Characteristics, Outcomes and Mortality Risk Factors of Pediatric In-Hospital Cardiac Arrest in Western China: A Retrospective Study Using Utstein Style
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection and Outcomes
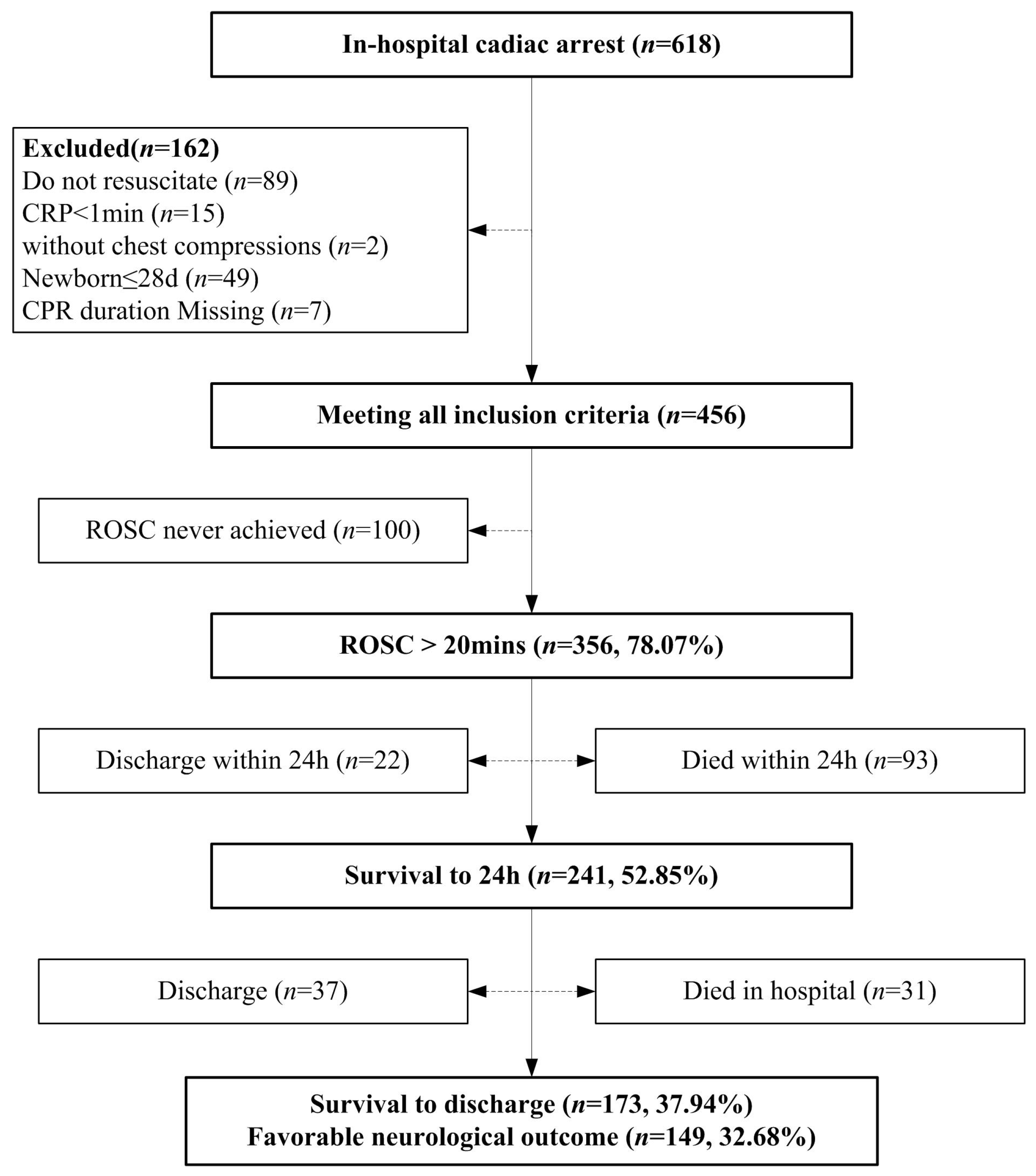
2.3. Inclusion and Exclusion Criteria
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CA | Cardiac arrest |
| IHCA | In-hospital cardiac arrest |
| OHCA | Out-of-hospital cardiac arrest |
| ROSC | Return of spontaneous circulation |
| CPR | Cardiopulmonary resuscitation |
| ECPR | Extracorporeal cardiopulmonary resuscitation |
| WLST | Withdrawal of life sustaining therapy |
| DNR | Do not resuscitate |
| ECMO | Extracorporeal membrane oxygenation |
| AHA | American Heart Association |
| GWTG | Get With The Guidelines |
| PCPC | Pediatric cerebral performance category |
| PICU | Pediatric intensive care unit |
| CICU | Cardiac surgery intensive care unit |
| BMV | Bag-mask ventilation |
| ETI | Endotracheal intubation |
| PEA | Pulseless electrical activity |
| VF | Ventricular fibrillation |
| pVT | Pulseless ventricular tachycardia |
| Neuro | Neurological |
| OR | Odds ratio |
| CI | Confidence interval |
| BLS | Basic Life Support |
| PALS | Pediatric Advanced Life Support |
References
- Holmberg, M.J.; Ross, C.E.; Fitzmaurice, G.M.; Chan, P.S.; Duval-Arnould, J.; Grossestreuer, A.V.; Yankama, T.; Donnino, M.W.; Andersen, L.W. Annual Incidence of Adult and Pediatric In-Hospital Cardiac Arrest in the United States. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005580. [Google Scholar] [CrossRef]
- Berg, R.A.; Nadkarni, V.M.; Clark, A.E.; Moler, F.; Meert, K.; Harrison, R.E.; Newth, C.J.; Sutton, R.M.; Wessel, D.L.; Berger, J.T.; et al. Incidence and Outcomes of Cardiopulmonary Resuscitation in PICUs. Crit. Care Med. 2016, 44, 798–808. [Google Scholar] [CrossRef] [PubMed]
- Alten, J.A.; Klugman, D.; Raymond, T.T.; Cooper, D.S.; Donohue, J.E.; Zhang, W.; Pasquali, S.K.; Gaies, M.G. Epidemiology and Outcomes of Cardiac Arrest in Pediatric Cardiac ICUs. Pediatr. Crit. Care Med. 2017, 18, 935–943. [Google Scholar] [CrossRef]
- Zeng, J.; Qian, S.; Zheng, M.; Wang, Y.; Zhou, G.; Wang, H. The epidemiology and resuscitation effects of cardiopulmonary arrest among hospitalized children and adolescents in Beijing: An observational study. Resuscitation 2013, 84, 1685–1690. [Google Scholar] [CrossRef] [PubMed]
- Reis, A.G.; Nadkarni, V.; Perondi, M.B.; Grisi, S.; Berg, R.A. A prospective investigation into the epidemiology of in-hospital pediatric cardiopulmonary resuscitation using the international Utstein reporting style. Pediatrics 2002, 109, 200–209. [Google Scholar] [CrossRef]
- Suominen, P.; Olkkola, K.T.; Voipio, V.; Korpela, R.; Palo, R.; Räsänen, J. Utstein style reporting of in-hospital paediatric cardiopulmonary resuscitation. Resuscitation 2000, 45, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Holmberg, M.J.; Wiberg, S.; Ross, C.E.; Kleinman, M.; Hoeyer-Nielsen, A.K.; Donnino, M.W.; Andersen, L.W. Trends in Survival After Pediatric In-Hospital Cardiac Arrest in the United States. Circulation 2019, 140, 1398–1408. [Google Scholar] [CrossRef]
- Martin, S.S.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Barone Gibbs, B.; Beaton, A.Z.; Boehme, A.K.; et al. Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Circulation 2024, 149, e347–e913. [Google Scholar] [CrossRef]
- Girotra, S.; Spertus, J.A.; Li, Y.; Berg, R.A.; Nadkarni, V.M.; Chan, P.S. Survival trends in pediatric in-hospital cardiac arrests: An analysis from Get With the Guidelines Resuscitation. Circ. Cardiovasc. Qual. Outcomes 2013, 6, 42–49. [Google Scholar] [CrossRef]
- López-Herce, J.; Del Castillo, J.; Matamoros, M.; Cañadas, S.; Rodriguez-Calvo, A.; Cecchetti, C.; Rodriguez-Núñez, A.; Alvarez, A.C. Factors associated with mortality in pediatric in-hospital cardiac arrest: A prospective multicenter multinational observational study. Intensive Care Med. 2013, 39, 309–318. [Google Scholar] [CrossRef]
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics-2020 Update: A Report from the American Heart Association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef] [PubMed]
- Berg, R.A.; Sutton, R.M.; Reeder, R.W.; Berger, J.T.; Newth, C.J.; Carcillo, J.A.; McQuillen, P.S.; Meert, K.L.; Yates, A.R.; Harrison, R.E.; et al. Association Between Diastolic Blood Pressure During Pediatric In-Hospital Cardiopulmonary Resuscitation and Survival. Circulation 2018, 137, 1784–1795. [Google Scholar] [CrossRef] [PubMed]
- Nadkarni, V.M.; Larkin, G.L.; Peberdy, M.A.; Carey, S.M.; Kaye, W.; Mancini, M.E.; Nichol, G.; Lane-Truitt, T.; Potts, J.; Ornato, J.P.; et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA 2006, 295, 50–57. [Google Scholar] [CrossRef]
- Samson, R.A.; Nadkarni, V.M.; Meaney, P.A.; Carey, S.M.; Berg, M.D.; Berg, R.A. Outcomes of in-hospital ventricular fibrillation in children. N. Engl. J. Med. 2006, 354, 2328–2339. [Google Scholar] [CrossRef] [PubMed]
- Matos, R.I.; Watson, R.S.; Nadkarni, V.M.; Huang, H.H.; Berg, R.A.; Meaney, P.A.; Carroll, C.L.; Berens, R.J.; Praestgaard, A.; Weissfeld, L.; et al. Duration of cardiopulmonary resuscitation and illness category impact survival and neurologic outcomes for in-hospital pediatric cardiac arrests. Circulation 2013, 7, 442–451. [Google Scholar] [CrossRef]
- Topjian, A.A.; de Caen, A.; Wainwright, M.S.; Abella, B.S.; Abend, N.S.; Atkins, D.L.; Bembea, M.M.; Fink, E.L.; Guerguerian, A.M.; Haskell, S.E.; et al. Pediatric Post-Cardiac Arrest Care: A Scientific Statement from the American Heart Association. Circulation 2019, 140, e194–e233. [Google Scholar] [CrossRef]
- Wang, C.; Zheng, W.; Zheng, J.; Shao, F.; Zhu, Y.; Li, C.; Ma, Y.; Tan, H.; Yan, S.; Han, X.; et al. A national effort to improve outcomes for in-hospital cardiac arrest in China: The BASeline Investigation of Cardiac Arrest (BASIC-IHCA). Resusc. Plus 2022, 11, 100259. [Google Scholar] [CrossRef]
- Zheng, J.; Lv, C.; Zheng, W.; Zhang, G.; Tan, H.; Ma, Y.; Zhu, Y.; Li, C.; Han, X.; Yan, S.; et al. Incidence, process of care, and outcomes of out-of-hospital cardiac arrest in China: A prospective study of the BASIC-OHCA registry. Lancet Public Health 2023, 8, e923–e932. [Google Scholar] [CrossRef]
- Zhao, X.; Zheng, W.; Ma, Y.; Hou, Y.; Zhu, Y.; Zheng, J.; Wang, Q.; Pan, C.; Zhang, J.; Wang, C.; et al. Epidemiology, Process of Care, and Associated Outcomes of Pediatric Out-of-Hospital Cardiac Arrest in China: Results from a Prospective, Multicenter, Population-Based Registry. Crit. Care Med. 2024, 52, e604–e615. [Google Scholar] [CrossRef]
- Nolan, J.P.; Berg, R.A.; Andersen, L.W.; Bhanji, F.; Chan, P.S.; Donnino, M.W.; Lim, S.H.; Ma, M.H.; Nadkarni, V.M.; Starks, M.A.; et al. Cardiac Arrest and Cardiopulmonary Resuscitation Outcome Reports: Update of the Utstein Resuscitation Registry Template for In-Hospital Cardiac Arrest: A Consensus Report from a Task Force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia). Resuscitation 2019, 144, 166–177. [Google Scholar] [CrossRef]
- Fiser, D.H.; Long, N.; Roberson, P.K.; Hefley, G.; Zolten, K.; Brodie-Fowler, M. Relationship of pediatric overall performance category and pediatric cerebral performance category scores at pediatric intensive care unit discharge with outcome measures collected at hospital discharge and 1- and 6-month follow-up assessments. Crit. Care Med. 2000, 28, 2616–2620. [Google Scholar] [CrossRef] [PubMed]
- Del Castillo, J.; López-Herce, J.; Cañadas, S.; Matamoros, M.; Rodríguez-Núnez, A.; Rodríguez-Calvo, A.; Carrillo, A. Cardiac arrest and resuscitation in the pediatric intensive care unit: A prospective multicenter multinational study. Resuscitation 2014, 85, 1380–1386. [Google Scholar] [CrossRef]
- Gaies, M.G.; Clarke, N.S.; Donohue, J.E.; Gurney, J.G.; Charpie, J.R.; Hirsch, J.C. Personnel and unit factors impacting outcome after cardiac arrest in a dedicated pediatric cardiac intensive care unit. Pediatr. Crit. Care Med. 2012, 13, 583–588. [Google Scholar] [CrossRef] [PubMed]
- López-Herce, J.; del Castillo, J.; Cañadas, S.; Rodríguez-Núñez, A.; Carrillo, A. Spanish Study Group of Cardiopulmonary Arrest in Children. In-hospital pediatric cardiac arrest in Spain. Rev. Esp. Cardiol. 2014, 67, 189–195. [Google Scholar] [CrossRef]
- Kwon, I.H.; Choi, Y. Analysis of characteristics and trends of the in-hospital cardiac arrest incidence in the Republic of Korea: Clinical usefulness of national health insurance claim data. Signa Vitae 2021, 7, 196–205. [Google Scholar] [CrossRef]
- Hamzah, M.; Othman, H.F.; Almasri, M.; Al-Subu, A.; Lutfi, R. Survival outcomes of in-hospital cardiac arrest in pediatric patients in the USA. Eur. J. Pediatr. 2021, 180, 2513–2520. [Google Scholar] [CrossRef]
- Morgan, R.W.; Kirschen, M.P.; Kilbaugh, T.J.; Sutton, R.M.; Topjian, A.A. Pediatric In-Hospital Cardiac Arrest and Cardiopulmonary Resuscitation in the United States: A Review. JAMA Pediatr. 2021, 175, 293–302. [Google Scholar] [CrossRef]
- Schleien, C.L. Pediatric cardiopulmonary resuscitation outcomes: Is bigger always better? Crit. Care Med. 2012, 40, 3084–3085. [Google Scholar] [CrossRef]
- Gardner, M.M.; Morgan, R.W.; Reeder, R.; Ghaffari, K.; Ortmann, L.; Raymond, T.; Lasa, J.J.; Fowler, J.; Dewan, M.; Nadkarni, V.; et al. Trends in cardiac arrest outcomes & management in children with cardiac illness category compared to non-cardiac illness category: An analysis from the AHA Get with the Guidelines®-Resuscitation Registry. Resuscitation 2024, 205, 110430. [Google Scholar] [CrossRef]
- Gupta, P.; Wilcox, A.; Noel, T.R.; Gossett, J.M.; Rockett, S.R.; Eble, B.K.; Rettiganti, M. Characterizing cardiac arrest in children undergoing cardiac surgery: A single-center study. J. Thorac. Cardiovasc. Surg. 2017, 153, 450–458.e1. [Google Scholar] [CrossRef]
- Ortmann, L.; Prodhan, P.; Gossett, J.; Schexnayder, S.; Berg, R.; Nadkarni, V.; Bhutta, A. Outcomes after in-hospital cardiac arrest in children with cardiac disease: A report from Get with the Guidelines–Resuscitation. Circulation 2011, 124, 2329–2337. [Google Scholar] [CrossRef] [PubMed]
- Gupta, P.; Jacobs, J.P.; Pasquali, S.K.; Hill, K.D.; Gaynor, J.W.; O’Brien, S.M.; He, M.; Sheng, S.; Schexnayder, S.M.; Berg, R.A.; et al. Epidemiology and outcomes after in-hospital cardiac arrest after pediatric cardiac surgery. Ann. Thorac. Surg. 2014, 98, 2138–2144. [Google Scholar] [CrossRef] [PubMed]
- Gupta, P.; Pasquali, S.K.; Jacobs, J.P.; Jacobs, M.L.; Tang, X.; Gossett, J.M.; Gaynor, J.W.; Praestgaard, A.H.; Schexnayder, S.M.; Berg, R.A.; et al. Outcomes Following Single and Recurrent In-Hospital Cardiac Arrests in Children with Heart Disease: A Report from American Heart Association’s Get with the Guidelines Registry-Resuscitation. Pediatr. Crit. Care Med. 2016, 17, 531–539. [Google Scholar] [CrossRef]
- Dagan, M.; Butt, W.; d’Udekem, Y.; Namachivayam, S.P. Timing of in-hospital cardiac arrest after pediatric cardiac surgery: An important metric for quality improvement and prognostication? J. Thorac. Cardiovasc. Surg. 2019, 157, e401–e406. [Google Scholar] [CrossRef]
- Dachepally, R.; Almasri, M.; Liu, W.; Hamzah, M. Factors influencing survival to hospital discharge in children following in-hospital cardiopulmonary arrest. Arch. Pediatr. 2023, 8, 291. [Google Scholar] [CrossRef]
- Pireddu, R.; Ristagno, G.; Gianquintieri, L.; Bonora, R.; Pagliosa, A.; Andreassi, A.; Sechi, G.M.; Signorelli, C.; Stirparo, G. Out-of-Hospital Cardiac Arrest in the Paediatric Patient: An Observational Study in the Context of National Regulations. J. Clin. Med. 2024, 13, 3133. [Google Scholar] [CrossRef] [PubMed]
- Khera, R.; Tang, Y.; Girotra, S.; Nadkarni, V.M.; Link, M.S.; Raymond, T.T.; Guerguerian, A.M.; Berg, R.A.; Chan, P.S. Pulselessness After Initiation of Cardiopulmonary Resuscitation for Bradycardia in Hospitalized Children. Circulation 2019, 140, 370–378. [Google Scholar] [CrossRef]
- Morgan, R.W.; Reeder, R.W.; Meert, K.L.; Telford, R.; Yates, A.R.; Berger, J.T.; Graham, K.; Landis, W.P.; Kilbaugh, T.J.; Newth, C.J.; et al. Outcomes of in-hospital ventricular fibrillation Arrest. Crit. Care Med. 2020, 48, 881–889. [Google Scholar] [CrossRef]
- Faria, J.C.P.; Victorino, C.A.; Sato, M.A. Epinephrine in pediatric cardiorespiratory arrest: When and how much? Einstein 2020, 18, eRW5055. [Google Scholar] [CrossRef]
- Mondal, A.; Dadana, S.; Parmar, P.; Mylavarapu, M.; Bollu, B.; Kali, A.; Dong, Q.; Butt, S.R.; Desai, R. Unfavorable neurological outcomes with incremental cardiopulmonary resuscitation duration in cardiac arrest brain injury: A systematic review and meta-analysis. SN Compr. Clin. Med. 2024, 6, 23. [Google Scholar] [CrossRef]
- Del Castillo, J.; López-Herce, J.; Matamoros, M.; Cañadas, S.; Rodríguez-Calvo, A.; Cecchetti, C.; Rodriguez-Núñez, A.; Álvarez, A.C. Long-term evolution after in-hospital cardiac arrest in children: Prospective multicenter multinational study. Resuscitation 2015, 96, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.W.; Raymond, T.T.; Berg, R.A.; Nadkarni, V.M.; Grossestreuer, A.V.; Kurth, T.; Donnino, M.W. Association Between Tracheal Intubation During Pediatric In-Hospital Cardiac Arrest and Survival. JAMA 2016, 316, 1786–1797. [Google Scholar] [CrossRef] [PubMed]
- Duff, J.P.; Topjian, A.A.; Berg, M.D.; Chan, M.; Haskell, S.E.; Joyner, B.L.; Lasa, J.J., Jr.; Ley, S.J.; Raymond, T.T.; Sutton, R.M.; et al. American Heart Association Focused Update on Pediatric Advanced Life Support: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2019, 140, e904–e914. [Google Scholar] [CrossRef] [PubMed]
- Donoghue, A.; Hsieh, T.C.; Nishisaki, A.; Myers, S. Tracheal intubation during pediatric cardiopulmonary resuscitation: A videography-based assessment in an emergency department resuscitation room. Resuscitation 2016, 99, 38–43. [Google Scholar] [CrossRef]
- Chan, P.S.; Krumholz, H.M.; Nichol, G.; Nallamothu, B.K. American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators. Delayed time to defibrillation after in-hospital cardiac arrest. N. Engl. J. Med. 2008, 358, 9–17. [Google Scholar] [CrossRef]
- Andersen, L.W.; Berg, K.M.; Saindon, B.Z.; Massaro, J.M.; Raymond, T.T.; Berg, R.A.; Nadkarni, V.M.; Donnino, M.W. Time to Epinephrine and Survival After Pediatric In-Hospital Cardiac Arrest. JAMA 2015, 314, 802–810. [Google Scholar] [CrossRef]
- McInnes, A.D.; Sutton, R.M.; Orioles, A.; Nishisaki, A.; Niles, D.; Abella, B.S.; Maltese, M.R.; Berg, R.A.; Nadkarni, V. The first quantitative report of ventilation rate during in-hospital resuscitation of older children and adolescents. Resuscitation 2011, 82, 1025–1029. [Google Scholar] [CrossRef]
- Donoghue, A.; Hsieh, T.C.; Myers, S.; Mak, A.; Sutton, R.; Nadkarni, V. Videographic assessment of cardiopulmonary resuscitation quality in the pediatric emergency department. Resuscitation 2015, 91, 19–25. [Google Scholar] [CrossRef]
- Callaway, C.W.; Donnino, M.W. Testing Epinephrine for Out-of-Hospital Cardiac Arrest. N. Engl. J. Med. 2018, 379, 787–788. [Google Scholar] [CrossRef]
- Gough, C.J.R.; Nolan, J.P. The role of adrenaline in cardiopulmonary resuscitation. Crit. Care. 2018, 22, 139. [Google Scholar] [CrossRef]
- Topjian, A.A.; Raymond, T.T.; Atkins, D.; Chan, M.; Duff, J.P.; Joyner, B.L.; Lasa, J.J., Jr.; Lavonas, E.J.; Levy, A.; Mahgoub, M.; et al. Part 4: Pediatric Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142 (Suppl. S2), S469–S523. [Google Scholar] [CrossRef] [PubMed]
- Meert, K.L.; Telford, R.; Holubkov, R.; Slomine, B.S.; Christensen, J.R.; Dean, J.M.; Moler, F.W. Pediatric Out-of-Hospital Cardiac Arrest Characteristics and Their Association with Survival and Neurobehavioral Outcome. Pediatr. Crit. Care Med. 2016, 17, e543–e550. [Google Scholar] [CrossRef] [PubMed]
- Moler, F.W.; Donaldson, A.E.; Meert, K.; Brilli, R.J.; Nadkarni, V.; Shaffner, D.H.; Schleien, C.L.; Clark, R.S.; Dalton, H.J.; Statler, K.; et al. Multicenter cohort study of out-of-hospital pediatric cardiac arrest. Crit. Care Med. 2011, 39, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, A.; Ikeda, D.J.; Grossestreuer, A.V.; Sheak, K.R.; Delfin, G.; Layden, T.; Abella, B.S.; Leary, M. Factors associated with re-arrest following initial resuscitation from cardiac arrest. Resuscitation 2017, 111, 90–95. [Google Scholar] [CrossRef]
- Zhang, Y.; Rao, C.; Ran, X.; Hu, H.; Jing, L.; Peng, S.; Zhu, W.; Li, S. How to predict the death risk after an in-hospital cardiac arrest (IHCA) in intensive care unit? A retrospective double-centre cohort study from a tertiary hospital in China. BMJ Open 2023, 13, e074214. [Google Scholar] [CrossRef]
- Greif, R.; Lockey, A.; Breckwoldt, J.; Carmona, F.; Conaghan, P.; Kuzovlev, A.; Pflanzl-Knizacek, L.; Sari, F.; Shammet, S.; Scapigliati, A.; et al. European Resuscitation Council Guidelines 2021: Education for Resuscitation. Resuscitation 2021, 161, 388–407. [Google Scholar] [CrossRef]


| Variables | Overall n = 456 | Variables | Overall n = 456 |
|---|---|---|---|
| Age, y, Median (quartiles) | 0.98 (0.33, 4.31) | Weekend 1, n (%) | 144 (31.58) |
| Age category, n (%) | Night 2, n (%) | 200 (43.86) | |
| 29 d–1 y | 230 (50.44) | First documented pulseless rhythm, n (%) | |
| 1–8 y | 162 (35.53) | Bradycardia with poor perfusion | 362 (79.39) |
| ≥8 y | 64 (14.04) | Asystole/PEA | 47 (10.31) |
| Male, n (%) | 253 (55.48) | VF/pVT | 19 (4.17) |
| Local, n (%) | 235 (51.54) | Other or Unknown | 28 (6.14) |
| Illness Category, n (%) | Duration of CPR, min, Median (quartiles) | 8 (3, 25) | |
| General medical | 240 (52.63) | Category of CPR duration, min, n (%) | |
| General surgical | 38 (8.33) | 1–15 | 309 (67.76) |
| Surgical cardiac | 114 (25.00) | 16–35 | 80 (17.54) |
| Medical cardiac | 45 (9.87) | >35 | 67 (14.69) |
| Trauma | 19 (4.17) | Airway management, n (%) | |
| Prehospital arrest, n (%) | 51 (11.18) | BMV | 66 (14.47) |
| Interventions in place before arrest | ETI in place before arrest | 261 (57.24) | |
| Respiratory support, n (%) | Emergency intubation at arrest | 129 (28.29) | |
| Invasive mechanical ventilation | 264 (57.89) | Pharmacological interventions | |
| Noninvasive ventilation | 16 (3.51) | Epinephrine, n (%) | 370 (81.14) |
| None | 176 (38.60) | Number of epinephrine doses, median | 2 (1, 5) |
| Vasoactive infusion, n (%) | 223 (48.90) | Number of epinephrine doses, n (%) | |
| Arrest location, n (%) | >2 | 174 (38.16) | |
| PICU | 248(54.39) | ≤2 | 282 (61.84) |
| Inpatient ward | 139(30.48) | Sodium bicarbonate, n (%) | 183 (40.13) |
| CICU | 43(9.43) | Calcium, n (%) | 52 (11.40) |
| Other | 26 | Atropine, n (%) | 33 (7.24) |
| Time from hospital admission to event, n (%) | Creatine phosphate sodium, n (%) | 86 (18.86) | |
| <1 h | 17 (3.73) | Vitamin C, n (%) | 38 (8.33) |
| 1 to <6 h | 43 (9.43) | Defibrillation, n (%) | 33 (7.24) |
| 6 to <24 h | 66 (14.47) | Rearrest, n (%) | 136 (29.82) |
| 24 h to <1 wk | 150 (32.89) | ECMO, n (%) | 0 (0) |
| 1 wk or more | 180 (39.47) | ||
| Variables | Univariate 1 | Multivariable 1 | ||
|---|---|---|---|---|
| p | OR (95%CI) | p | OR (95%CI) | |
| Age category (vs. 28 d–1 y) | ||||
| 1–8 y | <0.001 | 3.06 (1.93~4.84) | 0.375 | 1.39 (0.67~2.89) |
| ≥8 y | <0.001 | 3.58 (1.89~6.78) | 0.087 | 2.26 (0.89~5.76) |
| Illness Category (vs. General medical) | ||||
| General surgical | 0.181 | 2.44 (0.66~8.99) | 0.650 | 0.65 (0.10~4.23) |
| Surgical cardiac | 0.002 | 0.29 (0.13~0.64) | <0.001 | 0.06 (0.02~0.24) |
| Medical cardiac | 0.553 | 1.37 (0.49~3.81) | 0.739 | 0.75 (0.14~3.98) |
| Trauma | 0.619 | 1.21 (0.57~2.57) | 0.702 | 0.80 (0.24~2.65) |
| Respiratory support in place before arrest (vs. None) | ||||
| Invasive mechanical ventilation | 0.004 | 1.84 (1.21~2.79) | 0.380 | 2.62 (0.30~22.61) |
| Noninvasive ventilation | 0.018 | 0.16 (0.04~0.74) | 0.519 | 0.55 (0.09~3.41) |
| Vasoactive infusion in place before arrest | <0.001 | 2.79 (1.85~4.20) | <0.001 | 7.69 (3.49~16.93) |
| Night | 0.003 | 1.85 (1.23~2.78) | 0.565 | 1.12 (0.65~2.22) |
| Arrest location (vs. PICU) | ||||
| Inpatient ward | 0.004 | 0.51 (0.32~0.81) | 0.820 | 0.88 (0.30~2.59) |
| CICU | <0.001 | 0.15 (0.07~0.34) | 0.329 | 0.53 (0.15~1.88) |
| Other | 0.054 | 0.42 (0.17~1.02) | 0.772 | 0.81 (0.19~3.41) |
| First documented pulseless rhythm (vs. Bradycardia with poor perfusion) | ||||
| Asystole/PEA | 0.012 | 2.82 (1.25~6.36) | 0.194 | 2.16 (0.68~6.88) |
| VF/pVT | 0.223 | 0.52 (0.18~1.49) | 0.010 | 0.15 (0.03~0.63) |
| Other or Unknown | 0.055 | 0.44 (0.19~1.02) | 0.100 | 0.33 (0.09~1.23) |
| Category of CPR duration, min (vs. 1–15) | ||||
| 16–35 | <0.001 | 4.29 (2.36~7.80) | 0.848 | 1.11 (0.39~3.17) |
| >35 | <0.001 | 13.29 (5.54~31.88) | <0.001 | 13.92 (3.24~59.82) |
| Number of epinephrine doses > 2 | <0.001 | 5.98 (3.75~9.54) | 0.026 | 3.12 (1.15~8.46) |
| Sodium bicarbonate | <0.001 | 6.20 (3.90~9.86) | 0.132 | 1.88 (0.83~4.28) |
| Creatine phosphate sodium | 0.001 | 2.47 (1.43~4.27) | 0.232 | 0.57 (0.23~1.43) |
| Atropine | 0.057 | 2.25 (0.98~5.18) | 0.369 | 0.52 (0.12~2.18) |
| Vitamin C | <0.001 | 5.60 (2.13~14.70) | 0.720 | 1.27 (0.34~4.68) |
| Airway management (vs. Bag-Mask Ventilation) | ||||
| ETI in place before arrest | <0.001 | 9.82 (4.42~21.84) | 0.932 | 1.11 (0.11~11.01) |
| Emergency intubation at arrest | <0.001 | 8.07 (3.47~18.75 | 0.008 | 5.17 (1.54~17.36) |
| Rearrest | <0.001 | 2.70 (1.71~4.26) | <0.001 | 8.48 (4.11~17.52) |
| Factors not in Multivariable logistic regression analysis | ||||
| Male | 0.901 | 0.98 (0.65~1.45) | ||
| Local | 0.198 | 1.30 (0.87~1.94) | ||
| Prehospital arrest | 0.484 | 1.26 (0.66~2.39) | ||
| Weekend | 0.844 | 1.04 (0.68~1.60) | ||
| Time from hospital admission to event (vs. <1 h) | ||||
| 1 to <6 h | 0.135 | 0.33 (0.08~1.41) | ||
| 6 to <24 h | 0.477 | 0.60 (0.15~2.46) | ||
| 24 h to <1 wk | 0.113 | 0.34 (0.09~1.29) | ||
| 1 wk or more | 0.137 | 0.37 (0.10~1.38) | ||
| Defibrillation | 0.804 | 1.10 (0.51~2.37) | ||
| Calcium | 0.130 | 1.64 (0.87~3.09) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cao, J.; Song, J.; Shan, B.; Zhu, C.; Tan, L. Characteristics, Outcomes and Mortality Risk Factors of Pediatric In-Hospital Cardiac Arrest in Western China: A Retrospective Study Using Utstein Style. Children 2025, 12, 579. https://doi.org/10.3390/children12050579
Cao J, Song J, Shan B, Zhu C, Tan L. Characteristics, Outcomes and Mortality Risk Factors of Pediatric In-Hospital Cardiac Arrest in Western China: A Retrospective Study Using Utstein Style. Children. 2025; 12(5):579. https://doi.org/10.3390/children12050579
Chicago/Turabian StyleCao, Jiaoyang, Jing Song, Baoju Shan, Changxin Zhu, and Liping Tan. 2025. "Characteristics, Outcomes and Mortality Risk Factors of Pediatric In-Hospital Cardiac Arrest in Western China: A Retrospective Study Using Utstein Style" Children 12, no. 5: 579. https://doi.org/10.3390/children12050579
APA StyleCao, J., Song, J., Shan, B., Zhu, C., & Tan, L. (2025). Characteristics, Outcomes and Mortality Risk Factors of Pediatric In-Hospital Cardiac Arrest in Western China: A Retrospective Study Using Utstein Style. Children, 12(5), 579. https://doi.org/10.3390/children12050579






