Quality of Life and Mental Health Problems in Pediatric Cardiac Arrest Survivors
Highlights
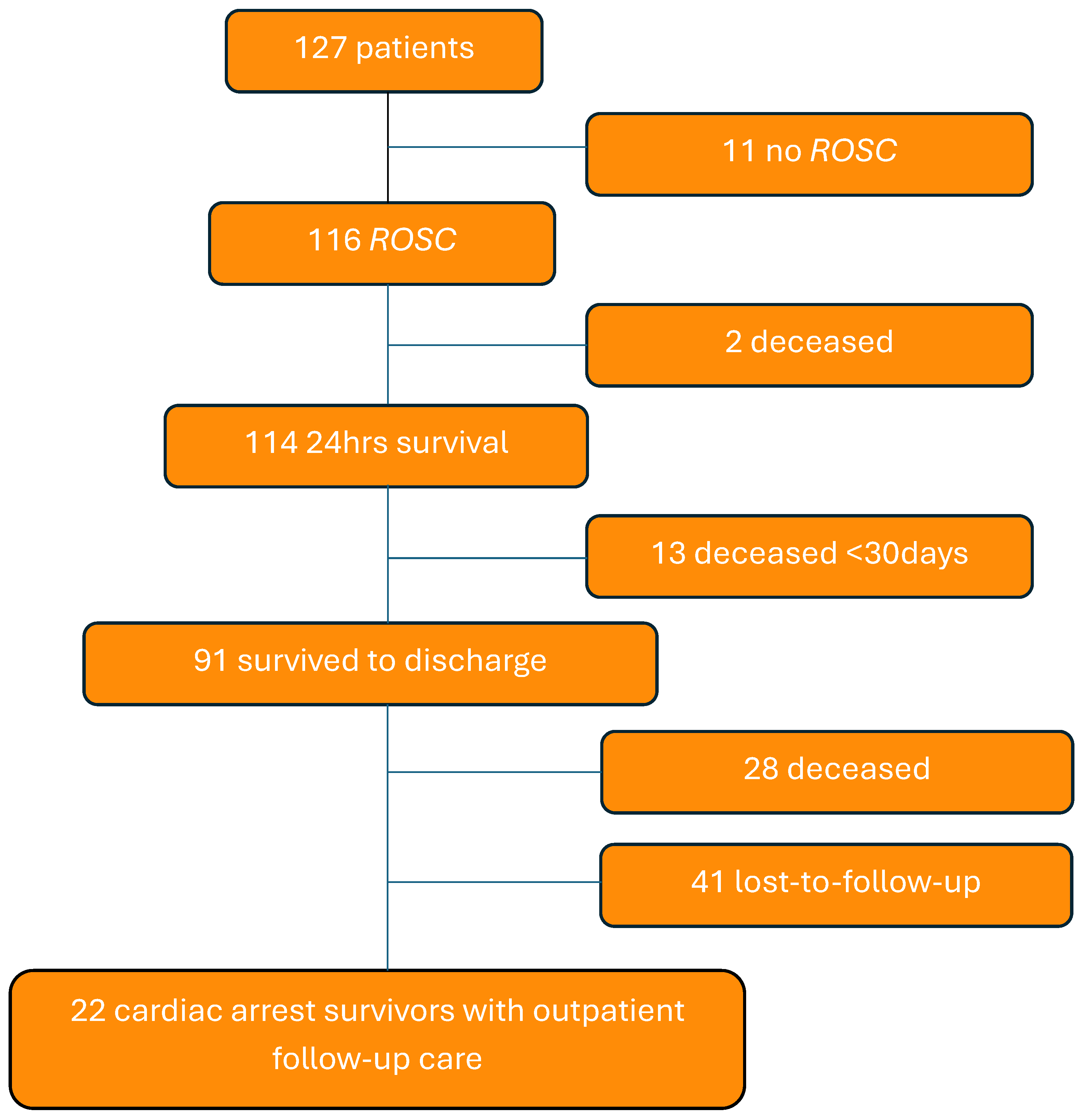
- Out of 127 pediatric cardiac arrest (CA) patients with heart disease, 72% survived to hospital discharge, and 22 are receiving follow-up care in an outpatient clinic.
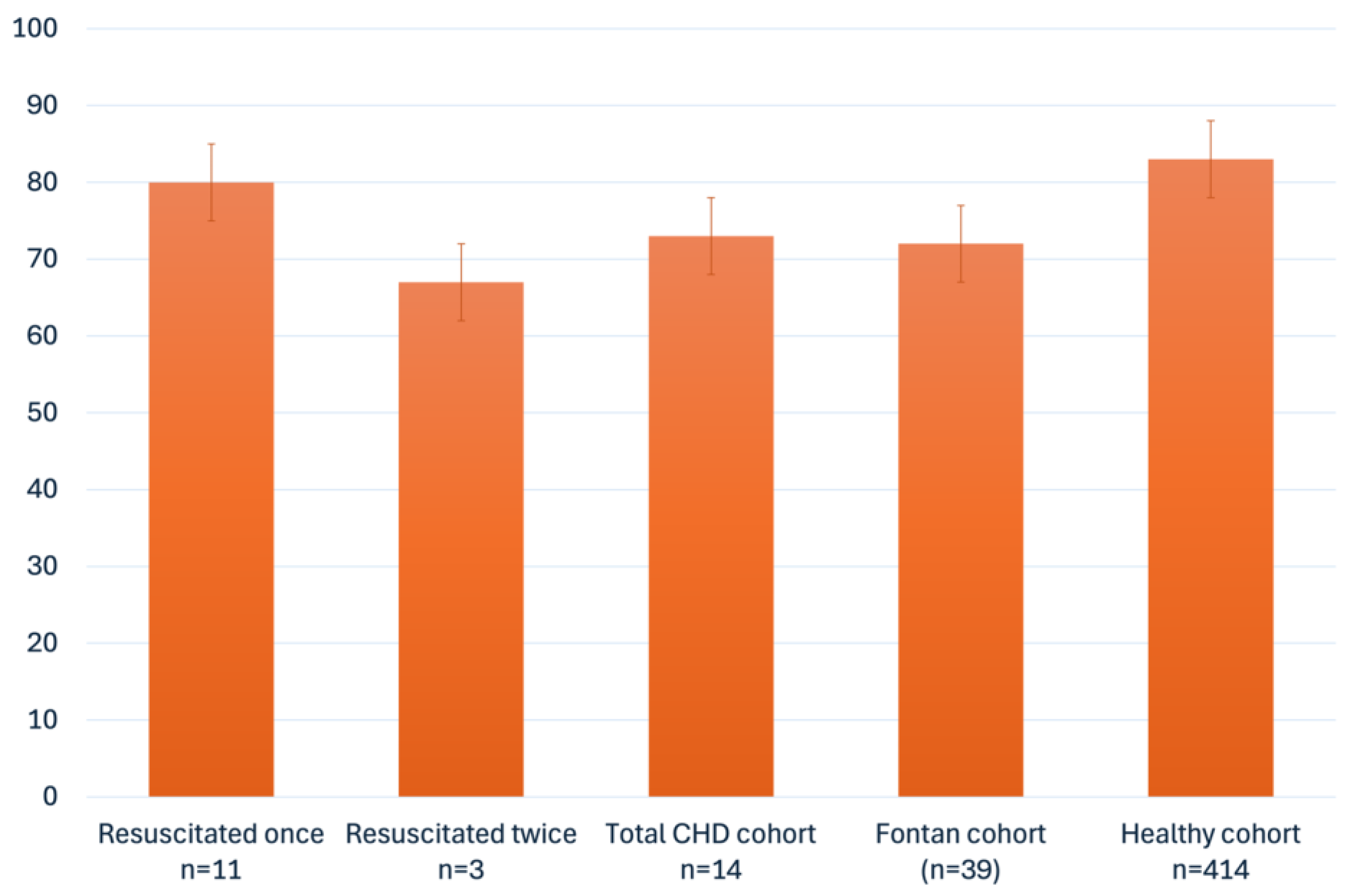
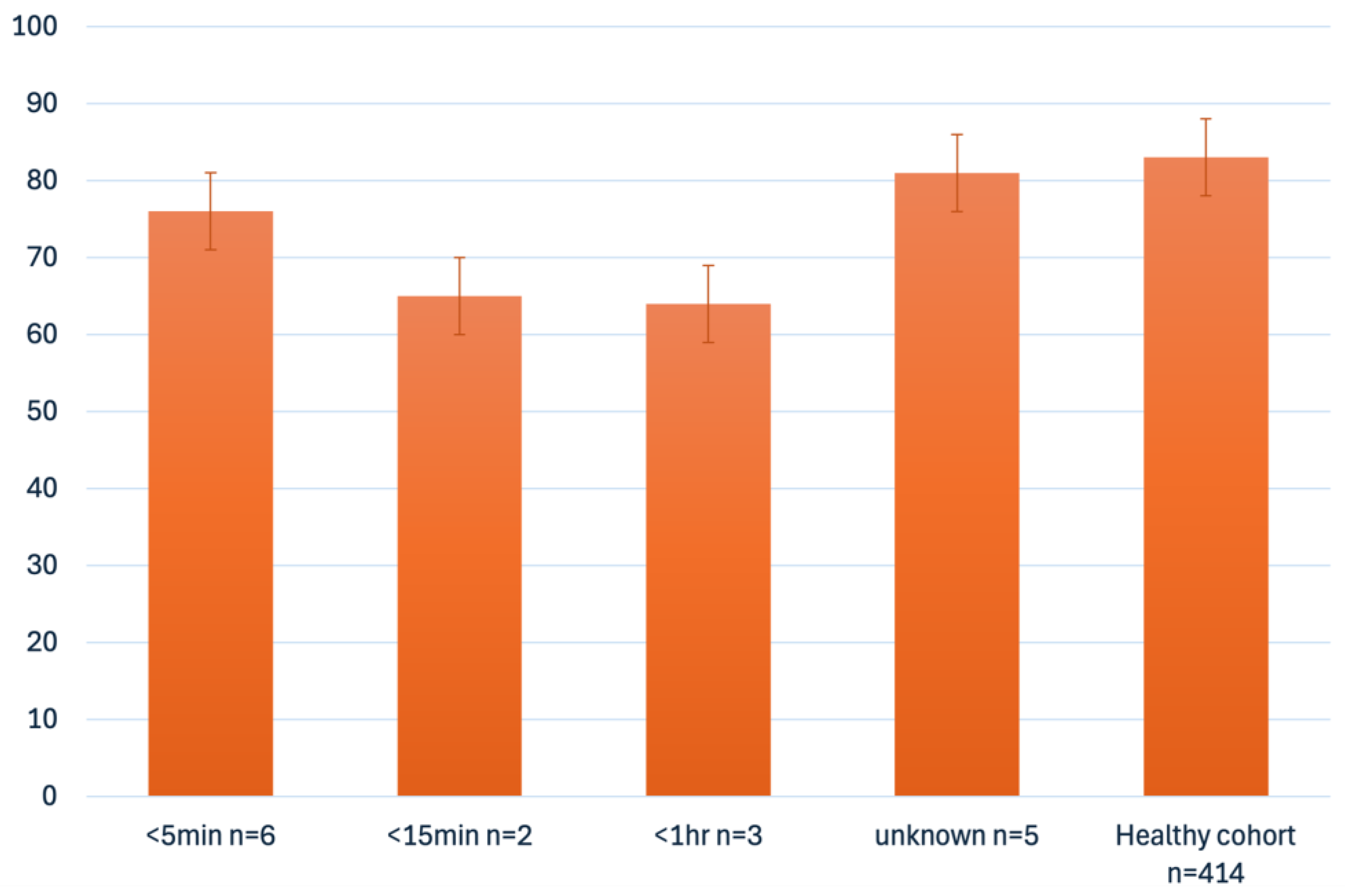
- Overall quality of life was comparable to healthy peers, but children with longer resuscitation time or multiple resuscitations showed lower scores in physical, emotional, social, and school functioning.
- A total of 21% of children showed elevated emotional and hyperactivity-related difficulties (based on parent reports), and peer problems (based on self-reports), indicating increased psychological stress.
- One-third of school-aged survivors attend special needs schools, highlighting potential neurodevelopmental and academic impact.
- While survival and average quality of life appear reassuring, a substantial proportion of survivors face subtle but relevant emotional, behavioral, and academic challenges.
- These findings underscore the urgent need for long-term follow-up programs with routine neurodevelopmental and neuropsychological screening to support at-risk pediatric cardiac arrest survivors.
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Population
- congenital or acquired heart disease
- age 0–18 years
- IHCA
- return of spontaneous circulation (ROSC)
- survival to date
- regular follow-up visits in the outpatient clinic
2.2. Data Collection
2.3. Assessments
2.3.1. The Pediatric Cerebral Performance Category Scale (PCPC)
2.3.2. Pediatric Quality of Life Inventory (PedsQL)
2.3.3. Strengths and Difficulties Questionnaire
2.4. Statistical Analysis
3. Results
4. Discussion
4.1. Outcome
4.2. Resuscitation Data Quality
4.3. Follow-Up After Cardiac Arrest
4.4. Quality of Life
4.5. Psychological Burden
4.6. Type of Education
4.7. Recommendations
4.8. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix A.1. First Data Query via ICD or OPS Codes
- ICD-Codes:
- R09.2 Respiratory arrest, including cardiopulmonary arrest
- I46. Cardiac arrest, I46.0 successful, I46.9 without successful resuscitation
- I49.0 Ventricular flutter and fibrillation
- R00.3 Pulseless electrical activity, excl. cardiac arrest
- R57.9 Peripheral circulatory failure
Appendix A.2. -T98.-Consequences of Other and Unspecified Effects of External Causes, Consequences of Amputation n.e.c. Consequences of Resuscitation
- 2.
- OPS codes:
- 8–779 Measures in the context of resuscitation
- 8–771 Cardiac or cardiopulmonary resuscitation
- 8–772 Operative resuscitation
Appendix A.3. Second Data Query Using Keywords from the Diagnosis List and the Epicrisis
- Post-resuscitation
- Post cardiopulmonary resuscitation
- Post-circulatory arrest
- Post-cardiac arrest
- Post-cardiac massage
- After resuscitation measures
- Exitus letalis
References
- Jung, P.; Brenner, S.; Bachmann, I.; Both, C.; Cardona, F.; Dohna-Schwake, C.; Eich, C.; Eifinger, F.; Huth, R.; Heimberg, E.; et al. More Than 500 Kids Could Be Saved Each Year! Ten Consensus Actions to Improve Quality of Pediatric Resuscitation in DACH-Countries (Austria, Germany, and Switzerland). Front. Pediatr. 2020, 8, 549710. [Google Scholar] [CrossRef]
- Lowry, A.W.; Knudson, J.D.; Cabrera, A.G.; Graves, D.E.; Morales, D.L.S.; Rossano, J.W. Cardiopulmonary Resuscitation in Hospitalized Children with Cardiovascular Disease. Pediatr. Crit. Care Med. 2013, 14, 248–255. [Google Scholar] [CrossRef]
- Markel, F.; Djakow, J.; Biarent, D.; de Lucas, N.; del Castillo, J.; Skellett, S.; Turner, N.M.; Buysse, C.M.; Lauridsen, K.G. Pediatric cardiac arrest registries and survival outcomes: A European study. Resusc. Plus 2025, 22, 100902. [Google Scholar] [CrossRef] [PubMed]
- del Castillo, J.; López-Herce, J.; Cañadas, S.; Matamoros, M.; Rodríguez-Núnez, A.; Rodríguez-Calvo, A.; Carrillo, A. Cardiac arrest and resuscitation in the pediatric intensive care unit: A prospective multicenter multinational study. Resuscitation 2014, 85, 1380–1386. [Google Scholar] [CrossRef] [PubMed]
- Meert, K.; Telford, R.; Holubkov, R.; Slomine, B.S.; Christensen, J.R.; Berger, J.; Ofori-Amanfo, G.; Newth, C.J.; Dean, J.M.; Moler, F.W. Paediatric in-hospital cardiac arrest: Factors associated with survival and neurobehavioural outcome one year later. Resuscitation 2018, 124, 96–105. [Google Scholar] [CrossRef]
- Brosig, S.; Wagner, R.; Twal, R.; Meier, S.; Vollroth, M.; Markel, F.; Dähnert, I.; Kostelka, M.; Paech, C. “Quality of life” analysis in the long-term follow-up after “Fontan” palliation for CHDs—A single-centre experience. Cardiol. Young 2024, 34, 1312–1324. [Google Scholar] [CrossRef]
- Meentken, M.G.; van Beynum, I.M.; Legerstee, J.S.; Helbing, W.A.; Utens, E.M.W.J. Medically Related Post-traumatic Stress in Children and Adolescents with Congenital Heart Defects. Front. Pediatr. 2017, 5, 20. [Google Scholar] [CrossRef]
- Cassedy, A.; Wray, J.; Qadir, A.A.; Ernst, M.M.; Brown, K.; Franklin, R.; Wernovsky, G.; Marino, B.S. Behavioral and Emotional Outcomes in Children with Congenital Heart Disease: Effects of Disease Severity, Family Life Stress, Disease-Related Chronic Stress, and Psychosocial Adaptation. J. Pediatr. 2023, 259, 113450. [Google Scholar] [CrossRef]
- Mercieca-Bebber, R.; King, M.T.; Calvert, M.J.; Stockler, M.R.; Friedlander, M. The importance of patient-reported outcomes in clinical trials and strategies for future optimization. Patient Relat. Outcome Meas. 2018, 2018, 353–367. [Google Scholar] [CrossRef]
- Topjian, A.A.; Scholefield, B.R.; Pinto, N.P.; Fink, E.L.; Buysse, C.M.; Haywood, K.; Maconochie, I.; Nadkarni, V.M.; de Caen, A.; Escalante-Kanashiro, R.; et al. P-COSCA (Pediatric Core Outcome Set for Cardiac Arrest) in Children. Resuscitation 2021, 162, 351–364. [Google Scholar] [CrossRef]
- van Zellem, L.; Utens, E.M.; Madderom, M.; Legerstee, J.S.; Aarsen, F.; Tibboel, D.; Buysse, C. Cardiac arrest in infants, children, and adolescents: Long-term emotional and behavioral functioning. Eur. J. Pediatr. 2016, 175, 977–986. [Google Scholar] [CrossRef] [PubMed]
- Cummins, R.; Chamberlain, D.; Hazinski, M.F.; Nadkarni, V.; Kloeck, W.; Kramer, E.; Becker, L.; Robertson, C.; Koster, R.; Zaritsky, A.; et al. Recommended Guidelines for Reviewing, Reporting, and Conducting Research on In-Hospital Resuscitation: The In-Hospital “Utstein Style”. Ann. Emerg. Med. 1997, 29, 650–679. [Google Scholar] [CrossRef] [PubMed]
- Suominen, P.; Olkkola, K.; Voipio, V.; Korpela, R.; Palo, R.; Räsänen, J. Utstein style reporting of in-hospital paediatric cardiopulmonary resuscitation. Resuscitation 2000, 45, 17–25. [Google Scholar] [CrossRef]
- Zaritsky, A.; Nadkarni, V.; Hazinski, M.F.; Foltin, G.; Quan, L.; Wright, J.; Fiser, D.; Zideman, D.; O’MAlley, P.; Chameides, L.; et al. Recommended guidelines for uniform reporting of pediatric advanced life support: The Pediatric Utstein Style. Resuscitation 1995, 30, 95–115. [Google Scholar] [CrossRef]
- A Warnes, C.; Liberthson, R.; Danielson, G.K.; Dore, A.; Harris, L.; Hoffman, J.I.; Somerville, J.; Williams, R.G.; Webb, G.D. Task Force 1: The changing profile of congenital heart disease in adult life. JACC 2001, 37, 1170–1175. [Google Scholar] [CrossRef]
- Förster, L.-J.; Vogel, M.; Stein, R.; Hilbert, A.; Breinker, J.L.; Böttcher, M.; Kiess, W.; Poulain, T. Mental health in children and adolescents with overweight or obesity. BMC Public Health 2023, 23, 135. [Google Scholar] [CrossRef]
- Brosig, C.L.; Mussatto, K.A.; Kuhn, E.M.; Tweddell, J.S. Psychosocial Outcomes for Preschool Children and Families After Surgery for Complex Congenital Heart Disease. Pediatr. Cardiol. 2007, 28, 255–262. [Google Scholar] [CrossRef]
- Joffe, A.R.; Lequier, L.; Robertson, C.M. Pediatric Outcomes After Extracorporeal Membrane Oxygenation for Cardiac Disease and for Cardiac Arrest. ASAIO J. 2012, 58, 297–310. [Google Scholar] [CrossRef]
- Fiser, D.H. Assessing the outcome of pediatric intensive care. J. Pediatr. 1992, 121, 68–74. [Google Scholar] [CrossRef]
- Varni, J.W.; Seid, M.; Kurtin, P.S. PedsQL™ 4.0: Reliability and Validity of the Pediatric Quality of Life Inventory™ Version 4.0 Generic Core Scales in Healthy and Patient Populations. Med. Care 2001, 39, 800–812. [Google Scholar] [CrossRef]
- Goodman, R. The Strengths and Difficulties Questionnaire: A Research Note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef]
- Woerner, W.; Becker, A.; Rothenberger, A. Normative data and scale properties of the German parent SDQ. Eur. Child Adolesc. Psychiatry 2004, 13, ii3–ii10. [Google Scholar] [CrossRef] [PubMed]
- Cooksey, R.W. Descriptive Statistics for Summarising Data. In Illustrating Statistical Procedures: Finding Meaning in Quantitative Data; Cooksey, R.W., Ed.; Springer: Singapore, 2020; pp. 61–139. [Google Scholar] [CrossRef]
- Rubinger, L.; Ekhtiari, S.; Gazendam, A.; Bhandari, M. Registries: Big data, bigger problems? Injury 2023, 54, S39–S42. [Google Scholar] [CrossRef] [PubMed]
- Lazem, M.; Sheikhtaheri, A. Barriers and facilitators for the implementation of health condition and outcome registry systems: A systematic literature review. J. Am. Med. Inform. Assoc. 2022, 29, 723–734. [Google Scholar] [CrossRef]
- A Topjian, A.; De Caen, A.; Wainwright, M.S.; Abella, B.S.; Abend, N.S.; Atkins, D.L.; Bembea, M.M.; Fink, E.L.; Guerguerian, A.-M.; E Haskell, S.; et al. Pediatric Post–Cardiac Arrest Care: A Scientific Statement from the American Heart Association. Circulation 2019, 140, E194–E233. [Google Scholar] [CrossRef]
- Nolan, J.P.; Sandroni, C.; Böttiger, B.W.; Cariou, A.; Cronberg, T.; Friberg, H.; Genbrugge, C.; Haywood, K.; Lilja, G.; Moulaert, V.R.M.; et al. Postreanimationsbehandlung. Notf. + Rettungsmedizin 2021, 24, 524–576. [Google Scholar] [CrossRef]
- Ijsselstijn, H.; Schiller, R.M.; Holder, C.; Shappley, R.K.H.; Wray, J.; Hoskote, A. Extracorporeal Life Support Organization (ELSO) Guidelines for Follow-up After Neonatal and Pediatric Extracorporeal Membrane Oxygenation. Asaio J. 2021, 67, 955–963. [Google Scholar] [CrossRef]
- Hunfeld, M.; Dulfer, K.; Del Castillo, J.; Vázquez, M.; Buysse, C. Long-term multidisciplinary follow-up programs in pediatric cardiac arrest survivors. Resusc. Plus 2024, 17, 100563. [Google Scholar] [CrossRef]
- Guerra, G.G.; Zorzela, L.; Robertson, C.M.; Alton, G.Y.; Joffe, A.R.; Moez, E.K.; Dinu, I.A.; Ross, D.B.; Rebeyka, I.M.; Lequier, L. Survival and neurocognitive outcomes in pediatric extracorporeal-cardiopulmonary resuscitation. Resuscitation 2015, 96, 208–213. [Google Scholar] [CrossRef]
- Cvetkovic, M.; Chiarini, G.; Belliato, M.; Delnoij, T.; Zanatta, P.; Taccone, F.S.; Miranda, D.d.R.; Davidson, M.; Matta, N.; Davis, C.; et al. International survey of neuromonitoring and neurodevelopmental outcome in children and adults supported on extracorporeal membrane oxygenation in Europe. Perfusion 2021, 38, 245–260. [Google Scholar] [CrossRef]
- Huebschmann, N.A.; Cook, N.E.; Murphy, S.; Iverson, G.L. Cognitive and Psychological Outcomes Following Pediatric Cardiac Arrest. Front. Pediatr. 2022, 10, 780251. [Google Scholar] [CrossRef] [PubMed]
- Shillingford, A.J.; Glanzman, M.M.; Ittenbach, R.F.; Clancy, R.R.; Gaynor, J.W.; Wernovsky, G. Inattention, Hyperactivity, and School Performance in a Population of School-Age Children with Complex Congenital Heart Disease. Pediatrics 2008, 121, e759–e767. [Google Scholar] [CrossRef]
- Brossard-Racine, M.; Panigrahy, A. Structural Brain Alterations and Their Associations with Function in Children, Adolescents, and Young Adults with Congenital Heart Disease. Can. J. Cardiol. 2022, 39, 123–132. [Google Scholar] [CrossRef]
- Matos, R.I.; Watson, R.S.; Nadkarni, V.M.; Huang, H.-H.; Berg, R.A.; Meaney, P.A.; Carroll, C.L.; Berens, R.J.; Praestgaard, A.; Weissfeld, L.; et al. Duration of Cardiopulmonary Resuscitation and Illness Category Impact Survival and Neurologic Outcomes for In-hospital Pediatric Cardiac Arrests. Circulation 2013, 127, 442–451. [Google Scholar] [CrossRef]
- Jaschinski, C.; Knetsch, V.; Parzer, P.; Meyr, J.; Schroeder, B.; Fonseca, E.; Karck, M.; Kaess, M.; Loukanov, T. Psychosocial Impact of Congenital Heart Diseases on Patients and Their Families: A Parent’s Perspective. World J. Pediatr. Congenit. Heart Surg. 2021, 13, 9–15. [Google Scholar] [CrossRef]
- Schmitt, K.R.L.; Sievers, L.K.; Hütter, A.; Abdul-Khaliq, H.; Poryo, M.; Berger, F.; Bauer, U.M.M.; Helm, P.C.; Pfitzer, C. New Insights into the Education of Children with Congenital Heart Disease with and without Trisomy 21. Medicina 2023, 59, 2001. [Google Scholar] [CrossRef]
- Geva, S.; Hoskote, A.; Saini, M.; Clark, C.A.; Banks, T.; Chong, W.K.K.; Baldeweg, T.; de Haan, M.; Vargha-Khadem, F. Cognitive outcome and its neural correlates after cardiorespiratory arrest in childhood. Dev. Sci. 2024, 27, e13501. [Google Scholar] [CrossRef]

| Heart Disease | Resuscitation Time (Minutes) | ECPR | Type of BGA | Minimum pH Value | Minimum Base Excess mmol/L | Maximum Lactate mmol/L | QoL Could Be Evaluated | Type of Education | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Aortic stenosis | 35 | - | n/a | n/a | n/a | n/a | ✓ | Special education |
| 2 | TGA | 15 | - | 2 | 7.33 | −3.8 | 2.6 | ✓ | Regular school |
| 3 | TGA | 2 | - | 2 | 7.4 | −0.6 | 3.2 | ✓ | Regular school |
| 4 | AVSD | 2 | - | 2 | 7.4 | −7.5 | 2.4 | - | Special education |
| 5 | DORV | n/a | - | n/a | n/a | n/a | n/a | ✓ | Regular school |
| 6 | AVSD | n/a | - | n/a | n/a | n/a | n/a | - | Special education |
| 7 | Perimyocarditis | n/a | ✓ | 2 | 7.4 | −1.5 | 3.5 | ✓ | Regular school |
| 8 | Long QT Syndrom | 5 | - | 2 | 7.2 | −7.8 | 4.3 | - | Regular school |
| 9 | VSD | 2 | - | 2 | 7.1 | −12 | 16 | ✓ | Regular school |
| 10 | Pulmonary atresia | n/a | - | 2 | 7.3 | −4.7 | 5.3 | ✓ | Regular school |
| 11 | Hypoplastic right heart | 10 | - | 2 | 7.3 | −3.7 | 3.1 | - | Regular school |
| 12 | Univentricular heart | n/a | - | 1 | 7.1 | 3.1 | 2 | - | Special education |
| 13 | Truncus art. comm. | 1 | - | 2 | 7.0 | −18 | 21 | ✓ | Regular school |
| 14 | TOF | 75 | ✓ | 2 | 7.36 | −3.7 | 3.1 | - | Regular school |
| 15 | AVSD | 2 | - | 2 | 7.29 | −0.8 | 1.1 | ✓ | Regular school delayed |
| 16 | Shone Komplex | 10 | - | n/a | n/a | n/a | n/a | - | Nursery school |
| 17 | TOF | 1 | - | n/a | n/a | n/a | n/a | ✓ | Nursery school |
| 18 | Univentricular heart | n/a | ✓ | n/a | n/a | n/a | n/a | - | Nursery school |
| 19 | Truncus art. comm. | n/a | ✓ | n/a | n/a | n/a | n/a | ✓ | Nursery school |
| 20 | Univentricular heart | 7 | - | n/a | n/a | n/a | n/a | ✓ | Special education |
| 40 | - | n/a | n/a | n/a | n/a | - | |||
| 21 | Hypoplastic left heart | n/a | - | 2 | 7.3 | −8.2 | 2.1 | ✓ | Regular school |
| n/a | ✓ | 2 | 6.6 | −31 | 18.0 | - | |||
| 22 | Aortic coarctation | 2 | - | 2 | 7.3 | −1.5 | 13.6 | ✓ | Special education |
| 16 | - | 2 | 7.3 | −3.7 | 16.0 | - |
| Children with Heart Disease (n = 22) | Healthy Cohort (n = 401) | |
|---|---|---|
| Total score | 77.3 (±2.8) | 83.0 (±14.79) |
| Physical health | 75.44 (±22.1) | 84.41 (±17.26) |
| Emotional functioning | 71.79 (±10.6) | 80.86 (±19.64) |
| Social functioning | 77.14 (±31.8) | 87.42 (±17.18) |
| School functioning | 76.5 (±14.1) | 78.63 (±20.53) |
| Children with Heart Disease | Healthy Cohort | Limit Values | |||
|---|---|---|---|---|---|
| Behavioral strengths and difficulties parent reports | |||||
| n = 6 | n = 1186 | normal | borderline | abnormal | |
| Total score | 13.5 (±3.0) | n/a | 0–13 | 14–16 | 17–40 |
| Prosocial behavior | 8.6 (±2.2) | 7.91 (±1.89) | 6–10 | 5 | 0–4 |
| Hyperactivity | 5.8 (±0.7) | 3.74 (±2.43) | 0–5 | 6 | 7–10 |
| Emotional symptoms | 2.6 (±1.8) | 1.11 (±1.45) | 0–3 | 4 | 4–10 |
| Conduct problems | 1.3 (±1.4) | 2.05 (±1.56) | 0–2 | 3 | 4–10 |
| Peer relationship problems | 2.0 (±0.7) | 1.11 (±1.45) | 0–2 | 3 | 4–10 |
| Behavioral strengths and difficulties self-reports | |||||
| n = 8 | n = 1042 | ||||
| Total score | 11.75 (±3.0) | n/a | 0–15 | 16–19 | 20–40 |
| Prosocial behavior | 7.4 (±2.1) | 7.88 (±1.80) | 6–10 | 4 | 0–4 |
| Hyperactivity | 4.0 (±0.7) | 3.46 (±2.26) | 0–5 | 6 | 7–10 |
| Emotional symptoms | 3.75 (±2.1) | 2.47 (±2.17) | 0–5 | 6 | 7–10 |
| Conduct problems | 1.9 (±1.4) | 1.55 (±1.37) | 0–3 | 4 | 5–10 |
| Peer relationship problems | 3.1 (±0.8) | 2.05 (±1.63) | 0–3 | 4 | 5–10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schwartz, T.; Weidenbach, M.; Dähnert, I.; Paech, C.; Markel, F. Quality of Life and Mental Health Problems in Pediatric Cardiac Arrest Survivors. Children 2025, 12, 1397. https://doi.org/10.3390/children12101397
Schwartz T, Weidenbach M, Dähnert I, Paech C, Markel F. Quality of Life and Mental Health Problems in Pediatric Cardiac Arrest Survivors. Children. 2025; 12(10):1397. https://doi.org/10.3390/children12101397
Chicago/Turabian StyleSchwartz, Tina, Michael Weidenbach, Ingo Dähnert, Christian Paech, and Franziska Markel. 2025. "Quality of Life and Mental Health Problems in Pediatric Cardiac Arrest Survivors" Children 12, no. 10: 1397. https://doi.org/10.3390/children12101397
APA StyleSchwartz, T., Weidenbach, M., Dähnert, I., Paech, C., & Markel, F. (2025). Quality of Life and Mental Health Problems in Pediatric Cardiac Arrest Survivors. Children, 12(10), 1397. https://doi.org/10.3390/children12101397