The Body as a Battlefield: Identity Development and Psychosomatic Expression in Eating Disorders Across Childhood and Adolescence
Highlights
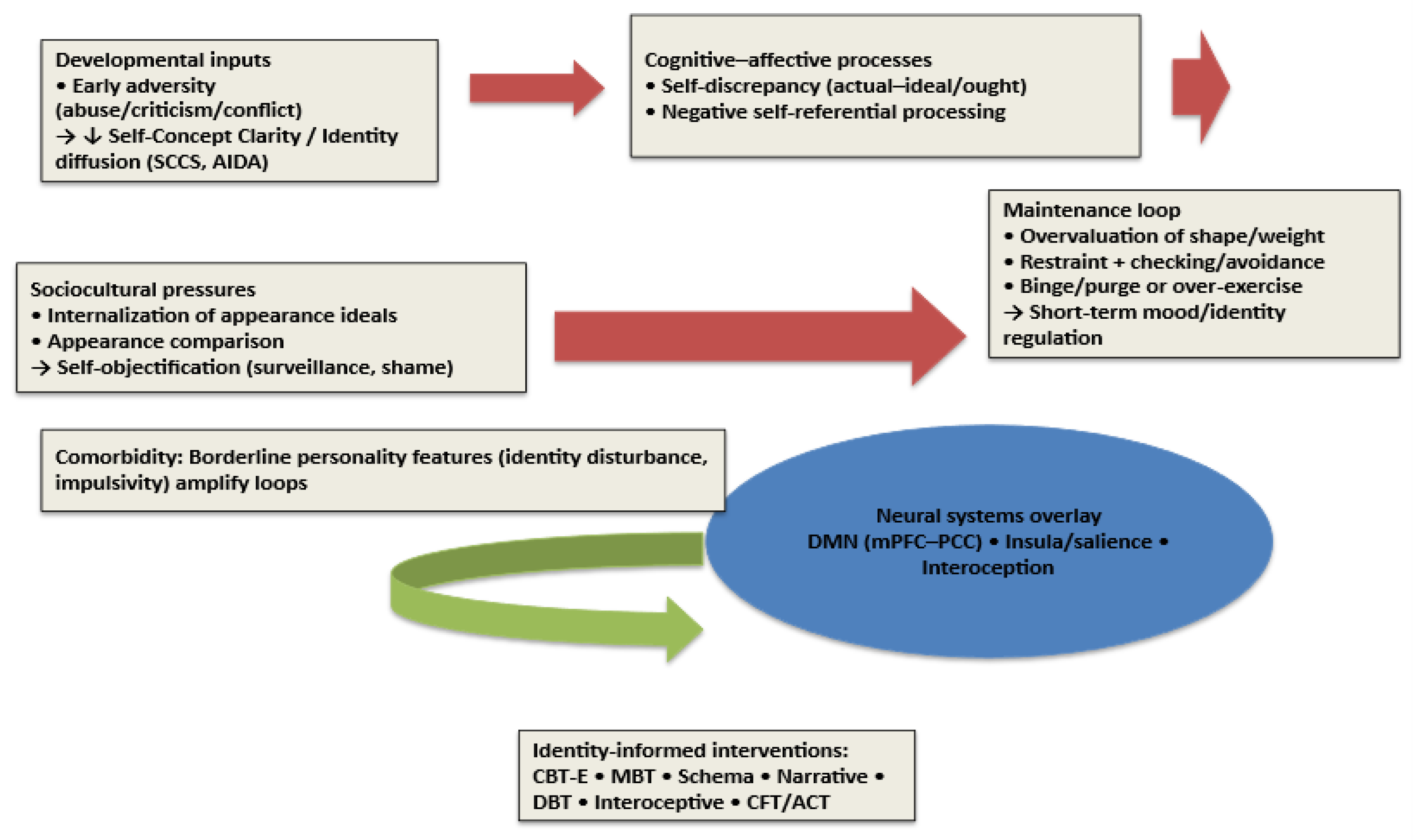
- Identity disturbance links early adversity to eating disorders.
- Low self-concept clarity and self-objectification maintain symptoms.
- Identity-focused therapies may enhance recovery in young patients.
- Early identity screening can improve prevention and treatment.
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Screening and Selection Process
2.4. Data Extraction and Synthesis
2.5. Risk of Bias and Methodological Considerations
3. Conceptual Frameworks Linking Identity and EDs
3.1. Developmental Identity Theory and Self-Concept Clarity
3.2. Self-Discrepancy Theory
3.3. Self-Objectification Theory and Self-Objectification
3.4. Eating Disorders-Specific Maintenance Models: The Transdiagnostic Enhanced Cognitive-Behavioral Therapy (CBT-E) Model
4. Developmental and Psychosocial Pathways
4.1. From Early Adversity to Identity Disruption, Sociocultural Pressures, Body Dissatisfaction, and ED Symptoms
4.2. Sociocultural and Developmental Influences
4.3. Identity Development Status and Clinical Course
4.4. Shame, Self-Blame, and Hostile Self-Attitudes
5. Neurocognitive and Neurobiological Correlates of the “Self” in EDs
5.1. Self-Referential Processing and the Default Mode Network (DMN)
5.2. Interoception and Insular Cortex
5.3. Body-Image Processing Networks
6. Clinical Phenomenology Across Diagnoses
6.1. Anorexia Nervosa (AN)
6.2. Bulimia Nervosa (BN) and Binge-Eating Disorder (BED)
6.3. Comorbidity with Borderline Personality Features
6.4. Childhood-Specific Clinical Aspects
7. Treatment Implications: Targeting Identity to Augment Standard Care
7.1. Evidence-Based ED Treatments and Identity
7.2. Mentalization-Based Approaches
7.3. Schema Therapy
7.4. Narrative Therapy and Identity Reconstruction
7.5. Skills for Emotion/Impulse Regulation: DBT-Informed (DBT-BED)
7.6. Integration of Identity-Focused Approaches
8. Psychodynamic Perspective and Psychodynamic Therapy in EDs
9. Discussion: What Is the Future for Research and Care?
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACT | Acceptance and Commitment Therapy |
| AFT | Adolescent-Focused Psychotherapy |
| AIDA | Assessment of Identity Development in Adolescence |
| AN | Anorexia Nervosa |
| BED | Binge-Eating Disorder |
| BMI | Body Mass Index |
| BN | Bulimia Nervosa |
| BPD | Borderline Personality Disorder |
| CBT-E | Enhanced Cognitive-Behavioral Therapy For Eating Disorders |
| CFT | Compassion-Focused Therapy |
| DBT | Dialectical Behavior Therapy |
| DBT-BED | DBT Adapted for Binge-Eating Disorder. |
| DERS | Difficulties in Emotion Regulation Scale |
| DMN | Default Mode Network |
| ED | Eating Disorder |
| EDE-Q | Eating Disorder Examination–Questionnaire |
| FBT | Family-Based Treatment |
| fMRI | Functional Magnetic Resonance Imaging |
| FPT | Focal Psychodynamic Therapy |
| GST | Group Schema Therapy |
| MAIA | Multidimensional Assessment of Interoceptive Awareness |
| MBT | Mentalization-Based Therapy |
| MBT-ED | Mentalization-Based Therapy for Eating Disorders |
| mPFC | Medial Prefrontal Cortex |
| OBCS | Objectified Body Consciousness Scale |
| PACS/PACS-3 | Physical Appearance Comparison Scale (versions 1 and 3) |
| PCC | Posterior Cingulate Cortex |
| RCT | Randomized Controlled Trial |
| rTMS | Repetitive Transcranial Magnetic Stimulation |
| SASB | Structural Analysis of Social Behavior |
| SCC | Self-Concept Clarity |
| SCCS | Self-Concept Clarity Scale |
| SMI-ED | Schema Mode Inventory—Eating Disorders |
| SSCM-ED | Specialist Supportive Clinical Management—Eating Disorders |
| tDCS | Transcranial Direct Current Stimulation |
| Δ | Change (post-pre) |
References
- Vartanian, L.R.; Hayward, L.E.; Smyth, J.M.; Paxton, S.J.; Touyz, S.W. Risk and resiliency factors related to body dissatisfaction and disordered eating: The identity disruption model. Int. J. Eat. Disord. 2018, 51, 322–330. [Google Scholar] [CrossRef] [PubMed]
- Vartanian, L.R.; Nicholls, K.; Fardouly, J. Testing the Identity Disruption Model among adolescents: Pathways connecting adverse childhood experiences to body dissatisfaction. J. Youth Adolesc. 2023, 52, 134–148. [Google Scholar] [CrossRef] [PubMed]
- Verschueren, M.; Claes, L.; Palmeroni, N.; Raemen, L.; Moons, P.; Bruckers, L.; Molenberghs, G.; Dierckx, E.; Schoevaerts, K.; Luyckx, K. Identity functioning in patients with an eating disorder: Developmental trajectories throughout treatment. Nutrients 2024, 16, 591. [Google Scholar] [CrossRef] [PubMed]
- Higgins, E.T. Self-discrepancy: A theory relating self and affect. Psychol. Rev. 1987, 94, 319–340. [Google Scholar] [CrossRef]
- Fredrickson, B.L.; Roberts, T.-A. Objectification theory: Toward understanding women’s lived experiences and mental health risks. Psychol. Women Q. 1997, 21, 173–206. [Google Scholar] [CrossRef]
- Daniels, E.A.; Zurbriggen, E.L.; Ward, L.M. Becoming an object: A review of self-objectification in girls. Body Image 2020, 33, 278–299. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Cooper, Z.; Shafran, R. Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behav. Res. Ther. 2003, 41, 509–528. [Google Scholar] [CrossRef]
- Chen, X.; Ai, C.; Liu, Z.; Wang, G. Neuroimaging studies of resting-state functional magnetic resonance imaging in eating disorders. BMC Med. Imaging 2024, 24, 265. [Google Scholar] [CrossRef]
- Gondo, M.; Kawai, K.; Moriguchi, Y.; Hiwatashi, A.; Takakura, S.; Yoshihara, K.; Morita, C.; Yamashita, M.; Eto, S.; Sudo, N. Effects of integrated hospital treatment on the default mode, salience, and frontal-parietal networks in anorexia nervosa: A longitudinal resting-state functional magnetic resonance imaging study. PLoS ONE 2023, 18, e0283318. [Google Scholar] [CrossRef]
- Ayrolles, A.; Clarke, J.; Godart, N.; André-Carletti, C.; Barbe, C.; Bargiacchi, A.; Blanchet, C.; Bergametti, F.; Bertrand, V.; Caldagues, E.; et al. Early-onset anorexia nervosa: A scoping review and management guidelines. J. Eat. Disord. 2024, 12, 182. [Google Scholar] [CrossRef]
- Verschueren, M.; Rassart, J.; Claes, L.; Moons, P.; Luyckx, K. Identity statuses throughout adolescence and emerging adulthood: A meta-analysis. Eur. J. Pers. 2017, 31, 385–403. [Google Scholar] [CrossRef]
- Goth, K.; Foelsch, P.; Schlüter-Müller, S.; Birkhölzer, M.; Jung, E.; Pick, O.; Schmeck, K. Assessment of identity development and identity diffusion in adolescence: Theoretical basis and psychometric properties of the self-report questionnaire AIDA. Child Adolesc. Psychiatry Ment. Health 2012, 6, 27. [Google Scholar] [CrossRef]
- Erikson, E.H. Identity: Youth and Crisis; W.W. Norton: New York, NY, USA, 1968. [Google Scholar]
- Marcia, J.E. Development and validation of ego-identity status. J. Pers. Soc. Psychol. 1966, 3, 551–558. [Google Scholar] [CrossRef]
- Kroger, J.; Martinussen, M.; Marcia, J.E. Identity status change during adolescence and young adulthood: A meta-analysis. J. Adolesc. 2010, 33, 683–698. [Google Scholar] [CrossRef]
- Smink, F.R.E.; van Hoeken, D.; Hoek, H.W. Epidemiology of eating disorders: Incidence, prevalence and mortality rates. Curr. Psychiatry Rep. 2012, 14, 406–414. [Google Scholar] [CrossRef]
- van Eeden, A.E.; van Hoeken, D.; Hoek, H.W. Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Curr. Opin. Psychiatry 2021, 34, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.D.; Trapnell, P.D.; Heine, S.J.; Katz, I.M.; Lavallee, L.F.; Lehman, D.R. Self-concept clarity: Measurement, personality correlates, and cultural boundaries. J. Pers. Soc. Psychol. 1996, 70, 141–156. [Google Scholar] [CrossRef]
- van den Berg, P.; Thompson, J.K.; Obremski-Brandon, K.; Coovert, M. The Tripartite Influence model of body image and eating disturbance: A covariance structure modeling investigation testing the mediational role of appearance comparison. J. Psychosom. Res. 2002, 53, 1007–1020. [Google Scholar] [CrossRef] [PubMed]
- Keery, H.; van den Berg, P.; Thompson, J.K. An evaluation of the Tripartite Influence Model of body dissatisfaction and eating disturbance with adolescent girls. Body Image 2004, 1, 237–251. [Google Scholar] [CrossRef]
- Budde, L.; Haenschel, C.; Herpertz-Dahlmann, B.; Konrad, K. Influence of identity development on weight gain in adolescent anorexia nervosa. Front. Psychiatry 2022, 13, 887588. [Google Scholar] [CrossRef]
- Simpson, S.G.; McDonald, J.; Stewart, C. Factorial structure and validation of the Schema Mode Inventory for Eating Disorders (SMI-ED). Front. Psychol. 2018, 9, 600. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, L.M.; Burke, N.L.; Calogero, R.M.; Menzel, J.E.; Krawczyk, R.; Thompson, J.K. Self-objectification, body shame, and disordered eating: Testing a core mediational model of objectification theory among White, Black, and Hispanic women. Body Image 2018, 24, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Karsay, K.; Knoll, J.; Matthes, J. Sexualizing media use and self-objectification: A meta-analysis. Psychol. Women Q. 2018, 42, 9–28. [Google Scholar] [CrossRef] [PubMed]
- Bonfanti, R.C.; Melchiori, F.; Teti, A.; Albano, G.; Raffard, S.; Rodgers, R.; Lo Coco, G. The association between social comparison in social media, body image concerns and eating disorder symptoms: A systematic review and meta-analysis. Body Image 2025, 52, 101841. [Google Scholar] [CrossRef]
- Strauman, T.J.; Vookles, J.; Berenstein, V.; Chaiken, S.; Higgins, E.T. Self-discrepancies and vulnerability to body dissatisfaction and disordered eating. J. Pers. Soc. Psychol. 1991, 61, 946–956. [Google Scholar] [CrossRef]
- Mason, T.B.; Smith, K.E.; Engwall, A.; Lass, A.; Mead, M.; Sorby, M.; Bjorlie, K.; Strauman, T.J.; Wonderlich, S. Self-discrepancy theory as a transdiagnostic framework: A meta-analysis of self-discrepancy and psychopathology. Psychol. Bull. 2019, 145, 372–389. [Google Scholar] [CrossRef]
- Mason, T.B.; Lavender, J.M.; Wonderlich, S.A.; Crosby, R.D.; Engel, S.G.; Strauman, T.J.; Mitchell, J.E.; Crow, S.J.; Le Grange, D.; Klein, M.H.; et al. Self-discrepancy and eating disorder symptoms across eating disorder diagnostic groups. Eur. Eat. Disord. Rev. 2016, 24, 541–545. [Google Scholar] [CrossRef]
- Anton, S.D.; Perri, M.G.; Riley, J.R. III. Discrepancy between actual and ideal body images: Impact on eating and exercise behaviors. Eat. Behav. 2000, 1, 153–160. [Google Scholar] [CrossRef]
- Hernández-López, M.; Quiñones-Jiménez, L.; Blanco-Romero, A.L.; Rodríguez-Valverde, M. Testing the discrepancy between actual and ideal body image with the IRAP. J. Eat. Disord. 2021, 9, 82. [Google Scholar] [CrossRef]
- Boyd, H.K.; Bodell, L.P.; Jennings, K.M.; Graham, A.K.; Crosby, R.D.; Wildes, J.E. Relationship between desired weight constructs and eating disorder severity following treatment for anorexia nervosa. Int. J. Eat. Disord. 2018, 51, 870–878. [Google Scholar] [CrossRef]
- Rienecke, R.D.; Ebeling, M. Desired weight and treatment outcome among adolescents in a novel family-based partial hospitalization program. Psychiatry Res. 2019, 273, 149–152. [Google Scholar] [CrossRef] [PubMed]
- Moradi, B.; Huang, Y.-P. Objectification theory and psychology of women: A decade of advances and future directions. Psychol. Women Q. 2008, 32, 377–398. [Google Scholar] [CrossRef]
- Schaefer, L.M.; Thompson, J.K. Self-objectification and disordered eating: A meta-analysis. Int. J. Eat. Disord. 2018, 51, 483–502. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, K.S.; Mazzeo, S.E. Evaluation of a structural model of objectification theory and eating disorder symptomatology among European American and African American undergraduate women. Psychol. Women Q. 2009, 33, 384–395. [Google Scholar] [CrossRef]
- Saunders, J.F.; Nutter, S.; Waugh, R.; Hayden, K.A. Testing body-related components of objectification theory: A meta-analysis of the relations between body shame, self-objectification, and body dissatisfaction. Body Image 2024, 50, 101738. [Google Scholar] [CrossRef]
- Fardouly, J.; Willburger, B.; Vartanian, L.R. Instagram use and young women’s body image concerns and self-objectification: Testing mediational pathways. New Media Soc. 2017, 20, 1380–1395. [Google Scholar] [CrossRef]
- Dane, A.; Bhatia, K. The social media diet: A scoping review to investigate the association between social media, body image and eating disorders amongst young people. PLoS Glob. Public Health 2023, 3, e0001091. [Google Scholar] [CrossRef]
- Bacevičienė, M.; Jankauskienė, R. Associations between self-objectification and lifestyle habits, body shame, and disordered eating in adults. Int. J. Environ. Res. Public Health 2022, 19, 8662. [Google Scholar] [CrossRef]
- Fairburn, C.G. Cognitive Behavior Therapy and Eating Disorders; Guilford Press: New York, NY, USA, 2008. [Google Scholar]
- Cooper, Z.; Fairburn, C.G. The Evolution of “Enhanced” Cognitive Behavior Therapy for Eating Disorders: Learning From Treatment Nonresponse. Cogn. Behav. Pract. 2011, 18, 394–402. [Google Scholar] [CrossRef]
- Williams, S.; Reid, M. “It’s like there are two people in my head”: A phenomenological exploration of anorexia nervosa and its relationship to the self. Psychol. Health 2012, 27, 798–815. [Google Scholar] [CrossRef]
- Conti, J.; Heywood, L.; Arcelus, J. Paper 2: A systematic review of narrative therapy treatment outcomes for eating disorders. J. Eat. Disord. 2022, 10, 116. [Google Scholar] [CrossRef]
- Croce, S.R.; Malcolm, A.C.; Ralph-Nearman, C.; Phillipou, A. Examining identity functioning in anorexia nervosa across illness and recovery stages. Int. J. Eat. Disord. 2024, 57, 1959–1968. [Google Scholar] [CrossRef]
- Srivastava, P.; Felonis, C.; Lin, M.; Clarke, K.; Juarascio, A. Reciprocal association between session-by-session change in overvaluation of shape and weight and session-by-session change in bulimia nervosa symptoms during cognitive behavior therapies. Eat. Disord. 2023, 31, 242–257. [Google Scholar] [CrossRef]
- Escandón-Nagel, N.; Peró-Cebollero, M.; Grau, A.; Soriano, J.; Feixas, G. Overvaluation of weight and shape in obesity: A comparative study between people with and without binge eating disorder. Front. Psychol. 2024, 15, 1414455. [Google Scholar] [CrossRef] [PubMed]
- Walker, D.C.; White, E.K.; Srinivasan, V.J. A meta-analysis of the relationships between body checking, body image avoidance, body image dissatisfaction, mood, and disordered eating. Int. J. Eat. Disord. 2018, 51, 745–770. [Google Scholar] [CrossRef] [PubMed]
- Lampard, A.M.; Byrne, S.M.; McLean, N. An evaluation of the enhanced cognitive-behavioural model of eating disorders. Behav. Res. Ther. 2011, 49, 529–535. [Google Scholar] [CrossRef] [PubMed]
- de Jong, M.; Spinhoven, P.; Korrelboom, K.; Deen, M.; van der Meer, I.; Danner, U.; van der Schuur, S.; Schoorl, M.; Hoek, H.W. Effectiveness of enhanced cognitive behavior therapy for eating disorders: A randomized controlled trial. Int. J. Eat. Disord. 2020, 53, 587–597. [Google Scholar] [CrossRef]
- Dalle Grave, R. Enhanced cognitive behaviour therapy for adolescents with eating disorders. Front. Psychiatry 2024, 15, 1375465. [Google Scholar] [CrossRef]
- Le Grange, D.; Lock, J.; Accurso, E.C.; Agras, W.S.; Darcy, A.; Forsberg, S.; Bryson, S.W. Relapse from remission at two- to four-year follow-up in two treatments for adolescent anorexia nervosa. J. Am. Acad. Child Adolesc. Psychiatry 2014, 53, 1162–1167. [Google Scholar] [CrossRef]
- Voswinkel, M.M.; van Voorst, Y.; van Furth, E.F. Externalizing your eating disorder: A qualitative interview study of patients’ experiences. J. Eat. Disord. 2021, 9, 133. [Google Scholar] [CrossRef]
- Vartanian, L.R.; Froreich, F.V.; Smyth, J.M. A serial mediation model testing early adversity, self-concept clarity, and thin-ideal internalization as predictors of body dissatisfaction. Body Image 2016, 19, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.S.; Fuller-Tyszkiewicz, M.; Utpala, R.; Yeung, V.W.; De Paoli, T.; Loughan, S.; Krug, I. Western Cultural Identification Explains Variations in the Objectification Model for Eating Pathology Across Australian Caucasians and Asian Women. Front. Psychol. 2016, 7, 1578. [Google Scholar] [CrossRef] [PubMed]
- Vandenbosch, L.; Fardouly, J.; Tiggemann, M. Social media and body image: Recent trends and future directions. Curr. Opin. Psychol. 2022, 45, 101289. [Google Scholar] [CrossRef] [PubMed]
- Rohde, J.; Obbarius, A.; Voigt, B.; Sarrar, L.; Biesenthal-Matthes, S.; Kind, C.-S.; Rose, M.; Hofmann, T. Differences and similarities in personality functioning across different types of eating disorders. Front. Psychiatry 2023, 14, 1155725. [Google Scholar] [CrossRef]
- Jarry, J.L. The meaning of body image for women with eating disorders. Can. J. Psychiatry 1998, 43, 367–374. [Google Scholar] [CrossRef]
- Forsén Mantilla, E.; Norring, C.; Birgegård, A. Self-image and 12-month outcome in females with eating disorders: Extending previous findings. J. Eat. Disord. 2019, 7, 15. [Google Scholar] [CrossRef]
- Petersson, S.; Birgegård, A.; Brudin, L.; Forsén Mantilla, E.; Monell, E.; Clinton, D.; Björck, C. Initial self-blame predicts eating disorder remission after 9 years. J. Eat. Disord. 2021, 9, 81. [Google Scholar] [CrossRef]
- Paranjothy, S.M.; Wade, T.D. A meta-analysis of disordered eating and its association with self-criticism and self-compassion. Int. J. Eat. Disord. 2024, 57, 473–536. [Google Scholar] [CrossRef]
- Gu, S.J.; Aimufua, I.; Pagliaccio, D.; Shankman, S.A.; Steinglass, J.E.; Auerbach, R.P.; Walsh, B.T.; Ranzenhofer, L.M. Self-referential processing in anorexia nervosa. Int. J. Eat. Disord. 2024, 57, 1055–1067. [Google Scholar] [CrossRef]
- Kaufmann, L.-K.; Hänggi, J.; Jäncke, L.; Baur, V.; Piccirelli, M.; Kollias, S.; Schnyder, U.; Martin-Soelch, C.; Milos, G. Disrupted longitudinal restoration of brain connectivity during weight normalization in severe anorexia nervosa. Transl. Psychiatry 2023, 13, 136. [Google Scholar] [CrossRef]
- Gaudio, S.; Wiemerslage, L.; Brooks, S.J.; Schiöth, H.B. A systematic review of resting-state functional-MRI studies in anorexia nervosa: Evidence for functional connectivity impairment in cognitive control and visuospatial and body-signal integration. Neurosci. Biobehav. Rev. 2016, 71, 578–589. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Yang, Y.; Zhang, Y.; Zhang, X.; Li, G. Neuroimaging studies of resting-state functional MRI in eating disorders: A review of the last decade. BMC Med. Imaging 2024, 24, 83. [Google Scholar] [CrossRef] [PubMed]
- Cowdrey, F.A.; Filippini, N.; Park, R.J.; Smith, S.M.; McCabe, C. Increased resting-state functional connectivity in the default mode network in recovered anorexia nervosa. Hum. Brain Mapp. 2014, 35, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Datta, N.; Hughes, A.; Modafferi, M.; Klabunde, M. An FMRI meta-analysis of interoception in eating disorders. Neuroimage 2025, 305, 120933. [Google Scholar] [CrossRef]
- Khalsa, S.S.; Berner, L.A.; Anderson, L.M. Gastrointestinal interoception in eating disorders: Charting a new path. Curr. Psychiatry Rep. 2022, 24, 47–60. [Google Scholar] [CrossRef]
- Menon, V. Insular cortex: A hub for saliency, cognitive control, and interoceptive awareness. In Encyclopedia of the Human Brain; Elsevier: Amsterdam, The Netherlands, 2024; pp. 159–183. [Google Scholar] [CrossRef]
- Boehm, I.; Mennigen, E.; Geisler, D.; Poller, N.W.; Gramatke, K.; Calhoun, V.D.; Roessner, V.; King, J.A.; Ehrlich, S. Dynamic functional connectivity in anorexia nervosa: Alterations in states of low connectivity and state transitions. J. Child. Psychol. Psychiatry 2024, 65, 1299–1310. [Google Scholar] [CrossRef]
- Wang, J.; Wang, X.; Wang, Y.; Li, W.; Li, Z.; Tang, L.; Huang, X.; Grzegorzek, M.; Chen, Q.; Wang, Z.; et al. Changes in resting-state functional connectivity of large-scale brain networks in bulimia nervosa: Evidence from causal analysis. Cereb. Cortex 2024, 34, bhae430. [Google Scholar] [CrossRef]
- Gaudio, S.; Quattrocchi, C.C. Neural basis of a multidimensional model of body image distortion in anorexia nervosa. Neurosci. Biobehav. Rev. 2012, 36, 1839–1847. [Google Scholar] [CrossRef]
- de Carvalho, M.R.; Dias, T.G.C.; de Raphael Nogueira, F.; Cordás, T.A.; Teixeira, A.L. The neurobiology of body image disturbance in anorexia nervosa: A systematic review. Compr. Psychiatry 2024, 123, 152446. [Google Scholar] [CrossRef]
- Norrlin, C.; Baumann, O. Neural correlates of body-image disturbance in eating disorders: A systematic review and ALE meta-analysis. Int. J. Environ. Res. Public. Health 2025, 22, 123. [Google Scholar] [CrossRef]
- Hamamoto, Y.; Suzuki, S.; Sugiura, M. Two components of body-image disturbance are differentially associated with distinct eating disorder characteristics in healthy young women. PLoS ONE 2022, 17. [Google Scholar] [CrossRef]
- Ambrosecchia, M.; Ardizzi, M.; Russo, E.C.; Ditaranto, F.; Speciale, M.; Vinai, P.; Todisco, P.; Maestro, S.; Gallese, V. Bodily self-recognition and body size overestimation in restrictive anorexia nervosa: Implicit and explicit mechanisms. Front. Psychol. 2023, 14, 1197319. [Google Scholar] [CrossRef] [PubMed]
- Croce, S.R.; Malcolm, A.C.; Ralph-Nearman, C.; Phillipou, A. The role of identity in anorexia nervosa: A narrative review. New Ideas Psychol. 2024, 71, 101036. [Google Scholar] [CrossRef]
- Cripps, S.; Hwang, S.; Fox, J.R.E. Experiences of externalisation in recovery from anorexia nervosa. J. Eat. Disord. 2024, 12, 87. [Google Scholar] [CrossRef]
- Ali, S.I.; Keel, P.K. Examining the association between deficits in self-concept clarity and eating disorder severity. Eat. Behav. 2023, 51, 101810. [Google Scholar] [CrossRef]
- Carr, M.M.; Wiedemann, A.A.; Macdonald-Gagnon, G.; Potenza, M.N. Impulsivity and compulsivity in binge-eating disorder: A systematic review of behavioral studies. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 110, 110318. [Google Scholar] [CrossRef]
- Pasquale, E.K.; Svaldi, J. Reward and inhibitory control as mechanisms and targets for treatment in binge-eating disorder. Curr. Psychiatry Rep. 2024, 26, 307–318. [Google Scholar] [CrossRef]
- Hambleton, A.; Le Grange, D.; Hay, P. Psychiatric and medical comorbidities of eating disorders: A rapid review. J. Eat. Disord. 2022, 10, 58. [Google Scholar] [CrossRef]
- Mendoza, R.R.; Joyce, P.R.; Bedrick, E.J.; Chen, G. Examining associations of borderline personality disorder symptom dimensions with eating-disorder diagnoses in a nationally representative sample. J. Psychiatr. Res. 2025, 171, 158–166. [Google Scholar] [CrossRef]
- Claes, L.; van der Kaap-Deeder, J.; Luyckx, K.; Dierckx, E. The association between identity functioning and personality pathology in female patients with eating disorders. Nutrients 2025, 17, 2329. [Google Scholar] [CrossRef]
- Cunningham, C.; Frayn, M.; Touyz, S. Toward integrated treatment for co-occurring borderline personality disorder and eating disorders: A clinician perspective. Int. J. Eat. Disord. 2025, 58, 1161–1166. [Google Scholar] [CrossRef] [PubMed]
- Madden, S.; Morris, A.; Zurynski, Y.A.; Kohn, M.; Elliot, E.J. Burden of eating disorders in 5–13-year-old children in Australia. Med. J. Aust. 2009, 190, 410–414. [Google Scholar] [CrossRef]
- Waller, G.; Beard, J. Recent Advances in Cognitive-Behavioural Therapy for Eating Disorders (CBT-ED). Curr. Psychiatry Rep. 2024, 26, 351–358. [Google Scholar] [CrossRef]
- Kessler, U.; Kleppe, M.M.; Rekkedal, G.Å.; Rø, Ø.; Danielsen, Y. Experiences when implementing enhanced cognitive behavioral therapy as a standard treatment for anorexia nervosa in outpatients at a public specialized eating-disorder treatment unit. J. Eat. Disord. 2022, 10, 15. [Google Scholar] [CrossRef] [PubMed]
- Dalle Grave, R.; Calugi, S.; Doll, H.A.; Fairburn, C.G. Enhanced cognitive behaviour therapy for adolescents with anorexia nervosa: An alternative to family therapy? Behav. Res. Ther. 2013, 51, R9–R12. [Google Scholar] [CrossRef]
- Lock, J.; Le Grange, D.; Agras, W.S.; Moye, A.; Bryson, S.W.; Jo, B. Randomized clinical trial comparing family-based treatment and adolescent-focused individual therapy for adolescents with anorexia nervosa. Arch. Gen. Psychiatry 2010, 67, 1025–1032. [Google Scholar] [CrossRef]
- Jewell, T.; Apostolidou, E.; Sadikovic, K.; Tahta-Wraith, K.; Liston, S.; Simic, M.; Eisler, I.; Fonagy, P.; Yorke, I. Attachment in individuals with eating disorders compared to community controls: A systematic review and meta-analysis. Int. J. Eat. Disord. 2023, 56, 888–908. [Google Scholar] [CrossRef]
- Kjaersdam Telléus, G.; Simonsen, C.B.; Jakobsen, A.G.; Dalgaard, M.K.; Rasmussen, S.M.; Nilsson, K.K. A multifaceted approach to assessment of mentalization: The mentalization profile in patients with eating disorders. Nord. J. Psychiatry 2024, 78, 146–152. [Google Scholar] [CrossRef]
- Zeeck, A.; Lau, I.; Endorf, K.; Schaefer, L.; Euler, S.; Lahmann, C.; Hartmann, A. Mentalizing in psychotherapeutic processes of patients with EDs. Front. Psychiatry 2024, 15, 1367863. [Google Scholar] [CrossRef]
- Robinson, P.; Hellier, J.; Barrett, B.; Barzdaitiene, D.; Bateman, A.; Bogaardt, A.; Clare, A.; Somers, N.; O’Callaghan, A.; Goldsmith, K.; et al. The NOURISHED randomized controlled trial: MBT-ED vs SSCM-ED. Trials 2016, 17, 549. [Google Scholar] [CrossRef]
- Golan, M. Eating and Control Styles Axis in Mentalisation-Based Psychotherapy in Eating Disorders: A randomised clinical trial. Front. Psychiatry 2022, 13, 774382. [Google Scholar] [CrossRef]
- Pugh, M. A narrative review of schemas and schema therapy in eating disorders. Clin. Psychol. Rev. 2015, 38, 41–51. [Google Scholar] [CrossRef]
- Rochman, D. Minds Love to Hate: A Mentalizing Approach to Self-Hatred and Negative Self-Representations in Eating Disorders. Psychodyn. Psychiatry 2025, 53, 357–374. [Google Scholar] [CrossRef] [PubMed]
- Meier, A.F.; Zeeck, A.; Taubner, S.; Gablonski, T.; Lau, I.; Preiter, R.; Gläser, H.; Zipfel, S.; Herzog, W.; Wild, B.; et al. Mentalization-enhancing therapeutic interventions in the psychotherapy of anorexia nervosa: An analysis of use and influence on patients’ mentalizing capacity. Psychother. Res. 2023, 33, 595–607. [Google Scholar] [CrossRef] [PubMed]
- Sonntag, M.; Russell, J. The mind-in-mind study: A pilot randomised controlled trial that compared modified mentalisation based treatment with supportive clinical management for patients with eating disorders without borderline personality disorder. Eur. Eat. Disord. Rev. 2022, 30, 206–220. [Google Scholar] [CrossRef] [PubMed]
- Talbot, D.; Gavin, J.; van Vreeswijk, M.; de Jongh, A. Schema modes in EDs vs community sample. J. Eat. Disord. 2015, 3, 18. [Google Scholar] [CrossRef]
- Simpson, S.G.; Morrow, E.; van Vreeswijk, M.; Reid, C. Group Schema Therapy for eating disorders: A pilot study. Front. Psychol. 2010, 1, 182. [Google Scholar] [CrossRef]
- Schumacher, A.M.; Tschitsaz, A.; Lerch, S.; Wyssen, A.; Schlensog-Schuster, F.; Mürner-Lavanchy, I.; Koenig, J.; Cavelti, M.; Kaess, M. Impairments in personality functioning in adolescents with anorexia nervosa. Eur. Eat. Disord. Rev. 2024, 33, 360–373. [Google Scholar] [CrossRef]
- Calvert, F.; Tait, P.; Tasca, G.A.; Balfour, L. Group schema therapy for eating disorders: Study protocol for a randomized controlled trial. J. Eat. Disord. 2018, 6, 46. [Google Scholar] [CrossRef]
- Mares, S.H.W.; Roelofs, J.; Zinzen, J.; Béatse, M.; Elgersma, H.J.; Drost, R.M.W.A.; Evers, S.M.A.A.; Elburg, A.A.V. Clinical effectiveness, cost-effectiveness and process evaluation of group schema therapy for eating disorders: Study protocol for a multicenter randomized controlled trial. BMC Psychol. 2024, 12, 123. [Google Scholar] [CrossRef]
- Marney, C.; House, L.; Clarke, S. A mixed-methods study of schema modes in people with eating disorders. J. Eat. Disord. 2024, 12, 31. [Google Scholar] [CrossRef]
- Heywood, L.; Conti, J.; Arcelus, J. Paper 1: A systematic synthesis of narrative therapy treatment content and use for eating disorders. J. Eat. Disord. 2022, 10, 115. [Google Scholar] [CrossRef]
- Safer, D.L.; Robinson, A.H.; Jo, B. Outcome from a randomized controlled trial of group therapy for binge eating disorder: Comparing dialectical behavior therapy adapted for binge eating to an active comparison group therapy. Behav. Ther. 2010, 41, 106–120. [Google Scholar] [CrossRef]
- Linardon, J.; Anderson, C.; McClure, Z.; Liu, C.; Messer, M.; Jarman, H.K.; Fuller-Tyszkiewicz, M. A DBT skills training smartphone app for recurrent binge eating: A randomized clinical trial. Psychol. Med. 2024, 54, 4646–4657. [Google Scholar] [CrossRef]
- Chen, E.Y.; Cacioppo, J.; Fettich, K.; Gallop, R.; McCloskey, M.S.; Olino, T.; Zeffiro, T.A. An adaptive randomized trial of dialectical behavior therapy and cognitive behavior therapy for binge-eating. Psychol. Med. 2017, 47, 703–717. [Google Scholar] [CrossRef]
- Boswell, J.F.; Anderson, L.M.; Oswald, J.M.; Reilly, E.E.; Gorrell, S.; Anderson, D.A. A preliminary naturalistic clinical case series study of the feasibility and impact of interoceptive exposure for eating disorders. Behav. Res. Ther. 2019, 117, 54–64. [Google Scholar] [CrossRef]
- Hildebrandt, T.; Peyser, D.; Sysko, R. Lessons learned developing and testing family-based interoceptive exposure for adolescents with low-weight eating disorders. Int. J. Eat. Disord. 2021, 54, 2037–2045. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.A.; Vanzhula, I.A.; Reilly, E.E.; Levinson, C.A.; Berner, L.A.; Krueger, A.; Lavender, J.M.; Kaye, W.H.; Wierenga, C.E. Body mistrust bridges interoceptive awareness and eating disorder symptoms. J. Abnorm. Psychol. 2020, 129, 445–456. [Google Scholar] [CrossRef] [PubMed]
- Vrabel, K.R.; Waller, G.; Goss, K.; Wampold, B.; Kopland, M.; Hoffart, A. Cognitive behavioral therapy versus compassion focused therapy for adult patients with eating disorders with and without childhood trauma: A randomized controlled trial in an intensive treatment setting. Behav. Res. Ther. 2024, 174, 104480. [Google Scholar] [CrossRef] [PubMed]
- Kelly, A.C.; Carter, J.C.; Borairi, S. Self-compassion training for binge-eating disorder: A pilot randomized controlled trial. Clin. Psychol. Psychother. 2015, 21, 488–501. [Google Scholar] [CrossRef]
- Millard, L.A.; Wan, M.W.; Smith, D.M.; Wittkowski, A. The effectiveness of compassion focused therapy with clinical populations: A systematic review and meta-analysis. J. Affect. Disord. 2023, 326, 168–192. [Google Scholar] [CrossRef] [PubMed]
- Fogelkvist, M.; Aila Gustafsson, S.; Kjellin, L.; Parling, T. Acceptance and commitment therapy to reduce eating disorder symptoms and body image problems in patients with residual symptoms: A randomized controlled trial. Body Image 2020, 32, 155–166. [Google Scholar] [CrossRef] [PubMed]
- Afari, N.; Herbert, M.S.; Godfrey, K.M.; Cuneo, J.G.; Salamat, J.S.; Mostoufi, S.; Gasperi, M.; Ober, K.; Backhaus, A.; Rutledge, T.; et al. Acceptance and commitment therapy as an adjunct to the MOVE! programme: A randomized controlled trial. Obes. Sci. Pract. 2019, 5, 397–407. [Google Scholar] [CrossRef] [PubMed]
- Wu, K.; Wang, Y.; Xue, H.; Guo, X.; He, Y. Neuromodulation of eating disorders: A review of rTMS/tDCS/DBS. Biomedicines 2024, 12, 384. [Google Scholar] [CrossRef]
- Longo, P.; Bevione, F.; Lacidogna, M.C.; Lavalle, R.; Abbate Daga, G.; Preti, A. Neuromodulatory techniques in eating disorders: From electroconvulsive therapy to transcranial magnetic stimulation and beyond: A mixed method systematic meta-review. Psychiatry Res. 2025, 344, 116346. [Google Scholar] [CrossRef]
- Bruch, H. Eating Disorders: Obesity, Anorexia Nervosa, and the Person Within; Basic Books: New York, NY, USA, 1973. [Google Scholar]
- Skårderud, F. Eating One’s Words, Part I: “Concretised metaphors” and reflective function in anorexia nervosa—An interview study. Eur. Eat. Disord. Rev. 2007, 15, 163–174. [Google Scholar] [CrossRef]
- Skårderud, F. Eating One’s Words, Part II: The embodied mind and reflective function in anorexia nervosa—Theory. Eur. Eat. Disord. Rev. 2007, 15, 243–252. [Google Scholar] [CrossRef]
- Clinton, D. Affect regulation, object relations and the central symptoms of eating disorders. Eur. Eat. Disord. Rev. 2006, 14, 203–211. [Google Scholar] [CrossRef]
- Tasca, G.A.; Balfour, L. Eating disorders and attachment: A contemporary psychodynamic perspective. Psychodyn. Psychiatry 2014, 42, 257–276. [Google Scholar] [CrossRef]
- Craba, A.; Mazza, M.; Marano, G.; Crosta, M.L.; Moroni, F.; Di Pietro, S.; Balocchi, M.; Della Casa, S.; Rinaldi, L.; Janiri, L.; et al. Defense mechanisms and parenting styles in patients with anorexia and bulimia. J. Nerv. Ment. Dis. 2023, 211, 174–181. [Google Scholar] [CrossRef]
- Jewell, T.; Herle, M.; Serpell, L.; Eivors, A.; Simic, M.; Fonagy, P.; Eisler, I. Attachment and mentalization as predictors of outcome in family therapy for adolescent anorexia nervosa. Eur. Child Adolesc. Psychiatry 2023, 32, 1241–1251. [Google Scholar] [CrossRef] [PubMed]
- Zerbe, K.J. The crucial role of psychodynamic understanding in the treatment of eating disorders. Psychiatr. Clin. N. Am. 2001, 24, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Zeeck, A.; Endorf, K.; Euler, S.; Schaefer, L.; Lau, I.; Flösser, K.; Geiger, V.; Meier, A.F.; Walcher, P.; Lahmann, C.; et al. Implementation of mentalization-based treatment in a day hospital program for eating disorders—A pilot study. Eur. Eat. Disord. Rev. 2021, 29, 783–801. [Google Scholar] [CrossRef] [PubMed]
- Zipfel, S.; Wild, B.; Groß, G.; Friederich, H.C.; Teufel, M.; Schellberg, D.; Giel, K.E.; de Zwaan, M.; Dinkel, A.; Herpertz, S.; et al. Focal psychodynamic therapy, cognitive behaviour therapy, and optimised treatment as usual in outpatients with anorexia nervosa (ANTOP study): Randomised controlled trial. Lancet 2014, 383, 127–137. [Google Scholar] [CrossRef]
- Herzog, W.; Wild, B.; Giel, K.E.; Junne, F.; Friederich, H.C.; Resmark, G.; Teufel, M.; Schellberg, D.; de Zwaan, M.; Dinkel, A.; et al. Focal psychodynamic therapy, cognitive behaviour therapy, and optimised treatment as usual in female outpatients with anorexia nervosa (ANTOP study): 5-year follow-up of a randomised controlled trial in Germany. Lancet Psychiatry 2022, 9, 280–290. [Google Scholar] [CrossRef]
- Egger, N.; Wild, B.; Zipfel, S.; Junne, F.; Konnopka, A.; Schmidt, U.; de Zwaan, M.; Herpertz, S.; Zeeck, A.; Löwe, B.; et al. Cost-effectiveness of focal psychodynamic therapy and enhanced cognitive-behavioural therapy in outpatients with anorexia nervosa (ANTOP). Psychol. Med. 2016, 46, 3291–3301. [Google Scholar] [CrossRef]
- Poulsen, S.; Lunn, S.; Daniel, S.I.F.; Folke, S.; Mathiesen, B.B.; Katznelson, H.; Fairburn, C.G. A randomized controlled trial of psychoanalytic psychotherapy vs CBT for bulimia nervosa. Am. J. Psychiatry 2014, 171, 109–116. [Google Scholar] [CrossRef]
- Russell, H.; Aouad, P.; Le, A.; Marks, P.; Maloney, D.; National Eating Disorder Research Consortium; Touyz, S.; Maguire, S. Psychotherapies for eating disorders: Findings from a rapid review. J. Eat. Disord. 2023, 11, 175. [Google Scholar] [CrossRef]
- Trombetta, T.; Bottaro, D.; Paradiso, M.N.; Santoniccolo, F.; Abbate Daga, G.; Rollè, L. Psychodynamic group therapy for eating disorders: A narrative review. J. Contemp. Psychother. 2024, 54, 253–264. [Google Scholar] [CrossRef]
- Friederich, H.-C.; Zipfel, S.; Wild, B. Psychodynamic therapies and eating disorders. In Eating Disorders; Springer: Cham, Switzerland, 2023. [Google Scholar]
- Sharp, C.; McLaren, V.; Musetti, A.; Vanwoerden, S.; Hernandez Ortiz, J.; Schmeck, K.; Birkhoelzer, M.; Goth, K. The Assessment of Identity Development in Adolescence (AIDA) Questionnaire: First psychometric evaluation in two North American samples of young people. J. Pers. Assess. 2023, 105, 451–462. [Google Scholar] [CrossRef]
- Butterfield, R.D.; Grad-Freilich, M.; Silk, J.S. The role of neural self-referential processes underlying self-concept in adolescent depression: A comprehensive review and proposed neurobehavioral model. Neurosci. Biobehav. Rev. 2023, 149, 105183. [Google Scholar] [CrossRef]
- Voderholzer, U.; Favreau, M.; Schlegl, S.; Hessler-Kaufmann, J.B. Impact of comorbid borderline personality disorder on the outcome of inpatient treatment for anorexia nervosa: A retrospective chart review. Borderline Pers. Disord. Emot. Dysregul. 2021, 8, 8. [Google Scholar] [CrossRef]

| Construct | Instrument (Acronym) | What It Measures/Key Subscales | Format (Items; Response Range) | Typical Populations | Clinical/Research Use in EDs (Example) | Example References |
|---|---|---|---|---|---|---|
| Self-concept clarity | Self-Concept Clarity Scale (SCCS) | Clarity/consistency/stability of self-beliefs | 12 items; Likert (typically 1–5) | Adolescents; Adults | Mediator/moderator in the Identity Disruption pathway; track change during treatment | Campbell, Trapnell, Heine, Katz, Lavallee, and Lehman [18]; Vartanian, Hayward, Smyth, Paxton, and Touyz [1]; Vartanian, Nicholls, and Fardouly [2] |
| Identity functioning (youth) | Assessment of Identity Development in Adolescence (AIDA) | Identity synthesis vs. diffusion (e.g., continuity, coherence) | 58 items; Likert | Adolescents (clinical and community) | Severity stratification/prognosis in AN; track inpatient change | Goth, Foelsch, Schlüter-Müller, Birkhölzer, Jung, Pick, and Schmeck [12]; Budde, Haenschel, Herpertz-Dahlmann, and Konrad [21] |
| Identity processes (modes) | Schema Mode Inventory—ED version (SMI-ED) | Maladaptive/functional modes (e.g., Punitive parent, demanding parent, vulnerable child, healthy adult) | ≈100 items; Likert | Adults with EDs | Targets for schema therapy: externalize the ‘ED part’ | Simpson, McDonald, and Stewart [22] |
| Self-objectification | Objectified Body Consciousness Scale (OBCS) | Body surveillance; body shame (and control beliefs) | 24 items; Likert | Adolescents; Adults | Mediators to disordered eating: change with comparison/media-literacy interventions | Fredrickson and Roberts [5]; Daniels, Zurbriggen, and Ward (2020) [6]; Schaefer and Thompson [23] |
| Appearance comparison | Physical Appearance Comparison Scale (PACS/PACS-3) | Frequency/direction of appearance comparisons | Likert (varies by version) | Adolescents; Young adults | Proximal mechanism in social-media contexts | van den Berg, Thompson, Obremski-Brandon, and Coovert (2002) [19]; Karsay, Knoll, and Matthes [24]; Bonfanti, Melchiori, Teti, Albano, Raffard, Rodgers, and Lo Coco [25] |
| Self-discrepancy | Selves Questionnaire/discrepancy scoring | Actual–Ideal; Actual–Ought gaps (idiographic trait lists) | Idiographic; discrepancy indices | Adolescents; Adults | Risk/maintenance mapping to affect (shame/dejection; guilt/agitation) | Higgins [4]; Strauman, Vookles, Berenstein, Chaiken, and Higgins [26]; Mason, Smith, Engwall, Lass, Mead, Sorby, Bjorlie, Strauman, and Wonderlich [27] |
| ED psychopathology anchor | Eating Disorder Examination–Questionnaire (EDE-Q) | Global ED severity; subscales include restraint, eating concern, shape concern, weight concern; overvaluation indices | 28 items; Likert | All ED diagnoses | Primary outcome: mediator with identity measures | Fairburn, Cooper, and Shafran [7] |
| Feature | Children (<12 Years) | Adolescents (13–18 Years) | Adults (>18 Years) |
|---|---|---|---|
| Typical onset | Increasing cases of early-onset AN and BED reported in preadolescence | Peak incidence of AN, BN, and BED | More chronic or relapsing presentations |
| Phenotype | Atypical AN (normal weight with severe complications); early BED with obesity | Classic AN with marked weight loss; BN with binge/purge; BED more frequent | Full DSM-5 syndromes, often comorbid with depression, anxiety, and personality disorders |
| Medical complications | Growth impairment, pubertal delay, bone mineral deficits, high medical instability | Amenorrhea, reduced bone density, electrolyte disturbances | Cardiovascular, metabolic, and gastrointestinal complications; osteoporosis |
| Psychosocial impact | Bullying, school avoidance, social withdrawal | Peer comparison, identity conflict, self-esteem vulnerability | Work, relationship, and role functioning impairment |
| Preferred treatment | Family-Based Treatment (FBT), pediatric medical monitoring | FBT, CBT-E adapted for adolescents, prevention programs | CBT-E, schema therapy, MBT, psychodynamic, or adjunctive methods |
| Mechanism/Maintenance Factor | Primary Intervention(s) | Key Techniques | Process Measures (Mechanism Capture) | Clinical Outcomes (Examples) |
|---|---|---|---|---|
| Overvaluation of weight/shape | CBT-E (focused) | Cognitive restructuring of overvaluation; pattern-breaking for checking/avoidance; regular eating | EDE-Q Overvaluation; body checking/body image avoidance scales | ↓ EDE-Q global; symptom remission; BMI/weight restoration (when indicated) |
| Identity diffusion/low SCC | Narrative therapy, schema therapy, and values-based work (ACT) | Externalize ED identity; re-author self-story; schema/mode work; values clarification | SCCS; AIDA; SMI-ED | ↑ SCC; ↓ drive for thinness/body dissatisfaction; ↑ quality-of-life |
| Self-objectification/appearance comparison | CBT-E + comparison-disruption; media-literacy; functionality appreciation | Reduce surveillance; guided comparison exposure; cultivate body functionality focus | OBCS (surveillance/shame); PACS-3 | ↓ body dissatisfaction; ↓ ED symptoms (EDE-Q) |
| Emotion/impulse dysregulation (binge/purge) | DBT-informed modules | Distress tolerance, emotion regulation, opposite action, and urge surfing | DERS; binge/purge urge logs | ↓ objective binge/purge frequency; ↓ global ED psychopathology |
| Mentalization deficits (self/other) | MBT-ED (adjunct or program) | Mentalizing stance; affect-marked reflection; rupture repair; self-mentalizing | Reflective functioning measures; mentalization tasks | ↓ weight/shape concern; improved alliance and functioning |
| Interoceptive/DMN disturbances | Interoceptive exposure; compassion-focused practices; neuromodulation (adjunct) | Signal labeling/exposure to hunger/fullness; compassion practices; rTMS/tDCS (selected cases) | MAIA (interoception); resting-state/task indices (research settings) | ↑ satiety tolerance; ↓ ED cognitions; functional gains |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marano, G.; Napolitano, D.; Capristo, E.; Traversi, G.; Mazza, O.; Gaetani, E.; Mazza, M. The Body as a Battlefield: Identity Development and Psychosomatic Expression in Eating Disorders Across Childhood and Adolescence. Children 2025, 12, 1465. https://doi.org/10.3390/children12111465
Marano G, Napolitano D, Capristo E, Traversi G, Mazza O, Gaetani E, Mazza M. The Body as a Battlefield: Identity Development and Psychosomatic Expression in Eating Disorders Across Childhood and Adolescence. Children. 2025; 12(11):1465. https://doi.org/10.3390/children12111465
Chicago/Turabian StyleMarano, Giuseppe, Daniele Napolitano, Esmeralda Capristo, Gianandrea Traversi, Osvaldo Mazza, Eleonora Gaetani, and Marianna Mazza. 2025. "The Body as a Battlefield: Identity Development and Psychosomatic Expression in Eating Disorders Across Childhood and Adolescence" Children 12, no. 11: 1465. https://doi.org/10.3390/children12111465
APA StyleMarano, G., Napolitano, D., Capristo, E., Traversi, G., Mazza, O., Gaetani, E., & Mazza, M. (2025). The Body as a Battlefield: Identity Development and Psychosomatic Expression in Eating Disorders Across Childhood and Adolescence. Children, 12(11), 1465. https://doi.org/10.3390/children12111465











