Gynecomastia Outpatient Surgical Treatment in Children Without Closed-Suction Drain Placement: Is It Safe and Effective?
Abstract
1. Introduction
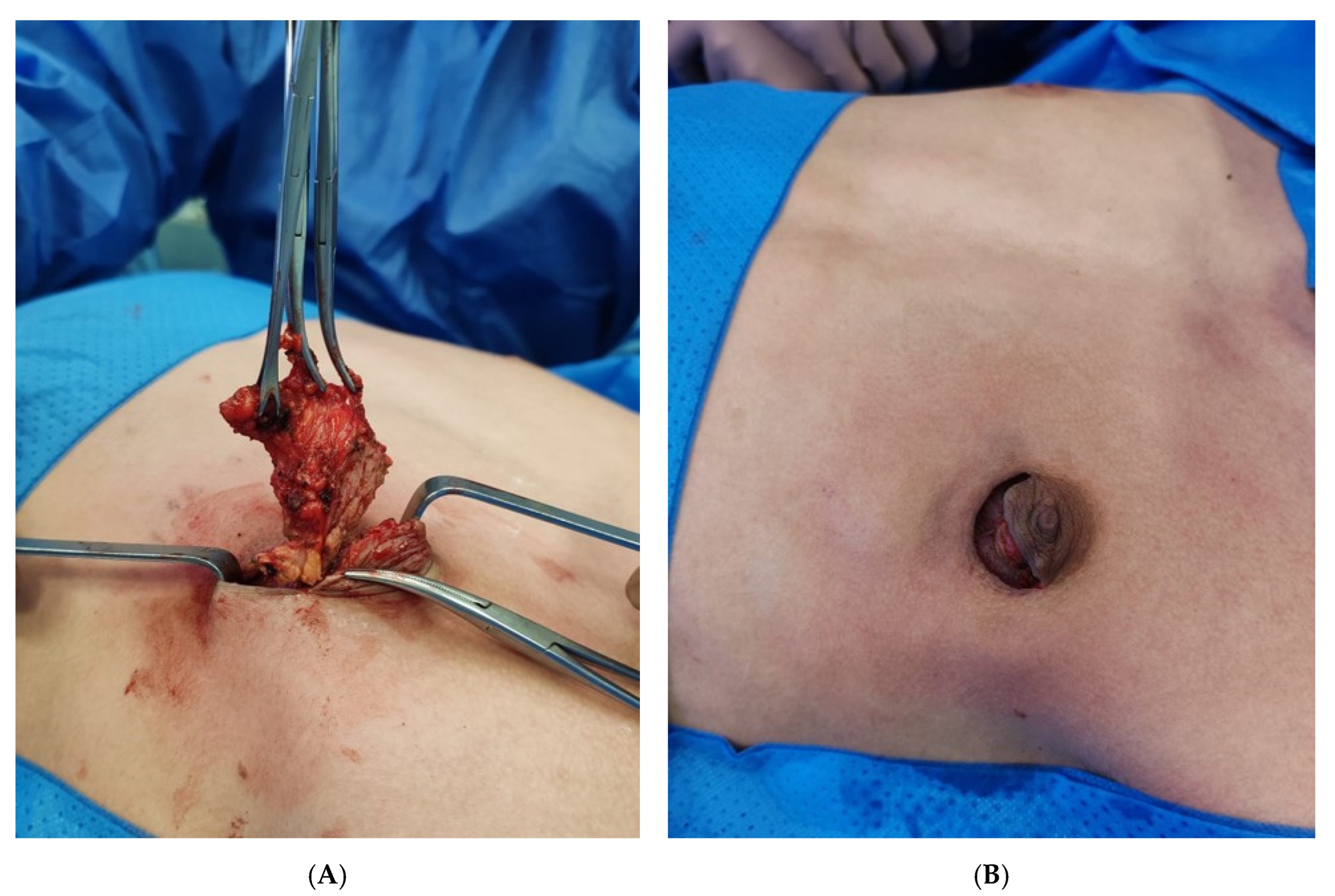
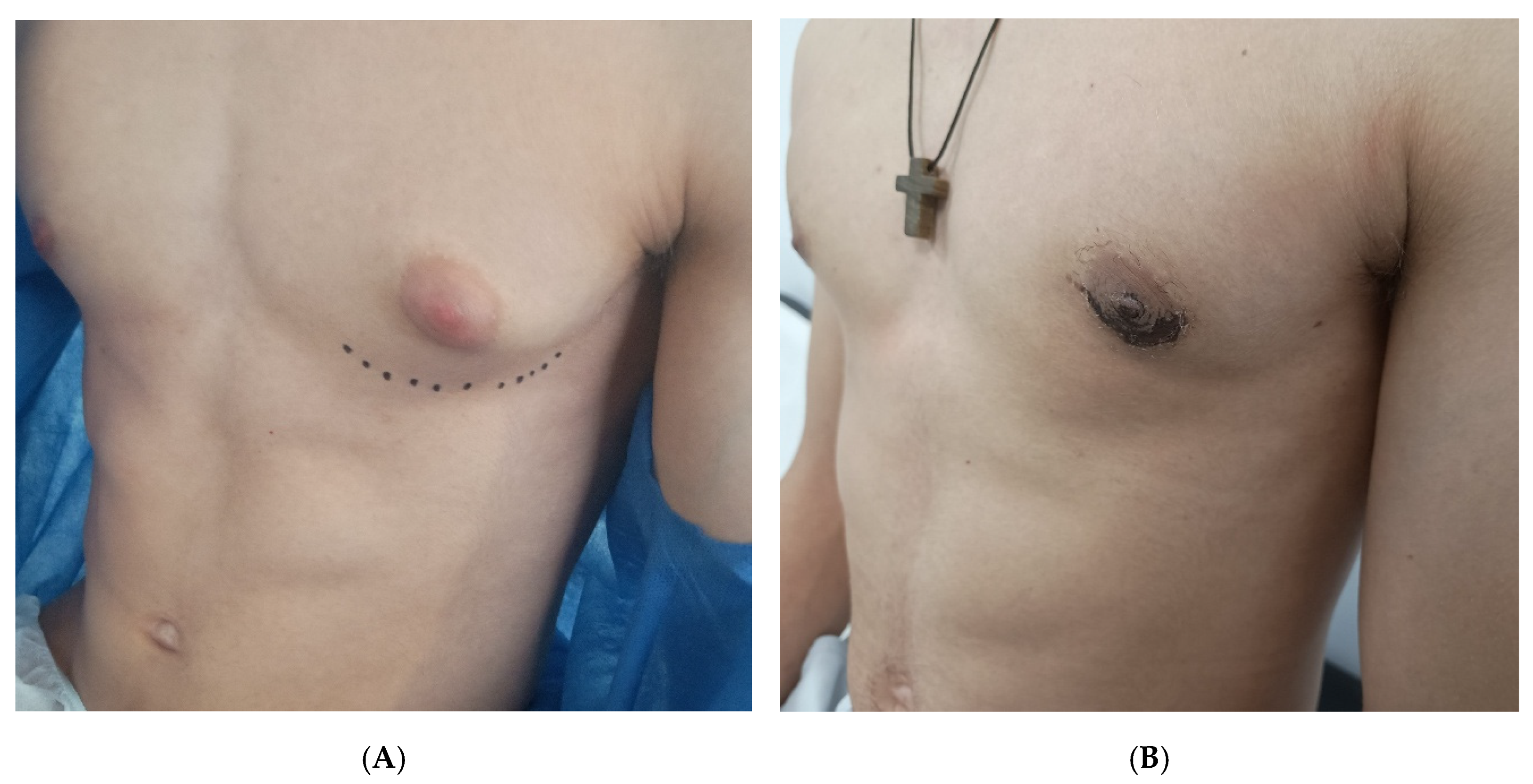
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cuhaci, N.; Polat, S.B.; Evranos, B.; Ersoy, R.; Cakir, B. Gynecomastia: Clinical evaluation and management. Indian J. Endocrinol. Metab. 2014, 18, 150–158. [Google Scholar] [CrossRef]
- Chang, D.K.; Siy, R.; Friedman, J.; Brown, R.H. Trends in the surgical correction of gynecomastia. Semin. Plast. Surg. 2015, 29, 122–130. [Google Scholar] [CrossRef]
- Kinsella, C., Jr.; Landfair, A.; Rottgers, S.A.; Cray, J.J.; Weidman, C.; Deleyiannis, F.W.-B.; Grunwaldt, L.; Losee, J.E. The psychological burden of idiopathic adolescent gynecomastia. Plast. Reconstr. Surg. 2012, 129, 1–7. [Google Scholar] [CrossRef]
- Rew, L.; Young, C.; Harrison, T.; Caridi, R. A systematic review of literature on psychosocial aspects of gynecomastia in adolescents and young men. J. Adolesc. 2015, 43, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Fagerlund, A.; Lewin, R.; Rufolo, G.; Elander, A.; Santanelli di Pompeo, F.; Selvaggi, G. Gynecomastia: A systematic review. J. Plast. Surg. Hand Surg. 2015, 49, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Teimourian, B.; Perlman, R. Surgery for gynecomastia. Aesthetic Plast. Surg. 1983, 7, 155–157. [Google Scholar] [CrossRef] [PubMed]
- Varley, G.W.; Milner, S.; Turner, G.M.; Crisp, A.J.; Szypryt, E.P. Ultrasound assessment of the efficacy of wound drains. J. R. Coll. Surg. Edinb. 1994, 39, 97–99. [Google Scholar]
- Matarasso, A.; Wallach, S.G.; Rankin, M. Reevaluating the need for routine drainage in reduction mammoplasty. Plast. Reconstr. Surg. 1998, 102, 1917–1921. [Google Scholar] [CrossRef]
- Keskin, M.; Sutcu, M.; Cigsar, B.; Karacaoglan, N. Necessity of suction drains in gynecomastia surgery. Aesthetic Surg. J. 2014, 34, 538–544. [Google Scholar] [CrossRef]
- Chao, J.W.; Raveendran, J.A.; Maly, C.; Rogers, G.; Boyajian, M.; Oh, A.K. Closed-Suction Drains After Subcutaneous Mastectomy for Gynecomastia: Do They Reduce Complications? Aesthetic Plast. Surg. 2017, 41, 1291–1294. [Google Scholar] [CrossRef]
- Simon, B.E.; Hoffman, S.; Kahn, S. Classification and surgical correction of gynecomastia. Plast. Reconstr. Surg. 1973, 51, 48Y56. [Google Scholar] [CrossRef]
- Balcı, Ö.; Karaman, İ.; Karaman, A. Infra-areolar subcutaneous mastectomy in the surgical treatment of adolescent gynecomastia. Pediatr. Surg. Int. 2024, 40, 92. [Google Scholar] [CrossRef]
- Kumanov, P.; Deepinder, F.; Robeva, R.; Tomova, A.; Li, J.; Agarwal, A. Relationship of adolescent gynecomastia with varicocele and somatometric parameters: A cross-sectional study in 6200 healthy boys. J. Adolesc. Health 2007, 41, 126–131. [Google Scholar] [CrossRef]
- Holzmer, S.W.; Lewis, P.G.; Landau, M.J.; Hill, M.E. Surgical Management of Gynecomastia: A Comprehensive Review of the Literature. Plast. Reconstr. Surg. Glob. Open 2020, 8, e3161. [Google Scholar] [CrossRef] [PubMed]
- Choi, B.S.; Lee, S.R.; Byun, G.Y.; Hwang, S.B.; Koo, B.H. The Characteristics and Short-Term Surgical Outcomes of Adolescent Gynecomastia. Aesthetic Plast. Surg. 2017, 41, 1011–1021. [Google Scholar] [CrossRef] [PubMed]
- Ridha, H.; Colville, R.J.; Vesely, M.J. How happy are patients with their gynaecomastia reduction surgery? J. Plast. Reconstr. Aesthet. Surg. 2009, 62, 1473–1478. [Google Scholar] [CrossRef]
- Davanço, R.A.; Sabino Neto, M.; Garcia, E.B.; Matsuoka, P.K.; Huijsmans, J.P.; Ferreira, L.M. Quality of life in the surgical treatment of gynecomastia. Aesthetic Plast. Surg. 2009, 33, 514–517. [Google Scholar] [CrossRef] [PubMed]
- Nuzzi, L.C.; Cerrato, F.E.; Erickson, C.R.; Webb, M.L.; Rosen, H.; Walsh, E.M.; Labow, B.I. Psychosocial impact of adolescent gynecomastia: A prospective case-control study. Plast. Reconstr. Surg. 2013, 131, 890–896. [Google Scholar] [CrossRef]
- Reiffel, A.J.; Pharmer, L.A.; Weinstein, A.L.; Spector, J.A. A prospective analysis of the association between indwelling surgical drains and surgical site infection in plastic surgery. Ann. Plast. Surg. 2013, 71, 561–565. [Google Scholar] [CrossRef]
- Arrowsmith, J.; Eltigani, E.; Krarup, K.; Varma, S. An audit of breast reduction without drains. Br. J. Plast. Surg. 1999, 52, 586–590. [Google Scholar] [CrossRef]
- Corion, L.U.; Smeulders, M.J.; van Zuijlen, P.P.; van der Horst, C.M. Draining after breast reduction: A randomized controlled inter-patient study. J. Plast. Reconstr. Aesthet. Surg. 2009, 62, 865–868. [Google Scholar] [CrossRef]
- Langer, S.; Guenther, J.M.; DiFronzo, L.A. Does fibrin sealant reduce drain output and allow earlier removal of drainage catheters in women undergoing operation for breast cancer? Am. Surg. 2003, 69, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Fischer, S.; Hirsch, T.; Hirche, C.; Kiefer, J.; Kueckelhaus, M.; Germann, G.; Reichenberger, M.A. Surgical treatment of primary gynecomastia in children and adolescents. Pediatr. Surg. Int. 2014, 30, 641–647. [Google Scholar] [CrossRef]
- Lanitis, S.; Starren, E.; Read, J.; Heymann, T.; Tekkis, P.; Hadjiminas, D.J.; Al Mufti, R. Surgical management of gynaecomastia: Outcomes from our experience. Breast 2008, 17, 596–603. [Google Scholar] [CrossRef] [PubMed]
- Handschin, A.E.; Bietry, D.; Hu¨sler, R.; Banic, A.; Constantinescu, M. Surgical management of gynecomastiaVa 10-year analysis. World J. Surg. 2008, 32, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Ramon, Y.; Fodor, L.; Peled, I.J.; Eldor, L.; Egozi, D.; Ullmann, Y. Multimodality gynecomastia repair by crosschest power-assisted superficial liposuction combined with endoscopic-assisted pull-through excision. Ann. Plast. Surg. 2005, 55, 591–594. [Google Scholar] [CrossRef]
- Innocenti, A.; Melita, D.; Ghezzi, S. Closed-Suction Drains After Subcutaneous Mastectomy for Gynecomastia: Do they Reduce Complications? Aesthetic Plast. Surg. 2019, 43, 1124–1125. [Google Scholar] [CrossRef]

| Variable | Median (Range) or n (%) |
|---|---|
| Age (years) | 14.5 (13.6–17.4) |
| Weight (kg) | 68 (56–94) |
| Height (cm) | 174 (162–184) |
| Body Mass Index (kg/m2) | 24.5 (23.1–26.2) |
| Simon Grade I | 6 (28.6%) |
| Simon Grade II | 12 (57.1%) |
| Simon Grade III | 3 (14.3%) |
| Bilateral surgery | 16 (76.2%) |
| Unilateral surgery | 5 (23.8%) |
| Mean resection weight (per breast, g) | 135 ± 22 |
| Outpatient discharge | 21 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delgado-Miguel, C.; Fuentes, E.; Aguado, P.; Díez, R. Gynecomastia Outpatient Surgical Treatment in Children Without Closed-Suction Drain Placement: Is It Safe and Effective? Children 2025, 12, 1571. https://doi.org/10.3390/children12111571
Delgado-Miguel C, Fuentes E, Aguado P, Díez R. Gynecomastia Outpatient Surgical Treatment in Children Without Closed-Suction Drain Placement: Is It Safe and Effective? Children. 2025; 12(11):1571. https://doi.org/10.3390/children12111571
Chicago/Turabian StyleDelgado-Miguel, Carlos, Ennio Fuentes, Pablo Aguado, and Ricardo Díez. 2025. "Gynecomastia Outpatient Surgical Treatment in Children Without Closed-Suction Drain Placement: Is It Safe and Effective?" Children 12, no. 11: 1571. https://doi.org/10.3390/children12111571
APA StyleDelgado-Miguel, C., Fuentes, E., Aguado, P., & Díez, R. (2025). Gynecomastia Outpatient Surgical Treatment in Children Without Closed-Suction Drain Placement: Is It Safe and Effective? Children, 12(11), 1571. https://doi.org/10.3390/children12111571







