The Management of a Post-Extraction Gingival Lesion in a Paediatric Patient: A Case Report
Abstract
1. Introduction
2. Case Report
2.1. Patient Information
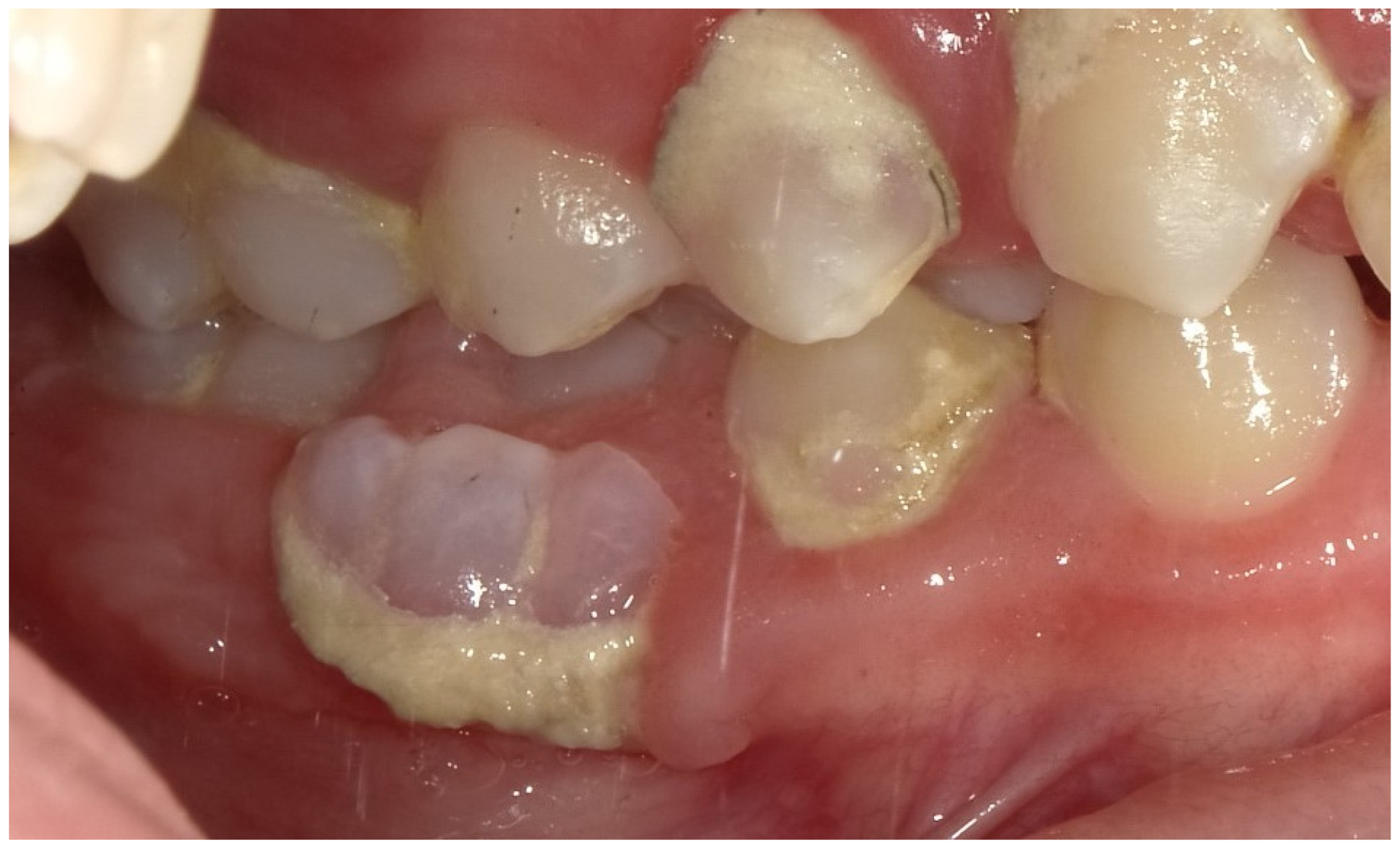
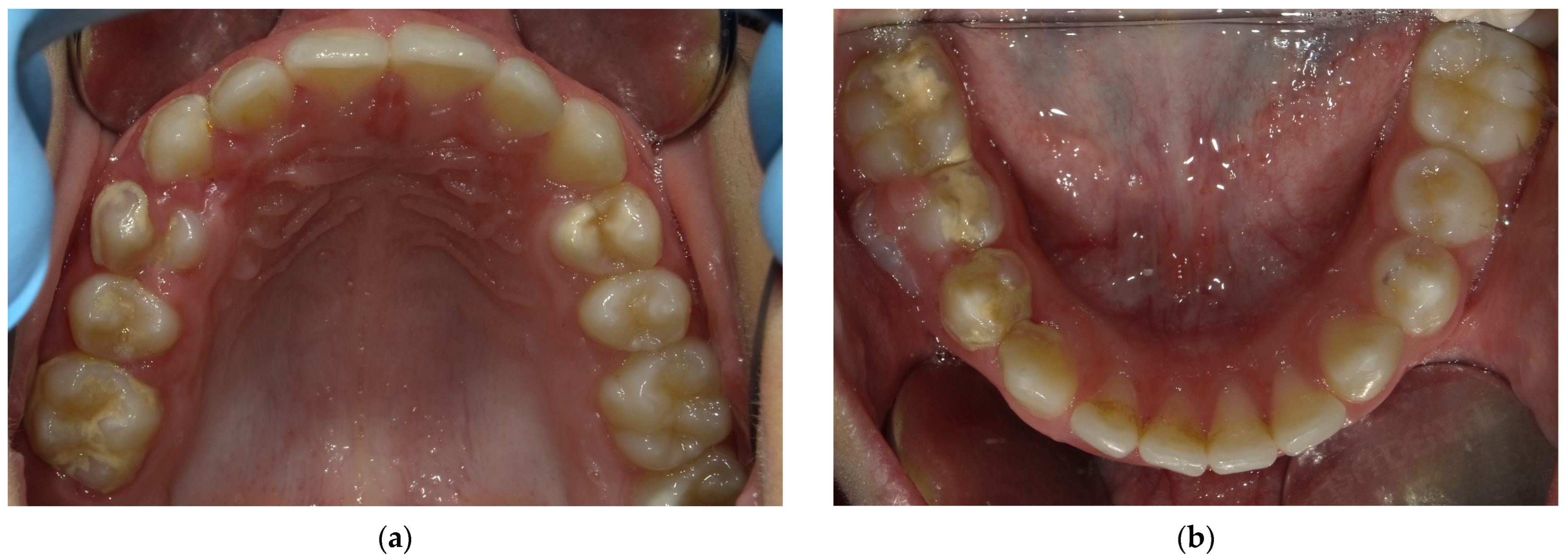
2.2. Clinical Findings
2.3. Diagnostic Assessment
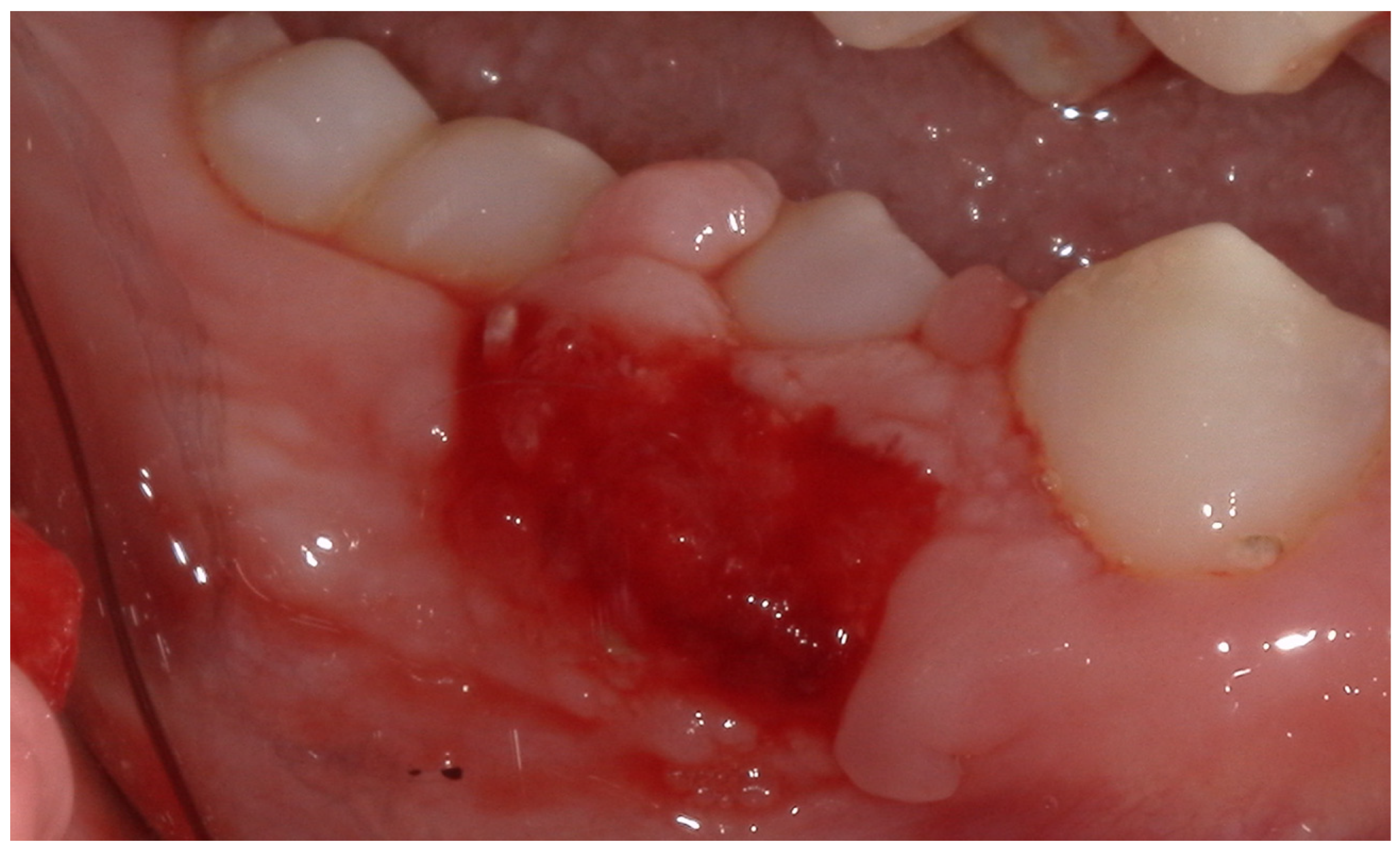
2.4. Therapeutic Intervention
2.5. Follow-Up and Outcomes
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Xiao, M.; Qian, H.; Lv, J.; Wang, P. Advances in the Study of the Mechanisms of Physiological Root Resorption in Deciduous Teeth. Front. Pediatr. 2022, 10, 850826. [Google Scholar] [CrossRef]
- Orilisi, G.; Cosi, A.; Vitiello, F.; Santoni, C.; Notarstefano, V.; Giorgini, E.; Orsini, G.; Tripodi, D. Physiological Root Resorption of Deciduous Teeth: An ATR-FTIR Approach. J. Clin. Med. 2024, 14, 48. [Google Scholar] [CrossRef] [PubMed]
- Ishizuka, K.; Kato, C.; Fujita, A.; Misawa-Omori, E.; Ono, T. Factors Influencing Root Resorption in Retained Mandibular Second Deciduous Molars with Congenital Absence of Second Premolars: A Cross-Sectional Study. Prog. Orthod. 2024, 25, 14. [Google Scholar] [CrossRef] [PubMed]
- Šimunović, L.; Lapter Varga, M.; Negovetić Vranić, D.; Čuković-Bagić, I.; Bergman, L.; Meštrović, S. The Role of Malocclusion and Oral Parafunctions in Predicting Signs and Symptoms of Temporomandibular Disorders—A Cross-Sectional Study. Dent. J. 2024, 12, 213. [Google Scholar] [CrossRef] [PubMed]
- Zou, J.; Meng, M.; Law, C.S.; Rao, Y.; Zhou, X. Common Dental Diseases in Children and Malocclusion. Int. J. Oral. Sci. 2018, 10, 7. [Google Scholar] [CrossRef]
- Temming, T.; Waldmann, S.; Jablonski-Momeni, A.; Korbmacher-Steiner, H. Qualitative and Quantitative Assessment of Infraoccluded Deciduous Teeth: A Systematic Review. Head Face Med. 2024, 20, 65. [Google Scholar] [CrossRef]
- Nadelman, P.; Bedran, N.; Magno, M.B.; Masterson, D.; de Castro, A.C.R.; Maia, L.C. Premature Loss of Primary Anterior Teeth and Its Consequences to Primary Dental Arch and Speech Pattern: A Systematic Review and Meta-Analysis. Int. J. Paediatr. Dent. 2020, 30, 687–712. [Google Scholar] [CrossRef]
- Nadelman, P.; Magno, M.B.; Pithon, M.M.; Castro, A.C.R.; Maia, L.C. Does the Premature Loss of Primary Anterior Teeth Cause Morphological, Functional and Psychosocial Consequences? Braz. Oral Res. 2021, 35, e092. [Google Scholar] [CrossRef]
- American Academy of Pediatric Dentistry. Reference Manual 2022–2023; American Academy of Pediatric Dentistry: Chicago, IL, USA, 2022. [Google Scholar]
- Suárez-Rodríguez, B.; Regueira-Iglesias, A.; Blanco-Pintos, T.; Sánchez-Barco, A.; Vila-Blanco, N.; Balsa-Castro, C.; Carreira, M.J.; Tomás, I. Randomised-Crossover Clinical Trial on the Substantivity of a Single Application of a Gel Containing Chlorhexidine and o-Cymen-5-Ol on the Oral Biofilm and Saliva. BMC Oral Health 2024, 24, 1247. [Google Scholar] [CrossRef]
- Sun, H.; Chen, S.; Yang, C.; Kuang, H.; Huang, Y.; He, X.; Luo, W. Advances in the Use of Chlorhexidine for Periodontitis Treatment in Diabetic Patients: A Review. Medicine 2024, 103, e39627. [Google Scholar] [CrossRef]
- Sekuła-Kamińska, B.; Nitecka-Buchta, A.; Wojciechowski, M.; Skucha-Nowak, M.; Rymarczyk, M.; Baron, S. Comparison of the Effects of Mucosa Tissue Healing with Chlorhexidine Digluconate and Choline Salicylate in Patients Wearing a Removable Prosthetic Restoration-A RCT. Clin. Pract. 2024, 14, 2350–2364. [Google Scholar] [CrossRef]
- Casarin, M.; de Matos, R.S.; da Silva Nolasco, W.; Pirih, F.Q.; Muniz, F.W.M.G. Effect of mouthwashes on gingival healing after surgical procedures: A systematic review. Eur. J. Oral Sci. 2023, 131, e12931. [Google Scholar] [CrossRef] [PubMed]
- Mummolo, S.; Cirillo, E.; Ciribè, M.; Manenti, R.J.; Galeotti, A. Periodontology. Part 1: Gingivitis in adolescence. Review of the literature and case reports. Eur. J. Paediatr. Dent. 2022, 23, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Saini, R. Ozone Therapy in Dentistry: A Strategic Review. J. Nat. Sci. Biol. Med. 2011, 2, 151. [Google Scholar] [CrossRef]
- Maglia, D.R.; Souza, B.D.A.F.; Visioli, F. Efficacy of Ozone Therapy for Oral Mucosa Wound Healing: A Systematic Review and Meta-Analysis. Clin. Oral Investig. 2024, 28, 490. [Google Scholar] [CrossRef]
- ISO 3950:2016; Dentistry—Designation System for Teeth and Areas of the Oral Cavity. International Organization for Standardization: Geneva, Switzerland, 2016.
- Shamash, S.; Reichert, F.; Rotshenker, S. The cytokine network of Wallerian degeneration: Tumor necrosis factor-α, inter-leukin-1α, and interleukin-1β. J. Neurosci. 2002, 22, 3052–3060. [Google Scholar] [CrossRef]
- Gadallah, L.K.; Elbardissy, A.; Elyazeed, M.A.; Alsamad, A.A.; Hamdy, M. Pulpotomy versus Pulpectomy in Carious Vital Pulp Exposure in Primary Incisors: A Randomized Controlled Trial. BMC Oral Health 2024, 24, 354. [Google Scholar] [CrossRef]
- Di, T.; Chen, Y.; Zhou, Z.; Liu, J.; Du, Y.; Feng, C.; Zhu, B.; Wang, L. Effect of α7 nAChR-autophagy axis of deciduous tooth pulp stem cells in regulating IL-1β in the process of physiological root resorption of deciduous teeth. J. Mol. Med. 2024, 102, 1135–1149. [Google Scholar] [CrossRef]
- Hirst, L.; Evans, R. Wiedemann-Steiner syndrome: A case report. Clin. Case Rep. 2021, 9, 1158–1162. [Google Scholar] [CrossRef]
- Shakti, P.; Singh, A.; Purohit, B.M.; Purohit, A.; Taneja, S. Effect of premature loss of primary teeth on prevalence of malocclusion in permanent dentition: A systematic review and meta-analysis. Int. Orthod. 2023, 21, 100816. [Google Scholar] [CrossRef]
- Acharya, S.; Biswas, R. Body Image in Preschool Children Following Premature Loss of Primary Teeth: A Cross-sectional Study. Int. J. Clin. Pediatr. Dent. 2022, 15, 293–298. [Google Scholar] [CrossRef]
- Putrino, A.; Abed, M.R.; Barbato, E.; Galluccio, G. A Current Tool in Facial Aesthetics Perception of Orthodontic Patient: The Digital Warping. Cadmos 2021, 89, 46–52. [Google Scholar] [CrossRef]
- Rajput, H.A.S.; Ahmed, A.; Bilgrami, A.; Haider, B.; Khan, J.N.; Afnan, M. The Diagnosis and Initial Management of Children Presenting with Premature Loss of Primary Teeth Associated with a Systemic Condition. Cureus 2024, 16, e62402. [Google Scholar] [CrossRef]
- Spinola, S.G.; Sobral, A.P.T.; Mandetta, A.R.H.; Gimenez, T.; Gonçalves, M.L.L.; Soares, P.V.; Santos, E.M.; Imparato, J.C.P.; Horliana, A.C.R.T.; Mesquita-Ferrari, R.A. Childhood Early Oral Ageing Syndrome: Prevalence and Association with Possible Aetiological Factors and Consequences for the Vertical Dimension of Occlusion: Protocol for a Cross-Sectional Study. BMJ Open 2024, 14, e090085. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zhou, F.; Peng, Y.; Chen, L.; Wang, Y. Non-Syndromic Occurrence of True Generalized Microdontia with Hypodontia: A Case Report. Medicine 2019, 98, e16283. [Google Scholar] [CrossRef] [PubMed]
- Putrino, A.; Caputo, M.; Galeotti, A.; Marinelli, E.; Zaami, S. Type I Dentin Dysplasia: Literature Review and Case Report of a Family Affected by Misrecognition and Late Diagnosis. Medicina 2023, 59, 1477. [Google Scholar] [CrossRef] [PubMed]
- Henklein, S.D.; Küchler, E.C.; Proff, P.; Lepri, C.P.; Baratto-Filho, F.; Mattos, N.H.R.; Hueb de Menezes, F.C.; Kirschneck, C.; Madalena, I.R.; Hueb de Menezes-Oliveira, M.A. Prevalence and local causes for retention of primary teeth and the associated delayed per-manent tooth eruption. J. Orofac. Orthop. 2024, 85 (Suppl. S1), 73–78. [Google Scholar] [CrossRef]
- Shetty, S.; Agarwal, N.; Shetty, P.; Iqbal, A.M. Twin Supernumerary Teeth: A Tale of Two Cases. Can. J. Dent. Hyg. 2019, 53, 67–71. [Google Scholar]
- Munhoz, L.; Arita, E.S.; Nishimura, D.A.; Watanabe, P.C.A. Maxillofacial manifestations of Proteus syndrome: A systematic re-view with a case report. Oral Radiol. 2021, 37, 2–12. [Google Scholar] [CrossRef]
- Zheng, S.G. Early Treatment Principles of Tooth Replacement Disorders Associated with Hereditary Oral Diseases. Zhonghua Kou Qiang Yi Xue Za Zhi 2023, 58, 772–780. [Google Scholar] [CrossRef]
- Tu, Y.Y.; Yang, C.Y.; Chen, R.S.; Chen, M.H. Effects of chlorhexidine on stem cells from exfoliated deciduous teeth. J. Formos. Med. Assoc. 2015, 114, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Nogales, C.G.; Ferrari, P.H.; Kantorovich, E.O.; Lage-Marques, J.L. Ozone therapy in medicine and dentistry. J. Contemp. Dent. Pract. 2008, 9, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Suh, Y.; Patel, S.; Kaitlyn, R.; Gandhi, J.; Joshi, G.; Smith, N.L.; Khan, S.A. Clinical utility of ozone therapy in dental and oral medicine. Med. Gas. Res. 2019, 9, 163–167. [Google Scholar] [PubMed]
- Louw, A.; Diener, I.; Butler, D.S.; Puentedura, E.J. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Arch. Phys. Med. Rehabil. 2011, 92, 2041–2056. [Google Scholar] [CrossRef] [PubMed]
- Elvis, A.M.; Ekta, J.S. Ozone therapy: A clinical review. J. Nat. Sci. Biol. Med. 2011, 2, 66–70. [Google Scholar] [CrossRef]
- Barczyk, I.; Masłyk, D.; Walczuk, N.; Kijak, K.; Skomro, P.; Gronwald, H.; Pawlak, M.; Rusińska, A.; Sadowska, N.; Gronwald, B.; et al. Potential Clinical Applications of Ozone Therapy in Dental Specialties—A Literature Review, Supported by Own Observations. Int. J. Environ. Res. Public Health 2023, 20, 2048. [Google Scholar] [CrossRef]
- Ciribè, M.; Cirillo, E.; Arduino, P.G.; Putrino, A.; Caputo, M.; Zaami, S.; Bompiani, G.; Galeotti, A. The Management of Necrotizing Gingivitis in Paediatric Patients: A Scoping Review and Two Case Reports. Children 2024, 11, 1019. [Google Scholar] [CrossRef]
- Adhami, Z.E.; Erfanparast, L.; Molaei, Z.; Sadeghi, J.; Yazdanparas, A. Effect of 20-Ppm Ozone and 1% Chlorhexidine Gels on Plaque Index and Streptococcus Mutans Counts in the Dental Plaque in 6–12-Year-Old Children: A Randomized, Double-Blind Clinical Trial. J. Dent. Res. Dent. Clin. Dent. Prospect. 2023, 17, 177–181. [Google Scholar] [CrossRef]
- Romero-Olid, M.N.; Bucataru, E.; Ramos-García, P.; González-Moles, M.Á. Efficacy of Chlorhexidine after Oral Surgery Procedures on Wound Healing: Systematic Review and Meta-Analysis. Antibiotics 2023, 12, 1552. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Srivastava, V.; Dwivedi, S.; Sharma, S. Periodontal wound healing: An absolute literature review. J. Clin. Images Med. Case Rep. 2022, 3, 1726. [Google Scholar] [CrossRef]
- Rezaeianjam, M.; Khabazian, A.; Khabazian, T.; Ghorbani, F.; Abbasi, T.; Asghari, S.; Heidari, F.; Shiri, A.; Naderi, M. Efficacy of ozone therapy in dentistry with approach of healing, pain management, and therapeutic outcomes: A systematic review of clinical trials. BMC Oral Health 2025, 25, 433. [Google Scholar] [CrossRef]
- El Meligy, O.A.; Elemam, N.M.; Talaat, I.M. Ozone Therapy in Medicine and Dentistry: A Review of the Literature. Dent. J. 2023, 11, 187. [Google Scholar] [CrossRef]
- Shekhar, A.; Sikdar, C.; Srivastava, S.; Chaturvedi, A.; Bhatia, L.K.; Sarkar, D. The Efficacy of Ozone Therapy on Pain and Soft Tissue Healing Associated With the Surgical Placement of Dental Implants: A Randomized Controlled Trial. Cureus 2025, 17, e85482. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cirillo, E.; Ciribè, M.; Putrino, A.; Vanacore, S.; Litta, F.P.; Galeotti, A. The Management of a Post-Extraction Gingival Lesion in a Paediatric Patient: A Case Report. Children 2025, 12, 1331. https://doi.org/10.3390/children12101331
Cirillo E, Ciribè M, Putrino A, Vanacore S, Litta FP, Galeotti A. The Management of a Post-Extraction Gingival Lesion in a Paediatric Patient: A Case Report. Children. 2025; 12(10):1331. https://doi.org/10.3390/children12101331
Chicago/Turabian StyleCirillo, Erika, Massimiliano Ciribè, Alessandra Putrino, Sonia Vanacore, Francesco Pio Litta, and Angela Galeotti. 2025. "The Management of a Post-Extraction Gingival Lesion in a Paediatric Patient: A Case Report" Children 12, no. 10: 1331. https://doi.org/10.3390/children12101331
APA StyleCirillo, E., Ciribè, M., Putrino, A., Vanacore, S., Litta, F. P., & Galeotti, A. (2025). The Management of a Post-Extraction Gingival Lesion in a Paediatric Patient: A Case Report. Children, 12(10), 1331. https://doi.org/10.3390/children12101331






