Intraoperative Methadone Versus Non-Methadone Analgesia in Pediatric Cardiac Surgery: A Retrospective Cohort Study
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Anesthetic Management
2.3. Outcome Measurements
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics and Analgesia Groups
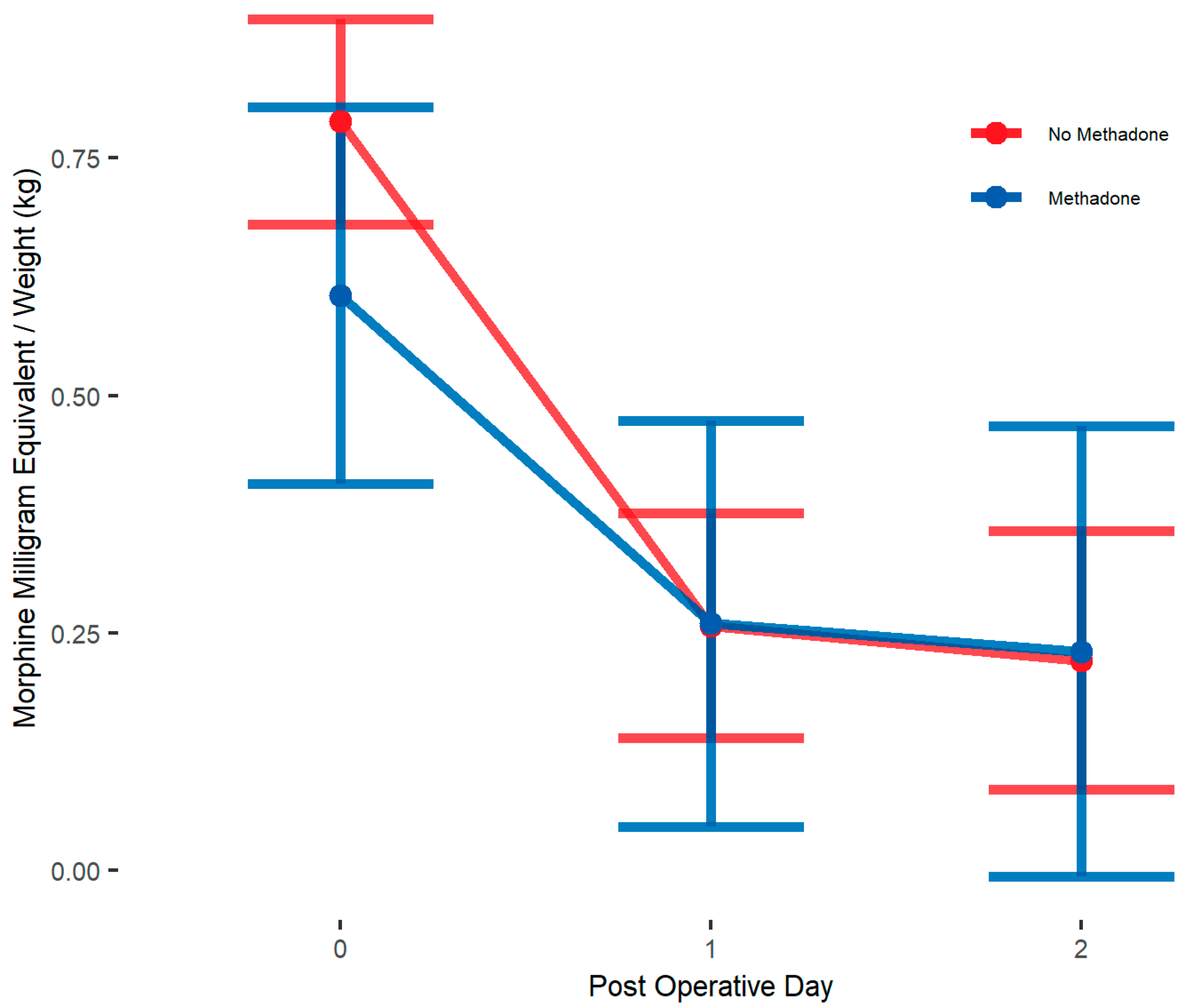
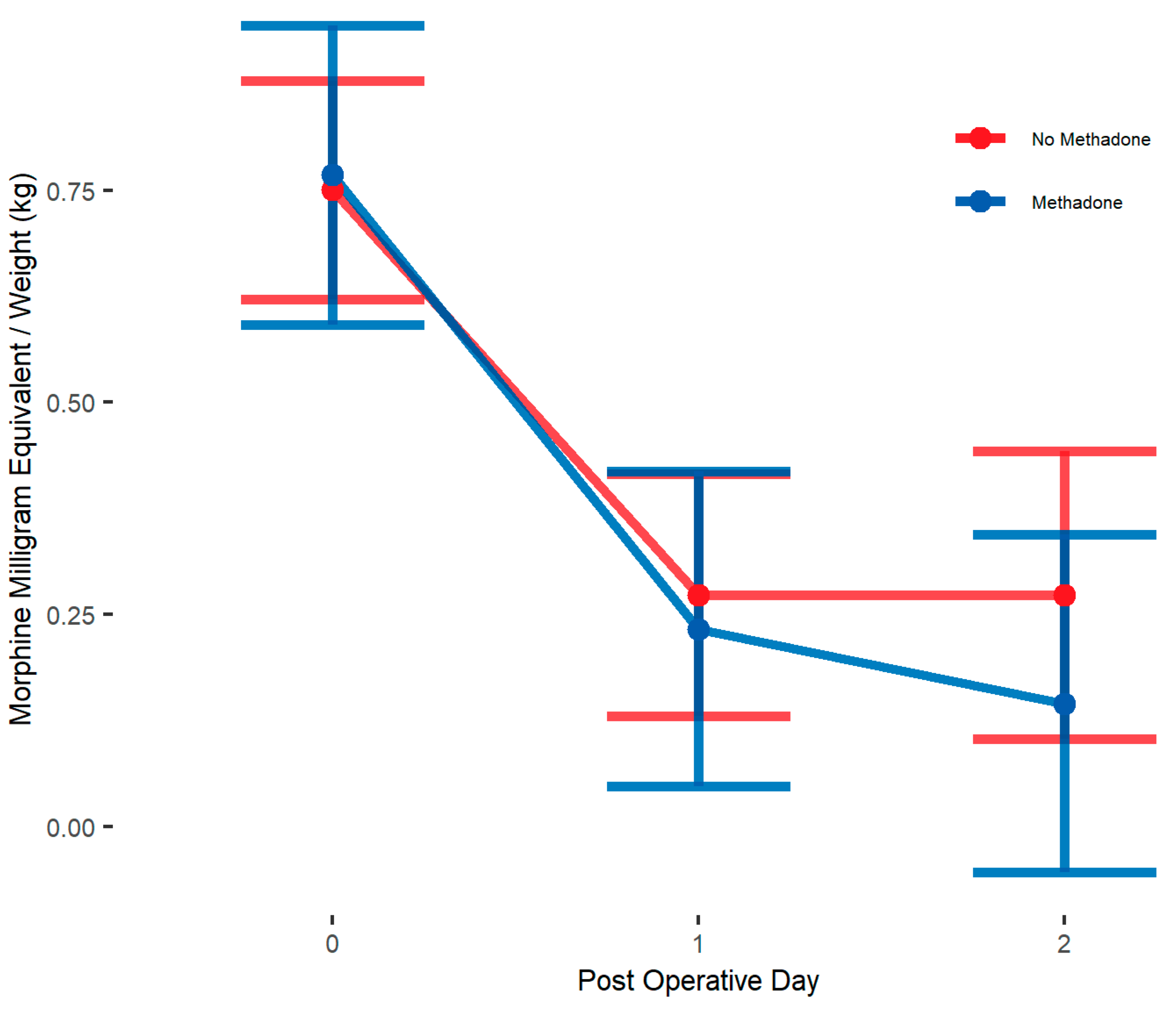
3.2. Primary Outcome—Postoperative Opioid Consumption (MME/kg)
3.3. Secondary Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stanley, T.H. The fentanyl story. J. Pain 2014, 15, 1215–1226. [Google Scholar] [CrossRef] [PubMed]
- Pathan, H.; Williams, J. Basic opioid pharmacology: An update. Br. J. Pain 2012, 6, 11–16. [Google Scholar] [CrossRef]
- Scholz, J.; Steinfath, M.; Schulz, M. Clinical pharmacokinetics of alfentanil, fentanyl and sufentanil. An update. Clin. Pharmacokinet. 1996, 31, 275–292. [Google Scholar] [CrossRef] [PubMed]
- Anand, K.J.; Willson, D.F.; Berger, J.; Harrison, R.; Meert, K.L.; Zimmerman, J.; Carcillo, J.; Newth, C.J.; Prodhan, P.; Dean, J.M.; et al. Tolerance and withdrawal from prolonged opioid use in critically ill children. Pediatrics 2010, 125, e1208–e1225. [Google Scholar] [CrossRef]
- Nguyen, K.N.; Byrd, H.S.; Tan, J.M. Caudal analgesia and cardiothoracic surgery: A look at postoperative pain scores in a pediatric population. Paediatr. Anaesth. 2016, 26, 1060–1063. [Google Scholar] [CrossRef]
- Rosen, K.R.; Rosen, D.A. Caudal epidural morphine for control of pain following open heart surgery in children. Anesthesiology 1989, 70, 418–421. [Google Scholar] [CrossRef]
- Horlocker, T.T.; Vandermeuelen, E.; Kopp, S.L.; Gogarten, W.; Leffert, L.R.; Benzon, H.T. Regional Anesthesia in the Patient Receiving Antithrombotic or Thrombolytic Therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Fourth Edition). Reg. Anesth. Pain Med. 2018, 43, 263–309. [Google Scholar] [CrossRef] [PubMed]
- Ramaiah, V.K.; Kharasch, E.D. Methadone and Enhanced Recovery After Surgery: Concepts and Protocols. Anesth. Analg. 2024, 139, 670–674. [Google Scholar] [CrossRef]
- Garcia, S.; Mali, M.; Grewal, A. Pro: Methadone Should Be Used as a Part of Enhanced Recovery After Cardiac Surgery Protocol. J. Cardiothorac. Vasc. Anesth. 2024, 38, 1268–1271. [Google Scholar] [CrossRef]
- Sadhasivam, S.; Aruldhas, B.W.; Packiasabapathy, S.; Overholser, B.R.; Zhang, P.; Zang, Y.; Renschler, J.S.; Fitzgerald, R.E.; Quinney, S.K. A Novel Perioperative Multidose Methadone-Based Multimodal Analgesic Strategy in Children Achieved Safe and Low Analgesic Blood Methadone Levels Enabling Opioid-Sparing Sustained Analgesia With Minimal Adverse Effects. Anesth. Analg. 2021, 133, 327–337. [Google Scholar] [CrossRef]
- Ye, J.; Myung, K.; Packiasabapathy, S.; Yu, J.S.; Jacobson, J.E.; Whittaker, S.C.; Castelluccio, P.; Drayton Jackson, M.; Sadhasivam, S. Methadone-Based Multimodal Analgesia Provides the Best-in-Class Acute Surgical Pain Control and Functional Outcomes with Lower Opioid Use Following Major Posterior Fusion Surgery in Adolescents with Idiopathic Scoliosis. Pediatr. Qual. Saf. 2020, 5, e336. [Google Scholar] [CrossRef] [PubMed]
- Barnett, A.M.; Machovec, K.A.; Ames, W.A.; Homi, H.M.; Turi, J.L.; Koo, J.; Fuller, M.; Jooste, E.H. The effect of intraoperative methadone during pediatric cardiac surgery on postoperative opioid requirements. Paediatr. Anaesth. 2020, 30, 773–779. [Google Scholar] [CrossRef]
- Santa Cruz Mercado, L.A.; Liu, R.; Bharadwaj, K.M.; Johnson, J.J.; Gutierrez, R.; Das, P.; Balanza, G.; Deng, H.; Pandit, A.; Stone, T.A.D.; et al. Association of Intraoperative Opioid Administration With Postoperative Pain and Opioid Use. JAMA Surg. 2023, 158, 854–864. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, S.; Degenhardt, L.; Hoban, B.; Gisev, N. A synthesis of oral morphine equivalents (OME) for opioid utilisation studies. Pharmacoepidemiol. Drug Saf. 2016, 25, 733–737. [Google Scholar] [CrossRef] [PubMed]
- Merkel, S.I.; Voepel-Lewis, T.; Shayevitz, J.R.; Malviya, S. The FLACC: A behavioral scale for scoring postoperative pain in young children. Pediatr. Nurs. 1997, 23, 293–297. [Google Scholar]
- Krechel, S.W.; Bildner, J. CRIES: A new neonatal postoperative pain measurement score. Initial testing of validity and reliability. Paediatr. Anaesth. 1995, 5, 53–61. [Google Scholar] [CrossRef]
- Aruldhas, B.W.; Quinney, S.K.; Overholser, B.R.; Heathman, M.A.; Masters, A.R.; Ly, R.C.; Gao, H.; Packiasabapathy, S.; Sadhasivam, S. Pharmacokinetic modeling of R and S-Methadone and their metabolites to study the effects of various covariates in post-operative children. CPT Pharmacomet. Syst. Pharmacol. 2021, 10, 1183–1194. [Google Scholar] [CrossRef]
- Packiasabapathy, S.; Aruldhas, B.W.; Zhang, P.; Overholser, B.R.; Quinney, S.K.; Sadhasivam, S. Novel associations between CYP2B6 polymorphisms, perioperative methadone metabolism and clinical outcomes in children. Pharmacogenomics 2021, 22, 591–602. [Google Scholar] [CrossRef]
- D’Souza, R.S.; Esfahani, K.; Dunn, L.K. Pro-Con Debate: Role of Methadone in Enhanced Recovery After Surgery Protocols-Superior Analgesic or Harmful Drug? Anesth. Analg. 2023, 137, 76–82. [Google Scholar] [CrossRef]
- Murphy, G.S.; Avram, M.J.; Greenberg, S.B.; Shear, T.D.; Deshur, M.A.; Dickerson, D.; Bilimoria, S.; Benson, J.; Maher, C.E.; Trenk, G.J.; et al. Postoperative Pain and Analgesic Requirements in the First Year after Intraoperative Methadone for Complex Spine and Cardiac Surgery. Anesthesiology 2020, 132, 330–342. [Google Scholar] [CrossRef]
- Murphy, G.S.; Szokol, J.W.; Avram, M.J.; Greenberg, S.B.; Shear, T.D.; Deshur, M.A.; Vender, J.S.; Benson, J.; Newmark, R.L. Clinical Effectiveness and Safety of Intraoperative Methadone in Patients Undergoing Posterior Spinal Fusion Surgery: A Randomized, Double-blinded, Controlled Trial. Anesthesiology 2017, 126, 822–833. [Google Scholar] [CrossRef] [PubMed]
- McClain, M.R.; Subramaniam, K.; Cheema, R.; Lavage, D.R.; Lin, H.S.; Sultan, I.; Sadhasivam, S.; Howard-Quijano, K. Intraoperative Methadone in Adult Cardiac Surgical Patients and Risks for Postoperative QTc Prolongation. J. Cardiothorac. Vasc. Anesth. 2025, 39, 406–413. [Google Scholar] [CrossRef] [PubMed]
| Variable | Variable Value | Total n = 287 | No Methadone n = 220 (77%) | Methadone n = 67 (23%) | p-Value |
|---|---|---|---|---|---|
| Age, mean (SD) | years | 3.83 (4.87) | 2.7 (3.9) | 7.6 (5.9) | <0.001 |
| Age Groups, n (%) | ≤6 years | 226 (78.7%) | 196 (89%) | 30 (45%) | <0.001 |
| >6 years | 61 (21.3%) | 24 (11%) | 37 (55%) | ||
| Sex, n (%) | Female | 118 (41.1%) | 93 (42%) | 25 (37%) | 0.470 |
| Male | 169 (58.9%) | 127 (58%) | 42 (63%) | ||
| Race, n (%) | White | 207 (72.1%) | 157 (71%) | 50 (75%) | 0.361 |
| Black | 21 (7.3%) | 19 (9%) | 2 (3%) | ||
| American Indian | 3 (1%) | 1 (0%) | 2 (3%) | ||
| Multiple Race | 1 (0.3%) | 1 (0%) | 0 (0%) | ||
| Other or Asian | 2 (0.7%) | 2 (1%) | 0 (0%) | ||
| Not Specified | 4 (1.4%) | 3 (1%) | 1 (1%) | ||
| Patient Declined | 49 (17.1%) | 37 (17%) | 12 (18%) | ||
| Surgery Type, n (%) | CPB Cardiovascular | 271 (94.4%) | 210 (95%) | 61 (91%) | 0.020 |
| No CPB Cardiovascular | 12 (4.2%) | 9 (4%) | 3 (4%) | ||
| Other | 1 (0.3%) | 1 (0%) | 0 (0%) | ||
| VAD Operation Done With CPB | 3 (1%) | 0 (0%) | 3 (4%) | ||
| STAT category, n (%) | 1 | 164 (58%) | 132 (60%) | 32 (50%) | 0.331 |
| 2 | 93 (32.9%) | 69 (32%) | 24 (38%) | ||
| 3 | 21 (7.4%) | 15 (7%) | 6 (9%) | ||
| 4 | 5 (1.8%) | 3 (1%) | 2 (3%) | ||
| Weight, mean (SD) | kg | 18.25 (18.53) | 14.5 (14.8) | 30.6 (23.7) | <0.001 |
| Variable | Total n = 287 | No Methadone n = 220 (77%) | Methadone n = 67 (23%) | p-Value |
|---|---|---|---|---|
| Caudal, n (%) | 173 (60.3%) | 171 (78%) | 2 (3%) | <0.001 |
| Fentanyl, n (%) | 276 (96.2%) | 220 (100%) | 56 (84%) | <0.001 |
| Methadone, n (%) | 67 (23.3%) | 0 (0%) | 67 (100%) | <0.001 |
| Sufentanil, n (%) | 35 (12.2%) | 34 (15%) | 1 (1%) | 0.001 |
| Hydromorphone, n (%) | 1 (0.3%) | 1 (0%) | 0 (0%) | 0.999 |
| Ketamine, n (%) | 1 (0.3%) | 0 (0%) | 1 (1%) | 0.233 |
| Intraoperative Opioid MME/kg, Median (IQR) | 0.5 (0.39–0.56) | 0.5 (0.4–0.6) | 0.5 (0.4–0.5) | 0.649 |
| Outcome Variable | Total n = 287 | No Methadone n = 220 (77%) | Methadone n = 67 (23%) | p-Value |
|---|---|---|---|---|
| Postoperative Opioid Use in MME/kg, median (IQR) | ||||
| POD 0 | 0.43 (0.16–1.03) | 0.5 (0.2–1.1) | 0.3 (0.1–0.7) | 0.005 |
| POD 1 | 0.1 (0.05–0.19) | 0.1 (0.1–0.2) | 0.1 (0–0.2) | 0.718 |
| POD 2 | 0.07 (0.04–0.15) | 0.1 (0–0.1) | 0.1 (0–0.2) | 0.052 |
| Total (POD 0–4) | 0.69 (0.3–1.31) | 0.7 (0.3–1.4) | 0.5 (0.3–1.1) | 0.132 |
| Average Pain Score, mean (SD) | ||||
| POD 0 | 2.05 (1.49) | 2.1 (1.5) | 1.9 (1.3) | 0.422 |
| POD 1 | 1 (1.01) | 1 (1) | 1 (1.1) | 0.890 |
| POD 2 | 1.02 (1.46) | 1 (1.4) | 0.9 (1.5) | 0.680 |
| Max Pain Score, mean (SD) | ||||
| POD 0 | 7.54 (2.67) | 7.6 (2.7) | 7.3 (2.7) | 0.403 |
| POD 1 | 4.54 (3.55) | 4.6 (3.6) | 4.4 (3.4) | 0.718 |
| POD 2 | 3.92 (3.37) | 3.9 (3.3) | 4.1 (3.6) | 0.739 |
| Any Postoperative Antiemetic, n (%) | 59 (20.7%) | 32 (15%) | 27 (40%) | <0.001 |
| POD 0 | 43 (15%) | 22 (10%) | 21 (31%) | <0.001 |
| POD 1 | 24 (8.4%) | 11 (5%) | 13 (19%) | <0.001 |
| POD 2 | 16 (5.6%) | 7 (3%) | 9 (13%) | <0.001 |
| Postoperative Hospital LOS, median (IQR) | 5 (3–8) | 5 (3–8) | 5 (4–9.8) | 0.089 |
| ICU LOS, median (IQR) | 2.1 (1.15–3.21) | 2.1 (1.2–3.2) | 2.1 (1.2–4) | 0.823 |
| Reintubated, n (%) | 30 (10.5%) | 21 (10%) | 9 (13%) | 0.366 |
| Naloxone, n (%) | 6 (2.1%) | 5 (2%) | 1 (1%) | 0.999 |
| Outcome Variable | Total n = 567.6 | No Methadone n = 281.9 (49.7%) | Methadone n = 285.68 (50.3%) | p-Value |
|---|---|---|---|---|
| Postoperative Opioid Use in MME/kg, median (IQR) | ||||
| POD 0 | 0.5 (0.2–1.1) | 0.4 (0.2–1) | 0.6 (0.2–1.2) | 0.496 |
| POD 1 | 0.1 (0.1–0.2) | 0.1 (0.1–0.2) | 0.1 (0.1–0.3) | 0.311 |
| POD 2 | 0.1 (0–0.2) | 0.1 (0–0.1) | 0.1 (0.1–0.4) | 0.017 |
| Total (POD 0–4) | 0.7 (0.3–1.4) | 0.7 (0.3–1.2) | 0.7 (0.4–1.8) | 0.139 |
| Average Pain Score, mean (SD) | ||||
| POD 0 | 1.99 (1.38) | 2.00 (1.54) | 1.97 (1.19) | 0.889 |
| POD 1 | 1.02 (1.04) | 0.94 (0.99) | 1.12 (1.11) | 0.450 |
| POD 2 | 1.08 (1.58) | 1.01 (1.42) | 1.15 (1.74) | 0.719 |
| Max Pain Score, mean (SD) | ||||
| POD 0 | 7.60 (2.74) | 7.23 (2.95) | 8.03 (2.43) | 0.082 |
| POD 1 | 4.76 (3.65) | 4.30 (3.62) | 5.27 (3.66) | 0.236 |
| POD 2 | 4.44 (3.43) | 3.74 (3.33) | 5.15 (3.45) | 0.068 |
| Any Postoperative Antiemetic, n (%) | 108.6 (19.2) | 49.1 (17.5) | 59.5 (20.8) | 0.557 |
| POD 0 | 85.1 (15.0) | 35.7 (12.7) | 49.4 (17.3) | 0.359 |
| POD 1 | 41.0 (7.2) | 17.7 (6.3) | 23.3 (8.1) | 0.565 |
| POD 2 | 31.2 (5.5) | 11.2 (4.0) | 19.9 (7.0) | 0.356 |
| Postoperative Hospital LOS, median (IQR) | 5 (3–10) | 4 (3–8) | 8 (4–23.4) | 0.002 |
| ICU LOS, median (IQR) | 2.2 (1.2–4.9) | 2.1 (1.1–3.1) | 2.8 (1.8–6.3) | 0.018 |
| Reintubated, n (%) | 65.5 (11.5) | 27.4 (9.7) | 38.1 (13.3) | 0.515 |
| Naloxone, n (%) | 10.0 (1.8) | 8.0 (2.9) | 2.0 (0.7) | 0.171 |
| Outcomes | Opioid Use in MME/kg | Average Pain Score | Max Pain Score | Postoperative Antiemetic | Postoperative Hospital LOS |
|---|---|---|---|---|---|
| Estimates | Mean Difference 95% CI | Mean Difference 95% CI | Mean Difference 95% CI | Relative Risk 95% CI | Mean Ratio 95% CI |
| Overall (n = 287) | p = 0.73 −0.03 (−0.22, 0.16) | p = 0.66 −0.07 (−0.40, 0.26) | p = 0.99 −0.002 (−0.76, 0.76) | p = 0.56 1.19 (0.67, 2.1) | p < 0.001 2.62 (1.55, 4.41) |
| Age ≤ 6 years (n = 226, 79%) | p = 0.20 0.17 (−0.09, 0.44) | p = 0.87 0.03 (−0.37, 0.44) | p = 0.02 0.91 (0.15, 1.68) | p = 0.8 1.14 (0.41, 3.23) | p < 0.001 2.14 (1.3, 3.55) |
| Age > 6 years (n = 61, 21%) | p = 0.76 0.02 (−0.22, 0.27) | p = 0.32 0.54 (−0.55, 1.64) | p = 0.68 0.4 (−1.59, 2.4) | p = 0.19 1.86 (0.73, 4.72) | p = 0.36 1.13 (0.87, 1.46) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blasiole, B.; Lavage, D.R.; Lin, H.-H.S.; Licata, S.E.; Sivam, S.; Sivam, I.; Le, L.M.; Sadhasivam, S. Intraoperative Methadone Versus Non-Methadone Analgesia in Pediatric Cardiac Surgery: A Retrospective Cohort Study. Children 2025, 12, 567. https://doi.org/10.3390/children12050567
Blasiole B, Lavage DR, Lin H-HS, Licata SE, Sivam S, Sivam I, Le LM, Sadhasivam S. Intraoperative Methadone Versus Non-Methadone Analgesia in Pediatric Cardiac Surgery: A Retrospective Cohort Study. Children. 2025; 12(5):567. https://doi.org/10.3390/children12050567
Chicago/Turabian StyleBlasiole, Brian, Danielle R. Lavage, Hsing-Hua Sylvia Lin, Scott E. Licata, Sahana Sivam, Inesh Sivam, Laura M. Le, and Senthilkumar Sadhasivam. 2025. "Intraoperative Methadone Versus Non-Methadone Analgesia in Pediatric Cardiac Surgery: A Retrospective Cohort Study" Children 12, no. 5: 567. https://doi.org/10.3390/children12050567
APA StyleBlasiole, B., Lavage, D. R., Lin, H.-H. S., Licata, S. E., Sivam, S., Sivam, I., Le, L. M., & Sadhasivam, S. (2025). Intraoperative Methadone Versus Non-Methadone Analgesia in Pediatric Cardiac Surgery: A Retrospective Cohort Study. Children, 12(5), 567. https://doi.org/10.3390/children12050567






