Effects of Exergaming on Morphological Variables, Biochemical Parameters, and Blood Pressure in Children and Adolescents with Overweight/Obesity: A Systematic Review with Meta-Analysis of Randomized Controlled Trials
Abstract
1. Introduction
2. Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
| Category | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | Children or adolescents are considered to be participants under 18 years of age, according to UNICEF [22], and without distinction of sex, who are overweight/obese with a body mass index equal to or greater than 25.0 kg/m2 according to the World Health Organization [23]. | People over 18 have a body mass index below 25.0 kg/m2 [23]. |
| Intervention | Interventions use EXG or active non-immersive video games (i.e., Wii Sports, balance, and Fit, Switch Sports, Kinect Sports, Adventure and Your Shape, Sports Champions Move) for 4 weeks or more. | Interventions that do not use EXG or semi-immersive or immersive EXG as an intervention. There are no details of the intervention procedure. |
| Comparator | Interventions with active or inactive control groups. | Studies with no control groups or with inactive control groups. |
| Outcome | At least one assessment of morphological variables (i.e., body mass index, waist circumference, body composition), biochemical parameters (i.e., total cholesterol, HD-cholesterol, LDL-cholesterol, triglycerides, glucose), and blood pressure (systolic and diastolic blood pressure) before and after. | Lack of baseline data and/or follow-ups. |
| Study design | Randomized controlled trials, with pre- and post-assessment. | Non-randomized controlled trials, cross-sectional, retrospective, and prospective studies. |
2.3. Information Search Process and Databases
2.4. Studies Selection and Data Collection Process
2.5. Methodological Quality Assessment
2.6. Data Synthesis
2.7. Risk of Bias in Individual Studies
2.8. Summary Measures for Meta-Analysis
2.9. Moderator Analyses
2.10. Factor Analysis of Single Training
2.11. Certainty of Evidence
3. Results
3.1. Study Selection
3.2. Methodological Quality
| Study | Eligibility Criteria Specified | Randomly Allocated Participants | Allocation Concealed | Groups Similar at Baseline | Assessors Blinded | Outcome Measures Assessed >85% of Participants * | Intention to Treat Analysis | Reporting of Group Statistical Comparisons | Point Measures and Measures of Variability Reported ** | Activity Monitoring in Control Group | Relative Exercise Intensity Reviewed | Exercise Volume and Energy Expended | Overall TESTEX# |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abedelmalek, Aloui, Denguezli Bouzgarou, Adam, Souissi and Chtourou [36] | Yes | Yes | No | Yes | No | Yes (2) | No | Yes | Yes (2) | Yes | Yes | Yes | 11/15 |
| Staiano, Beyl, Guan, Hendrick, Hsia, and Newton [14] | Yes | Yes | Yes | Yes | Yes | Yes (2) | Yes | Yes | Yes (2) | Yes | No | Yes | 13/15 |
| Staiano, Marker, Beyl, Hsia, Katzmarzyk and Newton [34] | Yes | Yes | Yes | Yes | Yes | Yes (2) | Yes | Yes | Yes (2) | Yes | No | Yes | 13/15 |
| van Biljon, Longhurst, Shaw and Shaw [35] | Yes | Yes | No | Yes | No | Yes (1) | No | Yes | Yes (2) | Yes | No | Yes | 9/15 |
| Adamo, Rutherford and Goldfield [37] | Yes | Yes | No | Yes | No | Yes (2) | No | Yes | Yes (1) | Yes | Yes | Yes | 10/15 |
| Murphy, Carson, Neal, Baylis, Donley, and Yeater [38] | Yes | Yes | No | Yes | No | Yes (1) | No | Yes | Yes (1) | Yes | No | Yes | 8/15 |
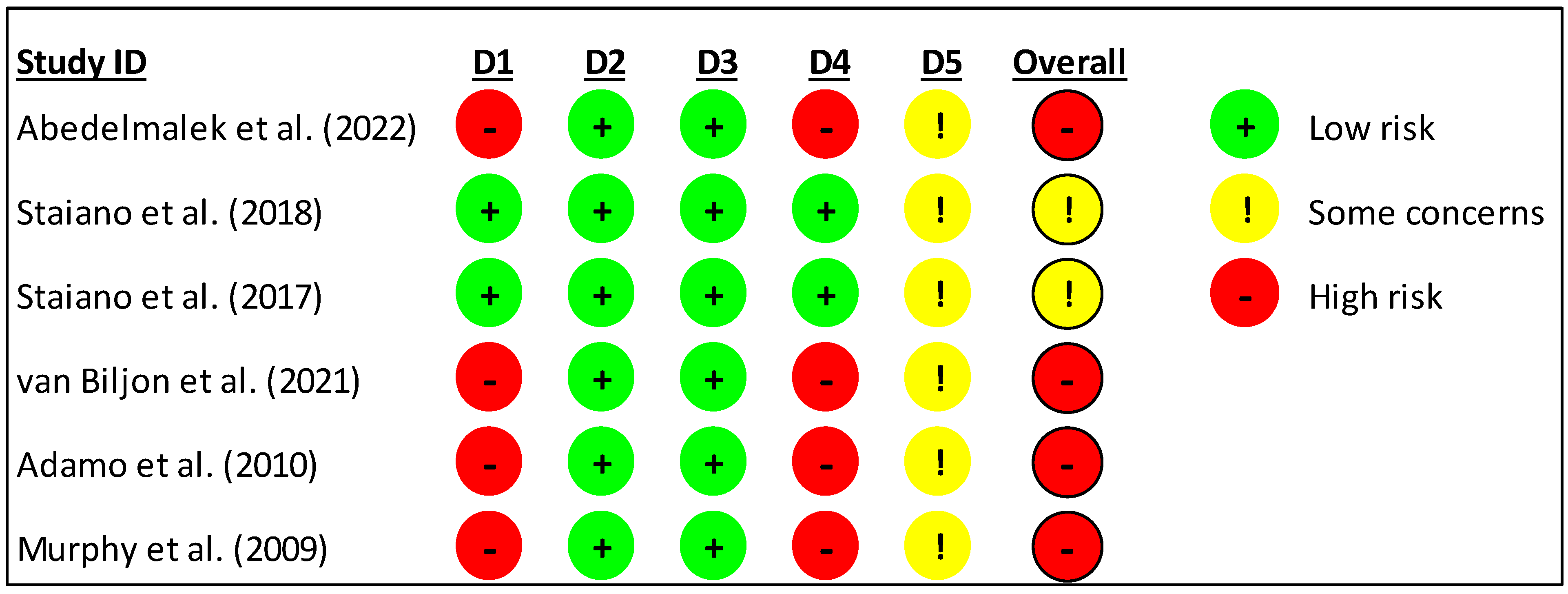
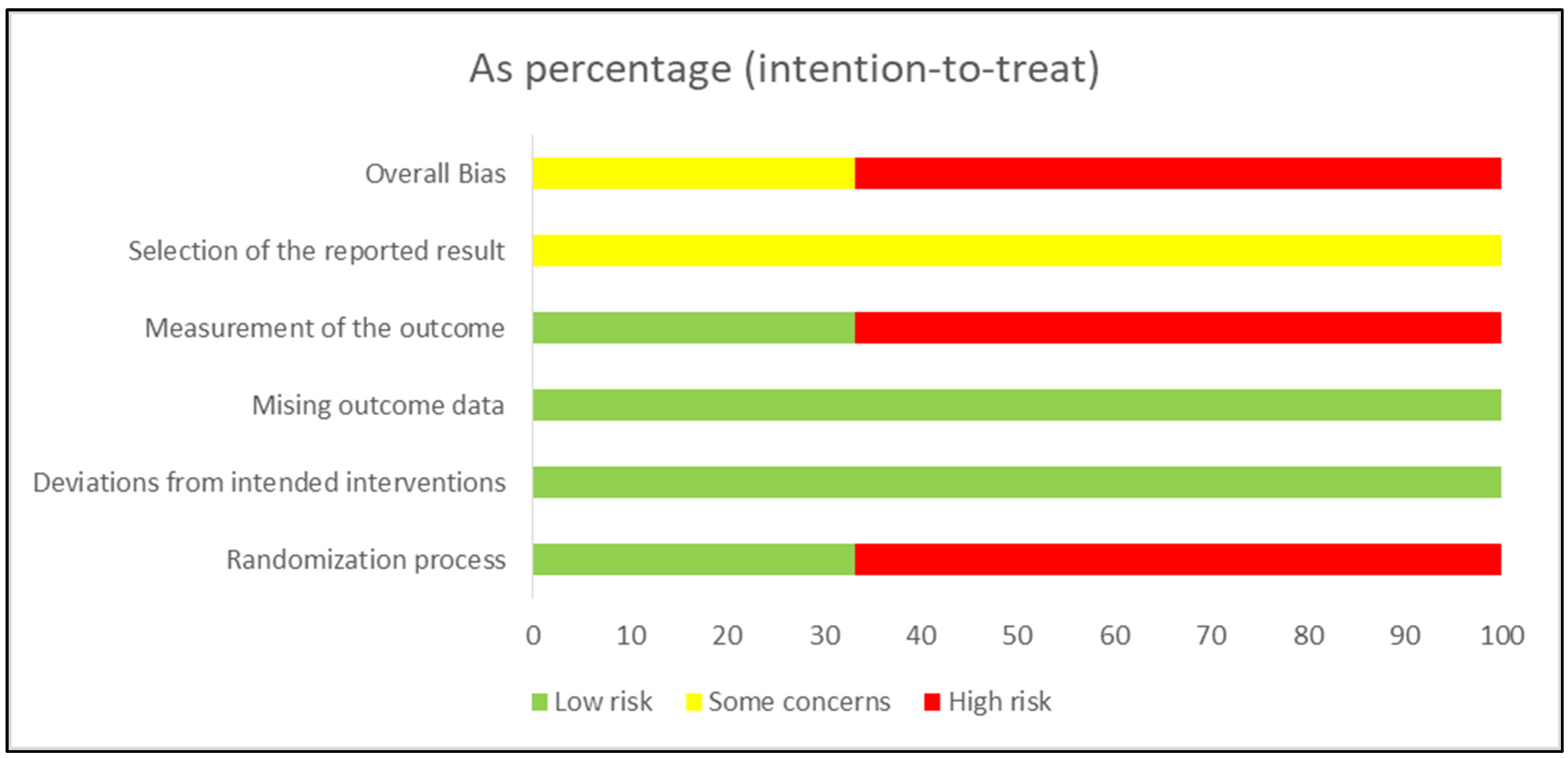
3.3. Risk of Bias
3.4. Studies Characteristics
3.5. Sample Characteristics
3.6. Dosing and Conducted Interventions
3.7. Meta-Analysis Results
3.8. Moderator Analyses
3.9. Certainty of Evidence
3.10. Adverse Events and Adherence
4. Discussion
4.1. Body Mass Index (BMI)
4.2. Waist Circumference
4.3. Body Fat Percentage
4.4. Biochemical Parameters (HDL-Cholesterol, LDL-Cholesterol, Total Cholesterol, and Triglycerides)
4.5. Blood Pressure
4.6. Glucose
4.7. Subgroup Analysis by Age
4.8. Subgroup Analysis by Training Duration
4.9. Subgroup Analysis by Training Frequency
4.10. Certainty of Evidence
4.11. Strengths and Limitations
4.12. Practical Applications
- EXG as a strategy for obesity management: the study highlights EXG as an effective strategy to combat childhood obesity. By integrating physical activity with gaming, EXG can enhance engagement and adherence among children and adolescents, making it a viable alternative to conventional physical activity programs.
- Improved biochemical parameters in children < 15 years of age: findings suggest that exercise with EXG can significantly improve lipid profiles, including reductions in total cholesterol, LDL-cholesterol, and triglycerides while increasing HDL cholesterol; this suggests that exercise with EXG can be incorporated into programs aimed at improving cardiovascular health in children and adolescents with overweight/obesity.
- Promotion of long-term physical activity: the study emphasizes the potential of EXG to increase enjoyment and motivation for physical activity, which is crucial for fostering long-term adherence to an active lifestyle; this can lead to sustained health benefits beyond the intervention period.
- Customizable intervention programs: given the variability in the types of games and consoles used, EXG interventions can be tailored to individual preferences and capabilities, enhancing their effectiveness and appeal to diverse populations.
- Integration with nutritional guidance: the study suggests that combining EXG with dietary control could optimize body composition and metabolic health outcomes. This integrated approach can be particularly beneficial in comprehensive weight management programs.
- Potential for school-based implementation: EXG can be easily implemented in school settings, providing a structured environment for regular physical activity; this can help reach a larger population of children and adolescents, contributing to public health efforts in reducing obesity rates.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Global Atlas on Childhood Obesity. The First Global Atlas on Childhood Obesity by the World Obesity Federation (WOF) Shows That Nocountry Has a Better than Fifty Percent Chance of Meeting Their Target for Tackling Childhood Obesity; World Obesity Federation: London, UK, 2021. [Google Scholar]
- Ling, J.; Chen, S.; Zahry, N.R.; Kao, T.A. Economic burden of childhood overweight and obesity: A systematic review and meta-analysis. Obes. Rev. 2023, 24, e13535. [Google Scholar] [CrossRef] [PubMed]
- Fabin-Czepiel, K.; Pieczyńska-Chapuła, K.; Deja, G. “The obesity pandemic” in the COVID-19 pandemic—New treatment for an old problem. Pediatr. Endocrinol. Diabetes Metab. 2023, 29, 104–111. [Google Scholar] [CrossRef]
- Orsini, F.; D’Ambrosio, F.; Scardigno, A.; Ricciardi, R.; Calabrò, G.E. Epidemiological Impact of Metabolic Syndrome in Overweight and Obese European Children and Adolescents: A Systematic Literature Review. Nutrients 2023, 15, 3895. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Martinez, J.; Vera-Assaoka, T.; González-Castillo, C.; Castillo-Cerda, M.A.; Therrera-Valenzuela, T.; Guzmán-Muñoz, E.; Magani Branco, B.H.; Valdés-Badilla, P. Hábitos de actividad física asociados a variables de salud en escolares chilenos varones: Estilos de vida en escolares chilenos. Nutr. Clínica Dietética Hosp. 2024, 44, 74–83. [Google Scholar] [CrossRef]
- Lindberg, L.; Danielsson, P.; Persson, M.; Marcus, C.; Hagman, E. Association of childhood obesity with risk of early all-cause and cause-specific mortality: A Swedish prospective cohort study. PLoS Med. 2020, 17, e1003078. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Xiang, S.T.; Dong, J.; Zhong, Y.; Zhao, S.; Xiao, Z.; Li, L. Association between Physical Activity and Age among Children with Overweight and Obesity: Evidence from the 2016–2017 National Survey of Children’s Health. Biomed. Res. Int. 2020, 2020, 9259742. [Google Scholar] [CrossRef] [PubMed]
- García-Hermoso, A.; López-Gil, J.F.; Izquierdo, M.; Ramírez-Vélez, R.; Ezzatvar, Y. Exercise and Insulin Resistance Markers in Children and Adolescents With Excess Weight: A Systematic Review and Network Meta-Analysis. JAMA Pediatr. 2023, 177, 1276–1284. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Li, Q.; Lu, F.; Zhu, D. Effects of aerobic exercise combined with resistance training on body composition and metabolic health in children and adolescents with overweight or obesity: Systematic review and meta-analysis. Front. Public Health 2024, 12, 1409660. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Liu, J.; Yu, Y.; Tian, Z. Effect of high-intensity interval training on cardiometabolic risk factors in childhood obesity: A meta-analysis. J. Sports Med. Phys. Fit. 2021, 61, 743–752. [Google Scholar] [CrossRef]
- Qi, J.; Yan, Y.; Yin, H. Screen time among school-aged children of aged 6–14: A systematic review. Glob. Health Res. Policy 2023, 8, 12. [Google Scholar] [CrossRef] [PubMed]
- Mittal, P.; Bhadania, M.; Tondak, N.; Ajmera, P.; Yadav, S.; Kukreti, A.; Kalra, S.; Ajmera, P. Effect of immersive virtual reality-based training on cognitive, social, and emotional skills in children and adolescents with autism spectrum disorder: A meta-analysis of randomized controlled trials. Res. Dev. Disabil. 2024, 151, 104771. [Google Scholar] [CrossRef] [PubMed]
- Flôres, F.; Silva, A.; Willig, R.; Reyes, A.; Serpa, J.; Marconcin, P.; Vieira, F.; Soares, D.; Casanova, N. Exergames as an Effective Alternative to Real Environmental Tennis Training for Adolescents. Sports 2024, 12, 168. [Google Scholar] [CrossRef] [PubMed]
- Staiano, A.E.; Beyl, R.A.; Guan, W.; Hendrick, C.A.; Hsia, D.S.; Newton, R.L., Jr. Home-based exergaming among children with overweight and obesity: A randomized clinical trial. Pediatr. Obes. 2018, 13, 724–733. [Google Scholar] [CrossRef] [PubMed]
- Valeriani, F.; Protano, C.; Marotta, D.; Liguori, G.; Romano Spica, V.; Valerio, G.; Vitali, M.; Gallè, F. Exergames in Childhood Obesity Treatment: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 4938. [Google Scholar] [CrossRef] [PubMed]
- Marsigliante, S.; My, G.; Mazzotta, G.; Muscella, A. The Effects of Exergames on Physical Fitness, Body Composition and Enjoyment in Children: A Six-Month Intervention Study. Children 2024, 11, 1172. [Google Scholar] [CrossRef] [PubMed]
- Comeras-Chueca, C.; Marin-Puyalto, J.; Matute-Llorente, A.; Vicente-Rodriguez, G.; Casajus, J.A.; Gonzalez-Aguero, A. The Effects of Active Video Games on Health-Related Physical Fitness and Motor Competence in Children and Adolescents with Healthy Weight: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 6965. [Google Scholar] [CrossRef]
- Erçelik, Z.E.; Çağlar, S. Effectiveness of active video games in overweight and obese adolescents: A systematic review and meta-analysis of randomized controlled trials. Ann. Pediatr. Endocrinol. Metab. 2022, 27, 98–104. [Google Scholar] [CrossRef]
- Pereira, E.V.; Morais, G.L.d.; Gabriel, I.R.; Claumann, G.S.; Helal, L.C.A.S.; Roever, L.; Farias, J.M.d. Impact of Exergames on BMI and Cardiovascular Risk Factors: A Systematic Review. Rev. Bras. Med. Esporte 2024, 30, e2021_0508. [Google Scholar] [CrossRef]
- Chen, Y.; Cao, L.; Xu, Y.; Zhu, M.; Guan, B.; Ming, W.K. Effectiveness of virtual reality in cardiac rehabilitation: A systematic review and meta-analysis of randomized controlled trials. Int. J. Nurs. Stud. 2022, 133, 104323. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- UNICEF. Convention on the Rights of the Child: Children’s Version; UNICEF: New York, NY, USA, 2019. [Google Scholar]
- World Health Organization. Obesity and Overweight; World Health Organization: Geneva, Switzerland, 2024. [Google Scholar]
- Smart, N.A.; Waldron, M.; Ismail, H.; Giallauria, F.; Vigorito, C.; Cornelissen, V.; Dieberg, G. Validation of a new tool for the assessment of study quality and reporting in exercise training studies: TESTEX. Int. J. Evid. Based Healthc. 2015, 13, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Davey, J.; Turner, R.M.; Clarke, M.J.; Higgins, J.P. Characteristics of meta-analyses and their component studies in the Cochrane Database of Systematic Reviews: A cross-sectional, descriptive analysis. BMC Med. Res. Methodol. 2011, 11, 160. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive statistics for studies in sports medicine and exercise science. Med. Sci. Sports Exerc. 2009, 41, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Verhagen, A.P.; de Vet, H.C.; de Bie, R.A.; Kessels, A.G.; Boers, M.; Bouter, L.M.; Knipschild, P.G. The Delphi list: A criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J. Clin. Epidemiol. 1998, 51, 1235–1241. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Headid Iii, R.J.; Park, S.Y. The impacts of exercise on pediatric obesity. Clin. Exp. Pediatr. 2021, 64, 196–207. [Google Scholar] [CrossRef] [PubMed]
- Valentine, J.C.; Pigott, T.D.; Rothstein, H.R. How Many Studies Do You Need?: A Primer on Statistical Power for Meta-Analysis. J. Educ. Behav. Stat. 2010, 35, 215–247. [Google Scholar] [CrossRef]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; DeBeer, H.; et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef]
- Staiano, A.E.; Marker, A.M.; Beyl, R.A.; Hsia, D.S.; Katzmarzyk, P.T.; Newton, R.L. A randomized controlled trial of dance exergaming for exercise training in overweight and obese adolescent girls. Pediatr. Obes. 2017, 12, 120–128. [Google Scholar] [CrossRef]
- van Biljon, A.; Longhurst, G.; Shaw, I.; Shaw, B. Role of Exergame Play on Cardiorespiratory Fitness and Body Composition in Overweight and Obese Children. Asian J. Sports Med. 2021, 12, e106782. [Google Scholar] [CrossRef]
- Abedelmalek, S.; Aloui, K.; Denguezli Bouzgarou, M.; Adam, H.; Souissi, N.; Chtourou, H. Exergaming During Ramadan Intermittent Fasting Improve Body Composition as Well as Physiological and Psychological Responses to Physical Exercise in Adolescents With Obesity. Front. Nutr. 2022, 9, 851054. [Google Scholar] [CrossRef] [PubMed]
- Adamo, K.B.; Rutherford, J.A.; Goldfield, G.S. Effects of interactive video game cycling on overweight and obese adolescent health. Appl. Physiol. Nutr. Metab. 2010, 35, 805–815. [Google Scholar] [CrossRef]
- Murphy, E.C.; Carson, L.; Neal, W.; Baylis, C.; Donley, D.; Yeater, R. Effects of an exercise intervention using Dance Dance Revolution on endothelial function and other risk factors in overweight children. Int. J. Pediatr. Obes. 2009, 4, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Eglseer, D.; Traxler, M.; Embacher, S.; Reiter, L.; Schoufour, J.D.; Weijs, P.J.M.; Voortman, T.; Boirie, Y.; Cruz-Jentoft, A.; Bauer, S. Nutrition and Exercise Interventions to Improve Body Composition for Persons with Overweight or Obesity Near Retirement Age: A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials. Adv. Nutr. 2023, 14, 516–538. [Google Scholar] [CrossRef] [PubMed]
- Carayanni, V.; Vlachopapadopoulou, E.; Koutsouki, D.; Bogdanis, G.C.; Psaltopoulou, T.; Manios, Y.; Karachaliou, F.; Hatzakis, A.; Michalacos, S. Effects of Nutrition, and Physical Activity Habits and Perceptions on Body Mass Index (BMI) in Children Aged 12–15 Years: A Cross-Sectional Study Comparing Boys and Girls. Children 2021, 8, 277. [Google Scholar] [CrossRef] [PubMed]
- Aygün, C.; Çakır-Atabek, H. Classification of Exergames with Different Types: Perceptual and Physiological Responses in College Students. Appl. Sci. 2023, 13, 10769. [Google Scholar] [CrossRef]
- Gao, Z.; Chen, S. Are field-based exergames useful in preventing childhood obesity? A systematic review. Obes. Rev. 2014, 15, 676–691. [Google Scholar] [CrossRef] [PubMed]
- Calcaterra, V.; Vandoni, M.; Marin, L.; Carnevale Pellino, V.; Rossi, V.; Gatti, A.; Patanè, P.; Cavallo, C.; Re, F.; Albanese, I.; et al. Exergames to Limit Weight Gain and to Fight Sedentarism in Children and Adolescents with Obesity. Children 2023, 10, 928. [Google Scholar] [CrossRef] [PubMed]
- Lamboglia, C.M.; da Silva, V.T.; de Vasconcelos Filho, J.E.; Pinheiro, M.H.; Munguba, M.C.; Silva Júnior, F.V.; de Paula, F.A.; da Silva, C.A. Exergaming as a strategic tool in the fight against childhood obesity: A systematic review. J. Obes. 2013, 2013, 438364. [Google Scholar] [CrossRef][Green Version]
- Oliveira, C.B.; Pinto, R.Z.; Saraiva, B.T.C.; Tebar, W.R.; Delfino, L.D.; Franco, M.R.; Silva, C.C.M.; Christofaro, D.G.D. Effects of active video games on children and adolescents: A systematic review with meta-analysis. Scand. J. Med. Sci. Sports 2020, 30, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Yao, W.; Han, Y.; Yang, L.; Chen, Y.; Yan, S.; Cheng, Y. Electronic Interactive Games for Glycemic Control in Individuals With Diabetes: Systematic Review and Meta-Analysis. JMIR Serious Games 2024, 12, e43574. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.S.; Ho, B.; Goh, Y.S. Effectiveness of game-based exercise interventions on modifiable cardiovascular risk factors of individuals with type two diabetes mellitus: A systematic review and meta-analysis. Worldviews Evid. Based Nurs. 2023, 20, 377–400. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Ramie, J.J.; Barber, J.L.; Sarzynski, M.A. Effects of exercise on HDL functionality. Curr. Opin. Lipidol. 2019, 30, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Franczyk, B.; Gluba-Brzózka, A.; Ciałkowska-Rysz, A.; Ławiński, J.; Rysz, J. The Impact of Aerobic Exercise on HDL Quantity and Quality: A Narrative Review. Int. J. Mol. Sci. 2023, 24, 4653. [Google Scholar] [CrossRef]
- Kircher, E.; Ketelhut, S.; Ketelhut, K.; Röglin, L.; Hottenrott, K.; Martin-Niedecken, A.L.; Ketelhut, R.G. A Game-Based Approach to Lower Blood Pressure? Comparing Acute Hemodynamic Responses to Endurance Exercise and Exergaming: A Randomized Crossover Trial. Int. J. Environ. Res. Public Health 2022, 19, 1349. [Google Scholar] [CrossRef] [PubMed]
- Casonatto, J.; Goessler, K.F.; Cornelissen, V.A.; Cardoso, J.R.; Polito, M.D. The blood pressure-lowering effect of a single bout of resistance exercise: A systematic review and meta-analysis of randomised controlled trials. Eur. J. Prev. Cardiol. 2020, 23, 1700–1714. [Google Scholar] [CrossRef] [PubMed]
- Carrel, A.L.; Clark, R.R.; Peterson, S.E.; Nemeth, B.A.; Sullivan, J.; Allen, D.B. Improvement of fitness, body composition, and insulin sensitivity in overweight children in a school-based exercise program: A randomized, controlled study. Arch. Pediatr. Adolesc. Med. 2005, 159, 963–968. [Google Scholar] [CrossRef]
- Nassis, G.P.; Papantakou, K.; Skenderi, K.; Triandafillopoulou, M.; Kavouras, S.A.; Yannakoulia, M.; Chrousos, G.P.; Sidossis, L.S. Aerobic exercise training improves insulin sensitivity without changes in body weight, body fat, adiponectin, and inflammatory markers in overweight and obese girls. Metabolism 2005, 54, 1472–1479. [Google Scholar] [CrossRef]
- Ambelu, T.; Teferi, G. The impact of exercise modalities on blood glucose, blood pressure and body composition in patients with type 2 diabetes mellitus. BMC Sports Sci. Med. Rehabil. 2023, 15, 153. [Google Scholar] [CrossRef] [PubMed]
- Church, T.S.; Cheng, Y.J.; Earnest, C.P.; Barlow, C.E.; Gibbons, L.W.; Priest, E.L.; Blair, S.N. Exercise capacity and body composition as predictors of mortality among men with diabetes. Diabetes Care 2004, 27, 83–88. [Google Scholar] [CrossRef]
- Mann, S.; Beedie, C.; Jimenez, A. Differential effects of aerobic exercise, resistance training and combined exercise modalities on cholesterol and the lipid profile: Review, synthesis and recommendations. Sports Med. 2014, 44, 211–221. [Google Scholar] [CrossRef]
- Liu, W.; Zeng, N.; McDonough, D.J.; Gao, Z. Effect of Active Video Games on Healthy Children’s Fundamental Motor Skills and Physical Fitness: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 8264. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, M.J.; Ramos-Espinoza, F.; Muñoz-Vásquez, C.; Guzman-Muñoz, E.; Herrera-Valenzuela, T.; Branco, B.H.M.; Castillo-Cerda, M.; Valdés-Badilla, P. Effects of active exergames on physical performance in older people: An overview of systematic reviews and meta-analysis. Front. Public. Health 2024, 12, 1250299. [Google Scholar] [CrossRef]
- Hernandez, M.J.; Cid-Calfucura, I.; Herrera-Valenzuela, T.; Fritz-Silva, N.; Mello, J.B.; Perez-Carcamo, J.; Vásquez-Carrasco, E.; Merellano-Navarro, E.; Branco, B.H.M.; Valdés-Badilla, P. Xbox Kinect Sports vs. Nintendo Switch Sports and Their Effects on Body Composition and Physical Performance in Older Females: A Randomized Controlled Trial. J. Clin. Med. 2024, 13, 4987. [Google Scholar] [CrossRef] [PubMed]

| Morphological Variables, Biochemical Parameters, and Blood Pressure | n a | ES (95%CI) | p | I2 (%) | Egger’s Test (p) | RW (%) |
|---|---|---|---|---|---|---|
| Morphological variables | ||||||
| BMI (kg m−2) | 4, 4, 4, 155. | 0.51 (0.01 to 1.01) | 0.04 | 52.2 | 0.09 | 3.17 to 4.48 |
| Waist circumference (cm) | 3, 3, 3, 90. | 0.64 (0.03 to 1.26) | 0.03 | 52.8 | 0.12 | 3.12 to 3.85 |
| Body fat percentage (%) | 3, 3, 3, 90. | 0.003 (−0.39 to 0.40) | 0.99 | 0.00 | 0.68 | 6.38 to 10.5 |
| Biochemical parameters | ||||||
| Total cholesterol (mg/dl) | 5, 5, 5, 173. | 0.38 (−0.14 to 0.90) | 0.15 | 63.7 | 0.02 | 2.30 to 3.15 |
| LDL-cholesterol (mg/dl) | 5, 5, 5, 173. | 0.31 (−0.23 to 0.85) | 0.26 | 66.6 | 0.01 | 2.07 to 2.88 |
| HDL-cholesterol (mg/dl) | 5, 5, 5, 173. | −0.20 (−0.77 to 0.36) | 0.48 | 69.6 | 0.01 | 1.92 to 2.64 |
| Triglycerides (mmol/L−1) | 5, 5, 5, 173. | 0.42 (−0.19 to 1.03) | 0.17 | 72.9 | 0.005 | 1.77 to 2.27 |
| Glucose (mg/dl) | 3, 3, 3, 148. | 0.40 (−0.13 to 0.94) | 0.14 | 55,2 | 0.10 | 3.89 to 4.74 |
| Blood pressure | ||||||
| SBP (mmHg) | 4, 4, 4, 143. | 0.45 (0.12 to 0.78) | 0.007 | 0.00 | 0.44 | 5.64 to 11.0 |
| DBP (mmHg) | 4, 4, 4, 143. | 0.08 (−0.67 to 0.83) | 0.83 | 79.9 | 0.02 | 1.53 to 1.76 |
| Assessment of Certainty | Number of Patients | Effect | Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Studies | Study Design | Risk of Bias | Inconsistency | Indirect Evidence | Vagueness | Other Considerations | Exergaming | Control Group | Relative (95% CI) | Absolute (95% CI) | ||
| Exergaming During Ramadan Intermittent Fasting Improve Body Composition as Well as Physiological and Psychological Responses to Physical Exercise in Adolescents with Obesity | ||||||||||||
| 1 | Randomized trials | Very serious a | It’s not serious | It’s not serious | It’s not serious | None | 12/24 (50.0%) | 12/24 (50.0%) | not estimable | ⨁⨁ ◯◯ Go down a | IMPORTANT | |
| Effects of interactive video game cycling on overweight and obese adolescent health | ||||||||||||
| 1 | Randomized trials | Serious b | It’s not serious | It’s not serious | It’s not serious | None | 13/26 (50.0%) | 13/26 (50.0%) | not estimable | ⨁⨁⨁ ◯ Moderate b | IMPORTANT | |
| Effects of an exercise intervention using Dance Revolution on endothelial function and other risk factors in overweight children | ||||||||||||
| 1 | Randomized trials | Serious b | It’s not serious | It’s not serious | It’s not serious | None | 13/35 (37.1%) | 22/35 (62.9%) | not estimable | ⨁⨁⨁ ◯ Moderate b | IMPORTANT | |
| Home-based exergaming among children with overweight and obesity: a randomized clinical trial | ||||||||||||
| 1 | Randomized trials | Very serious a | It’s not serious | It’s not serious | It’s not serious | None | 23/46 (50.0%) | 23/46 (50.0%) | not estimable | ⨁⨁ ◯◯ Go down a | IMPORTANT | |
| A randomized controlled trial of dance exergaming for exercise training in overweight and obese adolescent girls | ||||||||||||
| 1 | Randomized trials | Serious b | It’s not serious | It’s not serious | It’s not serious | None | 22/41 (53.7%) | 19/41 (46.3%) | not estimable | ⨁⨁⨁ ◯ Moderate b | NOT IMPORTANT | |
| Role of Exergame Play on Cardiorespiratory Fitness and Body Composition in Overweight and Obese Children | ||||||||||||
| 1 | Randomized trials | Very serious a | It’s not serious | It’s not serious | It’s not serious | None | 21/31 (67.7%) | 10/31 (32.3%) | not estimable | ⨁⨁ ◯◯ Go down a | IMPORTANT | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernandez-Martinez, J.; Perez-Carcamo, J.; Melki, H.; Cid-Calfucura, I.; Vasquez-Carrasco, E.; Delgado-Floody, P.; Romero, C.; Herrera-Valenzuela, T.; Branco, B.H.M.; Valdés-Badilla, P. Effects of Exergaming on Morphological Variables, Biochemical Parameters, and Blood Pressure in Children and Adolescents with Overweight/Obesity: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. Children 2025, 12, 29. https://doi.org/10.3390/children12010029
Hernandez-Martinez J, Perez-Carcamo J, Melki H, Cid-Calfucura I, Vasquez-Carrasco E, Delgado-Floody P, Romero C, Herrera-Valenzuela T, Branco BHM, Valdés-Badilla P. Effects of Exergaming on Morphological Variables, Biochemical Parameters, and Blood Pressure in Children and Adolescents with Overweight/Obesity: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. Children. 2025; 12(1):29. https://doi.org/10.3390/children12010029
Chicago/Turabian StyleHernandez-Martinez, Jordan, Joaquín Perez-Carcamo, Hassan Melki, Izham Cid-Calfucura, Edgar Vasquez-Carrasco, Pedro Delgado-Floody, Claudio Romero, Tomás Herrera-Valenzuela, Braulio Henrique Magnani Branco, and Pablo Valdés-Badilla. 2025. "Effects of Exergaming on Morphological Variables, Biochemical Parameters, and Blood Pressure in Children and Adolescents with Overweight/Obesity: A Systematic Review with Meta-Analysis of Randomized Controlled Trials" Children 12, no. 1: 29. https://doi.org/10.3390/children12010029
APA StyleHernandez-Martinez, J., Perez-Carcamo, J., Melki, H., Cid-Calfucura, I., Vasquez-Carrasco, E., Delgado-Floody, P., Romero, C., Herrera-Valenzuela, T., Branco, B. H. M., & Valdés-Badilla, P. (2025). Effects of Exergaming on Morphological Variables, Biochemical Parameters, and Blood Pressure in Children and Adolescents with Overweight/Obesity: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. Children, 12(1), 29. https://doi.org/10.3390/children12010029










