1. Introduction
Assessing oral hygiene and dental health among schoolchildren is extremely important, as this age group lays the foundation for lifelong oral health habits. The main factors influencing children’s oral hygiene are parental education and involvement. When parents have knowledge and understand the importance of dental health, the plaque index in their children decreases significantly. This relationship is largely attributed to improvements in parents’ behaviors regarding dental hygiene practices, which in turn are reflected in children’s practices [
1,
2]. In addition, the level of education attained by parents has been linked to the prevalence of dental caries in children; parents who are more educated usually show greater awareness of effective oral care, leading to lower cases of dental problems among their children [
3]. Such findings suggest that parent-oriented educational programs could serve as an effective strategy for improving children’s oral health. Dental care anxiety is another key factor affecting children’s dental health. Children with poor oral health often have higher levels of dental anxiety [
4]. Addressing dental care anxiety through educational measures and providing positive dental experiences could lead to better health outcomes and increased cooperation during dental visits [
5]. Dental caries occurs because of demineralization of hard dental tissues, mainly attributed to the interaction of carbohydrates with bacterial biofilms in the oral cavity. The disease process begins when the bacteria that form plaque produce acids that dissolve minerals on the surface of the tooth, resulting in cavities. This process can be aggravated by various environmental and individual factors, including eating habits, oral hygiene practices, and inherent physiological characteristics [
6,
7]. Various demographic and socioeconomic factors play a key role in the prevalence and incidence of dental caries. Studies show that children and adolescents from lower socioeconomic backgrounds tend to have a higher prevalence of dental caries due to limited access to dental care, inadequate oral hygiene practices, and socioeconomic stressors that influence food choices [
8,
9]. Silva et al. highlighted a direct correlation between lower social status and increased prevalence of caries due to inadequate access to dental services, also emphasizing the role of maternal education in influencing children’s oral health behaviors [
10]. These findings are reinforced by the finding of Medina-Solís et al. who showed that children from lower-income backgrounds made less use of dental services, aligning poor oral health with limited access to health care [
11]. Parental education level and occupational status have been shown to correlate with caries prevalence, as parents with lower levels of education and income have children who are more likely to suffer from dental caries [
12,
13,
14]. Dental hygiene practices and eating habits are other crucial factors influencing the incidence of tooth decay. Research underlines that poor oral hygiene, such as inadequate brushing techniques, contributes significantly to the prevalence of caries [
15,
16]. In addition, frequent consumption of sugary snacks has been identified as a risk factor for the development of dental caries, and dietary changes have been recommended to limit this exposure [
15,
17]. Therefore, the prevalence of dental caries in children remains a significant public health concern worldwide, with varying degrees of incidence in different populations. Research indicates that about 60–90% of children are affected by dental caries globally, making it one of the most common chronic diseases in pediatric populations [
13,
18]. Identifying periodontal problems and oral diseases in children is another crucial issue today, as it affects not only their oral health but also their overall quality of life. Periodontal diseases are a complex group of inflammatory conditions that affect the periodontium, including the supporting structures of the teeth, and are mainly caused by various forms of bacteria. Specifically, periodontitis is marked by the loss of periodontal attachment and is often initiated by the buildup of bacterial plaque on the teeth, leading to inflammation and the potential for irreversible tissue damage [
19,
20,
21]. Gingivitis or periodontitis can be prevalent in pediatric populations and have the potential to cause serious consequences if left untreated [
22,
23]. Therefore, recognizing periodontal disease at an early stage can prevent progression into more severe forms that may occur in late adolescence or early adulthood, thus underlining the importance of routine oral health assessments [
24,
25,
26]. Early diagnosis of periodontal problems allows the development of personalized treatment plans specific to each child’s unique oral health needs. Parents and teachers play an essential role in keeping children’s oral health. Understanding the relationship between a child’s oral health and overall well-being can improve proactive prevention and treatment measures. Therefore, prioritizing oral health during children’s formative years leads to improved immediate health outcomes, paving the way to a healthier future. In the context of the above, the present study aimed to assess the oral-dental status of 700 children aged 7 to 10 years from urban and rural areas of two counties of Romania, identifying the prevalence and severity of dental caries alongside their relationship with dental hygiene and dietary habits.
2. Materials and Methods
2.1. Ethical Consideration, Study Design, and Sample Size
The research was carried out with the authorization of the Scientific Research Ethics Committee affiliated with the “George Emil Palade” University of Medicine, Pharmacy, Science and Technology in Târgu Mureş (approval number 3147, dated 20 May 2024). The participant pool consisted of 700 children, ranging from 7 to 10 years old, representing both genders. Healthy children were included in the study based on their dentition. The criteria for exclusion were established concerning mental health and physical illnesses (for instance, intellectual disabilities, muscular paralysis, cerebral palsy, autism spectrum disorders, and central nervous system disorders resulting from perinatal hypoxia, as well as chronic illnesses and conditions characterized by diminished saliva production, such as xerostomia). Children diagnosed with these conditions were omitted from the study to mitigate any possible impact from related health issues. Before the initiation of the study, parents were briefed about the objectives and procedures involved, and informed consent was secured accordingly. The school authorities, in Mureş and Bistriţa-Năsăud counties, also granted permission to conduct the study. Specialists from the “George Emil Palade” University of Medicine, Pharmacy, Sciences and Technology from Târgu Mureş visited the nine schools to collect data over 1 year (May 2024–May 2025). To uphold the uniformity of the study population and to guarantee both the consistency and efficacy of the analysis, the sample was restricted to children aged 7 to 10 from the two counties mentioned in Romania.
2.2. Data Collection
The children’s parents answered questions to draw the participant’s demographic profile (name, age, gender, location, education, and professional status of the parents). Classroom teachers contributed to the distribution and assistance in completing a questionnaire regarding the behavioral and educational analysis of children. Furthermore, the class teachers were present to offer clarifications on the inquiries posed in the surveys. This assistance aimed to promote candid and comprehensive responses from parents, reflecting the familiarity and rapport they had with their children’s educators. Each completed questionnaire and associated child evaluation was systematically documented using a distinct identification code, thereby maintaining the confidentiality of the data collected. The questionnaire also included questions regarding toothbrush use, brushing frequency, dental flossing, total number of meals per day, number of snacks between meals, and sugar consumption.
2.3. Clinical Screening
Children underwent an oral examination by a qualified pedodontist to detect caries or other oral problems. To ensure consistency and reproducibility of clinical caries assessments, the examiner underwent a calibration process before data collection began. The calibration procedure included a two-day training session based on the World Health Organization (WHO) diagnostic criteria for dental caries [
27]. During this session, both theoretical definitions and practical clinical exercises were performed. For reliability testing, a subsample of 30 children, representing the age groups between 7 and 10 years, was pre-examined. Dental caries was recorded separately for the permanent and primary dentitions. For permanent teeth, we used the DMFT index (Decayed, Missing due to caries, and Filled Teeth). For primary teeth, we used the dmft index (decayed, missing due to caries, and filled primary teeth). Indices were computed at the child level as sums across teeth and summarized as both prevalence (proportion with index > 0) and severity (mean, SD; median, IQR).
Dental plaque was assessed using the Silness–Löe Plaque Index (PI) on index teeth, scored 0–3 per tooth and averaged per child; higher scores indicate more plaque. For interpretability, we classified PI into 0 = excellent, 0.1–0.9 = good, 1.0–1.9 = fair, and 2.0–3.0 = poor.
2.4. Statistical Analysis
The results obtained were entered into a database for evaluation, and their expression was as mean ± standard deviation (SD). Statistical evaluation was carried out using SPSS software version 27 (IBM Company, Armonk, NY, USA), and a p value < 0.05 was considered statistically significant.
The DMFT and dmft by age (7, 8, 9, 10 years) and sex were summarized. The Significant Caries Index (SIC) was computed as the mean DMFT (or dmft) among the one-third of children with the highest scores; polarization was expressed as SIC divided by the overall mean. Caries prevalence (DMFT > 0; dmft > 0) was modeled with modified Poisson with robust errors (aPR), and severity (DMFT; dmft counts) with negative binomial regression after assessing overdispersion. Models adjusted for age, sex, urban/rural residence, PI, brushing frequency, flossing, sugar consumption/day, snack frequency/day, meals/day, and parental education. Significance was set at 0.05 (two-sided). PI was analyzed as a continuous variable (mean ± SD) and as categories (excellent/good/fair/poor). We compared PI across age groups (7–8, 8–9, 9–10 years), gender, and location (urban/rural), reporting p-values for group differences.
The prevalence (% with DMFT > 0; % with dmft > 0) and severity (means ± SD) overall and by age groups were summarized. Bivariate associations used χ2 tests for prevalence and ANOVA for means. We then estimated adjusted prevalence ratios (aPR) for DMFT > 0 using modified Poisson regression with robust errors, including age group, sex, and residence as covariates; exposures entered as categories (reference = healthiest pattern).
3. Results
Table 1 shows the demographic profile of the study participants. It can be seen that out of the total of 700 participating children, 356 were boys and 344 were girls, divided by age groups as follows: age group 7–8 years (107 boys vs. 117 girls), age group 8–9 years (97 boys vs. 87 girls), and age group 9–10 years (152 boys vs. 140 girls). 141 boys and 155 girls came from urban areas, and 215 boys and 189 girls from rural areas. In terms of fathers’ education, the fathers of 217 boys and 194 girls have finished a university; the fathers of 54 boys and 81 girls graduated from high school, and the fathers of 87 boys and 67 girls have finished only secondary school (8 classes). Regarding the mother’s education, the mothers of 270 boys and 261 girls presented a high level of education, the mothers of 48 boys and 54 girls had finished high school, and the mothers of 40 boys and 27 girls had finished only secondary school. Overall, 301 fathers of boys and 295 fathers of girls were employed, compared with 61 mothers of boys and 97 mothers of girls who were employed.
Following statistical analysis of the demographic profile of the participants, we obtained a significant difference (p < 0.05) when the participants were compared according to the mother’s education, as well as to the parents’ occupation. Therefore, it seems that parents’ education and the environment in which they work daily significantly affect the general condition, including the oral health, of their children.
Across the indexed ages (7–8, 8–9, and 9–10 years), caries experience in the primary dentition (dmft) decreased with age, whereas caries in the permanent dentition (DMFT) increased. Overall, the mean dmft was 2.0 ± 2.0, and 56% of children had dmft > 0, while the mean DMFT was 0.66 ± 1.00 with 37% DMFT > 0. Age-specific means were: dmft 2.6 ± 2.1 (7–8 years), 2.1 ± 2.0 (8–9 years), and 1.5 ± 1.8 (9–10 years); DMFT 0.45 ± 0.80, 0.62 ± 0.95, and 0.85 ± 1.10, respectively. Medians and interquartile ranges are shown in
Table 2.
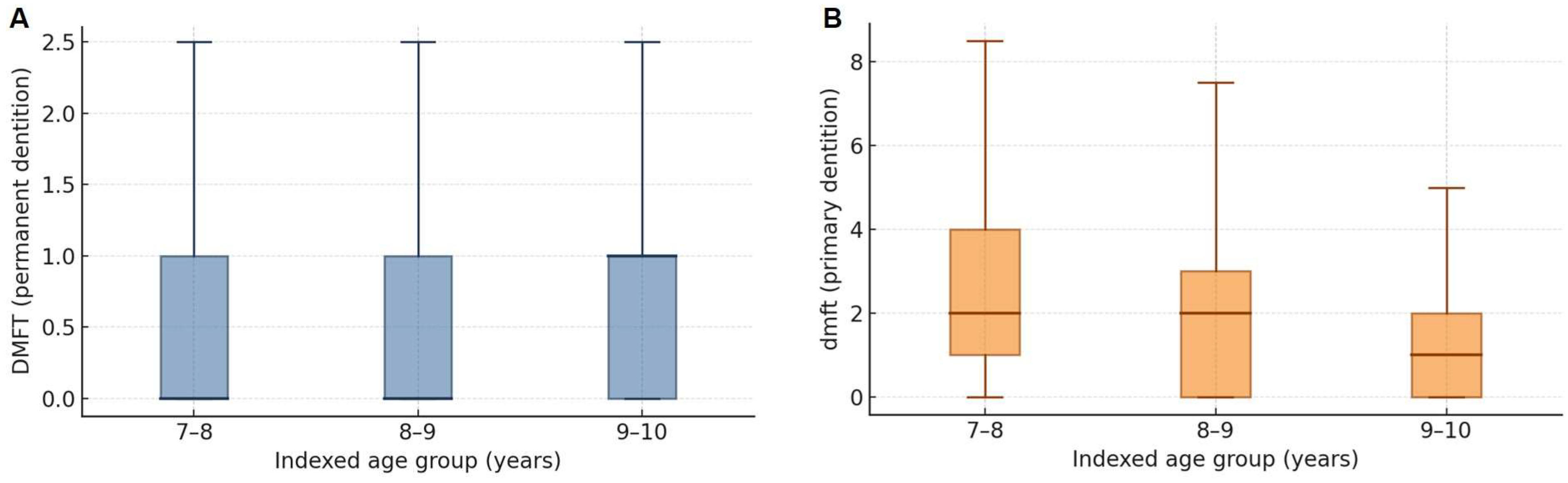
To complement
Table 2,
Figure 1 displays boxplots of caries experience by indexed age. In the permanent dentition (DMFT), medians were 0 at 7–8 and 8–9 years and 1 at 9–10 years, with IQR [0–1] across ages. In the primary dentition (dmft), medians declined from 2 at 7–8 and 8–9 years to 1 at 9–10 years, with IQR [1–4], [0–3], and [0–2], respectively. These distributions illustrate the shift from primary- to permanent-tooth caries with age.
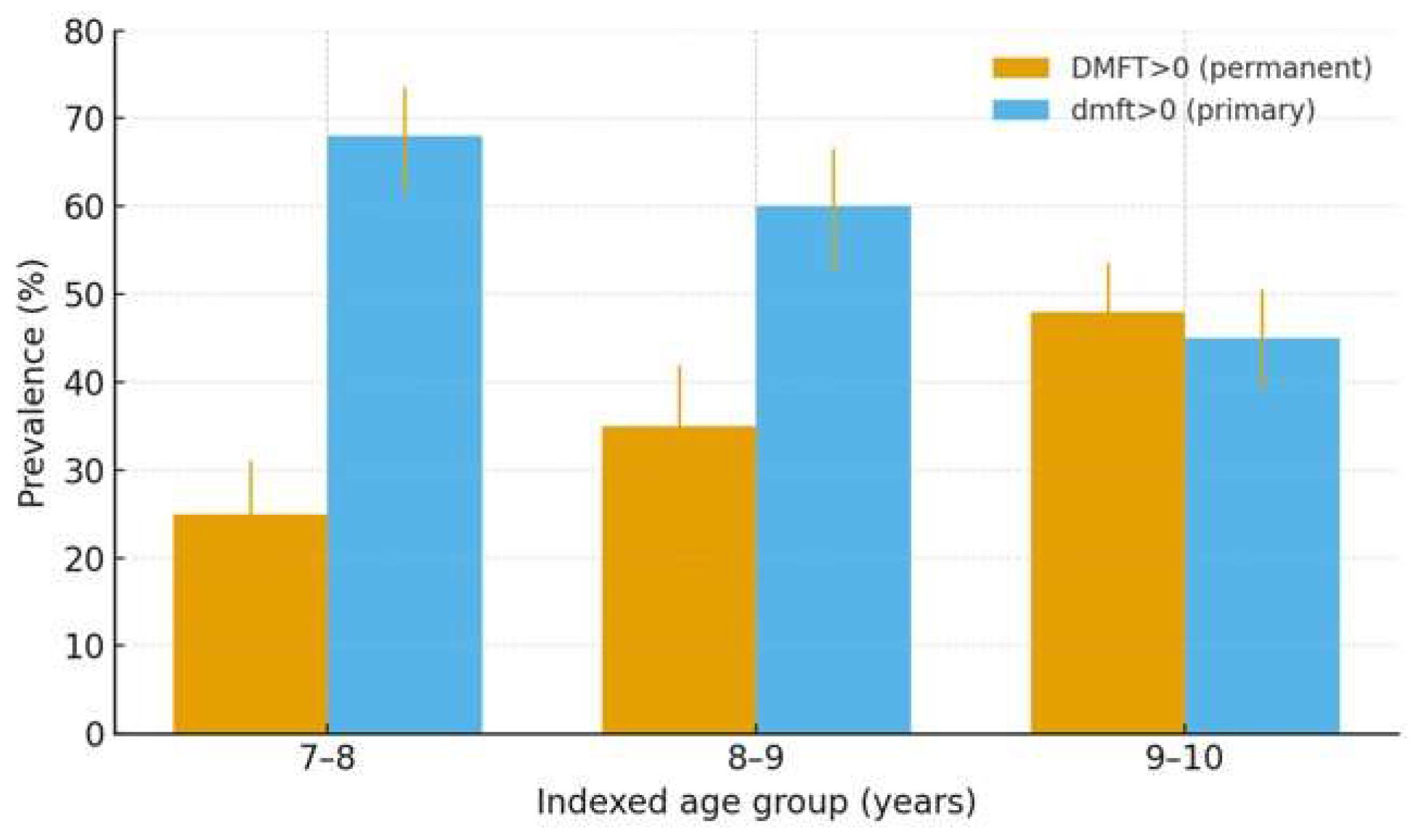
Figure 2 displays the prevalence of caries in the permanent (DMFT > 0) and primary dentitions (dmft > 0) across indexed ages. Consistent with
Table 2, DMFT > 0 increases from 25% at 7–8 years to 48% at 9–10 years, whereas dmft > 0 declines from 68% to 45% over the same range. Error bars indicate 95% confidence intervals (Wilson) based on the age-specific sample sizes.
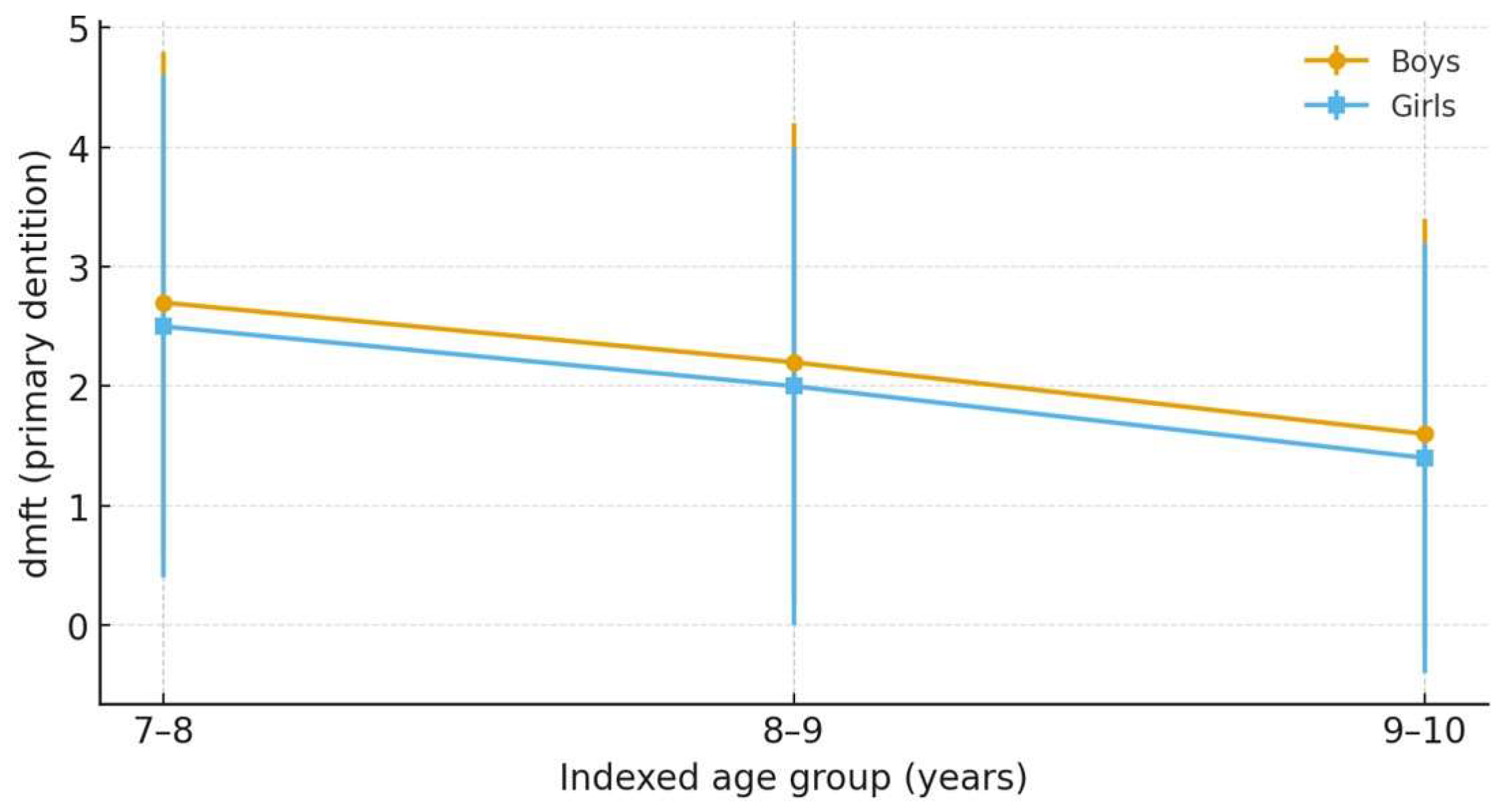
Gender-stratified dmft in the primary dentition decreased with age in both sexes (
Table 3). When sexes were combined (
Table 2), the mean dmft declined from 2.6 at 7–8 years to 1.5 at 9–10 years, while the proportion with dmft > 0 fell from 68% to 45%, indicating a marked reduction in primary-tooth caries burden across indexed ages.
Figure 3 depicts the primary-dentition dmft by indexed age and sex, shown as means with ± SD error bars (from
Table 3). In both sexes, dmft decreases with age—from 2.7 → 1.6 in boys and 2.5 → 1.4 in girls (7–8 to 9–10 years). Across ages, boys exhibit slightly higher dmft than girls; differences are modest and consistent with the gender-stratified values in
Table 3.
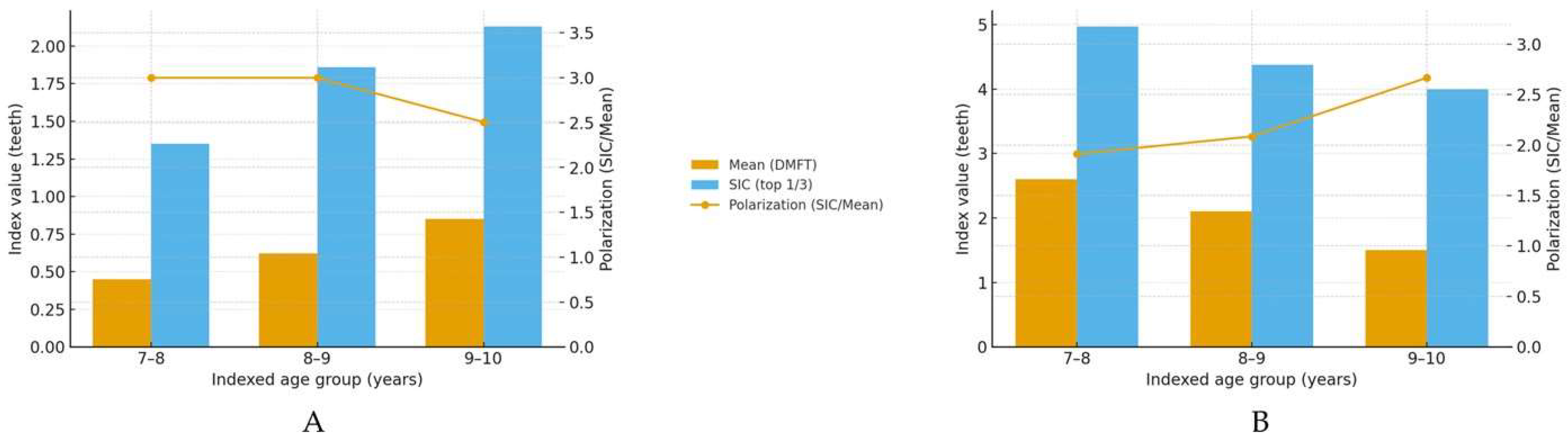
Age-specific SIC (mean ± SD) exceeded the corresponding mean in all groups, confirming polarization (
Table 4); in the primary dentition SIC declined from 4.97 ± 2.2 at 7–8 years to 4.00 ± 2.0 at 9–10 years (polarization 1.92→2.67), whereas in the permanent dentition it increased from 1.35 ± 1.2 to 2.13 ± 1.5 (polarization 3.00→2.50), consistent with the transition from primary to mixed dentition.
Figure 4 summarizes the Significant Caries Index (SIC) alongside the corresponding mean index within each age group and overlays the polarization (SIC/Mean). In the permanent dentition (DMFT), both the mean and SIC increase with age, while polarization declines modestly from ≈3.00 at 7–9 years to ≈2.50 at 9–10 years. In the primary dentition (dmft), the mean decreases with age, but SIC remains high, yielding higher polarization at 9–10 years (≈2.67), consistent with a concentrated burden among a minority of children as primary teeth exfoliate.
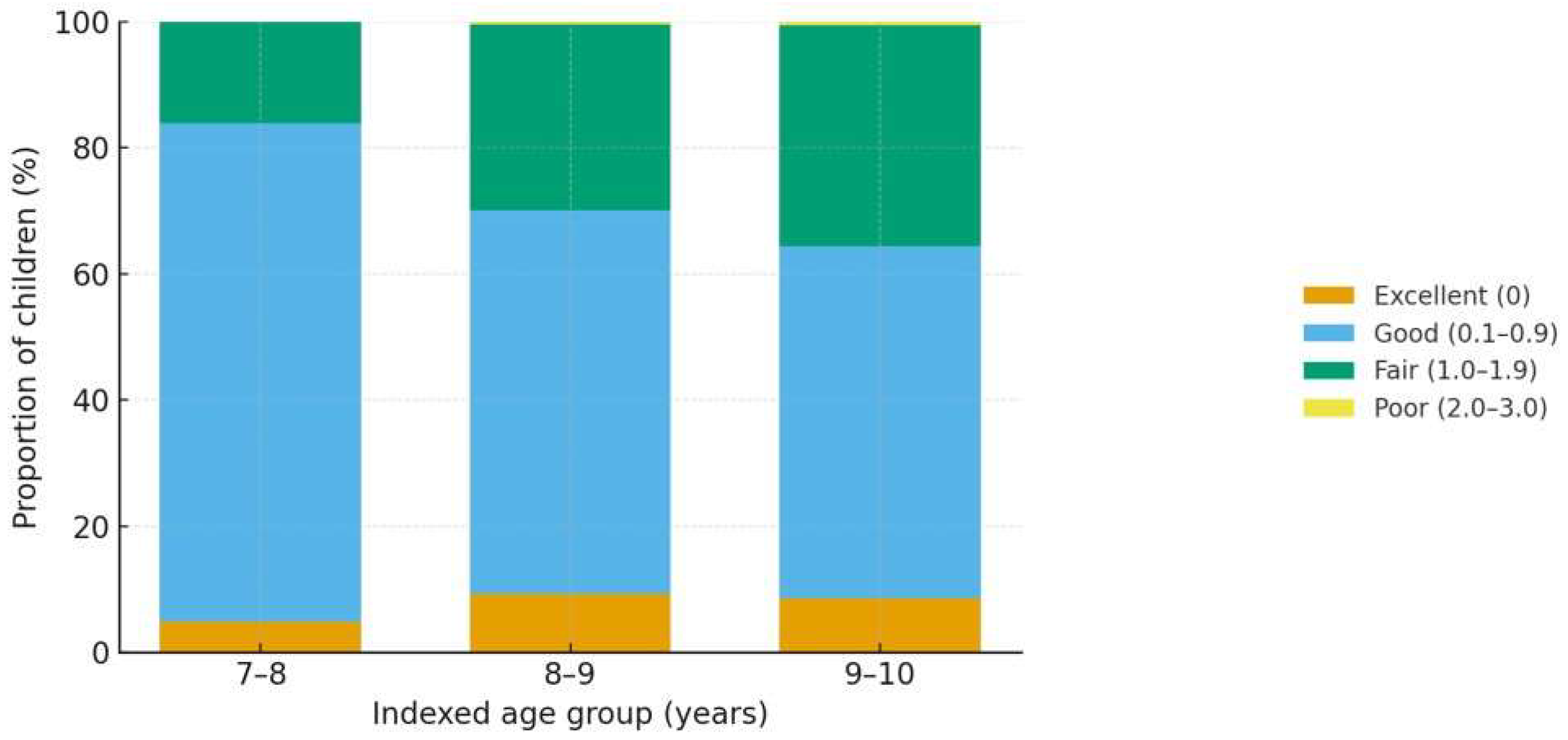
Table 5 presents the Silness–Löe Plaque Index (PI) by age, gender, and place of residence. The overall PI was 0.67 ± 0.41. By age, the mean plaque score increased progressively: 0.60 ± 0.30 at 7–8 years, 0.67 ± 0.43 at 8–9 years, and 0.73 ± 0.46 at 9–10 years, indicating a gradual rise in plaque accumulation across the indexed age groups. Consistent with this pattern, the distribution of PI categories (
Table 5) shows a higher share of children with clinically relevant plaque (PI ≥ 1.0) at older ages. Regarding gender, boys exhibited a slightly higher mean PI than girls (0.69 ± 0.36 vs. 0.65 ± 0.40;
p = 0.01). With respect to residence, children from rural areas recorded higher plaque levels than their urban counterparts (0.73 ± 0.38 vs. 0.61 ± 0.32;
p = 0.02). These differences underscore modest but consistent gradients by age, sex, and environment.
Figure 5 depicts the distribution of the Silness–Löe Plaque Index (PI) categories by indexed age groups. Consistent with
Table 5, the proportion of children in the fair category (PI 1.0–1.9) increases with age, while the good category (0.1–0.9) correspondingly decreases; the poor category (2.0–3.0) remains rare across ages.
In
Table 6, it is indicated that 563 children utilized toothpaste, resulting in an average plaque score of 0.75. In contrast, 137 children who employed dental floss achieved a plaque score of 0.88. Furthermore, among the cohort examined, 430 children reported brushing their teeth once per day, while 122 brushed twice daily, and 148 children brushed in an irregular manner. The corresponding mean plaque scores for these groups were recorded as 0.69, 0.60, and 0.75, respectively. Statistical analysis highlighted that these differences were significant, with a
p-value of less than 0.05.
Therefore, using toothpaste, flossing, and brushing teeth at least once a day has a significant impact on dental health among schoolchildren and, therefore, can prevent the development of cavities or periodontal disease. The values regarding children’s eating habits, together with the values for the average score of decayed, missing, and filled teeth, are presented in
Table 7.
The results show that the number of children with an eating frequency of 1–2 times per day was 61, 417 participants had an eating frequency of 2–3 times per day, and 222 participants declared that their eating frequency was above 4 times/day. The DMFT score according to the eating frequency was 0.61, 0.73, and 0.77, respectively. In addition, the results showed that 263 were low sugar usage children, 249 were medium usage, and 188 were high usage. The mean DMFT score according to the sugar usage per day was 0.55, 0.63, and 0.75, respectively. As concerns the administration of the snacks per day, the results showed that 245 children have a snack once/day; 280 children have snacks twice/day, and 175 children have snacks at least three times a day. The DMFT score according to the administration of the number of snacks/day was 0.56, 0.66, and 0.73, respectively. Also in this case, it seems that eating habits (especially daily sugar consumption (p = 0.01) and snacks between meals (p = 0.02)) significantly influence the occurrence of dental caries among schoolchildren.
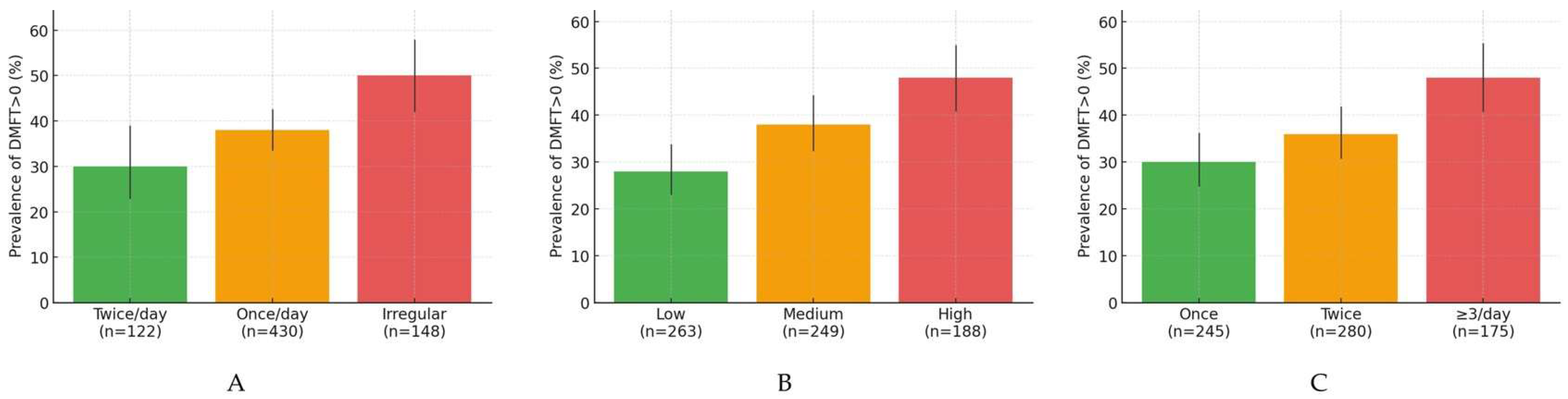
Figure 6A–C depicts the bivariate relationships between caries prevalence in the permanent dentition (DMFT > 0) and key hygiene/diet behaviors. Prevalence increases stepwise with poorer brushing frequency (twice/day → once/day → irregular), with higher daily sugar intake (low → medium → high), and with more snacks per day (once → twice → ≥3/day). Error bars indicate 95% Wilson confidence intervals based on the category-specific sample sizes shown on the
x-axis.
Table 8 shows the prevalence of caries in the permanent dentition (DMFT > 0) across hygiene and dietary categories. A clear graded pattern is evident: children who brush irregularly exhibit the highest prevalence, followed by those who brush once/day, with the lowest prevalence in those brushing twice/day. Similarly, prevalence rises from low to high daily sugar consumption and from 1 to ≥3 snacks per day. The gradient for the number of meals/day is modest by comparison. These bivariate findings mirror the severity trends reported in
Table 7 (higher mean DMFT with poorer hygiene and less favorable diet) and support a dose–response relationship between cariogenic behaviors and caries presence.
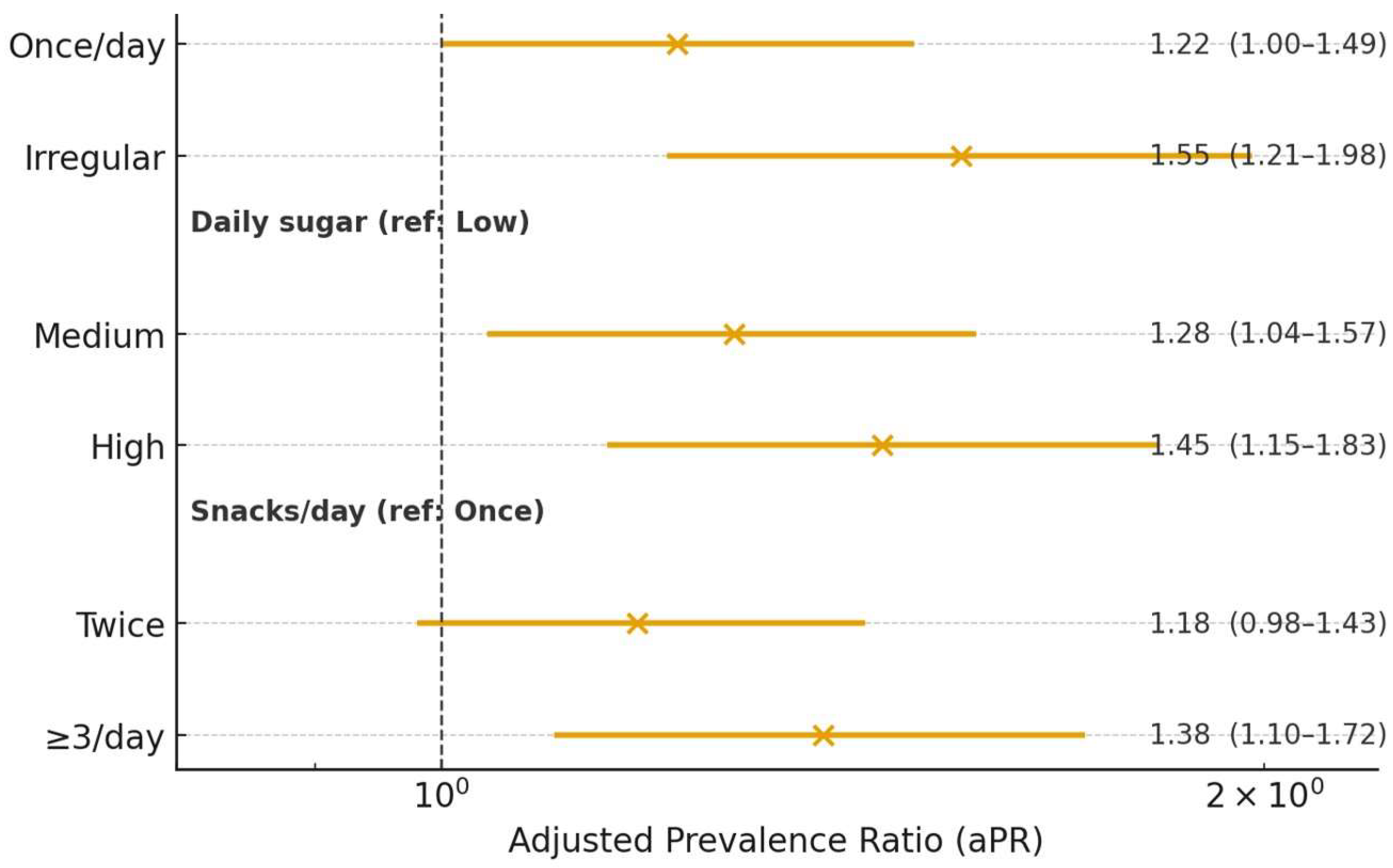
Table 9 presents adjusted prevalence ratios (aPR) from modified Poisson models with robust errors, controlling for age group, sex, and residence. After adjustment, irregular brushing remains independently associated with higher caries prevalence compared with twice/day brushing, while once/day brushing shows a smaller, intermediate increase. High daily sugar intake is associated with higher prevalence compared with low intake, and consuming ≥3 snacks/day is likewise associated with elevated prevalence relative to one snack/day; the “twice/day” snack category shows a weaker or borderline association. These results indicate that both hygiene practices and cariogenic dietary behaviors contribute independently to caries risk, reinforcing the need for combined hygiene education and sugar/snacking reduction strategies.
Figure 7 summarizes the adjusted associations between caries prevalence (DMFT > 0) and hygiene/diet behaviors. Estimates are adjusted prevalence ratios (aPR) from modified Poisson models with robust errors, controlling for age group, sex, and residence (
Table 9). As shown, the risk is higher with irregular brushing (aPR 1.55, 95% CI 1.21–1.98), high daily sugar intake (1.45, 1.15–1.83), and ≥3 snacks/day (1.38, 1.10–1.72), while intermediate categories show smaller or borderline effects.
Multivariable analyses confirmed the patterns observed regarding the eating and oral hygiene habits. After adjustment for age, sex, residence, plaque index, brushing frequency, flossing, daily sugar consumption, snack frequency, number of meals/day, and parental education, irregular brushing, higher daily sugar consumption, and ≥3 snacks/day were associated with higher prevalence ratios of having caries (DMFT > 0) and with greater DMFT counts (all p < 0.05). Similar associations were observed for dmft.
4. Discussion
Analyzing the results of this cross-sectional study, we can state that, by assessing the current dental status of the pediatric population and correlating it with hygiene and dietary habits, this study makes important contributions in the field of pediatric oral health and suggests new directions for improving preventive interventions. The study included 700 children with a nearly even split between boys (356) and girls (344), categorized into age groups 7–8, 8–9, and 9–10 years, from both urban and rural areas; children from rural areas participated in the study in greater numbers. A significant difference (
p < 0.05) was observed in the demographic profile based on the mother’s education and occupation, suggesting these factors influence children’s oral health. Caries experience in primary dentition (dmft index) decreased with age in both sexes from 7–8 to 9–10 years. Across ages, boys showed a slightly higher dmft index than girls. It has been stated that children in economically disadvantaged regions face considerable barriers to dental care due to a lack of awareness and lack of access to oral health education [
28,
29,
30,
31]. In economically underdeveloped regions, a lack of oral health awareness and education has been observed to further exacerbate the prevalence of dental caries among children [
32,
33,
34,
35,
36]. Instead, holistic programs that integrate oral hygiene awareness into broader public health promotion can significantly reduce the burden of oral disease among these populations [
37,
38,
39,
40]. Such integration can include interventions in schools that actively involve both children and their parents, leading to improved oral hygiene behaviors. Our results are in agreement with the literature data. For example, in the study reported by Babu et al. [
41], the authors determined the prevalence of dental caries and oral hygiene status in 1590 children (aged 7–12 years) of twenty schools in both rural and urban areas. The authors found a prevalence of dental caries of 65.6% among children (796 boys and 794 girls). Age groups 7–9 and 10–12 years of urban school children exhibited a higher prevalence of dental caries, and rural school children showed a poor oral hygiene status. Compared to boys and girls, the results of the authors showed that girls exhibit a higher prevalence of dental caries. Another research study found that socio-economic factors significantly correlated with higher caries rates in 6- and 12-year-olds, revealing both prevalence and severity reductions associated with increased access to preventive and restorative dental services [
42,
43]. Similarly, research in Kosovo emphasized that the prevalence of caries reflects regional disparities; schoolchildren’s dental caries was prevalent at alarming rates, further compounded by inadequate preventive measures and public health initiatives [
44].
In our study, the results showed that the father’s education did not have as significant an impact on the child’s dental health as the mother’s education (
p = 0.05 vs.
p = 0.02 (
Table 1). Numerous studies emphasize that a mother’s level of education and knowledge about dental health directly correlates with their children’s oral health behaviors and outcomes. Findings by Chen et al. suggest that mothers’ educational attainment confers a more substantial influence on family oral health practices than fathers’ [
45]. This observation aligns with the argument that mothers are often the primary caregivers who manage day-to-day health decisions, including oral hygiene, eating habits, and attendance at dental visits for their children [
2,
46]. In addition, maternal involvement in health behaviors tends to predict positive dental health outcomes in children. Research indicates that mothers with higher awareness and knowledge about dental hygiene not only set better oral health standards for their children but also actively participate in health-promoting behaviors such as regular dental check-ups [
47]. Therefore, while fathers play a critical role, particularly in terms of financial support for dental care, their involvement in daily health behaviors often does not match that of mothers in preventive oral health measures [
48].
Furthermore, our results showed that in the primary dentition, SIC declined from 4.97 ± 2.2 at 7–8 years to 4.00 ± 2.0 at 9–10 years, while in the permanent dentition, it increased. The concept of caries polarization is crucial for understanding how dental caries manifests among distinct subsets of populations. Research has revealed a consistent pattern where a minority of children bear the majority of the caries burden, referred to as “the 80/20 rule,” in which 20% of children experience 80% of the decay. This phenomenon has been assessed through the Caries Assessment Spectrum and Treatment (CAST) index, elucidating variations in caries severity among children, influenced significantly by their environment and educational background [
49,
50]. This is pertinent when considering implications for oral health interventions aimed at decreasing disparities, indicating educational improvements concerning dental hygiene could have substantial public health impacts. In addition, inadequate oral hygiene practices contribute significantly to the higher rates of dental caries observed in populations with lower socioeconomic status. This can often be attributed to a lack of awareness or education about proper oral health practices among parents and caregivers [
51]. This relationship is further complicated by eating habits influenced by socioeconomic stressors. Children from food-insecure families tend to consume diets high in carbohydrates and sugars, which favor the development of caries. Research indicates that these food choices are often driven by economic constraints, leading to poorer nutrition and subsequently poorer dental health outcomes. Studies have found that low socio-economic status is associated with dietary patterns that favor less nutritious choices, both due to financial limitations and lack of access to health-promoting foods [
52,
53].
Caries polarization is further emphasized through the use of the Simplified Oral Hygiene Index (SOPHI) and the Plaque Index. Studies demonstrate that despite knowledge about oral hygiene, such as tooth brushing frequency, there is often a gap in the practical application of this knowledge, with many children failing to brush effectively or regularly [
54,
55]. For example, while many children surveyed understood the necessity of regular brushing, many failed to adhere to this practice consistently, revealing a disconnect between knowledge and behavioral practices. This phenomenon is significant because correlations between poor oral hygiene habits and increased plaque indices have been established, leading to higher instances of gingivitis and caries [
56]. Our results showed that the mean plaque score increased progressively with age, with boys exhibiting slightly higher mean PI than girls (
p = 0.01), and rural children showing higher plaque levels than urban children (
p = 0.02) (
Table 5). Using toothpaste, flossing, and brushing teeth at least once a day has a significant impact on dental health among schoolchildren. In contrast with our study, Mahesh et al. [
57] reported that there was no statistically significant difference in the DMFT score of boys and girls in the age groups participating in their study (5-year-olds vs. 12-year-olds).
Additionally, dietary habits play an instrumental role in the prevalence and severity of dental caries in children aged 7–10 years. Several studies have highlighted that increased consumption of sugar-rich snacks and beverages correlates strongly with the incidence of caries among young children. Some studies outlined that frequent intake of sugar-rich diets and fizzy drinks is a contributing factor leading to a higher incidence of dental issues during formative years [
42,
54]. This trend reiterates the importance of dietary education alongside oral hygiene education in combating childhood caries. In our study, we found that regarding eating habits, daily sugar consumption (
p = 0.01) and snacks between meals (
p = 0.02) significantly influence the occurrence of dental caries among schoolchildren (
Table 7). These associations persisted after multivariable adjustment for demographic, hygiene, and dietary factors, indicating that irregular brushing, higher sugar intake, and frequent snacking are independent correlates of caries burden in this cohort. We found that children who brush irregularly exhibit the highest caries prevalence, followed by those who brush once/day. Caries prevalence rises with higher daily sugar consumption and more snacks per day. Irregular brushing, higher daily sugar consumption, and ≥3 snacks/day were associated with higher prevalence ratios of having caries (DMFT > 0) and with greater DMFT counts (all
p < 0.05). Once again, our data correlates with other reports. For example, previous studies showed that increased frequency of snacks and sugar intake was associated with higher DMFT values, while irregular brushing was linked to more caries, in line with our results [
58]. Other recent studies further emphasize the role of diet and microbiome [
59], as well as broader systemic processes such as neuroinflammation, in shaping oral and general health [
60].
Interventional studies have demonstrated that community-based oral health promotion projects can significantly enhance oral hygiene practices among schoolchildren. Programs designed to engage children with interactive and practical oral health education have successfully improved their brushing frequency and overall dental health awareness. In one longitudinal study conducted in Finland, a community intervention led to substantial improvements in children’s oral health knowledge and practices [
61]. The data suggest that such comprehensive programs could serve as effective models for enhancing oral health prevention strategies across diverse educational settings. Moreover, the involvement of teachers and parents in reinforcing oral hygiene practices is crucial. Several studies indicate that parental influence is a key determinant in children’s dental health behavior. Children whose parents exhibited good oral hygiene habits were more likely to adopt similar practices, highlighting the importance of socio-cultural factors in dental health promotion [
55,
62]. This underscores the necessity of developing educational initiatives that resonate well within various family and community contexts.
A multi-factorial approach emphasizing parent education, child-centered interactive learning, and psychological support for dental anxiety is needed to improve the dental status and oral hygiene practices of school children aged 7–10 years. Efficient implementation of these strategies can reduce the prevalence of dental caries and improve the overall dental health of this vulnerable population. Educational interventions designed specifically for children have proven effective in improving their oral health knowledge and subsequent oral health behaviors. Studies have reported that the use of engaging educational materials, such as animated videos and storytelling, can positively influence children’s attitudes towards dental hygiene and their willingness to participate in regular brushing habits [
63,
64,
65,
66,
67,
68]. Research indicates that children who engage in interactive learning experiences about dental care are more likely to maintain healthier dental practices outside the classroom environment. In the present study, there were 700 schoolchildren, with ages ranging from 7 to 10 years, of both genders.
In line with the results obtained in the present study, we believe that educational interventions aimed at parents and children will improve oral hygiene awareness and behaviors, thereby potentially reducing the incidence of periodontal disease in children. In addition, initiatives that emphasize the importance of oral health during early childhood can be effective, as early habits often influence long-term oral health outcomes [
69,
70]. Recent literature also highlights the importance of psychosocial factors, effective communication, and the use of modern methods such as virtual reality in improving both oral and general health [
71,
72,
73,
74,
75,
76,
77]. In addition, recent studies highlight the influence of contextual and behavioral factors on children’s oral health. The COVID-19 pandemic was associated with a deterioration of pediatric oral health, and the oral hygiene profile of Romanian schoolchildren indicates the need for preventive strategies adapted to local environments [
78,
79]. Socio-behavioral determinants remain strongly linked to caries status, while structured programs can improve oral hygiene behaviors in school-aged children [
80,
81]. Other findings emphasize the impact of environmental and lifestyle conditions, the effectiveness of interactive educational methods, the decisive role of parental involvement, and the value of preventive programs targeting mothers, even when delivered by non-dental professionals [
82,
83,
84,
85].
Taken together, these findings reinforce the importance of comprehensive, multi-level strategies that combine early education, psychosocial support, and contextual interventions to improve oral health in school-aged children.
5. Limitations of the Study
This study has several limitations that should be considered when interpreting the findings. First, the cross-sectional design precludes causal inference; the observed associations between hygiene/dietary behaviors and caries could be bidirectional or confounded by unmeasured factors.
Second, external validity is limited because participants were drawn from nine schools in two counties (Mureș and Bistrița-Năsăud, Romania) rather than from a nationally representative sample; selection and participation bias at the school or family level cannot be ruled out.
Third, behavioral exposures were parent/child-reported (tooth-brushing, flossing, meals/snacks, and sugar intake) and therefore are subject to recall and social-desirability bias; moreover, we did not apply a validated oral-health knowledge scale, so “knowledge and practice” were operationalized through reported behaviors rather than a separate knowledge score.
Fourth, caries was assessed clinically in school settings without adjunctive radiography, which likely led to under-detection of approximal/early lesions (a conservative bias in prevalence and severity estimates).
Fifth, residual confounding is possible: while models adjusted for key covariates (age, sex, residence, PI, brushing/flossing, sugar, snacks, meals, parental education), data on other determinants (e.g., fluoride exposure/sealants, beverage patterns, dental service use) were not collected, and clustering by school was not explicitly modeled, which could narrow confidence intervals.
Finally, data collection spanned one year (May 2024–May 2025); unmeasured period or seasonal effects in diet and routines may have influenced results.