Influence of Sensory Needs on Sleep and Neurodevelopmental Care in At-Risk Neonates
Abstract
1. Introduction
2. Methods
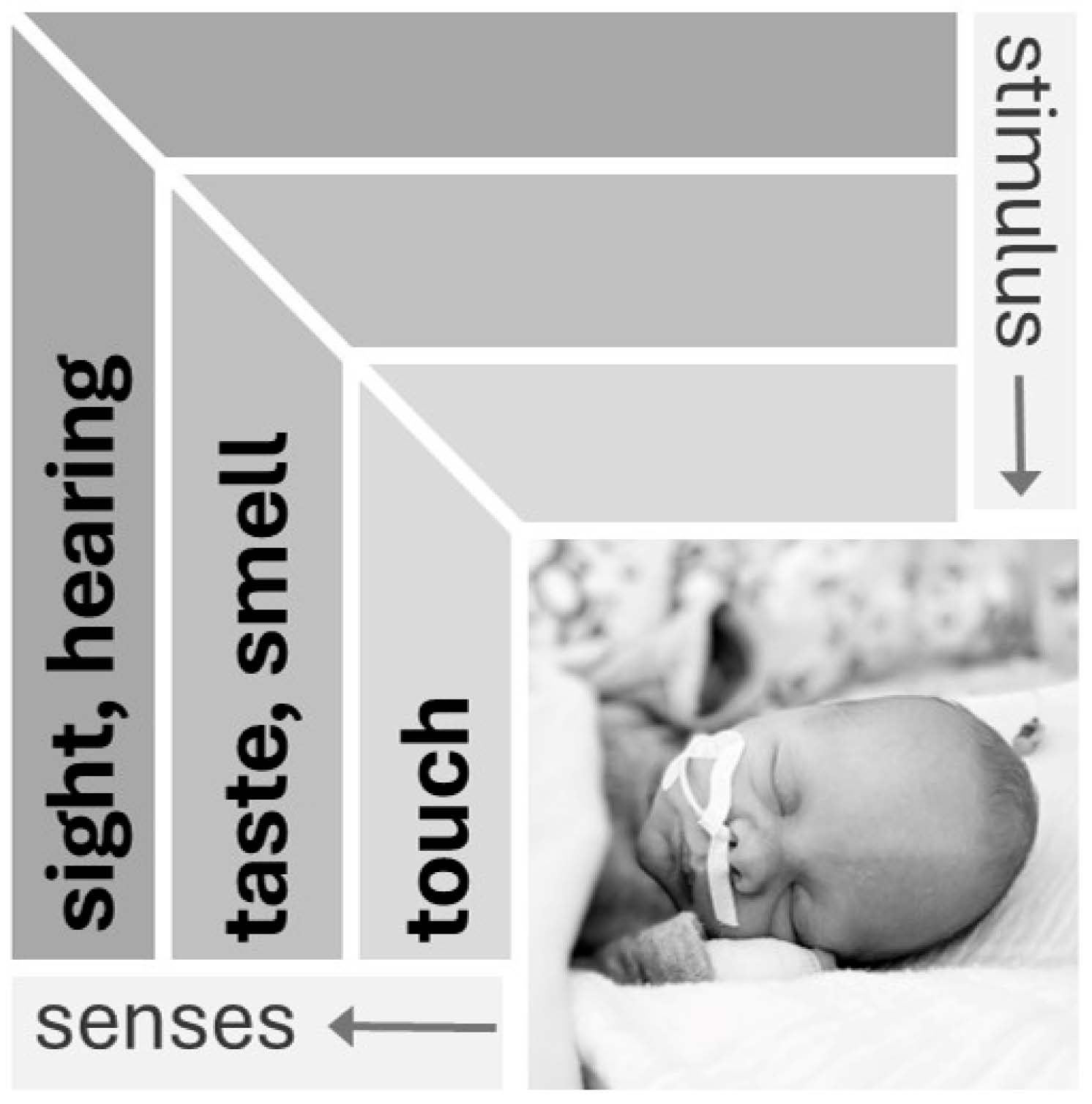
3. Sensory Development and Sensory Environment
| Sensory Modality | Intrauterine (Fetus) | Extrauterine (Premature Infant) |
|---|---|---|
| Touch | Amnion as a protective shell | Direct contact of the immature stratum corneum of the epidermis with the environment |
| Taste | Stimuli are offered via amniotic fluid | Stimuli via teats, disinfectants, care products, different caregivers, food, etc. |
| Smell | Perception of volatile taste components via the amniotic fluid (gustatory smell) | Perception of foreign odors in the air (disinfectants, olfactory signature of the practitioner, food, incubator…); possible toxicity of individual substances |
| Hearing | Perception of predominantly low-frequency sound waves via bone conduction; own mother’s voice is continuously present, external and body sounds of the mother mix | Perception of all frequency ranges via air conduction; background noise includes technical equipment of intensive care medicine and conversations of different people; voice of own mother inconsistently present |
| Sight | Optical input extremely limited; retina and lens developing; functional immaturity of the visual cortex; influence of the mother’s circadian rhythm | Visual environment varies from almost complete darkness to strong brightness; in intensive care, there is little day–night difference; retinal pathology due to high oxygen partial pressure |
4. Postnatal Sleep Characteristics
4.1. Development of Sleep–Dream Cycle and Sleep Stages in the First Weeks
4.2. Sleep Monitoring in the Neonate
4.3. Early SIDS
5. Bonding and Kangaroo Mother Care
6. Sleep Hygiene and Neurodevelopmental Care
| Condition | Suggestion | Practical Aspects |
|---|---|---|
| Lighting conditions | Lighting adapted to the time of day | Light transmission to the visual system is possible even when the eyes are closed Use of moderate daylight during the day and a dark environment at night No direct exposure to light (stress reactions, unphysiological activation) |
| Background noise | Avoiding high noise levels | Limitation of communication directly in the patient’s unit [121] Ensure sufficient rest periods during intensive therapy |
| Parent–infant bond | Spend sleep phases as part of kangaroo care | From the moment of birth, every “small and sick” newborn should remain with mother in immediate and continuous skin-to-skin contact [23] |
| Work organization | Internal ward rules for activities on patients | Day half (“from 8 a.m. to 8 p.m.”): planned interventions Night half (“from 8 p.m. to 8 a.m.”): only regular care Extubation attempts after a longer ventilation should be carried out during the day |
| Nutrition | Promoting breastfeeding | Attention to human milk’s potential to function as a “synchronizer” due to its several bioactive components [119] |
7. Discussion
8. Conclusions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Myers, J.M. Sensory Processing Impacts on Sleep Patterns in Children with Neurodevelopmental Disorders During the COVID-19 Pandemic. Ph.D. Dissertation, Seattle Pacific Library, Seattle, WA, USA, 2023; p. 89. [Google Scholar]
- Morag, I.; Xiao, Y.T.; Bruschettini, M. Cycled light in the intensive care unit for preterm and low birth weight infants. Cochrane Database Syst. Rev. 2024, 2024, CD006982. [Google Scholar]
- Robinson, J.; Fielder, A.R. Light and the neonatal eye. Behav. Brain Res. 1992, 49, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Philbin, M.K. The influence of auditory experience on the behavior of preterm newborns. J. Perinatol. 2000, 20 Pt 2, S77–S87. [Google Scholar] [CrossRef] [PubMed]
- Coston, A.D.; Aune, C. Reducing Noise in the Neonatal Intensive Care Unit. Pediatrics 2019, 144, 154. [Google Scholar] [CrossRef]
- Anand, K.J. Clinical importance of pain and stress in preterm neonates. Biol. Neonate 1998, 73, 1–9. [Google Scholar] [CrossRef]
- Duerden, E.G.; McLean, M.A.; Chau, C.; Guo, T.; Mackay, M.; Chau, V.; Synnes, A.; Miller, S.P.; Grunau, R.E. Neonatal pain, thalamic development and sensory processing behaviour in children born very preterm. Early Hum. Dev. 2022, 170, 105617. [Google Scholar] [CrossRef]
- Weiss, S.J.; Wilson, P. Origins of tactile vulnerability in high-risk infants. Adv. Neonatal Care 2006, 6, 25–36. [Google Scholar] [CrossRef]
- Lebel, V.; Campbell-Yeo, M.; Feeley, N.; Axelin, A. Understanding factors associated with emotional closeness in parents with a preterm infant in the neonatal intensive care unit. Early Hum. Dev. 2022, 173, 105664. [Google Scholar] [CrossRef]
- Mann, P.C.; Stansfield, B.K. Optimal presence: Enhancing parent integration to maximize neurodevelopmental outcomes in preterm infants. Pediatr. Res. 2024, 96, 1445–1453. [Google Scholar] [CrossRef]
- Neugebauer, C.; Oh, W.; Mastergeorge, A.M. Patterns of proximity and maternal-infant engagement in a neonatal intensive care unit. Infant Ment. Health J. 2025, 46, 30–45. [Google Scholar] [CrossRef]
- Alyahya, W.; Simpson, J.; Garcia, A.L.; Mactier, H.; Young, D.; Edwards, C.A. Association between Early Feeding Patterns and Neonatal Outcomes in Very Preterm Infants: A Retrospective Cohort Study. Neonatology 2023, 120, 71–80. [Google Scholar] [CrossRef] [PubMed]
- McClintock, T.; Fiddes, C.; Harris, S.; Embleton, N.; Lin, L.; Bloomfield, F.H.; Muelbert, M. Donor human milk versus infant formula for low-risk infants: A systematic review. Pediatr. Res. 2025, 97, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Strobel, N.A.; Adams, C.; McAullay, D.R.; Edmond, K.M. Mother’s Own Milk Compared with Formula Milk for Feeding Preterm or Low Birth Weight Infants: Systematic Review and Meta-analysis. Pediatrics 2022, 150 (Suppl. 1), e2022057092D. [Google Scholar] [CrossRef]
- Wielek, T.; Del Giudice, R.; Lang, A.; Wislowska, M.; Ott, P.; Schabus, M. On the development of sleep states in the first weeks of life. PLoS ONE 2019, 14, e0224521. [Google Scholar] [CrossRef]
- Freudigman, K.A.; Thoman, E.B. Infant sleep during the first postnatal day: An opportunity for assessment of vulnerability. Pediatrics 1993, 92, 373–379. [Google Scholar]
- Ando, A.; Ohta, H.; Yoshimura, Y.; Nakagawa, M.; Asaka, Y.; Nakazawa, T.; Mitani, Y.; Oishi, Y.; Mizushima, M.; Adachi, H.; et al. Sleep maturation influences cognitive development of preterm toddlers. Sci. Rep. 2021, 11, 15921. [Google Scholar] [CrossRef]
- Figueiredo, S.; Vieira, R. The Effect of Chronotype on Oppositional Behaviour and Psychomotor Agitation of School-Age Children: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 13233. [Google Scholar] [CrossRef]
- Verma, S.; Pinnington, D.; Manber, R.; Bei, B. P153 Sleep timing and chronotype in perinatal periods: Longitudinal changes and associations with wellbeing from pregnancy to 2 years postpartum. Sleep Adv. 2021, 2 (Suppl. 1), A71. [Google Scholar] [CrossRef]
- Pineda, R.G.; Neil, J.; Dierker, D.; Smyser, C.D.; Wallendorf, M.; Kidokoro, H.; Reynolds, L.C.; Walker, S.; Rogers, C.; Mathur, A.M.; et al. Alterations in brain structure and neurodevelopmental outcome in preterm infants hospitalized in different neonatal intensive care unit environments. J. Pediatr. 2014, 164, 52–60.e2. [Google Scholar] [CrossRef]
- Pineda, R.; Kellner, P.; Ibrahim, C.; Smith, J.; SENSE Advisory Team Working Group. Supporting and Enhancing NICU Sensory Experiences (SENSE), 2nd Edition: An Update on Developmentally Appropriate Interventions for Preterm Infants. Children 2023, 10, 961. [Google Scholar] [CrossRef]
- Sibrecht, G.; Wróblewska-Seniuk, K.; Bruschettini, M. Noise or sound management in the neonatal intensive care unit for preterm or very low birth weight infants. Cochrane Database Syst. Rev. 2024, 2024, CD010333. [Google Scholar]
- WHO. Kangaroo Mother Care: Atransformative Innovation in Health Care: Global Position Paper; WHO: Geneva, Switzerland, 2023. [Google Scholar]
- Philbin, M.K.; White, R.D.; Schaal, B.; Hoath, S.B. The Sensory Environment of the Intensive Care Nursery. In Neonatal-Perinatal Medicin; Martin, R.J., Fanaroff, A.A., Walsh, M.C., Eds.; Mosby Elsevier: Philadelphia, PA, USA, 2006; pp. 597–608. [Google Scholar]
- Gottlieb, G. Ontogenesis of sensory function in birds and mammals. In The Biopsychology of Development; Tobach, E., Aronson, L., Shaw, E., Eds.; Academic: New York, NY, USA, 1971; pp. 67–128. [Google Scholar]
- Geva, R.; Feldman, R. A neurobiological model for the effects of early brainstem functioning on the development of behavior and emotion regulation in infants: Implications for prenatal and perinatal risk. J. Child Psychol. Psychiatry 2008, 49, 1031–1041. [Google Scholar] [CrossRef] [PubMed]
- Scammell, T.E.; Arrigoni, E.; Lipton, J.O. Neural Circuitry of Wakefulness and Sleep. Neuron 2017, 93, 747–765. [Google Scholar] [CrossRef]
- Datta, S.; Siwek, D.F.; Stack, E.C. Identification of cholinergic and non-cholinergic neurons in the pons expressing phosphorylated cyclic adenosine monophosphate response element-binding protein as a function of rapid eye movement sleep. Neuroscience 2009, 163, 397–414. [Google Scholar] [CrossRef][Green Version]
- Ninomiya, Y.; Koyama, Y.; Kayama, Y. Postnatal development of choline acetyltransferase activity in the rat laterodorsal tegmental nucleus. Neurosci. Lett. 2001, 308, 138–140. [Google Scholar] [CrossRef]
- Davis, M.R.; Magnusson, J.L.; Cummings, K.J. Increased central cholinergic drive contributes to the apneas of serotonin-deficient rat pups during active sleep. J. Appl. Physiol. 2019, 126, 1175–1183. [Google Scholar] [CrossRef]
- Darnall, R.A.; Schneider, R.W.; Tobia, C.M.; Commons, K.G. Eliminating medullary 5-HT neurons delays arousal and decreases the respiratory response to repeated episodes of hypoxia in neonatal rat pups. J. Appl. Physiol. 2016, 120, 514–525. [Google Scholar] [CrossRef]
- Porges, S.W.; Doussard-Roosevelt, J.A.; Stifter, C.A.; McClenny, B.D.; Riniolo, T.C. Sleep state and vagal regulation of heart period patterns in the human newborn: An extension of the polyvagal theory. Psychophysiology 1999, 36, 14–21. [Google Scholar] [CrossRef]
- Hübler, A. Entwicklung der Schmerzwahrnehmung. In Neonatologie—Die Medizin des Früh- und Reifgeborenen, 2nd ed.; Hübler, A., Jorch, G., Eds.; Thieme: Stuttgart, Germany, 2019; pp. 600–612. [Google Scholar]
- Lagercrantz, H.; Changeux, J.P. The emergence of human consciousness: From fetal to neonatal life. Pediatr. Res. 2009, 65, 255–260. [Google Scholar] [CrossRef]
- Wolf, A.R. Analgesia in the neonate. In Textbook of Neonatology; Rennie, J.M., Roberton, N.R., Eds.; Churchill Livingstonet: London, UK, 1999; pp. 435–441. [Google Scholar]
- Marchal, A.; Melchior, M.; Dufour, A.; Poisbeau, P.; Zores, C.; Kuhn, P. Pain Behavioural Response to Acoustic and Light Environmental Changes in Very Preterm Infants. Children 2021, 8, 1081. [Google Scholar] [CrossRef]
- Koch, S.C.; Fitzgerald, M. Activity-dependent development of tactile and nociceptive spinal cord circuits. Ann. N. Y. Acad. Sci. 2013, 1279, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Hellerud, B.C.; Storm, H. Skin conductance and behaviour during sensory stimulation of preterm and term infants. Early Hum. Dev. 2002, 70, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Goldman, R.D.; Koren, G. Biologic markers of pain in the vulnerable infant. Clin. Perinatol. 2002, 29, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, M.; Millard, C.; MacIntosh, N. Hyperalgesia in premature infants. Lancet 1988, 1, 292. [Google Scholar] [CrossRef]
- Grunau, R.E.; Oberlander, T.F.; Whitfield, M.F.; Fitzgerald, C.; Lee, S.K. Demographic and therapeutic determinants of pain reactivity in very low birth weight neonates at 32 Weeks’ postconceptional Age. Pediatrics 2001, 107, 105–112. [Google Scholar] [CrossRef]
- Pineles, B.L.; Sandman, C.A.; Waffarn, F.; Uy, C.; Davis, E.P. Sensitization of cardiac responses to pain in preterm infants. Neonatology 2007, 91, 190–195. [Google Scholar] [CrossRef]
- Sharma, A.; Sharma, N.; Chahal, A. Navigating the Landscape of Preterm Neonatal Pain: A New Horizon in Sensory Stimulation. J. Clin. Neonatol. 2024, 13, 19–26. [Google Scholar] [CrossRef]
- Hübler, A. Wahrnehmung. In Fetoneonatale Neurologie; Jorch, G., Ed.; Thieme: Stuttgart, Germany; New York, NY, USA, 2013; pp. 60–70. [Google Scholar]
- Bozzette, M. Healthy preterm infant responses to taped maternal voice. J. Perinat. Neonatal. Nurs. 2008, 22, 307–316, quiz 317–318. [Google Scholar] [CrossRef]
- Rivkees, S.A.; Mayes, L.; Jacobs, H.; Gross, I. Rest-activity patterns of premature infants are regulated by cycled lighting. Pediatrics 2004, 113, 833–839. [Google Scholar] [CrossRef]
- Seron-Ferre, M.; Torres-Farfan, C.; Forcelledo, M.L.; Valenzuela, G.J. The development of circadian rhythms in the fetus and neonate. Semin. Perinatol. 2001, 25, 363–370. [Google Scholar] [CrossRef]
- Colonnese, M.T.; Kaminska, A.; Minlebaev, M.; Milh, M.; Bloem, B.; Lescure, S.; Moriette, G.; Chiron, C.; Ben-Ari, Y.; Khazipov, R. A conserved switch in sensory processing prepares developing neocortex for vision. Neuron 2010, 67, 480–498. [Google Scholar] [CrossRef] [PubMed]
- Lickliter, R. Atypical perinatal sensory stimulation and early perceptual development: Insights from developmental psychology. J. Perinatol. 2000, 20, 45. [Google Scholar] [CrossRef] [PubMed]
- Jameie, S.B.; Abdolrahmani, M.; Nobakht, M. Effects of total light deprivation on dorsal lateral geniculate nucleus of male neonate rats. Oman Med. J. 2010, 25, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Barbeau, D.Y.; Weiss, M.D. Sleep Disturbances in Newborns. Children 2017, 4, 90. [Google Scholar] [CrossRef]
- Anders, T.; Emde, R.; Parmelee, A. A Manual of Standardized Terminology, Techniques and Criteria for Scoring States of Sleep and Wakefulness in Newborn Infants; UCLA Brain Information Servie/BRI Publication Office: Los Angeles, CA, USA, 1971. [Google Scholar]
- Scholle, S.; Feldmann-Ulrich, E. Polysomnographischer Atlas der Schlaf-Wach-Stadien im Entwicklungsgang vom Säuglings zum Jugendalter; ecomed Medizin: Heidelberg, Germany, 2012. [Google Scholar]
- Hübler, A. Polysomnographie und Indikationen für Heimmonitoring. In Fetoneonatale Lunge; Hentschel, R., Jorch, G., Eds.; Thieme: Stuttgart, Germany, 2017; pp. 123–132. [Google Scholar]
- Sandyk, R. Melatonin and maturation of REM sleep. Int. J. Neurosci. 1992, 63, 105–114. [Google Scholar] [CrossRef]
- Dos Santos, A.A.; Khan, R.L.; Rocha, G.; Nunes, M.L. Behavior and EEG concordance of active and quiet sleep in preterm very low birth weight and full-term neonates at matched conceptional age. Early Hum. Dev. 2014, 90, 507–510. [Google Scholar] [CrossRef]
- Prechtl, H.F.; Beintema, D.J. Die Neurologische Untersuchung Beim Neugeborenen; Thieme: Stuttgart, Germany, 1971. [Google Scholar]
- Prechtl, H.F.; Theorell, K.; Blair, A.W. Behavioural state cycles in abnormal infants. Dev. Med. Child Neurol. 1973, 15, 606–615. [Google Scholar] [CrossRef]
- Jorch, G. Neurologische Untersuchungstechniken beim Neugeborenen. In Neonatologie—Die Medizin des Früh- und Reifgeborenen; Hübler, A., Jorch, G., Eds.; Thieme: Stuttgart, Germany, 2019; pp. 541–548. [Google Scholar]
- Guyer, C.; Huber, R.; Fontijn, J.; Bucher, H.U.; Nicolai, H.; Werner, H.; Molinari, L.; Latal, B.; Jenni, O.G. Very preterm infants show earlier emergence of 24-hour sleep-wake rhythms compared to term infants. Early Hum. Dev. 2015, 91, 37–42. [Google Scholar] [CrossRef]
- Huang, Y.S.; Paiva, T.; Hsu, J.F.; Kuo, M.C.; Guilleminault, C. Sleep and breathing in premature infants at 6 months post-natal age. BMC Pediatr. 2014, 14, 303. [Google Scholar] [CrossRef]
- Roffwarg, H.P.; Muzio, J.N.; Dement, W.C. Ontogenetic development of the human sleep-dream cycle. Science 1966, 152, 604–619. [Google Scholar] [CrossRef]
- Dereymaeker, A.; Pillay, K.; Vervisch, J.; De Vos, M.; Van Huffel, S.; Jansen, K.; Naulaers, G. Review of sleep-EEG in preterm and term neonates. Early Hum. Dev. 2017, 113, 87–103. [Google Scholar] [CrossRef]
- Ben-Ari, Y.; Gaiarsa, J.L.; Tyzio, R.; Khazipov, R. GABA: A pioneer transmitter that excites immature neurons and generates primitive oscillations. Physiol. Rev. 2007, 87, 1215–1284. [Google Scholar] [CrossRef]
- Vanhatalo, S.; Kaila, K. Development of neonatal EEG activity: From phenomenology to physiology. Semin. Fetal Neonatal Med. 2006, 11, 471–478. [Google Scholar] [CrossRef]
- de Groot, E.R.; Dudink, J.; Austin, T. Sleep as a driver of pre- and postnatal brain development. Pediatr. Res. 2024, 96, 1503–1509. [Google Scholar] [CrossRef]
- Cailleau, L.; Weber, R.; Cabon, S.; Flamant, C.; Roue, J.M.; Favrais, G.; Gascoin, G.; Thollot, A.; Esvan, M.; Poree, F.; et al. Quiet Sleep Organization of Very Preterm Infants Is Correlated with Postnatal Maturation. Front. Pediatr. 2020, 8, 559658. [Google Scholar] [CrossRef]
- Hornig, L.; Szmola, B.; Patzold, W.; Vox, J.P.; Wolf, K.I. Evaluation of Lateral Radar Positioning for Vital Sign Monitoring: An Empirical Study. Sensors 2024, 24, 3548. [Google Scholar] [CrossRef]
- Hübler, A.; Quante, M.; Poets, C. Schlaf beim Neugeborenen. NeonatologieScan 2023, 12, 145–159. [Google Scholar] [CrossRef]
- Brockmann, P.E.; Wiechers, C.; Pantalitschka, T.; Diebold, J.; Vagedes, J.; Poets, C.F. Under-recognition of alarms in a neonatal intensive care unit. Arch. Dis. Child. Fetal Neonatal Ed. 2013, 98, F524–F527. [Google Scholar] [CrossRef]
- de Groot, E.R.; Knoop, M.S.; van den Hoogen, A.; Wang, X.; Long, X.; Pillen, S.; Benders, M.; Dudink, J. The value of cardiorespiratory parameters for sleep state classification in preterm infants: A systematic review. Sleep Med. Rev. 2021, 58, 101462. [Google Scholar] [CrossRef]
- Bohnhorst, B.; Seidel, K.; Bohne, C.; Peter, C.; Pirr, S. Heart rate, respiratory rate, apnoeas and peripheral arterial oxygen saturation in healthy term neonates during quiet sleep. Acta Paediatr. 2019, 108, 231–238. [Google Scholar] [CrossRef]
- Goetz, E.M.; Tomlin, B.D.; Rinaldo, K.E.; Baumann-Blackmore, N.L.; Petro, R.L.; Smith, B.B.; Zapata, J.Y.; Lasarev, M.R.; McBride, E.B.; Kaluarachchi, D.C. Oxygen Saturation Profiles in Healthy Term Infants in Early Postnatal Life. Am. J. Perinatol. 2024, 41, 1269–1274. [Google Scholar] [CrossRef] [PubMed]
- Terrill, P.I.; Dakin, C.; Edwards, B.A.; Wilson, S.J.; MacLean, J.E. A graphical method for comparing nocturnal oxygen saturation profiles in individuals and populations: Application to healthy infants and preterm neonates. Pediatr. Pulmonol. 2018, 53, 645–655. [Google Scholar] [CrossRef] [PubMed]
- Paliwoda, M.; New, K.; Bogossian, F.; Ballard, E. Physiological vital sign reference ranges for well late preterm newborns calculated during a typical 2 h newborn period between 2 h and 7 days of life. Physiol. Meas. 2021, 42, 095001. [Google Scholar] [CrossRef]
- Huizing, M.J.; Villamor-Martinez, E.; Vento, M.; Villamor, E. Pulse oximeter saturation target limits for preterm infants: A survey among European neonatal intensive care units. Eur. J. Pediatr. 2017, 176, 51–56. [Google Scholar] [CrossRef]
- Schmidt, B.; Whyte, R.K. Oxygen saturation target ranges and alarm settings in the NICU: What have we learnt from the neonatal oxygenation prospective meta-analysis (NeOProM)? Semin. Fetal Neonatal Med. 2020, 25, 101080. [Google Scholar] [CrossRef]
- Huizing, M.J.; Hundscheid, T.M.; Bartos, F.; Villamor, E. A Bayesian Reanalysis of the Overall and Sex-Disaggregated Results of the Neonatal Oxygenation Prospective Meta-Analysis (NeOProM). Antioxidants 2024, 13, 509. [Google Scholar] [CrossRef]
- Poets, C.F.; Bohnhorst, B.; Kerst, G. Therapie Idiopathischer Apnoen, Bradykardien und Hypoxämien bei Frühgeborenen; Nr. 024/013(GNPI); AWMF: Frankfurt am Main, Germany, 2020. [Google Scholar]
- Seppa-Moilanen, M.; Andersson, S.; Kirjavainen, T. Supplemental Oxygen Treats Periodic Breathing without Effects on Sleep in Late-Preterm Infants. Neonatology 2022, 119, 567–574. [Google Scholar] [CrossRef]
- Seppa-Moilanen, M.; Andersson, S.; Kirjavainen, T. Monitoring of carbon dioxide in ventilated neonates: A prospective observational study. Arch. Dis. Child. Fetal Neonatal Ed. 2022, 107, 293–298. [Google Scholar]
- Beckwith, J.B. Discussion of terminology and definition of the sudden infant death syndrome. In Sudden Infant Death Syndrome. Proceedings of the Second International Conference of the Causes of the Sudden Death in Infants; Bergman, A.B., Beckwith, J.B., Ray, C.G., Eds.; University of Washington Press: Washington, DC, USA, 1970; pp. 14–22. [Google Scholar]
- de Visme, S.; Chalumeau, M.; Levieux, K.; Patural, H.; Harrewijn, I.; Briand-Huchet, E.; Rey, G.; Morgand, C.; Blondel, B.; Gras-Le Guen, C.; et al. National Variations in Recent Trends of Sudden Unexpected Infant Death Rate in Western Europe. J. Pediatr. 2020, 226, 179–185.e4. [Google Scholar] [CrossRef]
- Kurz, R.; Kerbl, R. SIDS-Definitionen und Klassifikationen. In Der Plötzliche Säuglingstod; Kurz, R., Kenner, T., Poets, C., Kerbl, R., Vennemann, M.M.T., Jorch, G., Eds.; Springer: Wien, Austria, 2014; pp. 23–26. [Google Scholar]
- Poets, A.; Steinfeldt, R.; Poets, C.F. Sudden deaths and severe apparent life-threatening events in term infants within 24 h of birth. Pediatrics 2011, 127, e869–e873. [Google Scholar] [CrossRef]
- Tieder, J.S.; Bonkowsky, J.L.; Etzel, R.A.; Franklin, W.H.; Gremse, D.A.; Herman, B.; Katz, E.S.; Krilov, L.R.; Merritt, J.L., 2nd; Norlin, C.; et al. Brief Resolved Unexplained Events (Formerly Apparent Life-Threatening Events) and Evaluation of Lower-Risk Infants. Pediatrics 2016, 137, e20160590. [Google Scholar] [CrossRef] [PubMed]
- Poets, A.; Urschitz, M.S.; Steinfeldt, R.; Poets, C.F. Risk factors for early sudden deaths and severe apparent life-threatening events. Arch. Dis. Child. Fetal Neonatal Ed. 2012, 97, F395–F397. [Google Scholar] [CrossRef] [PubMed]
- Madar, J.; Roehr, C.C.; Ainsworth, S.; Ersda, H.; Morley, C.; Rüdiger, M.; Skåre, C.; Szczapa, T.; te Pas, A.; Trevisanuto, D.; et al. Versorgung und Reanimation des Neugeborenen nach der Geburt. Notfall + Rettungsmedizin 2021, 24, 603–649. [Google Scholar] [CrossRef]
- Krous, H.F.; Beckwith, J.B.; Byard, R.W.; Rognum, T.O.; Bajanowski, T.; Corey, T.; Cutz, E.; Hanzlick, R.; Keens, T.G.; Mitchell, E.A. Sudden infant death syndrome and unclassified sudden infant deaths: A definitional and diagnostic approach. Pediatrics 2004, 114, 234–238. [Google Scholar] [CrossRef] [PubMed]
- Simma, A.; Potapow, A.; Brandstetter, S.; Michel, H.; Melter, M.; Seelbach-Gobel, B.; Apfelbacher, C.; Kabesch, M.; Gerling, S.; Group, K.K.S. Electrocardiographic Screening in the First Days of Life for Diagnosing Long QT Syndrome: Findings from a Birth Cohort Study in Germany. Neonatology 2020, 117, 756–763. [Google Scholar] [CrossRef]
- Pease, A.S.; Fleming, P.J.; Hauck, F.R.; Moon, R.Y.; Horne, R.S.; L’Hoir, M.P.; Ponsonby, A.L.; Blair, P.S. Swaddling and the Risk of Sudden Infant Death Syndrome: A Meta-analysis. Pediatrics 2016, 137, e20153275. [Google Scholar] [CrossRef]
- Bairoliya, N.; Fink, G. Causes of death and infant mortality rates among full-term births in the United States between 2010 and 2012: An observational study. PLoS Med. 2018, 15, e1002531. [Google Scholar] [CrossRef]
- Moon, R.Y.; Mindell, J.A.; Honaker, S.; Keim, S.; Roberts, K.J.; McAdams, R.J.; McKenzie, L.B. The Tension Between AAP Safe Sleep Guidelines and Infant Sleep. Pediatrics 2024, 153, e2023064675. [Google Scholar] [CrossRef]
- Kenner, T.; Zotter, H. Schlaf, autonome Regulation und Arousals. In Der Plötzliche Säuglingstod; Kurz, H., Kenner, T., Poets, C., Kerbl, R., Vennemann, M.M.T., Jorch, G., Eds.; Springer: Wien, Austria, 2014; pp. 135–154. [Google Scholar]
- Richardson, H.L.; Walker, A.M.; Horne, R.S. Stimulus type does not affect infant arousal response patterns. J. Sleep Res. 2010, 19 Pt 1, 111–115. [Google Scholar] [CrossRef]
- Thiriez, G.; Tournoud, M.; Wermenbol, V.; Vermeylen, D.; Ecochard, R.; Iwaz, J.; Lin, J.S.; Franco, P. Decreased spontaneous arousability in preterm newborns with impaired neurological outcome. J. Sleep Res. 2012, 21, 552–560. [Google Scholar] [CrossRef]
- Richardson, H.L.; Horne, R.S. Arousal from sleep pathways are affected by the prone sleeping position and preterm birth: Preterm birth, prone sleeping and arousal from sleep. Early Hum. Dev. 2013, 89, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Dipietro, J.A. Psychological and psychophysiological considerations regarding the maternal-fetal relationship. Infant Child Dev. 2010, 19, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Odent, M. The instincts of motherhood: Bringing joy back into newborn care. Early Hum. Dev. 2009, 85, 697–700. [Google Scholar] [CrossRef]
- Kennell, J.H.; Trause, M.A.; Klaus, M.H. Evidence for a sensitive period in the human mother. Ciba Found. Symp. 1975, 33, 87–101. [Google Scholar]
- Kostandy, R.R.; Ludington-Hoe, S.M. The evolution of the science of kangaroo (mother) care (skin-to-skin contact). Birth Defects Res. 2019, 111, 1032–1043. [Google Scholar] [CrossRef]
- Rey, E.S.; Martinez, H.G. Manejo racional del niño prematuro. In Curso de Medicina Fetal; Universidad Nacional, Ed.; Universidad Nacional: Bogotá, Colombia, 1983. [Google Scholar]
- Britton, G.R. Early mother-infant contact and infant temperature stabilization. JOGN Nurs. 1980, 9, 84–86. [Google Scholar] [CrossRef]
- Bauer, K.; Uhrig, C.; Sperling, P.; Pasel, K.; Wieland, C.; Versmold, H.T. Body temperatures and oxygen consumption during skin-to-skin (kangaroo) care in stable preterm infants weighing less than 1500 grams. J. Pediatr. 1997, 130, 240–244. [Google Scholar] [CrossRef]
- Boundy, E.O.; Dastjerdi, R.; Spiegelman, D.; Fawzi, W.W.; Missmer, S.A.; Lieberman, E.; Kajeepeta, S.; Wall, S.; Chan, G.J. Kangaroo Mother Care and Neonatal Outcomes: A Meta-analysis. Pediatrics 2016, 137, e20152238. [Google Scholar] [CrossRef]
- Lyngstad, L.T.; Tandberg, B.S.; Storm, H.; Ekeberg, B.L.; Moen, A. Does skin-to-skin contact reduce stress during diaper change in preterm infants? Early Hum. Dev. 2014, 90, 169–172. [Google Scholar] [CrossRef]
- Strand, H.; Blomqvist, Y.T.; Gradin, M.; Nyqvist, K.H. Kangaroo mother care in the neonatal intensive care unit: Staff attitudes and beliefs and opportunities for parents. Acta Paediatr. 2014, 103, 373–378. [Google Scholar] [CrossRef]
- Fernández-Medina, I.M.; Jiménez-Fernández, L.; Solaz-García, Á.J.; Llorca-Porcar, A.; Martínez-Miguel, E.; Collados-Gómez, L. Consensus document for the kangaroo mother care method. An. Pediatr. (Engl. Ed.) 2024, 101, 208–216. [Google Scholar] [CrossRef] [PubMed]
- WHO Immediate KMC Study Group; Arya, S.; Naburi, H.; Kawaza, K.; Newton, S.; Anyabolu, C.H.; Bergman, N.; Rao, S.P.N.; Mittal, P.; Assenga, E.; et al. Immediate “Kangaroo Mother Care” and Survival of Infants with Low Birth Weight. N. Engl. J. Med. 2021, 384, 2028–2038. [Google Scholar] [CrossRef] [PubMed]
- Kristoffersen, L.; Stoen, R.; Bergseng, H.; Flottorp, S.T.; Mageroy, G.; Grunewaldt, K.H.; Aker, K. Immediate Skin-to-Skin Contact in Very Preterm Neonates and Early Childhood Neurodevelopment: A Randomized Clinical Trial. JAMA Netw. Open 2025, 8, e255467. [Google Scholar] [CrossRef]
- Sehgal, A.; Yeomans, E.J.; Nixon, G.M. Kangaroo mother care improves cardiorespiratory physiology in preterm infants: An observational study. Arch. Dis. Child. Fetal Neonatal Ed. 2024, 109, 628–633. [Google Scholar] [CrossRef]
- Johansson, M.W.; Lillieskold, S.; Jonas, W.; Thernstrom Blomqvist, Y.; Skiold, B.; Linner, A. Early skin-to-skin contact and the risk of intraventricular haemorrhage and sepsis in preterm infants. Acta Paediatr. 2024, 113, 1796–1802. [Google Scholar] [CrossRef]
- Zengin, H.; Suzan, O.K.; Hur, G.; Kolukısa, T.; Eroglu, A.; Cinar, N. The effects of kangaroo mother care on physiological parameters of premature neonates in neonatal intensive care unit: A systematic review. J. Pediatr. Nurs. 2023, 71, e18–e27. [Google Scholar] [CrossRef]
- Sivanandan, S.; Sankar, M.J. Kangaroo mother care for preterm or low birth weight infants: A systematic review and meta-analysis. BMJ Glob. Health 2023, 8, e010728. [Google Scholar] [CrossRef]
- Montaner-Ramon, A.; Carrillo-Messa, E.; Merayo-Fernandez, L.; Cosmo-Garcia, I.; Ramos-Soriano, I.; Gonzalez-Garcia, L.; Camba-Longueira, F. Safety of Skin-to-Skin Contact with Umbilical Venous Catheter in Preterm Infants: A Prospective Study. Am. J. Perinatol. 2025, 42, 409–414. [Google Scholar] [CrossRef]
- Kluthe, C.; Wauer, R.R.; Rudiger, M. Extrasystoles: Side effect of kangaroo care? Pediatr. Crit. Care Med. 2004, 5, 455–456. [Google Scholar] [CrossRef]
- Ludington-Hoe, S.M.; Addison, C. Sudden Unexpected Postnatal Collapse: Review and Management. Neonatal Netw. 2024, 43, 76–91. [Google Scholar] [CrossRef]
- Bergman, N.J. New policies on skin-to-skin contact warrant an oxytocin-based perspective on perinatal health care. Front. Psychol. 2024, 15, 1385320. [Google Scholar] [CrossRef]
- Paditz, E. Postnatal Development of the Circadian Rhythmicity of Human Pineal Melatonin Synthesis and Secretion (Systematic Review). Children 2024, 11, 1197. [Google Scholar] [CrossRef] [PubMed]
- Arslanoglu, S.; Bertino, E.; Nicocia, M.; Moro, G.E. WAPM Working Group on Nutrition: Potential chronobiotic role of human milk in sleep regulation. J. Perinat. Med. 2012, 40, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Aubertin, C.; Barrowman, N.; Moreau, K.; Dunn, S.; Harrold, J. Examining the effects of a targeted noise reduction program in a neonatal intensive care unit. Arch. Dis. Child. Fetal Neonatal Ed. 2014, 99, F203–F208. [Google Scholar] [CrossRef]
- Harvey, E. Review of Cycled Lighting’s Effect on Premature Infants’ Circadian Rhythm Development and Clinical Outcomes Based on Gestational Age. Adv. Neonatal Care 2025, 25, 259–269. [Google Scholar] [CrossRef] [PubMed]
- Reuter, C.; Bartha-Doering, L.; Czedik-Eysenberg, I.; Maeder, M.; Bertsch, M.A.; Bibl, K.; Deindl, P.; Berger, A.; Giordano, V. Living in a box: Understanding acoustic parameters in the NICU environment. Front. Pediatr. 2023, 11, 1147226. [Google Scholar] [CrossRef]
- Hawkes, C.P.; Walsh, B.H.; Ryan, C.A.; Dempsey, E.M. Smartphone technology enhances newborn intubation knowledge and performance amongst paediatric trainees. Resuscitation 2013, 84, 223–226. [Google Scholar] [CrossRef]
- Hoffmann, I.M.; Andersen, A.M.; Lund, S.; Nygaard, U.; Joshua, D.; Poulsen, A. Smartphone apps hold promise for neonatal emergency care in low-resource settings. Acta Paediatr. 2024, 113, 2526–2533. [Google Scholar] [CrossRef]
- Okada, J.; Hisano, T.; Unno, M.; Tanaka, Y.; Saikusa, M.; Kinoshita, M.; Harada, E.; Iwata, S.; Iwata, O. Video-call based newborn triage system for local birth centres can be established without major instalment costs using commercially available smartphones. Sci. Rep. 2020, 10, 7552. [Google Scholar] [CrossRef]
- Chandrakanth, P.; Maitra, P.; Sivakumar, P.; Shah, P.K.; Narendran, V. SMART (SMartphone-Assisted frugal Retinopathy of premaTurity screening). Indian J. Ophthalmol. 2023, 71, 3571–3572. [Google Scholar] [CrossRef]
- Sharma, A.; Goyal, A.; Bilong, Y.; Shah, P.; Banker, A.; Kumar, N.; Sharma, R.; Kuppermann, B.D.; Bandello, F. Comparison of a Smartphone-Based Photography Method with Indirect Ophthalmoscopic Assessment in Referable Retinopathy of Prematurity: A Smart Retinopathy of Prematurity Model Pilot Study. Ophthalmol. Retin. 2019, 3, 911–912. [Google Scholar] [CrossRef] [PubMed]
- Ngeow, A.J.H.; Moosa, A.S.; Tan, M.G.; Zou, L.; Goh, M.M.R.; Lim, G.H.; Tagamolila, V.; Ereno, I.; Durnford, J.R.; Cheung, S.K.H.; et al. Development and Validation of a Smartphone Application for Neonatal Jaundice Screening. JAMA Netw. Open 2024, 7, e2450260. [Google Scholar] [CrossRef] [PubMed]
- Ustun, H.; Oncel, M.Y.; Kefeli, M.; Akar, M.; Engur, D. Bilirubin Measurement Through a Smartphone Application in Preterm Infants. Klin. Padiatr. 2023, 235, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Cubero, J.; Narciso, D.; Aparicio, S.; Garau, C.; Valero, V.; Rivero, M.; Esteban, S.; Rial, R.; Rodriguez, A.B.; Barriga, C. Improved circadian sleep-wake cycle in infants fed a day/night dissociated formula milk. Neuro Endocrinol. Lett. 2006, 27, 373–380. [Google Scholar]
- Matin, M.; Brockway, M.; Badejo, A.; Kouroupis, A.; Janke, R.; Keys, E. Effect of biotic supplementation on infant sleep and settling behaviours: A systematic review and meta-analysis. Benef. Microbes 2024, 15, 609–641. [Google Scholar] [CrossRef]
- Als, H. Newborn Individualized Developmental Care and Assessment Program (NIDCAP): An Education and Training Program for Health Care Professionals; NIDCAP Federation International: Woburn, MA, USA, 2000. [Google Scholar]
- Smith, K.; Buehler, D.; Als, H. NIDCAP Nursery Program: Nursery Assessment Manual; NIDCAP Federation International: Woburn, MA, USA, 2011. [Google Scholar]
- Vittner, D.; Butler, S.; Lawhon, g.; Buehler, D. The newborn individualised developmental care and assessment program: A model of care for infants and families in hospital settings. Acta Paediatr. 2025, 114, 743–751. [Google Scholar] [CrossRef]
- Ohlsson, A.; Jacobs, S.E. NIDCAP: A Systematic Review and Meta-analyses of Randomized Controlled Trials. Pediatrics 2013, 131, e881–e893. [Google Scholar] [CrossRef]
- Pineda, R.; Misikoff, M.; Ghahramani, S.; Smith, J.; Mathur, A. Description and evidence on the supporting and enhancing neonatal intensive care unit sensory experiences (SENSE) program. Acta Paediatr. 2025, 114, 731–742. [Google Scholar] [CrossRef]
- Ahlqvist-Björkroth, S.; Feeley, N.; Alberts, J.; Montirosso, R.; Lehtonen, L. Parenting interventions in neonatal intensive care units take different approaches. Acta Paediatr. 2025, 114, 692–694. [Google Scholar] [CrossRef]
| Heart Rate [bpm] 1 | Respiratory Rate [rpm] 2 | Oxygen Saturation [%] | Ref. | |
|---|---|---|---|---|
| Full-term 3 | 87–133 (112) | 32–57 (44) | 94–100 (98) | [72] * |
| Late-preterm 4 | 102–164 | 15–67 | 94–100 | [75] ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hübler, A. Influence of Sensory Needs on Sleep and Neurodevelopmental Care in At-Risk Neonates. Children 2025, 12, 781. https://doi.org/10.3390/children12060781
Hübler A. Influence of Sensory Needs on Sleep and Neurodevelopmental Care in At-Risk Neonates. Children. 2025; 12(6):781. https://doi.org/10.3390/children12060781
Chicago/Turabian StyleHübler, Axel. 2025. "Influence of Sensory Needs on Sleep and Neurodevelopmental Care in At-Risk Neonates" Children 12, no. 6: 781. https://doi.org/10.3390/children12060781
APA StyleHübler, A. (2025). Influence of Sensory Needs on Sleep and Neurodevelopmental Care in At-Risk Neonates. Children, 12(6), 781. https://doi.org/10.3390/children12060781






