Efficacy of Intravascular Therapeutic Hypothermia for Moderate to Severe Hypoxic–Ischemic Encephalopathy
Abstract
1. Introduction
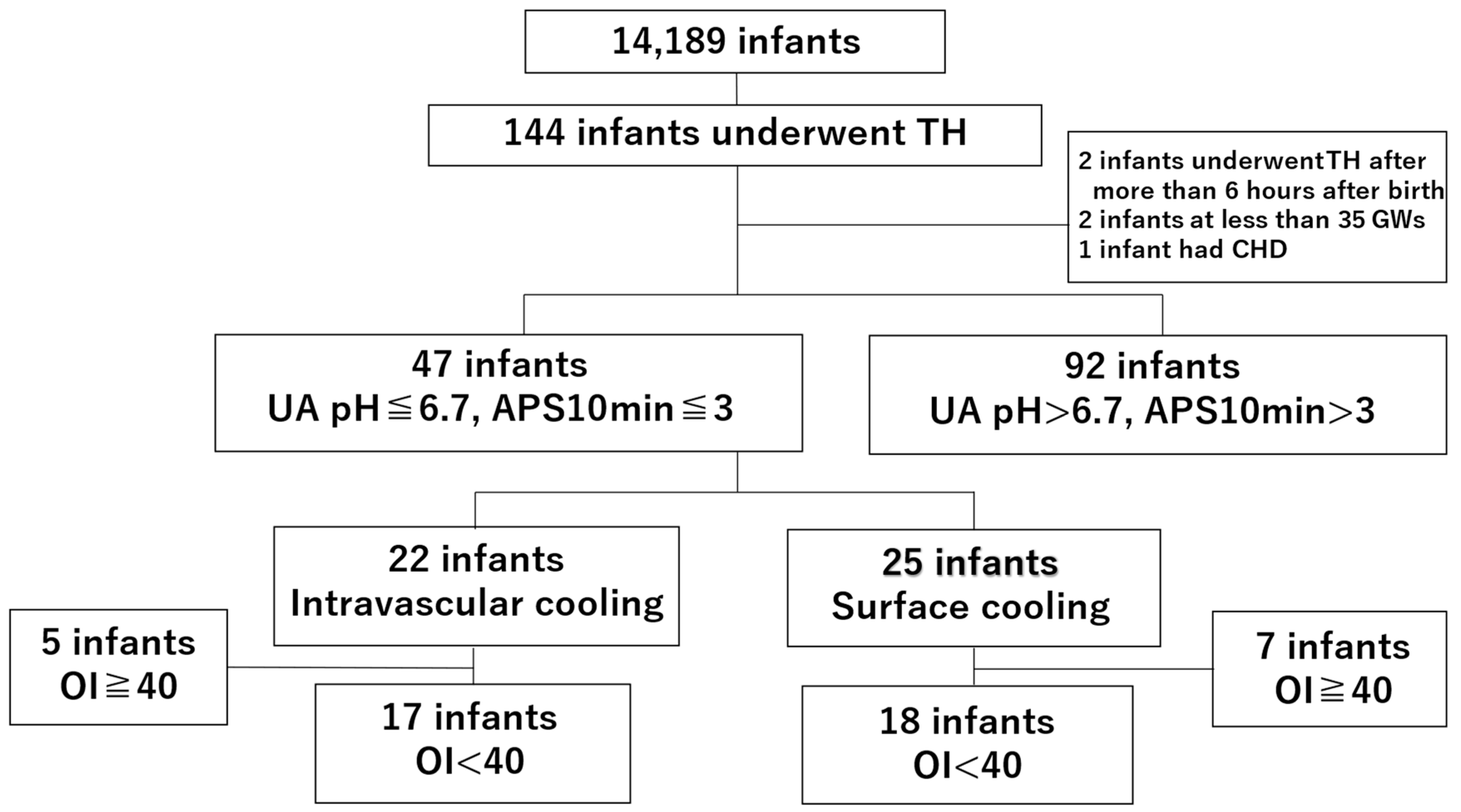
2. Materials and Methods
2.1. Study Outline and Target Group
2.2. Inclusion and Exclusion Criteria
2.3. Study Groups
2.4. Conventional Therapeutic Hypothermia (Surface Cooling Method)
2.5. Intravascular Therapeutic Hypothermia (Intravascular Cooling with ECMO)
2.6. Blood Sample pH ≤ 6.7 Within 60 min After Birth and 10 min Apgar Score ≤ 3
2.7. Data Collection
2.8. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kurinczuk, J.J.; White-Koning, M.; Badawi, N. Epidemiology of neonatal encephalopathy and hypoxic-ischaemic encephalopathy. Early Hum. Dev. 2010, 86, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Gluckman, P.D.; Wyatt, J.S.; Azzopardi, D.; Ballard, R.; Edwards, A.D.; Ferriero, D.M.; Polin, R.A.; Robertson, C.M.; Thoresen, M.; Whitelaw, A.; et al. Selective head cooling with mild systemic hypothermia after neonatal encephalopathy: Multicentre randomised trial. Lancet 2005, 365, 663–670. [Google Scholar] [CrossRef]
- Shankaran, S.; Pappas, A.; McDonald, S.A.; Vohr, B.R.; Hintz, S.R.; Yolton, K.; Gustafson, K.E.; Leach, T.M.; Green, C.; Bara, R.; et al. Childhood outcomes after hypothermia for neonatal encephalopathy. N. Engl. J. Med. 2012, 366, 2085–2092. [Google Scholar] [CrossRef] [PubMed]
- Azzopardi, D.; Strohm, B.; Linsell, L.; Hobson, A.; Juszczak, E.; Kurinczuk, J.J.; Brocklehurst, P.; Edwards, A.D.; UK TOBY Cooling Register. Implementation and conduct of therapeutic hypothermia for perinatal asphyxial encephalopathy in the UK—Analysis of national data. PLoS ONE 2012, 7, e38504. [Google Scholar] [CrossRef] [PubMed]
- Tsuda, K.; Mukai, T.; Iwata, S.; Shibasaki, J.; Tokuhisa, T.; Ioroi, T.; Sano, H.; Yutaka, N.; Takahashi, A.; Takeuchi, A.; et al. Therapeutic hypothermia for neonatal encephalopathy: A report from the first 3 years of the Baby Cooling Registry of Japan. Sci. Rep. 2017, 7, 39508. [Google Scholar] [CrossRef]
- Wayock, C.P.; Meserole, R.L.; Saria, S.; Jennings, J.M.; Huisman, T.A.; Northington, F.J.; Graham, E.M. Perinatal risk factors for severe injury in neonates treated with whole-body hypothermia for encephalopathy. Am. J. Obstet. Gynecol. 2014, 211, 41.e1–41.e8. [Google Scholar] [CrossRef]
- Goodwin, T.M.; Belai, I.; Hernandez, P.; Durand, M.; Paul, R.H. Asphyxial complications in the term newborn with severe umbilical acidemia. Am. J. Obstet. Gynecol. 1992, 167, 1506–1512. [Google Scholar] [CrossRef]
- Natarajan, G.; Shankaran, S.; Laptook, A.R.; Pappas, A.; Bann, C.M.; McDonald, S.A.; Das, A.; Higgins, R.D.; Hintz, S.R.; Vohr, B.R.; et al. Apgar scores at 10 min and outcomes at 6–7 years following hypoxic-ischaemic encephalopathy. Arch. Dis. Child. Fetal. Neonatal Ed. 2013, 98, F473–F479. [Google Scholar] [CrossRef]
- Lakshminrusimha, S.; Shankaran, S.; Laptook, A.; McDonald, S.; Keszler, M.; Van Meurs, K.; Guillet, R.; Chawla, S.; Sood, B.G.; Bonifacio, S.; et al. Pulmonary hypertension associated with hypoxic-ischemic encephalopathy—Antecedent characteristics and comorbidities. J. Pediatr. 2018, 196, 45–51.e3. [Google Scholar] [CrossRef]
- Azzopardi, D.; TOBY Study Group. Predictive value of the amplitude integrated EEG in Infants with hypoxic ischaemic encephalopathy: Data from a randomised trial of therapeutic hypothermia. Arch. Dis. Child. Fetal. Neonatal Ed. 2014, 99, F80–F82. [Google Scholar] [CrossRef]
- Azzopardi, D.V.; Strohm, B.; Edwards, A.D.; Dyet, L.; Halliday, H.L.; Juszczak, E.; Kapellou, O.; Levene, M.; Marlow, N.; Porter, E.; et al. Moderate hypothermia to treat perinatal asphyxial encephalopathy. N. Engl. J. Med. 2009, 361, 1349–1358. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, R.E.; Roloff, D.W.; Chapman, R.; Snedecor, S.; Bartlett, R.H. Extracorporeal membrane oxygenation in term newborns. A prospective cost-benefit analysis. ASAIO J. 1993, 39, 873–879. [Google Scholar] [CrossRef]
- Matsushita, Y. The Kyoto Scale of Psychological Development Test, 2001; Matsushita, Y., Gohma, H., Eds.; Nakanishiya Shuppan: Kyoto, Japan, 2008; pp. 25–46. (In Japanese) [Google Scholar]
- Maehara, T.; Shimizu, H.; Kawai, K.; Shigetomo, R.; Tamagawa, K.; Yamada, T.; Inoue, M. Postoperative development of children after hemispherotomy. Brain Dev. 2002, 24, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Tokuhisa, T.; Ibara, S.; Minakami, H.; Maede, Y.; Ishihara, C.; Matsui, T. Outcome of infants with hypoxic ischemic encephalopathy treated with brain hypothermia. J. Obstet. Gynecol. Res. 2015, 41, 229–237. [Google Scholar] [CrossRef]
- Macones, G.A.; Hankins, G.D.; Spong, C.Y.; Hauth, J.; Moore, T. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: Update on definitions, interpretation, and research guidelines. J. Obstet. Gynecol. Neonatal Nurs. 2008, 37, 510–515. [Google Scholar] [CrossRef] [PubMed]
- Kubli, F.W.; Hon, E.H.; Khazin, A.F.; Takemura, H. Observations on heart rate and pH in the human fetus during labor. Am. J. Obstet. Gynecol. 1969, 104, 1190–1206. [Google Scholar] [CrossRef]
- Okai, T.; Ikeda, T.; Kawarabayashi, T.; Kozuma, S.; Sugawara, J.; Chisaka, H.; Yoneda, S.; Matsuoka, R.; Nakano, H.; Okamura, K.; et al. Intrapartum management guidelines based on fetal heart rate pattern classification. J. Obstet. Gynaecol. Res. 2010, 36, 925–928. [Google Scholar] [CrossRef]
- Goldenberg, R.L.; Culhane, J.F.; Iams, J.D.; Romero, R. Epidemiology and causes of preterm birth. Lancet 2008, 371, 75–84. [Google Scholar] [CrossRef]
- Field, D.; Juszczak, E.; Linsell, L.; Azzopardi, D.; Cowan, F.; Marlow, N.; Edwards, D.; NEST Study Collaborative Group. Neonatal ECMO study of temperature (NEST): A randomized controlled trial. Pediatrics 2013, 132, e1247–e1256. [Google Scholar] [CrossRef]
- Cuevas Guaman, M.; Lucke, A.M.; Hagan, J.L.; Kaiser, J.R. Bleeding complications and mortality in neonates receiving therapeutic hypothermia and extracorporeal membrane oxygenation. Am. J. Perinatol. 2018, 35, 271–276. [Google Scholar]
- Agarwal, P.; Altinok, D.; Desai, J.; Shanti, C.; Natarajan, G. In-hospital outcomes of neonates with hypoxic-ischemic encephalopathy receiving extracorporeal membrane oxygenation. J. Perinatol. 2019, 39, 661–665. [Google Scholar] [CrossRef] [PubMed]
- de Waard, M.C.; Banwarie, R.P.; Jewbali, L.S.; Struijs, A.; Girbes, A.R.; Groeneveld, A.B. Intravascular versus surface cooling speed and stability after cardiopulmonary resuscitation. Emerg. Med. J. 2015, 32, 775–780. [Google Scholar] [CrossRef] [PubMed]
- Hoedemaekers, C.W.; Ezzahti, M.; Gerritsen, A.; van der Hoeven, J.G. Comparison of cooling methods to induce and maintain normo- and hypothermia in intensive care unit patients: A prospective intervention study. Crit. Care 2007, 11, R91. [Google Scholar] [CrossRef] [PubMed]
| Intravascular TH (% or IQR) | Conventional TH (% or IQR) | p Value | |
|---|---|---|---|
| 17 (48.6) | 18 (51.4) | ||
| Birth weight (g) | 2830 (2677–3081) | 2923 (2559–326) | 0.87 |
| GWs | 39 (38–40) | 38 (37–40) | 0.49 |
| Sex (male) | 10 (58.8) | 9 (50.0) | 0.74 |
| Twin | 1 (5.9) | 0 | 0.49 |
| Out-of-hospital birth | 17 (100.0) | 17 (94.4) | 1 |
| Maternal age (years) | 36 (27–37) | 31.5 (28–35) | 0.42 |
| Primipara | 10 (58.8) | 11 (61.1) | 1 |
| PROM | 2 (11.8) | 1 (5.6) | 0.6 |
| HDP | 1 (5.9) | 3 (16.7) | 0.6 |
| GDM | 0 | 2 (11.1) | 0.49 |
| HELLP | 0 | 0 | |
| CAM | 1 (5.9) | 0 | 0.49 |
| Funisitis | 1 (5.9) | 0 | 0.49 |
| Fertility treatment | 0 | 0 | |
| C/S | 8 (47.1) | 16 (88.9) | 0.01 |
| Cervical os bleeding | 1 (5.9) | 2 (11.1) | 1 |
| Placental abruption | 10 (58.8) | 9 (50.0) | 0.74 |
| Shoulder dystocia | 1 (5.9) | 0 | 0.49 |
| Umbilical cord prolapse | 3 (17.6) | 1 (5.6) | 0.34 |
| Protracted labor | 2 (11.8) | 1 (5.6) | 0.6 |
| Malpresentation | 0 | 1 (5.6) | 1 |
| Ineffective uterine contractions | 2 (11.8) | 0 | 0.23 |
| Soft-tissue dystocia | 1 (5.9) | 0 | 0.49 |
| Uterine rupture | 0 | 1 (5.6) | 1 |
| Umbilical injury | 1 (5.9) | 0 | 0.49 |
| NRFS | 17 (100.0) | 16 (88.9) | 0.49 |
| Severe V/Ds | 4 (23.5) | 4 (22.2) | 1 |
| Recurrent L/Ds | 6 (35.3) | 4 (22.2) | 0.47 |
| Severe P/Ds | 6 (35.3) | 1 (5.6) | 0.04 |
| Bradycardia | 12 (70.6) | 6 (33.3) | 0.04 |
| Loss of variability | 5 (29.4) | 2 (11.1) | 0.23 |
| Apgar, 1 min | 1 (1–2) | 1 (0–2) | 0.89 |
| Apgar, 5 min | 2 (1–3) | 3 (1–4) | 0.28 |
| Apgar, 10 min | 2 (1–4) | 3 (2–5) | 0.17 |
| UA pH | 6.67 (6.66–6.99) | 6.68 (6.57–6.90) | 0.41 |
| UA BE | −22.6 (−25.0–−14.6) | −19.6 (−25.7–−13.9) | 0.64 |
| Chest compressions (resuscitation) | 10 (58.8) | 8 (44.4) | 0.5 |
| Intubation (resuscitation) | 16 (94.1) | 12 (66.7) | 0.09 |
| Adrenaline (resuscitation) | 4 (23.5) | 6 (33.3) | 0.71 |
| Flat, low voltage (aEEG) | 9 (52.9) | 9 (50.0) | 1 |
| Severe HIE | 12 (70.6) | 11 (61.1) | 0.72 |
| Moderate HIE | 5 (29.4) | 7 (38.9) | 0.72 |
| Convulsion | 7 (41.2) | 8 (44.4) | 1 |
| IVH (II–III) | 2 (11.8) | 3 (16.7) | 1 |
| ICH | 1 (5.9) | 1 (5.6) | 1 |
| MAS | 3 (17.6) | 1 (5.6) | 0.34 |
| Sepsis | 0 | 1 (5.6) | 1 |
| Inhaled NO | 3 (17.6) | 1 (5.6) | 0.34 |
| CHDF | 2 (11.8) | 2 (11.1) | 1 |
| Adrenaline | 6 (35.3) | 8 (44.4) | 0.73 |
| DOA | 15 (88.2) | 17 (94.4) | 0.6 |
| DOB | 10 (58.8) | 12 (66.7) | 0.73 |
| DQ ≥ 70 | 12 (70.6) | 6 (33.3) | 0.04 |
| DQ ≥ 85 | 7 (41.2) | 4 (22.2) | 0.29 |
| Mortality | 1 (5.9) | 1 (5.6) | 1 |
| During hospitalization | 59 (36–179.5) | 44 (28.3–312.3) | 0.48 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kurimoto, T.; Tokuhisa, T.; Hayasaka, I.; Yamamoto, T.; Hirakawa, E.; Ohashi, H.; Kibe, M.; Yara, A.; Maeda, T.; Kamitomo, M.; et al. Efficacy of Intravascular Therapeutic Hypothermia for Moderate to Severe Hypoxic–Ischemic Encephalopathy. Children 2025, 12, 605. https://doi.org/10.3390/children12050605
Kurimoto T, Tokuhisa T, Hayasaka I, Yamamoto T, Hirakawa E, Ohashi H, Kibe M, Yara A, Maeda T, Kamitomo M, et al. Efficacy of Intravascular Therapeutic Hypothermia for Moderate to Severe Hypoxic–Ischemic Encephalopathy. Children. 2025; 12(5):605. https://doi.org/10.3390/children12050605
Chicago/Turabian StyleKurimoto, Tomonori, Takuya Tokuhisa, Itaru Hayasaka, Tsuyoshi Yamamoto, Eiji Hirakawa, Hiroshi Ohashi, Masaya Kibe, Asataro Yara, Takatsugu Maeda, Masato Kamitomo, and et al. 2025. "Efficacy of Intravascular Therapeutic Hypothermia for Moderate to Severe Hypoxic–Ischemic Encephalopathy" Children 12, no. 5: 605. https://doi.org/10.3390/children12050605
APA StyleKurimoto, T., Tokuhisa, T., Hayasaka, I., Yamamoto, T., Hirakawa, E., Ohashi, H., Kibe, M., Yara, A., Maeda, T., Kamitomo, M., & Ibara, S. (2025). Efficacy of Intravascular Therapeutic Hypothermia for Moderate to Severe Hypoxic–Ischemic Encephalopathy. Children, 12(5), 605. https://doi.org/10.3390/children12050605





