Preformed Elastodontic Appliances: Awareness and Attitude of Orthodontists and General Dental Practitioners
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. The Questionnaire: Structure and Content
2.3. Survey Dissemination
2.4. Data Collection and Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
List of Abbreviations
| EAs | performed elastodontic appliances |
| Os | orthodontists |
| GDPs | general dental practitioners |
| OVJ | overjet |
| OVB | overbite |
References
- Mostafiz, W. Fundamentals of Interceptive Orthodontics: Optimizing Dentofacial Growth and Development. Compend. Contin. Educ. Dent. 2019, 40, 149–154, quiz 155. [Google Scholar] [PubMed]
- Arvystas, M.G. The Rationale for Early Orthodontic Treatment. Am. J. Orthod. Dentofac. Orthop. 1998, 113, 15–18. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.L.; Awang, C.F.; Ng, L.K.; Norlian, D.; Burhanudin, R.D.; Gere, M.J. Role of Interceptive Orthodontics in Early Mixed Dentition. Singap. Dent. J. 2004, 26, 10–14. [Google Scholar]
- Wishney, M.; Darendeliler, M.A.; Dalci, O. Myofunctional Therapy and Prefabricated Functional Appliances: An Overview of the History and Evidence. Aust. Dent. J. 2019, 64, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Ronsivalle, V.; Quinzi, V.; La Rosa, S.; Leonardi, R.; Lo Giudice, A. Comparative Analysis of Skeletal Changes, Occlusal Changes, and Palatal Morphology in Children with Mild Class III Malocclusion Treated with Elastodontic Appliances and Bimaxillary Plates. Children 2023, 10, 1219. [Google Scholar] [CrossRef]
- Quinzi, V.; Gallusi, G.; Carli, E.; Pepe, F.; Rastelli, E.; Tecco, S. Elastodontic Devices in Orthodontics: An In-Vitro Study on Mechanical Deformation under Loading. Bioengineering 2022, 9, 282. [Google Scholar] [CrossRef]
- Macrì, M.; Ritrovato, L.; Pisanelli, E.L.; Festa, F. Elastodontic Therapy with Oral Bioactivator Devices: A Review. Appl. Sci. 2023, 13, 8868. [Google Scholar] [CrossRef]
- Ortu, E.; Barrucci, G.; Aprile, G.; Guerrini, L.; Pietropaoli, D.; Monaco, A. Electromyographic Evaluation during Orthodontic Therapy: Comparison of Two Elastodontic Devices. J. Biol. Regul. Homeost. Agents 2020, 34, 1935–1939. [Google Scholar] [CrossRef] [PubMed]
- Janson, G.; Nakamura, A.; Chiqueto, K.; Castro, R.; de Freitas, M.R.; Henriques, J.F.C. Treatment Stability with the Eruption Guidance Appliance. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 717–728. [Google Scholar] [CrossRef]
- Farronato, G.; Giannini, L.; Galbiati, G.; Grillo, E.; Maspero, C. Occlus-o-Guide® versus Andresen Activator Appliance: Neuromuscular Evaluation. Prog. Orthod. 2013, 14, 4. [Google Scholar] [CrossRef][Green Version]
- Fichera, G.; Martina, S.; Palazzo, G.; Musumeci, R.; Leonardi, R.; Isola, G.; Lo Giudice, A. New Materials for Orthodontic Interceptive Treatment in Primary to Late Mixed Dentition. A Retrosp. Study Using Elastodontic Devices. Materials 2021, 14, 1695. [Google Scholar] [CrossRef]
- Fleming, P.S. Timing Orthodontic Treatment: Early or Late? Aust. Dent. J. 2017, 62 (Suppl. S1), 11–19. [Google Scholar] [CrossRef] [PubMed]
- Ortu, E.; Di Nicolantonio, S.; Severino, M.; Cova, S.; Pietropaoli, D.; Monaco, A. Effectiveness of Elastodontic Appliances in the Treatment of Malocclusions: A Review of the Literature. Eur. J. Paediatr. Dent. 2024, 25, 1. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Hagg, U.; McGrath, C. Elastodontic Appliance Assisted Fixed Appliance Treatment: A New Two-Phase Protocol for Extraction Cases. J. Orthod. 2019, 46, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Grisar, K.; Luyten, J.; Preda, F.; Martin, C.; Hoppenreijs, T.; Politis, C.; Jacobs, R. Interventions for Impacted Maxillary Canines: A Systematic Review of the Relationship between Initial Canine Position and Treatment Outcome. Orthod. Craniofac Res. 2021, 24, 180–193. [Google Scholar] [CrossRef] [PubMed]
- Dianiskova, S.; Bucci, R.; Solazzo, L.; Rongo, R.; Caruso, S.; Caruso, S.; Gatto, R.; Fiasca, F.; Valletta, R.; D’Antò, V. Patient and Parental Satisfaction Following Orthodontic Treatment with Clear Aligners and Elastodontic Appliances during Mixed Dentition: A Cross-Sectional Case–Control Study. Appl. Sci. 2023, 13, 4074. [Google Scholar] [CrossRef]
- Di Spirito, F.; Amato, A.; Di Palo, M.P.; Ferraro, G.A.; Baroni, A.; Serpico, R.; Contaldo, M. COVID-19 Related Information on Pediatric Dental Care Including the Use of Teledentistry: A Narrative Review. Children 2022, 9, 1942. [Google Scholar] [CrossRef]
- d’Apuzzo, F.; Perillo, L.; Carrico, C.K.; Castroflorio, T.; Grassia, V.; Lindauer, S.J.; Shroff, B. Clear Aligner Treatment: Different Perspectives between Orthodontists and General Dentists. Prog. Orthod. 2019, 20, 10. [Google Scholar] [CrossRef]
- Cannatà, D.; Giordano, F.; Bartolucci, M.L.; Galdi, M.; Bucci, R.; Martina, S. Attitude of Italian Dental Practitioners toward Bruxism Assessment and Management: A Survey-Based Study. Orthod. Craniofac Res. 2024, 27, 228–236. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Montenegro, V.; Laudadio, C.; Pede, C.D.; et al. The Efficacy of a New AMCOP® Elastodontic Protocol for Orthodontic Interceptive Treatment: A Case Series and Literature Overview. Int. J. Environ. Res. Public Health 2022, 19, 988. [Google Scholar] [CrossRef]
- Arenholt-Bindslev, D.; Hörsted-Bindslev, P.; Philipsen, H.P. Toxic Effects of Two Dental Materials on Human Buccal Epithelium in Vitro and Monkey Buccal Mucosa in Vivo. Scand. J. Dent. Res. 1987, 95, 467–474. [Google Scholar] [CrossRef]
- Condò, R.; Costacurta, M.; Perugia, C.; Docimo, R. Atypical Deglutition: Diagnosis and Interceptive Treatment. A Clin. Study. Eur. J. Paediatr. Dent. 2012, 13, 209–214. [Google Scholar]
- Keski-Nisula, K.; Hernesniemi, R.; Heiskanen, M.; Keski-Nisula, L.; Varrela, J. Orthodontic Intervention in the Early Mixed Dentition: A Prospective, Controlled Study on the Effects of the Eruption Guidance Appliance. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 254–260, quiz 328.e2. [Google Scholar] [CrossRef]
- Ortu, E.; Pietropaoli, D.; Cova, S.; Marci, M.C.; Monaco, A. Efficacy of Elastodontic Devices in Overjet and Overbite Reduction Assessed by Computer-Aid Evaluation. BMC Oral Health 2021, 21, 269. [Google Scholar] [CrossRef]
- Condò, R.; Perugia, C.; Bartolino, M.; Docimo, R. Analysis of Clinical Efficacy of Interceptive Treatment of Class II Division 2 Malocclusion in a Pair of Twins through the Use of Two Modified Removable Appliances. Oral Implant. 2010, 3, 11–25. [Google Scholar]
- Janson, G.; de Souza, J.E.P.; de Freitas, M.R.; Henriques, J.F.C.; Cavalcanti, C.T. Occlusal Changes of Class II Malocclusion Treatment between Fränkel and the Eruption Guidance Appliances. Angle Orthod. 2004, 74, 521–525. [Google Scholar] [PubMed]
- Keski-Nisula, K.; Keski-Nisula, L.; Varrela, J. Class II Treatment in Early Mixed Dentition with the Eruption Guidance Appliance: Effects and Long-Term Stability. Eur. J. Orthod. 2020, 42, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Migliaccio, S.; Aprile, V.; Zicari, S.; Grenci, A. Eruption Guidance Appliance: A Review. Eur. J. Paediatr. Dent. 2014, 15, 163–166. [Google Scholar] [PubMed]
- Di Spirito, F.; D’Ambrosio, F.; Cannatà, D.; D’Antò, V.; Giordano, F.; Martina, S. Impact of Clear Aligners versus Fixed Appliances on Periodontal Status of Patients Undergoing Orthodontic Treatment: A Systematic Review of Systematic Reviews. Healthcare 2023, 11, 1340. [Google Scholar] [CrossRef]
- Di Spirito, F.; Amato, A.; Di Palo, M.P.; Cannatà, D.; Giordano, F.; D’Ambrosio, F.; Martina, S. Periodontal Management in Periodontally Healthy Orthodontic Patients with Fixed Appliances: An Umbrella Review of Self-Care Instructions and Evidence-Based Recommendations. Dent. J. 2023, 11, 35. [Google Scholar] [CrossRef]
- D’Ambrosio, F. Periodontal and Peri-Implant Diagnosis: Current Evidence and Future Directions. Diagnostics 2024, 14, 256. [Google Scholar] [CrossRef] [PubMed]
- Arreghini, A.; Trigila, S.; Lombardo, L.; Siciliani, G. Objective Assessment of Compliance with Intra- and Extraoral Removable Appliances. Angle Orthod. 2017, 87, 88–95. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, K.; Wright, J.; Conboy, F.; Sanjie, Y.; Mandall, N.; Chadwick, S.; Connolly, I.; Cook, P.; Birnie, D.; Hammond, M.; et al. Effectiveness of Treatment for Class II Malocclusion with the Herbst or Twin-Block Appliances: A Randomized, Controlled Trial. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Montenegro, V.; Inchingolo, A.D.; Malcangi, G.; Limongelli, L.; Marinelli, G.; Coloccia, G.; Laudadio, C.; Patano, A.; Inchingolo, F.; Bordea, I.R.; et al. Compliance of children with removable functional appliance with microchip integrated during covid-19 pandemic: A systematic review. J. Biol. Regul. Homeost. Agents 2021, 35, 365–377. [Google Scholar] [CrossRef] [PubMed]
| O | GDP | p-Value | |
|---|---|---|---|
| Age (n = 394) | |||
| 24–30 | 15 | 73 | <0.001 |
| 31–40 | 50 | 82 | <0.001 |
| 41–50 | 59 | 7 | <0.001 |
| 50+ | 102 | 6 | <0.001 |
| Gender (n = 394) | |||
| Male | 103 | 73 | 0.675 |
| Female | 123 | 95 | 0.675 |
| Years in dental profession (n = 394) | |||
| 1–5 | 3 | 99 | <0.001 |
| 6–10 | 7 | 55 | <0.001 |
| 11–20 | 78 | 6 | <0.001 |
| 20+ | 138 | 8 | <0.001 |
| Practice type (n = 394) | |||
| Private practice solo | 41 | 131 | <0.001 |
| Private practice team | 42 | 24 | 0.259 |
| Consultant | 114 | 2 | <0.001 |
| University/academic staff | 22 | 3 | 0.066 |
| Hospital staff | 7 | 8 | 0.413 |
| O | GDP | p-Value | |
|---|---|---|---|
| Level of knowledge (n = 398) | |||
| Adequately informed | 191 | 67 | <0.001 |
| Little informed, but interested in learning more | 35 | 43 | 0.013 |
| Little informed, and not interested in learning more | 0 | 22 | <0.001 |
| Never heard | 0 | 36 | <0.001 |
| Source of learning (n = 398) | |||
| Undergraduate education | 4 | 7 | 0.153 |
| Discussions with colleagues | 3 | 22 | <0.001 |
| Postgraduate course/webinar | 173 | 67 | <0.001 |
| Scientific articles/books | 35 | 15 | 0.053 |
| Sales representative or advertising brochures/flyers | 11 | 21 | 0.006 |
| Never heard | 0 | 36 | <0.001 |
| Use of EAs | |||
| Yes | 203 | 43 | <0.001 |
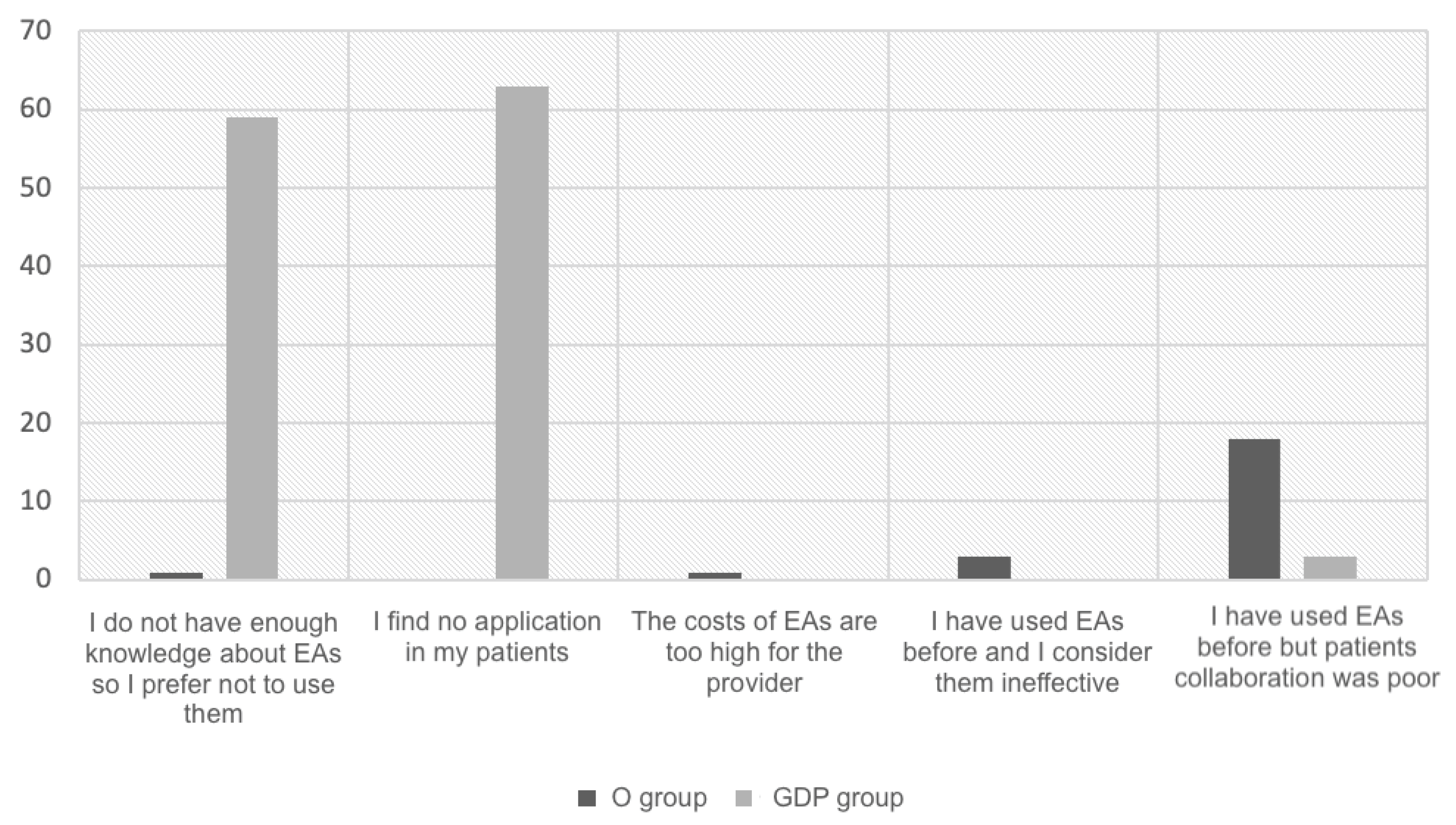
| No | 23 | 125 | <0.001 |
| O | GDP | p-Value | |
|---|---|---|---|
| Years using (n = 246) | |||
| Less than 1 | 9 | 41 | <0.001 |
| 1–5 | 108 | 2 | <0.001 |
| 6–10 | 42 | 0 | 0.001 |
| 10+ | 44 | 0 | <0.001 |
| Number of EA cases started in the last year (n = 246) | |||
| 1–10 | 110 | 39 | <0.001 |
| 11–20 | 66 | 4 | 0.002 |
| 21–30 | 18 | 0 | 0.043 |
| 31–40 | 3 | 0 | 0.423 |
| 41–50 | 3 | 0 | 0.423 |
| 50+ | 3 | 0 | 0.423 |
| Stage of dentition (n = 246) | |||
| Patients in primary dentition | 25 | 1 | 0.053 |
| Patients in early mixed dentition | 113 | 41 | <0.001 |
| Patients in late mixed dentition | 46 | 0 | <0.001 |
| Patients in permanent dentition | 20 | 0 | 0.032 |
| Main problem (n = 246) | |||
| Bad habits | 131 | 43 | <0.001 |
| Deep bite | 157 | 7 | <0.001 |
| Open bite | 164 | 24 | <0.001 |
| Dental or skeletal sagittal Class II | 74 | 0 | <0.001 |
| Dental or skeletal sagittal Class III | 31 | 3 | 0.152 |
| Teeth crowding | 48 | 18 | 0.014 |
| Interincisal diastema | 25 | 1 | 0.053 |
| Posterior cross-bite/scissor bite | 28 | 4 | 0.426 |
| Crowding (n = 246) | |||
| Mild dental crowding (1–3 mm) | 181 | 35 | 0.157 |
| Dental crowding from mild to moderate (4–6 mm) | 14 | 0 | 0.076 |
| Dental crowding from moderate to severe (7+ mm) | 8 | 0 | 0.186 |
| No use of EAs to correct dental crowding | 0 | 8 | <0.001 |
| OVJ (n = 246) | |||
| OVJ < 0 mm (anterior cross-bite) | 120 | 18 | 0.038 |
| OVJ = 4–6 mm | 184 | 16 | <0.001 |
| OVJ = 6–8 mm | 57 | 1 | <0.001 |
| OVJ > 8 mm | 11 | 3 | 0.689 |
| No use of EAs to correct OVJ | 0 | 20 | <0.001 |
| OVB (n = 246) | |||
| OVB < 0 mm (open bite) | 134 | 16 | <0.001 |
| OVB = 4–6 mm | 192 | 22 | <0.001 |
| OVB = 6–8 mm | 99 | 1 | <0.001 |
| OVB > 8 mm | 48 | 4 | 0.036 |
| No use of EAs to correct OVB | 0 | 10 | <0.001 |
| Combination (n = 246) | |||
| EAs together with other orthodontic appliances | 62 | 0 | <0.001 |
| EAs alone | 141 | 43 | <0.001 |
| O | GDP | p-Value | |
|---|---|---|---|
| Adverse effects (n = 246) | |||
| None | 64 | 40 | <0.001 |
| Headache | 15 | 1 | 0.221 |
| Toothache | 70 | 0 | <0.001 |
| Muscle pain | 32 | 0 | 0.005 |
| TMJ pain | 6 | 0 | 0.254 |
| Other | 16 | 2 | 0.460 |
| Appointment duration (n = 246) | |||
| Longer | 0 | 4 | <0.001 |
| Shorter | 179 | 19 | <0.001 |
| No difference | 24 | 20 | <0.001 |
| Overall treatment duration (n = 246) | |||
| Longer | 94 | 12 | 0.027 |
| Shorter | 40 | 0 | 0.001 |
| No difference | 69 | 31 | <0.001 |
| Compliance (n = 246) | |||
| Increased | 54 | 0 | <0.001 |
| Decreased | 66 | 2 | <0.001 |
| No difference | 83 | 41 | <0.001 |
| Oral hygiene (n = 246) | |||
| Increased | 28 | 15 | <0.001 |
| Decreased | 19 | 4 | 0.991 |
| No difference | 156 | 24 | 0.005 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cannatà, D.; Galdi, M.; Martina, S.; Rongo, R.; D’Antò, V.; Valletta, R.; Bucci, R. Preformed Elastodontic Appliances: Awareness and Attitude of Orthodontists and General Dental Practitioners. Children 2024, 11, 418. https://doi.org/10.3390/children11040418
Cannatà D, Galdi M, Martina S, Rongo R, D’Antò V, Valletta R, Bucci R. Preformed Elastodontic Appliances: Awareness and Attitude of Orthodontists and General Dental Practitioners. Children. 2024; 11(4):418. https://doi.org/10.3390/children11040418
Chicago/Turabian StyleCannatà, Davide, Marzio Galdi, Stefano Martina, Roberto Rongo, Vincenzo D’Antò, Rosa Valletta, and Rosaria Bucci. 2024. "Preformed Elastodontic Appliances: Awareness and Attitude of Orthodontists and General Dental Practitioners" Children 11, no. 4: 418. https://doi.org/10.3390/children11040418
APA StyleCannatà, D., Galdi, M., Martina, S., Rongo, R., D’Antò, V., Valletta, R., & Bucci, R. (2024). Preformed Elastodontic Appliances: Awareness and Attitude of Orthodontists and General Dental Practitioners. Children, 11(4), 418. https://doi.org/10.3390/children11040418










