevalence. Eur. J. Dent. 2013, 7, 181–185. [Google Scholar] [CrossRef]
- Mendoza-Mendoza, A.; Perea, M.B.; Yañez-Vico, R.M.; Iglesias-Linares, A. Dental Fear in Children: The Role of Previous Negative Dental Experiences. Clin. Oral Investig. 2015, 19, 745–751. [Google Scholar] [CrossRef]
- Cristea, R.A.; Ganea, M.; Potra Cicalău, G.I.; Ciavoi, G. Dentophobia and the Interaction Between Child Patients and Dentists: Anxiety Triggers in the Dental Office. Healthcare 2025, 13, 1021. [Google Scholar] [CrossRef] [PubMed]
- Queiroz, A.M.; Carvalho, A.B.; Censi, L.L.; Cardoso, C.L.; Leite-Panissi, C.R.; Silva, R.A.B.D.; Carvalho, F.K.D.; Nelson-Filho, P.; Silva, L.A.B.D. Prevalence of Dental Anxiety in Children and Adolescents Globally: A Systematic Review with Meta-Analyses. Braz. Dent. J. 2015, 26, 303–307. [Google Scholar] [CrossRef] [PubMed]
- Sérgio Luiz Pinheiro, Camila Silva, Lidiane Luiz, Nubia Silva, Rafaela Fonseca, Thaís Velásquez, Diana Roberta Grandizoli Dog-Assisted Therapy for Control of Anxiety in Pediatric Dentistry. J. Clin. Pediatr. Dent. 2023, 47, 38–43. [CrossRef]
- Smolarek, P.D.C.; Da Silva, L.S.; Martins, P.R.D.; Hartman, K.D.C.; Bortoluzzi, M.C.; Chibinski, A.C.R. Evaluation of Pain, Disruptive Behaviour and Anxiety in Children Aging 5-8 Years Old Undergoing Different Modalities of Local Anaesthetic Injection for Dental Treatment: A Randomised Clinical Trial. Acta Odontol. Scand. 2020, 78, 445–453. [Google Scholar] [CrossRef]
- Agrawal, A.; Rathi, N.V.; Thosar, N.R. A Comparative Evaluation of the Anxiolytic Effect of Oral Midazolam and a Homeopathic Remedy in Children During Dental Treatment. Cureus 2022, 14, e31041. [Google Scholar] [CrossRef]
- Ishan; Shivlingesh, K.K.; Agarwal, V.; Gupta, B.D.; Anand, R.; Sharma, A.; Kushwaha, S.; Khan, K. Anxiety Levels among Five-Year-Old Children Undergoing ART Restoration- A Cross-Sectional Study. J. Clin. Diagn. Res. 2017, 11, ZC45–ZC48. [Google Scholar] [CrossRef]


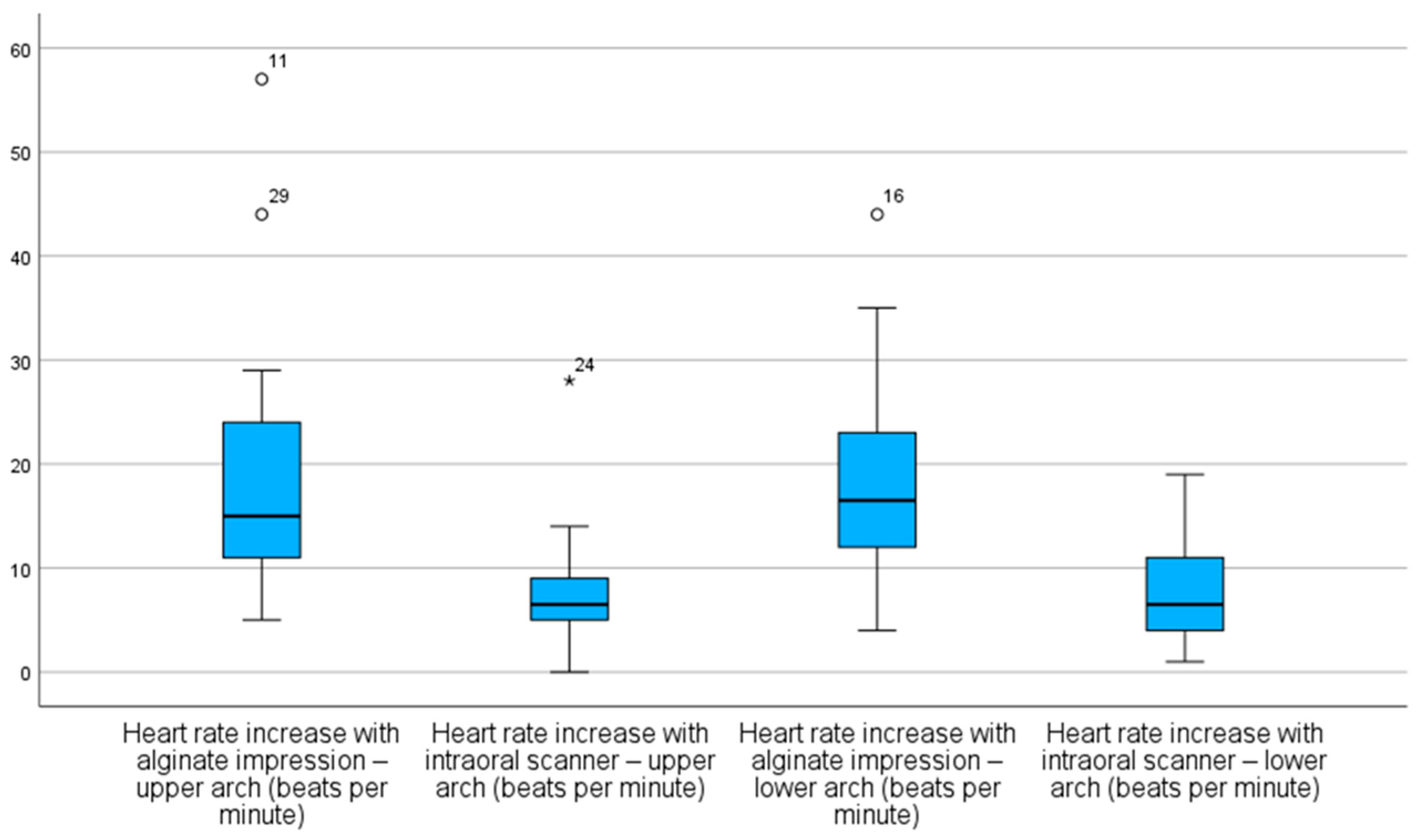
| Impression Method and Arch Type | N | INCR (bpm) (MEAN ± SD) | CI (0.95) |
|---|---|---|---|
| Maxillary Arch—Alginate | 30 | 19 ± 11 | 15–23 |
| Maxillary Arch—Scanner | 30 | 7 ± 5 | 5–9 |
| Mandibular Arch—Alginate | 30 | 18 ± 9 | 15–22 |
| Mandibular Arch–Scanner | 30 | 7 ± 4 | 6–9 |
| Impression Method and Arch Type | N | INCR (%) (MEAN ± SD) | CI (0.95) |
|---|---|---|---|
| Maxillary Arch—Alginate | 30 | −2 ± 2 | −2–(−1) |
| Maxillary Arch—Scanner | 30 | −1 ± 1 | −1–(−1) |
| Mandibular Arch—Alginate | 30 | −2 ± 3 | −2–(−1) |
| Mandibular Arch—Scanner | 30 | −1 ± 1 | −1–0 |
| Impression Method and Arch Type | HR INCR Maxillary Arch (bpm) Alginate | HR INCR Maxillary Arch (bpm) Scanner | HR INCR Mandibular Arch (bpm) Alginate | HR INCR Mandibular Arch (bpm) Scanner |
|---|---|---|---|---|
| HR INCR Maxillary Arch (bpm) Alginate | - | p = 0.004 | - | - |
| HR INCR Maxillary Arch Scanner | - | - | p = 0.004 | - |
| HR INCR Mandibular Arch (bpm) Alginate | - | - | - | p = 0.004 |
| HR INCR Mandibular Arch (bpm) Scanner | p = 0.004 | - | - | - |
| Impression Method and Arch Type | SpO2 INCR Maxillary Arch (%) Alginate | SpO2 INCR Maxillary Arch (%) Scanner | SpO2 INCR Mandibular Arch (%) Alginate | SpO2 INCR Mandibular Arch (%) Scanner |
|---|---|---|---|---|
| SpO2 INCR Maxillary Arch (%) Alginate | - | p = 0.056 | - | - |
| SpO2 INCR Maxillary Arch (%) Scanner | - | - | p = 0.004 | - |
| SpO2 INCR Mandibular Arch (%) Alginate | - | - | - | p = 0.004 |
| SpO2 INCR Mandibular Arch (%) Scanner | p = 0.016 | - | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miranda Ataíde, I.C.; Serna-Muñoz, C.; Ferreira Guimaraes Pereira Areias, C.M.; Ferreira de Azevedo, Á.A.; Pereirinha Henriques Ferreira de Andrade, R.E.; Ortiz-Ruiz, A.J. From Alginate to Pixel: Comparing the Effect of Two Dental Impression Methods on Children’s Anxiety. Children 2025, 12, 866. https://doi.org/10.3390/children12070866
Miranda Ataíde IC, Serna-Muñoz C, Ferreira Guimaraes Pereira Areias CM, Ferreira de Azevedo ÁA, Pereirinha Henriques Ferreira de Andrade RE, Ortiz-Ruiz AJ. From Alginate to Pixel: Comparing the Effect of Two Dental Impression Methods on Children’s Anxiety. Children. 2025; 12(7):866. https://doi.org/10.3390/children12070866
Chicago/Turabian StyleMiranda Ataíde, Isabel Cristina, Clara Serna-Muñoz, Cristina Maria Ferreira Guimaraes Pereira Areias, Álvaro Amadeu Ferreira de Azevedo, Romeu Eduardo Pereirinha Henriques Ferreira de Andrade, and Antonio José Ortiz-Ruiz. 2025. "From Alginate to Pixel: Comparing the Effect of Two Dental Impression Methods on Children’s Anxiety" Children 12, no. 7: 866. https://doi.org/10.3390/children12070866
APA StyleMiranda Ataíde, I. C., Serna-Muñoz, C., Ferreira Guimaraes Pereira Areias, C. M., Ferreira de Azevedo, Á. A., Pereirinha Henriques Ferreira de Andrade, R. E., & Ortiz-Ruiz, A. J. (2025). From Alginate to Pixel: Comparing the Effect of Two Dental Impression Methods on Children’s Anxiety. Children, 12(7), 866. https://doi.org/10.3390/children12070866








