Efficacy of Endoscopic Retrograde Cholangiopancreatography and Frey Procedure in the Treatment of Pediatric Pancreatic Duct Stones: A Single-Center Retrospective Cohort Study
Abstract
1. Introduction
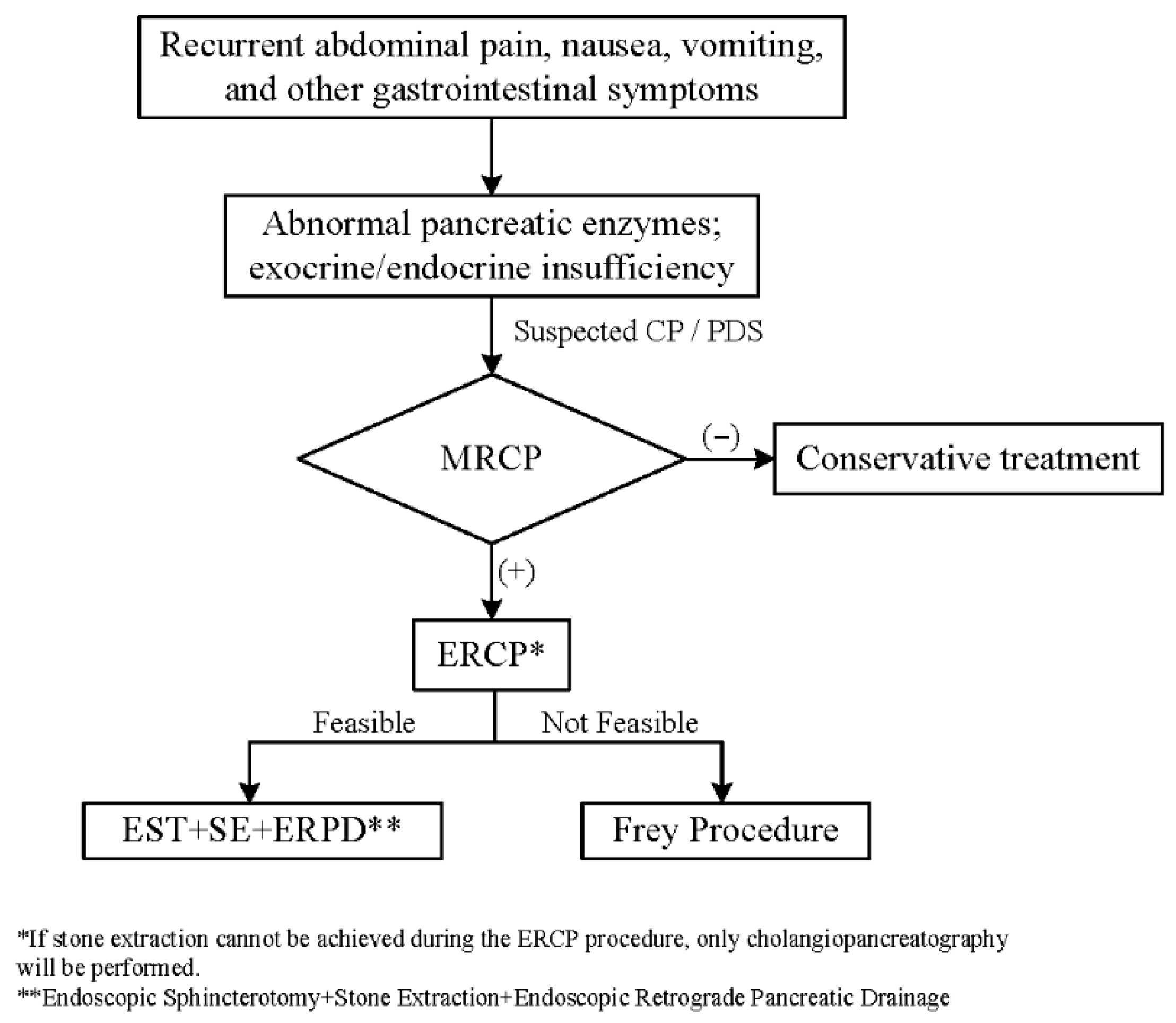
2. Data and Methods
2.1. Clinical Data
2.2. Surgical Approaches
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
Abbreviations
| ERCP | Endoscopic retrograde cholangiopancreatography |
| PDS | Pancreatic duct stones |
| CP | Chronic pancreatitis |
| BMI | Body mass index |
| DMPDD | Degree of main pancreatic duct dilatation |
| DT | Duration of treatment |
| WBC | White blood cell |
| CRP | C-reactive protein |
| AMY | Amylase |
| LIP | Lipase |
| ALT | Alanine aminotransferase |
| TB | Total bilirubin |
| FBG | Fasting blood glucose |
| ALB | Albumin |
| PR | Pain relief |
| MI | Multiple interventions |
| PP | Postoperative pancreatitis |
| PB | Postoperative bleeding |
| PF | Pancreatic fistula |
| IAI | Intra-abdominal infection |
| SR | Stone recurrence |
| TP-IAT | Total pancreatectomy with islet autotransplantation |
References
- Beyna, T.; Neuhaus, H.; Gerges, C. Endoscopic treatment of pancreatic duct stones under direct vision: Revolution or resignation? Systematic review. Dig. Endosc. 2018, 30, 29–37. [Google Scholar] [CrossRef]
- Tandan, M.; Nageshwar Reddy, D. Endotherapy in chronic pancreatitis. World J. Gastroenterol. 2013, 19, 6156–6164. [Google Scholar] [CrossRef] [PubMed]
- Ammann, R.W.; Muench, R.; Otto, R.; Buehler, H.; Freiburghaus, A.U.; Siegenthaler, W. Evolution and regression of pancreatic calcification in chronic pancreatitis. A prospective long-term study of 107 patients. Gastroenterology 1988, 95, 1018–1028. [Google Scholar] [CrossRef]
- Rösch, T.; Daniel, S.; Scholz, M.; Huibregtse, K.; Smits, M.; Schneider, T.; Ell, C.; Haber, G.; Riemann, J.F.; Jakobs, R.; et al. Endoscopic treatment of chronic pancreatitis: A multicenter study of 1000 patients with long-term follow-up. Endoscopy 2002, 34, 765–771. [Google Scholar] [CrossRef]
- Makita, S.; Amano, H.; Kawashima, H.; Hinoki, A.; Shirota, C.; Tainaka, T.; Sumida, W.; Yokota, K.; Okamoto, M.; Takimoto, A.; et al. Utility of endoscopic retrograde cholangiopancreatography in management of pediatric pancreaticobiliary disease. BMC Pediatr. 2022, 22, 134. [Google Scholar] [CrossRef] [PubMed]
- Boam, T.; Gabriel, M.; Rogoyski, B.G.; Ram, A.D.; Awan, A. Surgical drainage procedures for paediatric chronic pancreatitis: A scoping review. Pediatr. Surg. Int. 2022, 38, 1949–1964. [Google Scholar] [CrossRef] [PubMed]
- Ceppa, E.P.; Pitt, H.A.; Hunter, J.L.; Leys, C.M.; Zyromski, N.J.; Rescorla, F.J.; Sandrasegaran, K.; Fogel, E.L.; McHenry, L.W.; Watkins, J.L.; et al. Hereditary pancreatitis: Endoscopic and surgical management. J. Gastrointest. Surg. 2013, 17, 847–857. [Google Scholar] [CrossRef]
- Kohoutova, D.; Tringali, A.; Papparella, G.; Perri, V.; Boškoski, I.; Hamanaka, J.; Costamagna, G. Endoscopic treatment of chronic pancreatitis in pediatric population: Long-term efficacy and safety. United Eur. Gastroenterol. J. 2019, 7, 270–277. [Google Scholar] [CrossRef]
- Randall, M.M.; McDaniels, S.; Kyle, K.; Michael, M.; Giacopuzzi, J.; Brown, L.A. Pancreatitis in pre-adolescent children: A 10 year experience in the pediatric emergency department. BMC Emerg. Med. 2019, 19, 71. [Google Scholar] [CrossRef]
- Buxbaum, J.L.; Freeman, M.; Amateau, S.K.; Chalhoub, J.M.; Coelho-Prabhu, N.; Desai, M.; Elhanafi, S.E.; Forbes, N.; Fujii-Lau, L.L.; Kohli, D.R.; et al. American Society for Gastrointestinal Endoscopy guideline on post-ERCP pancreatitis prevention strategies: Summary and recommendations. Gastrointest. Endosc. 2023, 97, 153–162. [Google Scholar] [CrossRef]
- Sheth, S.G.; Machicado, J.D.; Chalhoub, J.M.; Forsmark, C.; Zyromski, N.; Thosani, N.C.; Thiruvengadam, N.R.; Ruan, W.; Pawa, S.; Ngamruengphong, S.; et al. American Society for Gastrointestinal Endoscopy guideline on the role of endoscopy in the management of chronic pancreatitis: Summary and recommendations. Gastrointest. Endosc. 2024, 100, 584–594. [Google Scholar] [CrossRef]
- Hosseini, A.; Sohouli, M.H.; Sharifi, E.; Sayyari, A.; Sridharan, K.; Tajalli, S.; Imanzadeh, N.; Fatahi, S. Indications, success, and adverse event rates of pediatric endoscopic retrograde cholangiopancreatography (ERCP): A systematic review and meta-analysis. BMC Pediatr. 2023, 23, 596. [Google Scholar] [CrossRef]
- Keane, M.G.; Kumar, M.; Cieplik, N.; Thorburn, D.; Johnson, G.J.; Webster, G.J.; Chapman, M.H.; Lindley, K.J.; Pereira, S.P. Paediatric pancreaticobiliary endoscopy: A 21-year experience from a tertiary hepatobiliary centre and systematic literature review. BMC Pediatr. 2018, 18, 42. [Google Scholar] [CrossRef] [PubMed]
- Rosen, J.D.; Lane, R.S.; Martinez, J.M.; Perez, E.A.; Tashiro, J.; Wagenaar, A.E.; Van Haren, R.M.; Kumar, A.; Sola, J.E. Success and safety of endoscopic retrograde cholangiopancreatography in children. J. Pediatr. Surg. 2017, 52, 1148–1151. [Google Scholar] [CrossRef]
- Frey, C.F.; Smith, G.J. Description and rationale of a new operation for chronic pancreatitis. Pancreas 1987, 2, 701–707. [Google Scholar] [CrossRef]
- Ray, S.; Ansari, Z.; Kumar, D.; Jana, K.; Khamrui, S. Short- and long-term outcome of surgery for chronic pancreatitis in children: A single surgeon experience. Pediatr. Surg. Int. 2020, 36, 1087–1092. [Google Scholar] [CrossRef]
- Tan, C.-L.; Zhang, H.; Li, K.-Z. Single center experience in selecting the laparoscopic Frey procedure for chronic pancreatitis. World J. Gastroenterol. 2015, 21, 12644–12652. [Google Scholar] [CrossRef]
- Kempeneers, M.A.; van Hemert, A.K.E.; van der Hoek, M.; Issa, Y.; van Hooft, J.E.; Nio, C.Y.; Busch, O.R.; van Santvoort, H.C.; Besselink, M.G.; Boermeester, M.A. Short- and long-term outcomes of selective use of Frey or extended lateral pancreaticojejunostomy in chronic pancreatitis. Br. J. Surg. 2022, 109, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Li, S.; Hou, S.; Zhang, L.; Chen, S.; Wang, J.; Lv, J.; Wu, Y.; Huang, Q.; Li, Y. ERCP-Related adverse events in pediatric patients: A 10-years single-site review. Pediatr. Surg. Int. 2024, 40, 199. [Google Scholar] [CrossRef]
- Poddar, U.; Thapa, B.R.; Bhasin, D.K.; Prasad, A.; Nagi, B.; Singh, K. Endoscopic retrograde cholangiopancreatography in the management of pancreaticobiliary disorders in children. J. Gastroenterol. Hepatol. 2001, 16, 927–931. [Google Scholar] [CrossRef] [PubMed]
- Kempeneers, M.A.; Issa, Y.; Ali, U.A.; Baron, R.D.; Besselink, M.G.; Büchler, M.; Erkan, M.; Fernandez-Del Castillo, C.; Isaji, S.; Izbicki, J.; et al. International consensus guidelines for surgery and the timing of intervention in chronic pancreatitis. Pancreatology 2020, 20, 149–157. [Google Scholar] [CrossRef]
- Durakbasa, C.U.; Balik, E.; Yamaner, S.; Bulut, T.; Büyükuncu, Y.; Sökücü, N.; Akyüz, A.; Bugra, D. Diagnostic and therapeutic endoscopic retrograde cholangiopancreatography (ERCP) in children and adolescents: Experience in a single institution. Eur. J. Pediatr. Surg. 2008, 18, 241–244. [Google Scholar] [CrossRef]
- Rocca, R.; Castellino, F.; Daperno, M.; Masoero, G.; Sostegni, R.; Ercole, E.; Lavagna, A.; Barbera, C.; Canavese, F.; Pera, A. Therapeutic ERCP in paediatric patients. Dig. Liver Dis. 2005, 37, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Rollins, M.D.; Meyers, R.L. Frey procedure for surgical management of chronic pancreatitis in children. J. Pediatr. Surg. 2004, 39, 817–820. [Google Scholar] [CrossRef]
- Ray, S.; Sanyal, S.; Ghatak, S.; Khamrui, S.; Biswas, J.; Saha, S.; Mandal, T.S.; Chattopadhyay, G. Frey procedure for chronic pancreatitis in children: A single center experience. J. Pediatr. Surg. 2015, 50, 1850–1853. [Google Scholar] [CrossRef]
- Zhou, Y.; Shi, B.; Wu, L.; Wu, X.; Li, Y. Frey procedure for chronic pancreatitis: Evidence-based assessment of short- and long-term results in comparison to pancreatoduodenectomy and Beger procedure: A meta-analysis. Pancreatology 2015, 15, 372–379. [Google Scholar] [CrossRef]
- Jeropoulos, R.M.; Joshi, D.; Aldeiri, B.; Davenport, M. Surgical and Endoscopic Intervention for Chronic Pancreatitis in Children: The Kings College Hospital Experience. Children 2024, 11, 74. [Google Scholar] [CrossRef]
- Pappas, S.G.; Pilgrim, C.H.C.; Keim, R.; Harris, R.; Wilson, S.; Turaga, K.; Tsai, S.; Dua, K.; Khan, A.; Oh, Y.; et al. The Frey procedure for chronic pancreatitis secondary to pancreas divisum. JAMA Surg. 2013, 148, 1057–1062. [Google Scholar] [CrossRef]
- Ray, S.; Basu, C.; Dhali, A.; Dhali, G.K. Frey procedure for chronic pancreatitis: A narrative review. Ann. Med. Surg. 2022, 80, 104229. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; You, Y.; Yan, H.; He, J.; Gong, J.; Wei, S. Drainage procedure for pancreatolithiasis: Re-examination of the pancreatic duct diameter standard. Ann. Surg. Treat. Res. 2020, 98, 190–198. [Google Scholar] [CrossRef] [PubMed]
- Green, J.A.; Scheeres, D.E.; Conrad, H.A.; Cloney, D.L.; Schlatter, M.G. Pediatric ERCP in a multidisciplinary community setting: Experience with a fellowship-trained general surgeon. Surg. Endosc. 2007, 21, 2187–2192. [Google Scholar] [CrossRef]
- Rieder, S.; Michalski, C.W.; Friess, H. Indications for endoscopic or surgical treatment of chronic pancreatitis. Dig. Dis. 2010, 28, 344–349. [Google Scholar] [CrossRef]
- Teng, R.; Yokohata, K.; Utsunomiya, N.; Takahata, S.; Nabae, T.; Tanaka, M. Endoscopic retrograde cholangiopancreatography in infants and children. J. Gastroenterol. 2000, 35, 39–42. [Google Scholar] [CrossRef]
- Iqbal, C.W.; Baron, T.H.; Moir, C.R.; Ishitani, M.B. Post-ERCP pancreatitis in pediatric patients. J. Pediatr. Gastroenterol. Nutr. 2009, 49, 430–434. [Google Scholar] [CrossRef]
- Lorio, E.; Moreau, C.; Hernandez, B.; Rabbani, T.; Michaud, K.; Hachem, J.; Aggarwal, P.; Stolow, E.; Brown, L.; Michalek, J.E.; et al. Pediatric ERCP: Factors for Success and Complication-A 17-Year, Multisite Experience. J. Pediatr. Gastroenterol. Nutr. 2023, 77, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Ueda, J.; Miyasaka, Y.; Ohtsuka, T.; Takahata, S.; Tanaka, M. Short- and long-term results of the Frey procedure for chronic pancreatitis. J. Hepatobiliary Pancreat. Sci. 2015, 22, 211–216. [Google Scholar] [CrossRef]
- Khatkov, I.; Izrailov, R.; Tsvirkun, V.; Alikhanov, R.; Vasnev, O.; Dyuzheva, T.; Egorov, V.; Dalgatov, K.; Baychorov, M.; Agami, P.; et al. Laparoscopic versus open Frey procedure: Comparative analysis of short and long-term outcomes. Pancreatology 2022, 22, 1181–1186. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.; Luo, J.; Yang, H.; Yang, J.; Bian, H.; Duan, X.; Wang, X. Pediatric endoscopic retrograde pancreatography expertise in chronic pancreatitis: A single-center analysis. Front. Pediatr. 2025, 13, 1491579. [Google Scholar] [CrossRef]
- Suzumura, K.; Hatano, E.; Okada, T.; Asano, Y.; Uyama, N.; Nakamura, I.; Hai, S.; Fujimoto, J. Short- and long-term outcomes of the Frey procedure for chronic pancreatitis: A single-center experience and summary of outcomes in Japan. Surg. Today 2018, 48, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Diener, M.K.; Rahbari, N.N.; Fischer, L.; Antes, G.; Büchler, M.W.; Seiler, C.M. Duodenum-preserving pancreatic head resection versus pancreatoduodenectomy for surgical treatment of chronic pancreatitis: A systematic review and meta-analysis. Ann. Surg. 2008, 247, 950–961. [Google Scholar] [CrossRef]
- Allen, C.J.; Yakoub, D.; Macedo, F.I.; Dosch, A.R.; Brosch, J.; Dudeja, V.; Ayala, R.; Merchant, N.B. Long-term Quality of Life and Gastrointestinal Functional Outcomes After Pancreaticoduodenectomy. Ann. Surg. 2018, 268, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Strate, T.; Bachmann, K.; Busch, P.; Mann, O.; Schneider, C.; Bruhn, J.P.; Yekebas, E.; Kuechler, T.; Bloechle, C.; Izbicki, J.R. Resection vs drainage in treatment of chronic pancreatitis: Long-term results of a randomized trial. Gastroenterology 2008, 134, 1406–1411. [Google Scholar] [CrossRef] [PubMed]

| Clinical Data | ERCP (n = 32) | Frey (n = 33) | p | Test Statistic |
|---|---|---|---|---|
| Gender (n) | 0.914 | 0.012 | ||
| Male | 18 | 19 | ||
| Female | 14 | 14 | ||
| Age (y) | 13 (8.77, 16) | 14(12, 15.5) | 0.425 | 0.798 |
| Height (cm) | 157 (132.25, 163.25) | 160 (148.5, 167) | 0.215 | 1.213 |
| Weight (kg) | 39.86 ± 15.94 | 43.70 ± 14.27 | 0.310 | 0.694 |
| BMI | 17.46 (14.41, 18.75) | 17.35 (14.85, 18.95) | 0.808 | 0.243 |
| Stone Type (n) | 0.384 | 0.757 | ||
| Single | 13 | 10 | ||
| Multiple | 19 | 23 | ||
| Stone Size (mm) | 7.12 ± 1.08 | 7.67 ± 1.49 | 0.094 | 1.699 |
| Stone Location | 0.524 | 1.294 | ||
| Head | 24 | 22 | ||
| Body | 8 | 10 | ||
| Tail | 0 | 1 | ||
| DMPDD (mm) | 6.45 ± 1.24 | 9.11 ± 1.38 | <0.001 | 8.166 |
| DT (m) | 4.4 (2.3, 6.7) | 1.8 (0.9, 2.9) | <0.001 | 4.822 |
| WBC (×109/L) | 7.04 (4.92, 8.72) | 6.17 (5.24, 8.3) | 0.568 | −0.571 |
| CRP (mg/L) | 7.23 (3.48, 10.97) | 7.56 (4.01, 11.35) | 0.096 | 0.052 |
| AMY (U/L) | 151 (71, 385) | 109 (60, 310) | 0.201 | −1.280 |
| LIP (U/L) | 127 (65, 276) | 138 (72, 245) | 0.679 | 0.420 |
| ALT (U/L) | 35 (28, 81) | 37 (25, 94) | 0.660 | 0.446 |
| TB (μmol/L) | 16.8 (12.1, 25.1) | 18.1 (11.9, 26.4) | 0.332 | 0.978 |
| FBG (mmol/L) | 5.16 (4.19, 6.38) | 5.21 (4.35, 6.51) | 0.273 | 1.102 |
| ALB (g/L) | 37 (33, 42) | 36 (32, 43) | 0.372 | −0.899 |
| Clinical Data | ERCP (n = 32) | Frey (n = 33) | p | Test Statistic |
|---|---|---|---|---|
| WBC (×109/L) | 6.11 (4.28, 7.13) | 5.35 (4.36, 7.64) | 0.922 | −0.105 |
| CRP (mg/L) | 1.35 (0.87, 2.02) | 1.69 (0.98, 2.25) | 0.906 | −0.125 |
| AMY (U/L) | 52 (31, 78) | 49 (32, 69) | 0.494 | 0.689 |
| LIP (U/L) | 38 (21, 52) | 35 (18, 55) | 0.404 | 0.840 |
| ALT (U/L) | 19 (8, 33) | 17 (7, 32) | 0.896 | −0.138 |
| ALT (μmol/L) | 10.6 (6.2, 15.3) | 11.3 (7.8, 16.4) | 0.586 | −0.551 |
| FBG (mmol/L) | 4.93 (4.28, 5.91) | 5.03 (4.41, 5.89) | 0.894 | 0.138 |
| ALB (g/L) | 42 (38, 47) | 41 (38, 49) | 0.579 | 0.558 |
| Outcomes | ERCP (n = 32) | Frey (n = 33) | p | Test Statistic |
|---|---|---|---|---|
| PP (n) | 3 | 3 | 0.968 | 0.002 |
| PB (n) | 1 | 2 | 0.573 | 0.318 |
| PF (n) | 0 | 1 | 0.321 | 0.985 |
| IAI (n) | 0 | 2 | 0.486 | 0.485 |
| PR (n) | 28 | 30 | 0.966 | 0.003 |
| SR (n) | 13 | 3 | 0.003 | 8.706 |
| MI (times) | 3.98 ± 0.52 | 1.27 ± 0.91 | <0.001 | 14.68 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xie, Z.; Deng, Y.; Luo, C.; Peng, Y.; Chen, Y.; Song, J. Efficacy of Endoscopic Retrograde Cholangiopancreatography and Frey Procedure in the Treatment of Pediatric Pancreatic Duct Stones: A Single-Center Retrospective Cohort Study. Children 2025, 12, 1555. https://doi.org/10.3390/children12111555
Xie Z, Deng Y, Luo C, Peng Y, Chen Y, Song J. Efficacy of Endoscopic Retrograde Cholangiopancreatography and Frey Procedure in the Treatment of Pediatric Pancreatic Duct Stones: A Single-Center Retrospective Cohort Study. Children. 2025; 12(11):1555. https://doi.org/10.3390/children12111555
Chicago/Turabian StyleXie, Zhenyu, Yifan Deng, Chengkun Luo, Yun Peng, Yang Chen, and Jiulin Song. 2025. "Efficacy of Endoscopic Retrograde Cholangiopancreatography and Frey Procedure in the Treatment of Pediatric Pancreatic Duct Stones: A Single-Center Retrospective Cohort Study" Children 12, no. 11: 1555. https://doi.org/10.3390/children12111555
APA StyleXie, Z., Deng, Y., Luo, C., Peng, Y., Chen, Y., & Song, J. (2025). Efficacy of Endoscopic Retrograde Cholangiopancreatography and Frey Procedure in the Treatment of Pediatric Pancreatic Duct Stones: A Single-Center Retrospective Cohort Study. Children, 12(11), 1555. https://doi.org/10.3390/children12111555






