The Effects of Pediatric Acute Lymphoblastic Leukemia Treatment on Cardiac Repolarization
Abstract
1. Introduction
2. Material and Methods
3. Results
4. Discussions
4.1. HR Changes on Chemotherapy
4.2. PR Interval on Chemotherapy
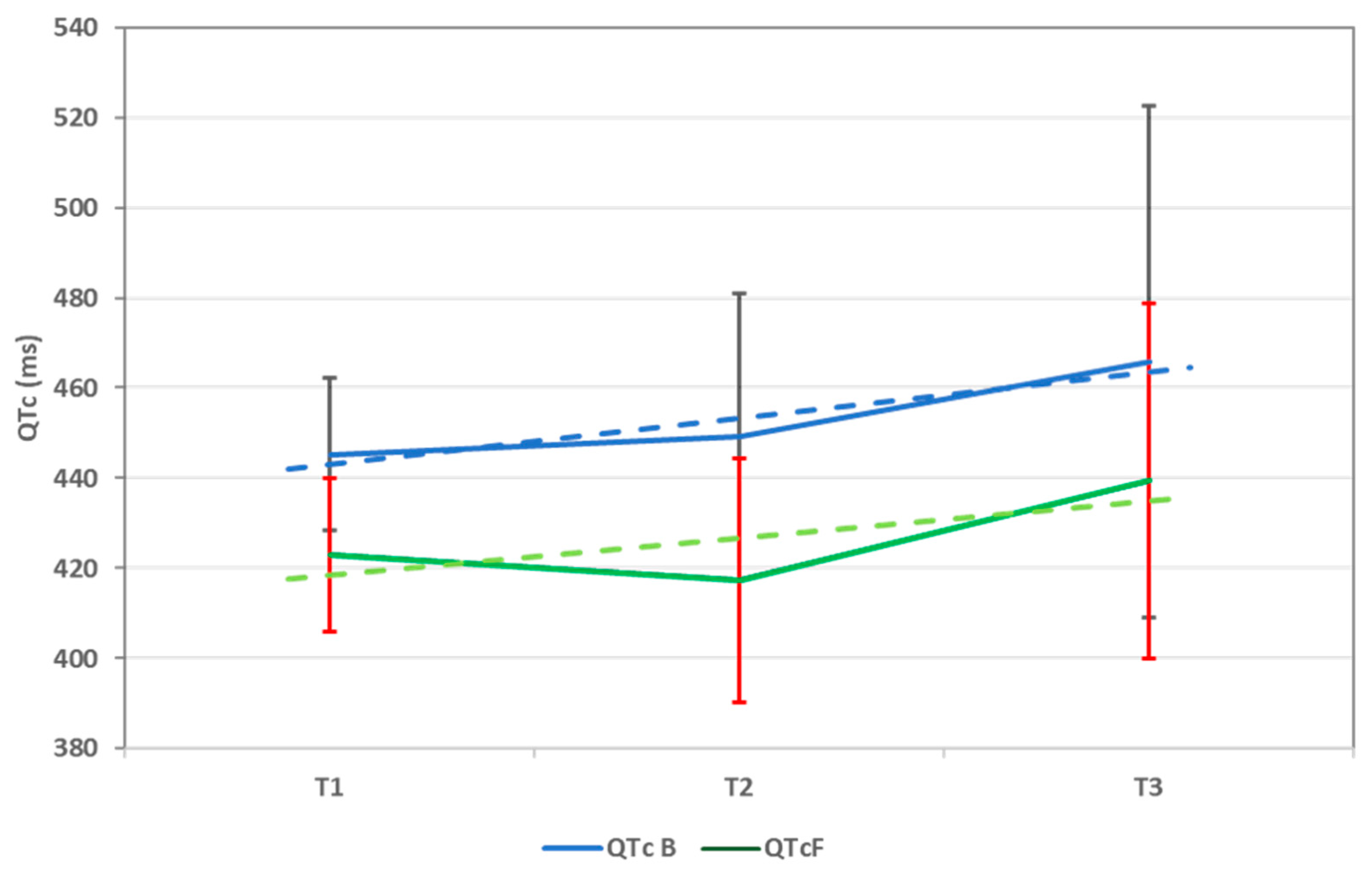
4.3. Repolarization Abnormalities
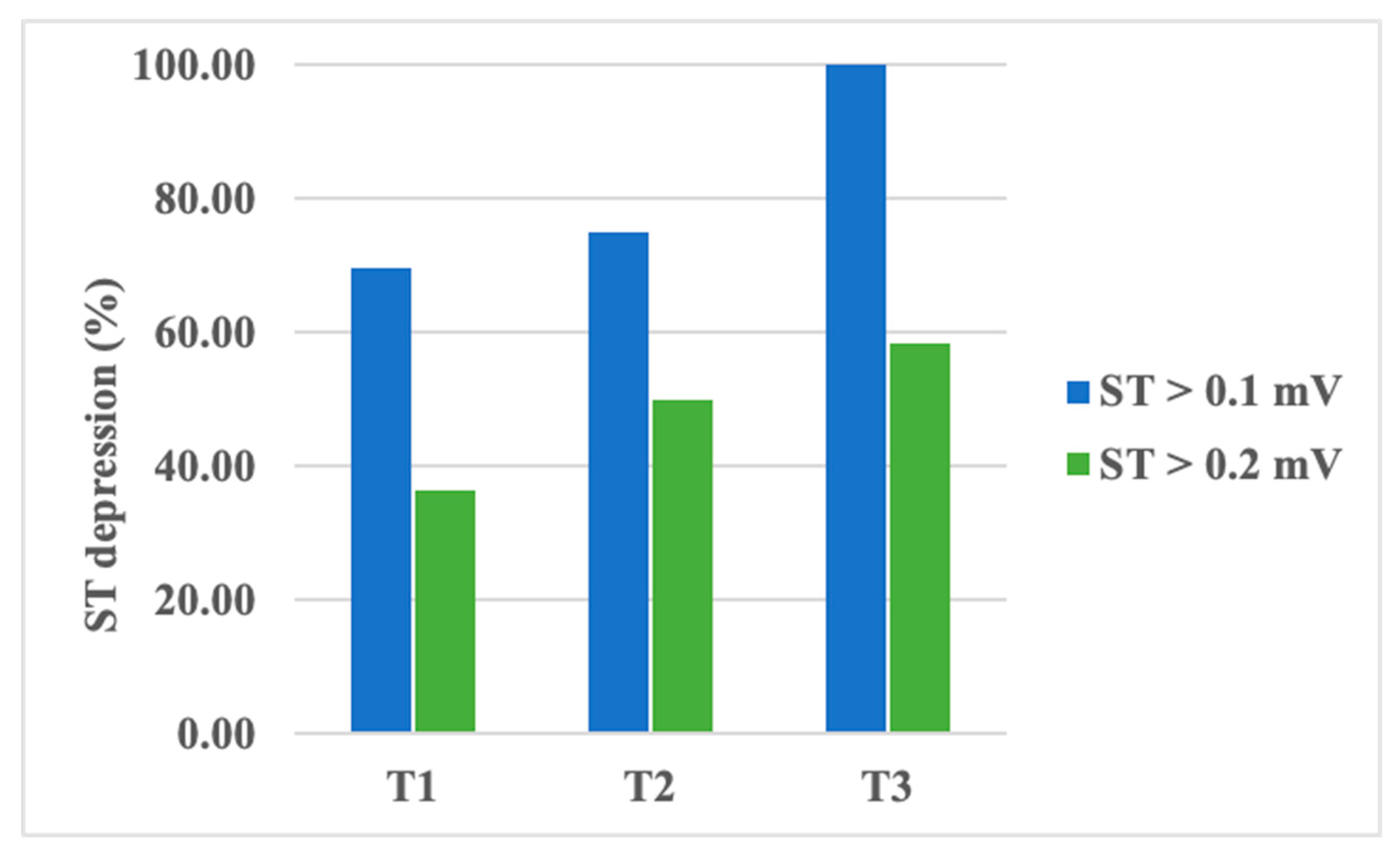
4.4. ST-T Changes on Chemotherapy
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rawat, P.S.; Jaiswal, A.; Khurana, A.; Bhatti, J.S.; Navik, U. Doxorubicin-induced cardiotoxicity: An update on the molecular mechanism and novel therapeutic strategies for effective management. Biomed. Pharmacother. 2021, 139, 111708. [Google Scholar] [CrossRef] [PubMed]
- Lipshultz, S.E.; Colan, S.D.; Gelber, R.D.; Perez-Atayde, A.R.; Sallan, S.E.; Sanders, S.P. Late Cardiac Effects of Doxorubicin Therapy for Acute Lymphoblastic Leukemia in Childhood. N. Engl. J. Med. 1991, 324, 808–815. [Google Scholar] [CrossRef] [PubMed]
- Ward, E.; DeSantis, C.; Robbins, A.; Kohler, B.; Jemal, A. Childhood and adolescent cancer statistics, 2014. CA Cancer J. Clin. 2014, 64, 83–103. [Google Scholar] [CrossRef] [PubMed]
- Dixon, S.B.; Chen, Y.; Yasui, Y.; Pui, C.-H.; Hunger, S.P.; Silverman, L.B.; Ness, K.K.; Green, D.M.; Howell, R.M.; Leisenring, W.M.; et al. Reduced Morbidity and Mortality in Survivors of Childhood Acute Lymphoblastic Leukemia: A Report from the Childhood Cancer Survivor Study. J. Clin. Oncol. 2020, 38, 3418–3429. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.-W.; Jiang, J.; Huang, S.; Shi, X.-M.; Xu, H.; Xu, J.; Peng, J.-Y.; Zhang, W.; Shi, L.; Zhong, X.-L.; et al. Long-term trends in cancer incidence and mortality among U.S. children and adolescents: A SEER database analysis from 1975 to 2018. Front. Pediatr. 2024, 12, 1357093. [Google Scholar] [CrossRef]
- Mulrooney, D.A.; Yeazel, M.W.; Leisenring, W.M.; Kawashima, T.; Mertens, A.C.; Mitby, P.; Stovall, M.; Donaldson, S.S.; Green, D.M.; Sklar, C.A.; et al. Cardiac outcomes in a cohort of adult survivors of childhood and adolescent cancer: Retrospective analysis of the Childhood Cancer Survivor Study cohort. BMJ 2009, 339, b4606. [Google Scholar] [CrossRef]
- Li, H.; Yang, W.; Yu, Z.; Peng, Y.; Huang, M.; Long, L.; Lu, A.; Tan, L.; Deng, M.; Qu, H.; et al. Risk of Arrhythmia with Exposure to Anthracyclines: A Systematic Review, Meta-Analysis, and Network Meta-Analysis. Res. Sq. 2022; preprint. [Google Scholar] [CrossRef]
- Benjanuwattra, J.; Siri-Angkul, N.; Chattipakorn, S.C.; Chattipakorn, N. Doxorubicin and its proarrhythmic effects: A comprehensive review of the evidence from experimental and clinical studies. Pharmacol. Res. 2020, 151, 104542. [Google Scholar] [CrossRef]
- Caru, M.; Corbin, D.; Périé, D.; Lemay, V.; Delfrate, J.; Drouin, S.; Bertout, L.; Krajinovic, M.; Laverdière, C.; Andelfinger, G.; et al. Doxorubicin treatments induce significant changes on the cardiac autonomic nervous system in childhood acute lymphoblastic leukemia long-term survivors. Clin. Res. Cardiol. 2019, 108, 1000–1008. [Google Scholar] [CrossRef]
- Christoffersen, L.; Gibson, T.M.; Pui, C.; Joshi, V.; Partin, R.E.; Green, D.M.; Lanctot, J.Q.; Howell, C.R.; Mulrooney, D.A.; Armstrong, G.T.; et al. Cardiac autonomic dysfunction in survivors of childhood acute lymphoblastic leukemia: The St. Jude Lifetime Cohort Study. Pediatr. Blood Cancer 2020, 67, e28388. [Google Scholar] [CrossRef]
- Lazar, D.R.; Cainap, S.; Maniu, D.; Blag, C.; Bota, M.; Lazar, F.-L.; Achim, A.; Colceriu, M.C.; Zdrenghea, M. Anthracycline’s Effects on Heart Rate Variability in Children with Acute Lymphoblastic Leukemia: Early Toxicity Signs—Pilot Study. JCM 2023, 12, 7052. [Google Scholar] [CrossRef] [PubMed]
- Dhesi, S.; Chu, M.P.; Blevins, G.; Paterson, I.; Larratt, L.; Oudit, G.Y.; Kim, D.H. Cyclophosphamide-Induced Cardiomyopathy. J. Investig. Med. High. Impact Case Rep. 2013, 1, 2324709613480346. [Google Scholar] [CrossRef] [PubMed]
- Atalay, F.; Gulmez, O.; Ugurlu, A.O. Cardiotoxicity following cyclophosphamide therapy: A case report. J. Med. Case Rep. 2014, 8, 252. [Google Scholar] [CrossRef] [PubMed]
- Morandi, P.; Ruffini, P.A.; Benvenuto, G.M.; La Vecchia, L.; Mezzena, G.; Raimondi, R. Serum cardiac troponin I levels and ECG/Echo monitoring in breast cancer patients undergoing high-dose (7 g/m2) cyclophosphamide. Bone Marrow Transplant. 2001, 28, 277–282. [Google Scholar] [CrossRef]
- Nakamae, H.; Hino, M.; Akahori, M.; Terada, Y.; Yamane, T.; Ohta, K.; Hayashi, T.; Tsumura, K. Predictive value of QT dispersion for acute heart failure after autologous and allogeneic hematopoietic stem cell transplantation. Am. J. Hematol. 2004, 76, 1–7. [Google Scholar] [CrossRef]
- Nakamae, H.; Tsumura, K.; Hino, M.; Hayashi, T.; Tatsumi, N. QT dispersion as a predictor of acute heart failure after high-dose cyclophosphamide. Lancet 2000, 355, 805–806. [Google Scholar] [CrossRef]
- Hegazy, R.A.; Lotfy, W.N. The value of Holter monitoring in the assessment of Pediatric patients. Indian Pacing Electrophysiol. J. 2007, 7, 204–214. [Google Scholar]
- 2022 ESC Guidelines on Cardio-Oncology Developed in Collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS) | European Heart Journal | Oxford Academic. Available online: https://academic.oup.com/eurheartj/article/43/41/4229/6673995?login=false (accessed on 11 September 2024).
- Priori, S.G.; Napolitano, C.; Diehl, L.; Schwartz, P.J. Dispersion of the QT interval. A marker of therapeutic efficacy in the idiopathic long QT syndrome. Circulation 1994, 89, 1681–1689. [Google Scholar] [CrossRef]
- Rijnbeek, P.R.; Witsenburg, M.; Schrama, E.; Hess, J.; Kors, J.A. New normal limits for the paediatric electrocardiogram. Eur. Heart J. 2001, 22, 702–711. [Google Scholar] [CrossRef]
- Bazett, H.C. An Analysis of the Time-Relations of Electrocardiograms. Ann. Noninvasive Electrocardiol. 1997, 2, 177–194. [Google Scholar] [CrossRef]
- Fridericia, L.S. The duration of systole in an electrocardiogram in normal humans and in patients with heart disease. Ann. Noninvasive Electrocardiol. 2003, 8, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Lai, Y.; Zhou, X.; Guo, F.; Jin, X.; Meng, G.; Zhou, L.; Chen, H.; Liu, Z.; Yu, L.; Jiang, H. Non-invasive transcutaneous vagal nerve stimulation improves myocardial performance in doxorubicin-induced cardiotoxicity. Cardiovasc. Res. 2022, 118, 1821–1834. [Google Scholar] [CrossRef] [PubMed]
- Duffy, C.; Hall, L.; Godown, J.; Koyama, T.; Borinstein, S.C. Steroid-induced Bradycardia During Induction Chemotherapy in Children and Young Adults Diagnosed With Acute Lymphoblastic Leukemia and Lymphoblastic Lymphoma. J. Pediatr. Hematol. Oncol. 2019, 41, 537–541. [Google Scholar] [CrossRef] [PubMed]
- Bertrand, É.; Caru, M.; Harvey, A.; Dodin, P.; Jacquemet, V.; Curnier, D. Cardiac electrical abnormalities in childhood acute lymphoblastic leukemia survivors: A systematic review. Cardiooncology 2023, 9, 40. [Google Scholar] [CrossRef] [PubMed]
- Liang, X.; Wang, Y.; Yin, X.; Gong, X.; Pan, S.; Chen, Z.; Geng, X. Electrocardiographic Characteristics of Breast Cancer Patients Treated with Chemotherapy. Cardiol. Res. Pract. 2020, 2020, 6678503. [Google Scholar] [CrossRef]
- Spînu, Ș.; Cismaru, G.; Boarescu, P.-M.; Istratoaie, S.; Negru, A.G.; Lazea, C.; Căinap, S.S.; Iacob, D.; Grosu, A.I.; Saraci, G.; et al. ECG Markers of Cardiovascular Toxicity in Adult and Pediatric Cancer Treatment. Dis. Markers 2021, 2021, 6653971. [Google Scholar] [CrossRef]
- Prestor, V.V.; Rakovec, P.; Kozelj, M.; Jereb, B. Late Cardiac Damage of Anthracycline Therapy for Acute Lymphoblastic Leukemia in Childhood. Pediatr. Hematol. Oncol. 2000, 17, 527–540. [Google Scholar] [CrossRef]
- Electrocardiographic Markers of Sudden Cardiac Death (Including Left Ventricular Hypertrophy)—ScienceDirect. Available online: https://www.sciencedirect.com/science/article/abs/pii/S1877918217300977 (accessed on 4 August 2024).
- Phan, D.Q.; Silka, M.J.; Lan, Y.T.; Chang, R.K. Comparison of formulas for calculation of the corrected QT interval in infants and young children. J. Pediatr. 2015, 166, 960–964.e2. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vandenberk, B.; Vandael, E.; Robyns, T.; Vandenberghe, J.; Garweg, C.; Foulon, V.; Ector, J.; Willems, R. Which QT Correction Formulae to Use for QT Monitoring? J. Am. Heart Assoc. 2016, 5, e003264. [Google Scholar] [CrossRef]
- Tamr Agha, M.K.; Fakhri, G.; Ahmed, M.; El Sedawy, O.; Abi Saleh, B.; Bitar, F.; Arabi, M. QTc interval on 24-hour holter monitor: To trust or not to trust? Ann. Noninvasive Electrocardiol. 2022, 27, e12899. [Google Scholar] [CrossRef]
- De Maria, E.; Curnis, A.; Garyfallidis, P.; Mascioli, G.; Santangelo, L.; Calabrò, R.; Dei Cas, L. QT dispersion on ECG Holter monitoring and risk of ventricular arrhythmias in patients with dilated cardiomyopathy. Heart Int. 2006, 2, 33. [Google Scholar] [CrossRef] [PubMed]
- Arsenos, P.; Gatzoulis, K.A.; Laina, A.; Doundoulakis, I.; Soulaidopoulos, S.; Kordalis, A.; Oikonomou, G.; Triantafyllou, K.; Fragakis, N.; Vasilikos, V. QT interval extracted from 30-minute short resting Holter ECG recordings predicts mortality in heart failure. J. Electrocardiol. 2022, 72, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, Y.; Tanaka, T.; Kido, S. Maximum QTc on Holter electrocardiography in children. Pediatr. Int. 2018, 60, 507–512. [Google Scholar] [CrossRef] [PubMed]
- Desai, L.; Balmert, L.; Reichek, J.; Hauck, A.; Gambetta, K.; Webster, G. Electrocardiograms for cardiomyopathy risk stratification in children with anthracycline exposure. Cardiooncology 2019, 5, 10. [Google Scholar] [CrossRef] [PubMed]
- Markman, T.M.; Ruble, K.; Loeb, D.; Chen, A.; Zhang, Y.; Beasley, G.S.; Thompson, W.R.; Nazarian, S. Electrophysiological effects of anthracyclines in adult survivors of pediatric malignancy. Pediatr. Blood Cancer 2017, 64, e26556. [Google Scholar] [CrossRef]
- Magnano, M.; Gallo, C.; Bocchino, P.P.; Briguglio, M.; Rivetti, A.; Gaita, F.; Anselmino, M. QT prolongation and variability: New ECG signs of atrial potentials dispersion before atrial fibrillation onset. J. Cardiovasc. Med. 2019, 20, 180–185. [Google Scholar] [CrossRef]
- Stankovic, I.; Putnikovic, B.; Janicijevic, A.; Jankovic, M.; Cvjetan, R.; Pavlovic, S.; Kalezic-Radmili, T.; Panic, M.; Milicevic, P.; Ilic, I.; et al. Myocardial mechanical and QTc dispersion for the detection of significant coronary artery disease. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 1015–1022. [Google Scholar] [CrossRef][Green Version]
- de Bruyne, M.C.; Hoes, A.W.; Kors, J.A.; Hofman, A.; van Bemmel, J.H.; Grobbee, D.E. QTc dispersion predicts cardiac mortality in the elderly: The Rotterdam Study. Circulation 1998, 97, 467–472. [Google Scholar] [CrossRef]
- QT Dispersion—An Overview|ScienceDirect Topics. Available online: https://www.sciencedirect.com/topics/medicine-and-dentistry/qt-dispersion# (accessed on 5 August 2024).
- Duan, J.; Tao, J.; Zhai, M.; Li, C.; Zhou, N.; Lv, J.; Wang, L.; Lin, L.; Bai, R. Anticancer drugs-related QTc prolongation, torsade de pointes and sudden death: Current evidence and future research perspectives. Oncotarget 2018, 9, 25738–25749. [Google Scholar] [CrossRef]
- Shabestari, A.A.; Dalirrooyfard, M.; Mazloomzadeh, S. Electrocardiographic Corrected QT (QTc) Dispersion Value as a Predictor for Estimation of Neonatal Mortality in Pre-Term Neonates. Acta Inform. Med. 2019, 27, 158–161. [Google Scholar] [CrossRef]
- Turan, Ö.; Ciftel, M. Investigation of QT Dispersion and T-Peak to T-End/Corrected QT Ratio in Multisystem Inflammatory Syndrome in Children. Cureus 2023, 15, e43086. [Google Scholar] [CrossRef] [PubMed]
- Locati, E.T.; Bagliani, G.; Padeletti, L. Normal Ventricular Repolarization and QT Interval: Ionic Background, Modifiers, and Measurements. Card. Electrophysiol. Clin. 2017, 9, 487–513. [Google Scholar] [CrossRef] [PubMed]
- Bjerregaard, P.; El-Shafei, A.; Kotar, S.L.; Labovitz, A.J. ST Segment Analysis by Holter Monitoring. Ann. Noninvasive Electrocardiol. 2003, 8, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Stone, P.H. ST-Segment Analysis in Ambulatory ECG (AECG or Holter) Monitoring in Patients with Coronary Artery Disease: Clinical Significance and Analytic Techniques. Ann. Noninvasive Electrocardiol. 2005, 10, 263–278. [Google Scholar] [CrossRef] [PubMed]
- Boon, D.; Van Goudoever, J.; Piek, J.J.; Van Montfrans, G.A. ST Segment Depression Criteria and the Prevalence of Silent Cardiac Ischemia in Hypertensives. Hypertension 2003, 41, 476–481. [Google Scholar] [CrossRef][Green Version]
- Ashraf, H.; Sable, C.; Sinha, P.; Jonas, R. ST segment depression after Norwood/systemic-pulmonary artery shunt. J. Saudi Heart Assoc. 2015, 27, 68–69. [Google Scholar]
- Hamed, A.A.; Elguindy, W.; Elhenawy, Y.I.; Ibrahim, R.H. Early Cardiac Involvement and Risk Factors for the Development of Arrhythmia in Patients With b-Thalassemia Major. J. Pediatr. Hematol. Oncol. 2015, 38, 5–11. [Google Scholar] [CrossRef]
- Candaş Kafalı, H.; Ergül, Y. Common Supraventricular and Ventricular Arrhythmias in Children. Turk. Arch. Pediatr. 2022, 57, 476–488. [Google Scholar] [CrossRef]
- Reeve, R.; DeBoer, K. Sinus Arrhythmia: I. Data and Patterns from Groups of Individuals Followed from I Month to 23 Years of Age. Pediatrics 1960, 26, 402–414. [Google Scholar] [CrossRef]

| Characteristics | Mean ± sd | n (%) |
|---|---|---|
| Age (years) | 5.86 ± 3.57 | |
| 1–3 years | 7 (18.92%) | |
| 3–6 years | 16 (43.42%) | |
| 6–10 years | 9 (24.32%) | |
| 10–18 years | 5 (13.51%) | |
| Gender | ||
| male | 19 (51.35%) | |
| female | 18 (48.65%) | |
| Origin | ||
| urban | 17 (45.95%) | |
| rural | 20 (54.05%) | |
| Weight (kg) | 23.71 ± 13.28 | |
| Height (m) | 1.17 ± 0.24 | |
| Relapse risk group | ||
| Standard-risk group | 2 (5.41%) | |
| Medium-risk group | 23 (62.16%) | |
| High-risk group | 12 (32.43%) | |
| ECG Parameters (T0) | |
|---|---|
| HR (bpm) | 101.76 ± 27.24 |
| PR interval (ms) | 118.08 ± 19.26 |
| QTc interval (ms) Bazett | 423.41 ± 36.85 |
| QTc interval (ms) Fridericia | 385.37 ± 30.96 |
| T1 | T2 | T3 | p-Value a | p-Value b | p-Value c | |
|---|---|---|---|---|---|---|
| HR (bpm) | ||||||
| minimum | 53.88 ± 11.87 | 65.5 ± 20.77 | 70.5 ± 21.07 | - | 0.016 | 0.001 |
| average | 86.24 ± 13.57 | 106.5 ± 19.01 | 107.25 ± 27.3 | 0.001 | <0.001 | 0.001 |
| maximum | 160.71 ± 25.27 | 169.83 ± 21.27 | 168.58 ± 28.09 | - | 0.141 | 0.261 |
| Tachycardia (%) | 6.4 ± 10.75 | 20.29 ± 27.59 | 34.74 ± 29.97 | - | 0.022 | 0.005 |
| Bradycardia (%) | 29.91 ± 25.41 | 7.75 ± 15.71 | 14.5 ± 26.52 | - | <0.001 | 0.010 |
| PR interval (ms) | ||||||
| minimum | 87.82 ± 12.21 | 92.08 ± 10.9 | 101.33 ± 17.35 | - | 0.374 | 0.017 |
| average | 122.41 ± 18.57 | 136.67 ± 20.88 | 135 ± 19.76 | 0.084 | 0.008 | 0.049 |
| maximum | 206.65 ± 57.6 | 218.33 ± 58.2 | 207 ± 55.5 | - | 0.281 | 0.822 |
| QT interval (ms) | ||||||
| minimum | 292.85 ± 41.92 | 268.15 ± 46.24 | 292.75 ± 41 | - | 0.235 | 0.582 |
| average | 377.35 ± 30.36 | 347.75 ± 38.58 | 369.25 ± 53.75 | <0.001 | <0.001 | 0.229 |
| maximum | 447.65 ± 43.07 | 446.5 ± 50.12 | 465.83 ± 68.47 | - | 0.772 | 0.847 |
| QTc interval (ms) Bazett | ||||||
| minimum | 376.06 ± 35.78 | 372.54 ± 45.07 | 375.5 ± 75.02 | - | 0.699 | 0.923 |
| average | 445.21 ± 16.89 | 449.21 ± 31.72 | 465.75 ± 56.78 | <0.001 | 0.484 | 0.244 |
| maximum | 568 ± 36.41 | 597.08 ± 43.21 | 593.25 ± 45.65 | - | 0.024 | 0.128 |
| QTc interval (ms) Fridericia | ||||||
| minimum | 281.31 ± 43.48 | 272.35 ± 47.62 | 303.50 ± 43.64 | - | 0.777 | 0.045 |
| average | 422.96 ± 17.08 | 417.31 ± 26.94 | 439.42 ± 39.46 | <0.001 | 0.369 | 0.324 |
| maximum | 618.82 ± 55.65 | 628.58 ± 59.32 | 650.96 ± 72.71 | - | 0.552 | 0.552 |
| Parameters | T1 | T2 | T3 | p-Value i | p-Value ii |
|---|---|---|---|---|---|
| QT d (ms) | 151.94 ± 74.83 | 178.35 ± 57 | 173.08 ± 71.66 | 0.5653 | 0.6646 |
| QTc d (B) (ms) | 191.94 ± 49.53 | 224.54 ± 45.04 | 217.75 ± 92.59 | 0.001 | 0.542 |
| QTc d (F) (ms) | 337.51 ± 87.44 | 356.22 ± 82.31 | 347.46 ± 95.04 | 0.886 | 0.283 |
| relative QTd | 19.15 ± 4.93 | 25.26 ± 9.48 | 22.65 ± 8.27 | 0.025 | 0.432 |
| T1 | T2 | T3 | |
|---|---|---|---|
| ST depression | 0.35 ± 0.58 | 0.36 ± 0.42 | 0.29 ± 0.20 |
| ST segment variability | 1.01 ± 1.07 | 1.01 ± 0.91 | 0.84 ± 0.44 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lazar, D.R.; Cainap, S.; Lazar, F.L.; Maniu, D.; Blag, C.; Bota, M.; Colceriu, M.C.; Zdrenghea, M. The Effects of Pediatric Acute Lymphoblastic Leukemia Treatment on Cardiac Repolarization. Children 2024, 11, 1158. https://doi.org/10.3390/children11101158
Lazar DR, Cainap S, Lazar FL, Maniu D, Blag C, Bota M, Colceriu MC, Zdrenghea M. The Effects of Pediatric Acute Lymphoblastic Leukemia Treatment on Cardiac Repolarization. Children. 2024; 11(10):1158. https://doi.org/10.3390/children11101158
Chicago/Turabian StyleLazar, Diana R., Simona Cainap, Florin Leontin Lazar, Dana Maniu, Cristina Blag, Madalina Bota, Marius C. Colceriu, and Mihnea Zdrenghea. 2024. "The Effects of Pediatric Acute Lymphoblastic Leukemia Treatment on Cardiac Repolarization" Children 11, no. 10: 1158. https://doi.org/10.3390/children11101158
APA StyleLazar, D. R., Cainap, S., Lazar, F. L., Maniu, D., Blag, C., Bota, M., Colceriu, M. C., & Zdrenghea, M. (2024). The Effects of Pediatric Acute Lymphoblastic Leukemia Treatment on Cardiac Repolarization. Children, 11(10), 1158. https://doi.org/10.3390/children11101158






