1. Introduction
Newborns are born able to speak, but oral language requires auditory experience to emerge. The lack of auditory stimulation, resulting from hearing loss, leads to a weakening of the synapses that should occur for the proper development of speech. Thus, the normal development of oral language requires, among other factors, an intact auditory system. Congenital hearing loss affects 2–4 neonates among 1000 live births in the rooming-in ward [
1]. Early detection and intervention programs for hearing loss have a positive impact on the auditory development of infants with congenital hearing loss, and neonatal hearing screening (NHS) is the first step in identifying hearing loss as soon as possible [
2]. The capture of otoacoustic emissions (OAEs) has been used in NHS programs mainly because it is a fast, objective, and effective method of differentiating children with hearing thresholds within normal limits from those with a degree of hearing loss [
3].
It is recommended that NHS of newborns who do not present risk indicators for hearing loss be performed using OAEs before hospital discharge; in cases of failure (that is, in the absence of otoacoustic emissions), it is necessary to perform a retest of the newborn within 15 days. If there is again a failure to capture emissions, the newborn is referred for audiological diagnosis using Brainstem Auditory Evoked Potentials (BAEPs) and other procedures.
Transient evoked otoacoustic emissions (TEOAEs) are sounds of specific frequencies generated by the cochlea in response to a repeated train of clicks; the responses are manifested as a complex sound wave. The presence of strong OAEs generally indicates healthy outer hair cells (OHC), although their absence does not necessarily mean defects in the inner ear since OHCs also depend on the integrity of the outer and middle ear. There are reports of limitations to current TEOAE procedures and there is still room for optimization [
4].
The pressure in the middle ear (ME) of the newborn may be different from the pressure in the outer ear due, for example, to the immaturity of the Eustachian tube or the presence of embryonic connective tissue, mesenchyme, or other materials [
5]. Since the middle ear is important for transmitting the stimulus to the cochlea, as well as for capturing the OAEs returning through the middle ear to the external acoustic meatus (EAM), a dysfunction in this pathway, including tension of the tympanic membrane caused by pressure, can attenuate the signal and prevent TEOAEs from being captured. Thus, the proper functioning of all the middle ear structures is essential for correct stimulation and measurement of OAEs [
5].
Using wideband tympanometry (WBT), it is possible to make several measurements of the auditory system, including its wideband absorbance (WBA). Studies have shown that, compared to 1 kHz tympanometry, WBT is more accurate in detecting newborns with anomalies in sound conduction [
6,
7]. Keefe et al. [
8] have shown that WBT responses allow for improved analysis of OAEs when middle ear dysfunction is present, and its use in NHS can improve subsequent diagnosis of hearing loss.
It is now possible to perform OAE and WBT measurements using the same equipment and, at the same time, equalize the pressure between the EAM and the middle ear, allowing OAEs to be captured at the maximum middle ear compliance. Given the documented negative impact of middle ear alterations on the detection of OAEs and the high prevalence of altered middle ear pressure in newborns, it appears to be important to consider compensating for middle ear pressure when measuring OAEs. Pressure compensation can result in increased detection of TEOAEs, which makes it possible to confirm the normal functioning of outer hair cells in a greater number of cases than when there is deviant middle ear pressure. This is important for NHS where the absence of TEOAEs can mean a delay in providing information about the child’s hearing to the family; in addition, a greater number of retests in hearing screening leads to a delay in detecting real cases of hearing loss.
This study investigates the use of pressurized OAEs in NHS. The aim is to test the effectiveness of pressurizing otoacoustic emissions in improving the results of screening, thereby reducing the number of return visits needed.
4. Discussion
Comparing WBA under the AP and PP conditions, it was found that, in G1 (the group of newborns who passed both tests), there was a statistically significant difference at the lowest frequency of 1000 Hz. At this frequency, the lowest WBA values were obtained under the AP condition. Hunter et al. [
9] stated that immature absorbance patterns were more apparent at low frequencies from birth to one month of age—as with the newborns evaluated in this study—and changed substantially to a more mature pattern at 6 months of age.
Regarding TEOAEs, in G1, there was a statistically significant difference only in the 1.94 kHz band, with a lower TEOAE S/N value under the AP condition.
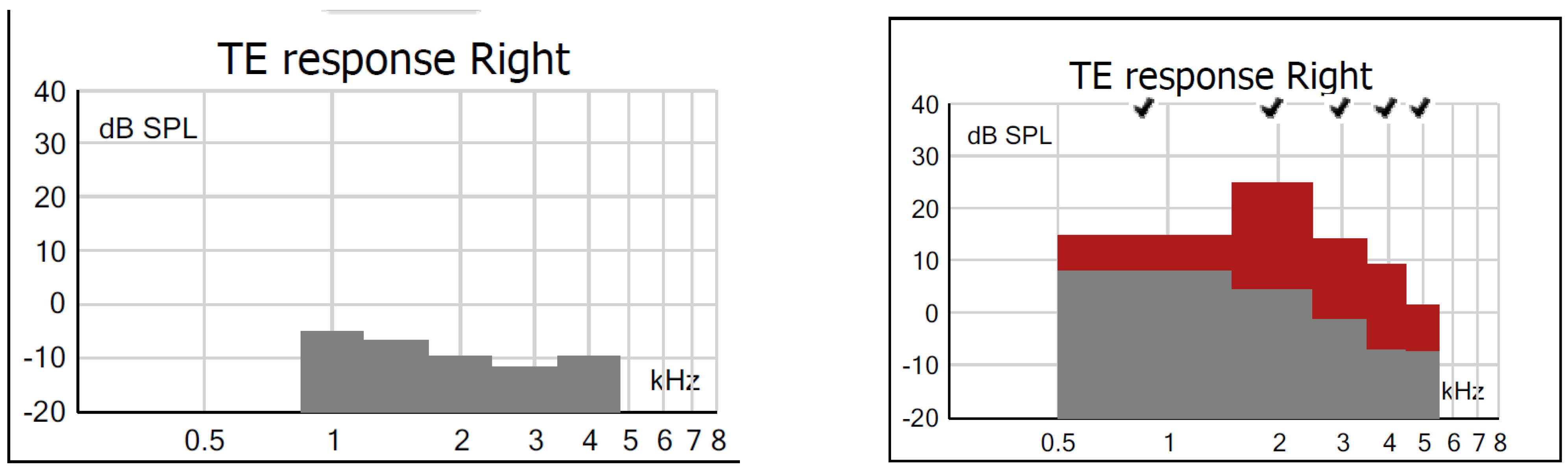
Figure 11 shows an example in which one can observe that, under both test conditions of ambient pressure and peak pressure, the subject presented a PASS result.
For low frequencies, the difference in WBA between AP and PP did not influence the TEOAE result since these were mostly captured in higher frequency bands (1.94, 2.96, 3.97, and 4.97 kHz) where there were no significant differences in WBA. For TEOAE S/N values, the absence of statistical differences between the AP and PP conditions for most frequencies can be explained by the fact that this is a homogeneous group with PASS results under both conditions. Although pressurization had a positive influence on TEOAE amplitudes at 1.94 kHz, the difference had no effect on the result, indicating that for this group of newborns, pressurization was not required. Thus, newborns who pass screening without the need for pressurization can, in the absence of risk indicators, be discharged since the standard WBT and OAE procedures are adequate to detect a normal middle and inner ear function.
However, for G2, the group of newborns who failed the AP stage and passed the PP stage, the difference in WBA was statistically significant for 2, 3, and 6 kHz, with the lowest WBA values found under the AP condition. Hunter et al. [
13] also found that newborns who do not pass OAE screening at birth also have lower absorbance for 1 to 3 kHz, suggesting that such screening failures are frequently associated with middle ear problems at birth.
For TEOAEs measured in G2, the differences were statistically significant in all bands, with lower values under the AP condition and higher under PP, showing that lower WBA values improve the capture of TEOAEs.
Figure 12 shows that in a newborn from G2, there is a difference between the amplitudes of TEOAEs at AP and PP, and this is representative of newborns who passed under the AP condition and failed under the PP condition.
In studies by Marshall et al. [
14], pressurization favored the lower frequency bands (<2 kHz), and the study by Zimatore et al. [
15] found differences at all frequencies, with a maximum difference at 4.97 kHz. In our study, however, the highest values were found in the bands beyond 2 kHz (1.94 and 2.96 kHz); however, it should not be forgotten that there are many differences in the application of methods between the studies cited and the current study, which may explain the discrepancy in the results, such as the sample size and age of assessment of newborns.
Changes in energy reflectance and, consequently, in absorbance in normal ears of newborns up to 1 month of age appear approximately in the range of 2 to 5 kHz but are not present at other frequencies [
16]. Likewise, Hunter et al. [
9] found that newborns in healthy nurseries who failed NHS had significantly lower energy absorbance in the region of 1 to 4 kHz compared with newborns who passed neonatal screening.
The findings of our study indicate that pressurization of the EAM is able to increase the S/N ratios of TEOAEs in all frequency bands tested. This means that many of these subjects were in the FAIL group under the AP condition but, after testing under the PP condition, were part of the PASS group. Such findings demonstrate the effectiveness of pressurization in a number of newborns who initially failed screening. Pressurization adjusts the EAM pressure so as to cancel the pressure difference between the EAM and the middle ear, reducing the rigidity of the system—tympanic membrane and ossicles—and making it possible to capture OAEs.
A major factor contributing to the cost of NHS programs is the high rate of false positives, that is, newborns screened with a failed result that was not confirmed in a retest. Studies have shown that this high rate is due to the inability of current screening methods to distinguish between minor conductive disorders and inner ear disorders, such as sensorineural hearing loss [
6,
17].
In newborns, the incidence of conductive disorders is approximately 30 times higher than that of inner ear disease [
18]. This is because, at birth, the external ear cavity may be obstructed with vernix and the middle ear may be filled with materials such as amniotic fluid, meconium, and epithelial cells. In addition, aeration of the middle ear usually occurs only 48 h after birth [
12], meaning that NHS, which is normally performed before the newborn is 2 days old, can be affected by middle ear changes.
According to the NHS flowchart from the JCIH [
2], newborns in the NICU might need an automated brainstem auditory evoked response (BAER) test if they fail the OAE test. BAER is a hearing screening exam that aims to evaluate the auditory system as a whole and can show the existence of auditory neuropathy. For newborns in rooming-in where the incidence of auditory neuropathy is very low, it is recommended that NHS be performed by capturing OAE and that, in cases of failure, a reassessment be performed using BAER. This is because BAER is much less affected by middle ear changes than OAEs [
19].
However, performing BAER requires greater technical knowledge and skill from the speech-language pathologist when dealing with newborns since it is a test that is much more sensitive to external factors than OAEs. It also requires more time to prepare the newborn and more expense to acquire the necessary material, which, in a public service facility, can be a drawback. For these reasons, in many hospitals, the use of BAER is not feasible, which means that newborns who fail OAE screening are discharged without a second evaluation being performed and have to return for a retest. A false-positive result requiring a retest can generate concern and anxiety in parents and caregivers, in addition to costs resulting from missing a day of work and travel, which can often result in some newborns not having a follow-up if they do not return for reassessment.
Furthermore, it is known that the hearing threshold detected by the BAER technique is slightly higher (40 to 45 dB HL) compared with the TEOAE technique (30 or 35 dB HL) [
2]. Thus, in cases of OAE failure, the use of BAER for NHS might mean that hearing loss of around 30 to 45 dB can sometimes be missed.
In our study, the improvement in TEOAE S/N values with the use of pressurization in G2 meant that around 38% of newborns (ears) that had previously failed TEOAE under AP conditions presented a PASS result in PP without the need to perform a new procedure, such as ABR, or return for retesting. We, therefore, suggest replacing ABR with OAE pressurization as the preferred method to reassess newborns who fail the initial screening. This helps avoid failing to detect newborns with hearing thresholds between 30 and 45 dB and reduces the rate of returns for retesting. The reduction in the number of retests also speeds up hearing diagnosis generally since the professional can now focus their efforts on newborns who actually failed, which also helps to reduce the overall cost of NHS programs.
Finally, in G3—the group of newborns who failed both stages, both in WBA and TEOAE—there was no statistically significant difference for any frequency tested. The absence of a statistical difference confirms that such newborns will remain in the FAIL group even after PP testing. In
Figure 13, for example, it is evident that a subject in G3 presented a FAIL result for TEOAE under both conditions.
Investigations have found that a pressure difference between the middle ear cavity and the EAM attenuates sound transmission through the middle ear and that, for monitoring TEOAE, the pressure in the middle ear should be close to ambient pressure or should be compensated by an equivalent pressure in the EAM [
13,
18].
Zebian et al. [
5] investigated OAEs in cases of alterations in the middle ear and concluded that, with an intact tympanic membrane, it is possible to apply counterpressure to the EAM and improve the admittance of the system.
Hof et al. [
18] evaluated 59 children using two OAE measurements, the first at ambient pressure and the second with compensated ME pressure, and reported that the TEOAE response increased by approximately 2 dB under the latter condition. They concluded that equalizing the pressure in the ME by changing the pressure in the EAM can increase the amplitude of TEOAEs, which is especially beneficial for children with negative middle ear pressure.
Finally, Beck et al. [
20] concluded that the ability to detect the presence of OAEs in a nonideal ME environment provides a significant advance in diagnostic ability as it leads to more appropriate treatment options.
Pressurization was effective in increasing the S/N ratio of TEOAEs in G2, but in G3, we infer that other issues, such as a change in the middle ear due to the presence of fluid, affected the capture of TEOAEs, which are not influenced by pressurization. For these newborns, referral for retesting is necessary. In such cases, it is important to inform parents about possible middle ear conditions as well as the possibility that there might be an inner ear defect, noting that the absence of OAEs in both tests is still not definitive, even if absorbance values are low.
In any case, absence of TEOAEs, even with normal absorbance values, can guide the examiner to think more critically regarding the referral of the newborn since normal middle ear conditions and absence of OAEs usually point to an inner ear alteration. Thus, a newborn with these conditions should be referred directly for audiological diagnosis, without going through the retest stage (since a FAIL result in the TEOAE would probably be confirmed). We conclude that, in NHS, it is important to include a test measuring the condition of the middle ear, preferably one evaluating absorbance values.
4.1. Comparison Between Groups
With regard to WBA, a comparison of the results between groups under the AP condition showed there was a statistically significant difference (
p < 0.05) between groups G1 and G2 at frequencies 2, 3, and 4 kHz and between groups G1 and G3 at all frequencies. However, there was no significant difference between groups G2 and G3.
Figure 7 shows that G2 presents intermediate values for all frequencies, with G1 having higher WBA and G3 lower WBA.
Comparing TEOAE S/N values between groups under the AP condition, there was a statistically significant difference (
p < 0.05) between groups G1 and G2 and between groups G1 and G3 in all frequency bands. Under AP conditions, G1 was the only group with a PASS result. In groups G2 and G3, PASS results occurred only in the frequency bands of 3.97 and 4.97 kHz.
Figure 8 shows that, in the same way as with WBA, G2 also presented intermediate values, with G1 having higher values and G3 having lower values.
Turning now to the results obtained at PP, there was a statistically significant difference (
p < 0.05) in WBA between the groups: between groups G1 and G2 at frequencies of 2, 3, and 4 kHz, and between groups G1 and G3 at frequencies of 2, 3, 4, and 6 kHz. This is similar to what was observed at AP, which leads us to conclude that pressurization affected all groups equally (although for groups G2 and G3, only for 2 kHz).
Figure 9 shows that, as at AP, the values of G2 are intermediate, with G2 values less than G1 values and G3 values less than G2 values.
Finally, when comparing TEOAE S/N results between groups under the PP condition, a statistically significant difference (
p < 0.05) was observed between groups G1 and G2 at frequencies of 2, 3, 4, and 6 kHz. Although G2 had TEOAE S/N values elevated by pressurization while obtaining a PASS result, the values were still lower than in G1. Between groups G1 and G3 and between G2 and G3, a statistically significant difference (
p < 0.05) was observed in all frequency bands tested, with lower values in G3 (
Figure 10). This is because, after pressurization of the EAM, the newborns in group G2 (11.9%) who had failed the AP, obtained higher TEOAE values, with only newborns from G3 (19.5%) remaining in the FAIL group. Analyzing the results of absorbance and S/N of TEOAE, we observed that the WBA values at AP increased after pressurization (PP) in all groups and at most frequencies, which shows us that pressurization was able to increase absorbance in all ears. The increase in WBA from one condition to the other (AP and PP) can be seen in the S/N values of TEOAE, which also increased after pressurization in all groups but with a greater increase in G2, which also presented higher levels of increase in WBA values.
In addition, we noted that G2 (FAIL/PASS) presented intermediate values between the other two groups, with G1 (PASS/PASS) always having higher values and G3 (FAIL/FAIL) having lower values, both for WBA and S/N ratios of TEOAE. This fact leads us to believe that the newborns in G2, having presented lower WBA values than G1 at AP, presented a failure result in the TEOAE under this testing condition; on the other hand, the WBA values in G2 were not as low as in G3 since, after pressurization, their WBA values increased, which led to a PASS result under the PP condition. This did not happen with G3: although their WBA values also increased after pressurization, these values were so low at AP that the pressurization was not sufficient to cause the newborns to present a PASS result at PP.
This leads us to confirm that the middle ear changes presented by the ears in G3 should be related to other issues that went beyond a pressure change, as observed in G2. Finally, the increase in WBA values in G1 also resulted in an increase in TEOAE S/N values; however, this was already a group with high AP values, presenting a PASS result since the first test.
Studies on the application of OAE at peak pressure in newborns are scarce, with the exception of the study by Beck et al. [
20], which deals with the application of DPOAE, and the study by Zimatore et al. [
15], which evaluated TEOAE in 294 newborn ears, using the same parameters as the current study. However, Zimatore et al. did not find any FAIL results, except for reasons of high noise due to the movement of the newborns, and concluded that pressurizing TEOAE generates responses with relatively higher S/N ratios in the range of 0.87 to 4.97 kHz. In the same way as our data, they confirmed that pressurization was effective in increasing TEOAE S/N values in newborns with altered ME pressure, allowing them to be included in the PASS group after pressurization.
4.2. Final Considerations
In our study, we found that WBT was effective in identifying conductive alterations in newborns, and when used in conjunction with pressurization of the EAM, the technique can be useful for improving the capture rates of TEOAE. Therefore, in cases where there is a failure in an OAE result, together with a decrease in absorbance, it is suggested that the conditions of the middle ear be analyzed using WBT, and TEOAE recaptured under the PP condition. Such a testing method can eliminate the need to return for a retest. A reduction in retest rates will help to reduce anxiety in parents and avoid not having a follow-up for newborns who do not return for reevaluation.
We therefore suggest the following:
- -
Introducing WBT measurements in NHS programs whenever possible;
- -
That newborns who fail the initial NHS be reevaluated before discharge by means of pressurized TEOAE;
- -
Newborns who PASS the screening after pressurization should be discharged from the NHS, together with instructions about treating middle ear conditions;
- -
Newborns who continue to fail the screening after pressurization should be evaluated in terms of their middle ear conditions, and if adequate absorbance values are observed, they should be referred directly for audiological diagnosis.
We also emphasize the need for similar studies to be carried out on larger samples in order to improve knowledge about the technology of pressurized TEOAE in newborns.