A New Experimental Design to Examine Cognitive Biases for Gastrointestinal Related Stimuli in Children and Adolescents
Abstract
1. Introduction
2. Materials and Methods
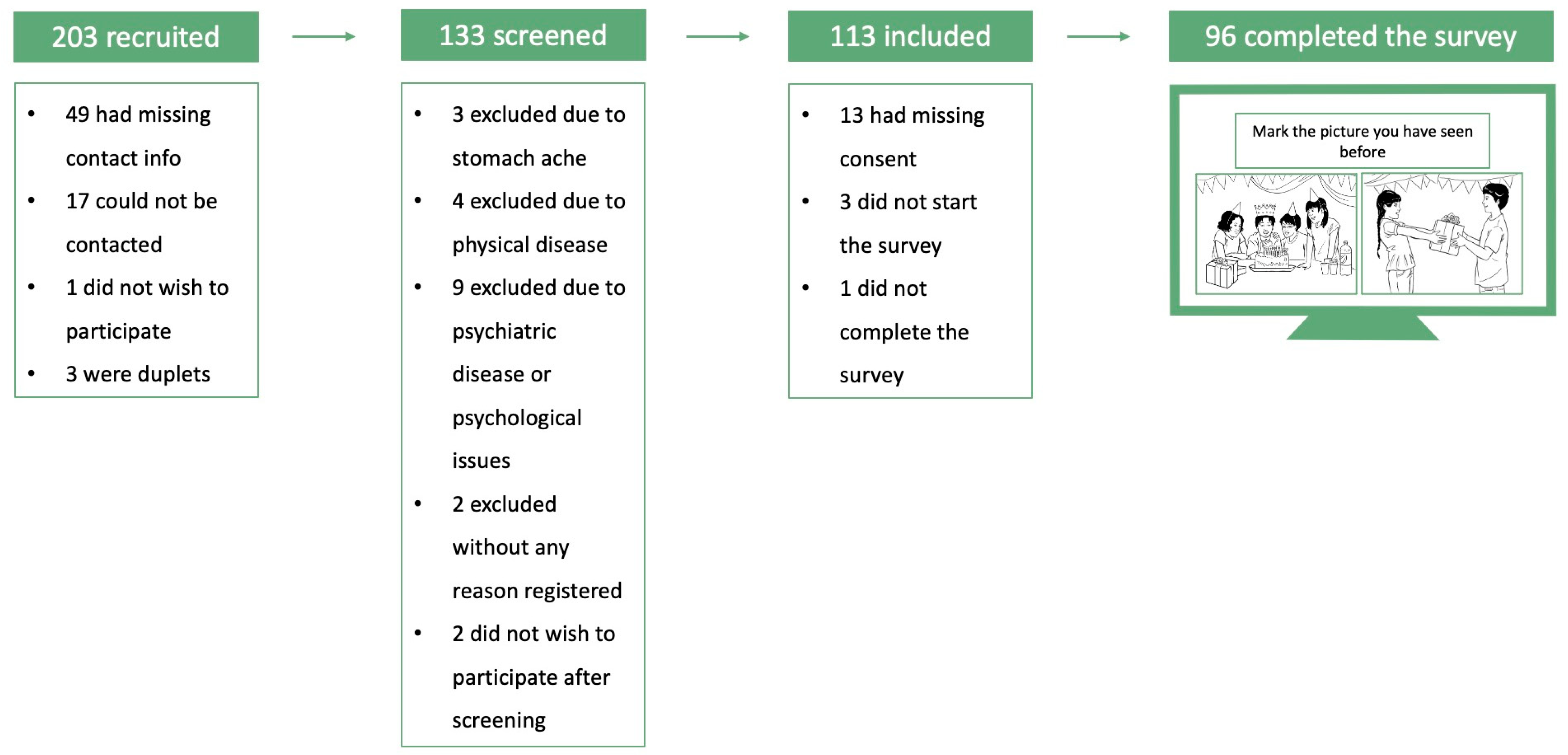
2.1. Study Design and Procedure
2.2. Experimental Design
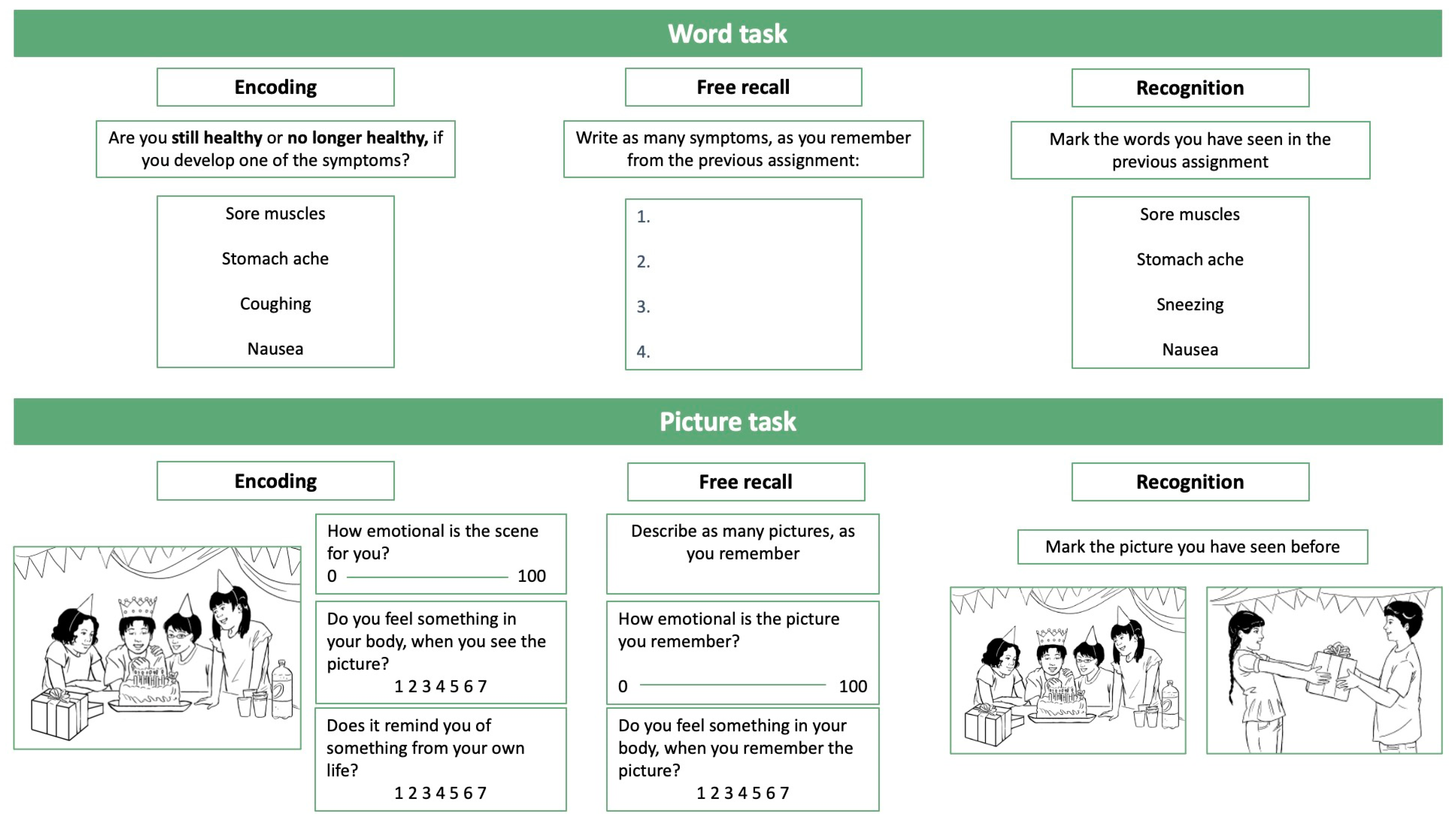
2.2.1. Word Task
- (1)
- general symptoms (e.g., coughing, headache);
- (2)
- gastrointestinal symptoms (e.g., nausea, constipation)
2.2.2. Picture Task
- (1)
- whether it was positive or negative (emotional valence, 0 = negative, 100 = positive);
- (2)
- if they experienced any bodily symptoms or sensations when seeing the picture (physical arousal, 1 = not at all, 7 = a great deal);
- (3)
- if the picture reminded them of something from their own life (self-relevance, 1 = not at all, 7 = a great deal).
2.3. Additional Measures
- (1)
- The Children’s Somatic Symptoms Inventory, formerly known as the Children Somatization Inventory, consists of 24 items assessing nonspecific somatic symptom complaints in children [35]. The questionnaire is rated on a 5-point Likert scale from 0 to 4 (0 = not at all, 4 = A whole lot).
- (2)
- The Childhood Illness Attitudes Scale assesses symptoms of health anxiety in school children [39] and is a modified version of the Illness Attitudes Scales. The Childhood Illness Attitudes Scale has 35 items and is rated on a 3-point Likert scale ranging from 1–3 (1 = none of the time, 3 = a lot of the time), with a higher score indicating a higher level of health anxiety. In the present study, only the “fears” subscale (11 items) was included [40].
- (3)
- The Pediatric Quality of Life Inventory, Gastrointestinal Symptom Scale measures symptoms related to functional gastrointestinal disorders [34]. The scale has nine items rated on a 5-point Likert scale from 0–4 (0 = never a problem, 4 = almost always a problem). Items are reverse-scored; thus, a higher score indicates a better quality of life [34].
2.4. Power Analysis
2.5. Data Analysis
Statistical Analysis
3. Results
3.1. Word Task
3.1.1. Encoding Phase
3.1.2. Free Recall Phase
3.1.3. Recognition Phase
3.2. Picture Task
3.2.1. Encoding Phase
3.2.2. Free Recall Phase
3.2.3. Recognition Phase
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Everaert, J.; Koster, E.H.; Derakshan, N. The combined cognitive bias hypothesis in depression. Clin. Psychol. Rev. 2012, 32, 413–424. [Google Scholar] [CrossRef]
- Brown, R.J. Psychological mechanisms of medically unexplained symptoms: An integrative conceptual model. Psychol. Bull. 2004, 130, 793–812. [Google Scholar] [CrossRef] [PubMed]
- Bar-Haim, Y.; Lamy, D.; Pergamin, L.; Bakermans-Kranenburg, M.J.; van Ijzendoorn, M.H. Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychol. Bull. 2007, 133, 1. [Google Scholar] [CrossRef] [PubMed]
- Burton, C.; Fink, P.; Henningsen, P.; Löwe, B.; Rief, W. Functional somatic disorders: Discussion paper for a new common classification for research and clinical use. BMC Med. 2020, 18, 34. [Google Scholar] [CrossRef]
- Fink, P.; Rosendal, M. Functional Disorders and Medically Unexplained Symptoms: Assessment and Treatment; Fink, P., Rosendal, M., Eds.; Aarhus University Press: Aarhus, Denmark, 2015. [Google Scholar]
- Deary, V.; Chalder, T.; Sharpe, M. The cognitive behavioural model of medically unexplained symptoms: A theoretical and empirical review. Clin. Psychol. Rev. 2007, 27, 781–797. [Google Scholar] [CrossRef]
- MacLeod, C.; Mathews, A.; Tata, P. Attentional bias in emotional disorders. J. Abnorm. Psychol. 1986, 95, 15–20. [Google Scholar] [CrossRef]
- Barsky, A.J.; Coeytaux, R.R.; Sarnie, M.K.; Cleary, P.D. Hypochondriacal patients’ beliefs about good health. Am. J. Psychiatry 1993, 150, 1085–1089. [Google Scholar] [CrossRef]
- Greenwald, A.G.; McGhee, D.E.; Schwartz, J.L.K. Measuring individual differences in implicit cognition: The implicit association test. J. Personal. Soc. Psychol. 1998, 74, 1464–1480. [Google Scholar] [CrossRef]
- Hughes, A.M.; Gordon, R.; Chalder, T.; Hirsch, C.R.; Moss-Morris, R. Maximizing potential impact of experimental research into cognitive processes in health psychology: A systematic approach to material development. Br. J. Health Psychol. 2016, 21, 764–780. [Google Scholar] [CrossRef] [PubMed]
- Phillips, K.; Wright, B.J.; Kent, S. Irritable bowel syndrome and symptom severity: Evidence of negative attention bias, diminished vigour, and autonomic dysregulation. J. Psychosom. Res. 2014, 77, 13–19. [Google Scholar] [CrossRef]
- Witthoft, M.; Mier, D.; Ofer, J.; Muller, T.; Rist, F.; Kirsch, P.; Bailer, J.; Diener, C. Neuronal and behavioral correlates of health anxiety: Results of an illness-related emotional Stroop task. Neuropsychobiology 2013, 67, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Lees, A.; Mogg, K.; Bradley, B.P. Health anxiety, anxiety sensitivity, and attentional biases for pictorial and linguistic health-threat cues. Cogn. Emot. 2005, 19, 453–462. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, C.R.; Clark, D.M.; Mathews, A. Imagery and interpretations in social phobia: Support for the combined cognitive biases hypothesis. Behav. Ther. 2006, 37, 223–236. [Google Scholar] [CrossRef] [PubMed]
- Keynejad, R.C.; Fenby, E.; Pick, S.; Moss-Morris, R.; Hirsch, C.; Chalder, T.; Hughes, A.M.; Nicholson, T.R. Attentional Processing and Interpretative Bias in Functional Neurological Disorder. Psychosom. Med. 2020, 82, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Lam, N.C.; Yeung, H.Y.; Li, W.K.; Lo, H.Y.; Yuen, C.F.; Chang, R.C.; Ho, Y.S. Cognitive impairment in Irritable Bowel Syndrome (IBS): A systematic review. Brain Res. 2019, 1719, 274–284. [Google Scholar] [CrossRef]
- Tkalcic, M.; Domijan, D.; Pletikosic, S.; Setic, M.; Hauser, G. Attentional biases in irritable bowel syndrome patients. Clin. Res. Hepatol. Gastroenterol. 2014, 38, 621–628. [Google Scholar] [CrossRef]
- Vernon-Roberts, A.; Alexander, I.; Day, A.S. Systematic Review of Pediatric Functional Gastrointestinal Disorders (Rome IV Criteria). J. Clin. Med. 2021, 10, 5087. [Google Scholar] [CrossRef]
- Cordeiro Santos, M.L.; da Silva Júnior, R.T.; de Brito, B.B.; França da Silva, F.A.; Santos Marques, H.; Lima de Souza Gonçalves, V.; Costa Dos Santos, T.; Ladeia Cirne, C.; Silva, N.O.E.; Oliveira, M.V.; et al. Non-pharmacological management of pediatric functional abdominal pain disorders: Current evidence and future perspectives. World J. Clin. Pediatr. 2022, 11, 105–119. [Google Scholar] [CrossRef]
- Abbott, R.A.; Martin, A.E.; Newlove-Delgado, T.V.; Bethel, A.; Whear, R.S.; Thompson Coon, J.; Logan, S. Recurrent Abdominal Pain in Children: Summary Evidence From 3 Systematic Reviews of Treatment Effectiveness. J. Pediatr. Gastroenterol. Nutr. 2018, 67, 23–33. [Google Scholar] [CrossRef]
- Bonvanie, I.J.; Kallesøe, K.H.; Janssens, K.A.M.; Schröder, A.; Rosmalen, J.G.M.; Rask, C.U. Psychological Interventions for Children with Functional Somatic Symptoms: A Systematic Review and Meta-Analysis. J. Pediatr. 2017, 187, 272–281.e17. [Google Scholar] [CrossRef]
- Boyer, M.C.; Compas, B.E.; Stanger, C.; Colletti, R.B.; Konik, B.S.; Morrow, S.B.; Thomsen, A.H. Attentional Biases to Pain and Social Threat in Children with Recurrent Abdominal Pain. J. Pediatr. Psychol. 2005, 31, 209–220. [Google Scholar] [CrossRef][Green Version]
- Beck, J.E.; Lipani, T.A.; Baber, K.F.; Dufton, L.; Garber, J.; Smith, C.A.; Walker, L.S. Attentional bias to pain and social threat in pediatric patients with functional abdominal pain and pain-free youth before and after performance evaluation. PAIN 2011, 152, 1061–1067. [Google Scholar] [CrossRef]
- van der Veek, S.M.; Derkx, B.H.; Plak, R.D.; Benninga, M.A.; Boer, F.; Lindauer, R.J.; de Haan, E. Attentional bias to activity of different parts of the body in children with functional abdominal pain: An experimental study. J. Pediatr. Psychol. 2014, 39, 438–449. [Google Scholar] [CrossRef][Green Version]
- Hermann, C.; Zohsel, K.; Hohmeister, J.; Flor, H. Cortical correlates of an attentional bias to painful and innocuous somatic stimuli in children with recurrent abdominal pain. PAIN 2008, 136, 397–406. [Google Scholar] [CrossRef]
- Lau, J.Y.F.; Heathcote, L.C.; Beale, S.; Gray, S.; Jacobs, K.; Wilkinson, N.; Crombez, G. Cognitive Biases in Children and Adolescents with Chronic Pain: A Review of Findings and a Call for Developmental Research. J. Pain 2018, 19, 589–598. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, C.E.; Dunkel, L.; McEver, M.; Israel, T.; Taylor, R.; Chiriboga, G.; Goins, K.V.; Rahn, E.J.; Mudano, A.S.; Roberson, E.D.; et al. A REDCap-based model for electronic consent (eConsent): Moving toward a more personalized consent. J. Clin. Transl. Sci. 2020, 4, 345–353. [Google Scholar] [CrossRef] [PubMed]
- Carlson, M.J.; Moore, C.E.; Tsai, C.M.; Shulman, R.J.; Chumpitazi, B.P. Child and parent perceived food-induced gastrointestinal symptoms and quality of life in children with functional gastrointestinal disorders. J. Acad. Nutr. Diet 2014, 114, 403–413. [Google Scholar] [CrossRef] [PubMed]
- Teh, E.J.; Yap, M.J.; Liow, S.J.R. PiSCES: Pictures with social context and emotional scenes with norms for emotional valence, intensity, and social engagement. Behav. Res. Methods 2018, 50, 1793–1805. [Google Scholar] [CrossRef] [PubMed]
- Jungmann, S.M.; Witthöft, M. Medically unexplained symptoms in children and adolescents: Illness-related self-concept and parental symptom evaluations. J. Behav. Ther. Exp. Psychiatry 2020, 68, 101565. [Google Scholar] [CrossRef]
- Weck, F.; Witthöft, M. Context effects in the evaluation of bodily symptoms: Comparing three versions of the Health Norms Sorting Task. J. Exp. Psychopathol. 2017, 8, 241–251. [Google Scholar] [CrossRef]
- Varni, J.W.; Lane, M.M.; Burwinkle, T.M.; Fontaine, E.N.; Youssef, N.N.; Schwimmer, J.B.; Pardee, P.E.; Pohl, J.F.; Easley, D.J. Health-related quality of life in pediatric patients with irritable bowel syndrome: A comparative analysis. J. Dev. Behav. Pediatr. 2006, 27, 451–458. [Google Scholar] [CrossRef]
- Walker, L.S.; Beck, J.E.; Garber, J.; Lambert, W. Children’s Somatization Inventory: Psychometric properties of the revised form (CSI-24). J. Pediatr. Psychol. 2009, 34, 430–440. [Google Scholar] [CrossRef] [PubMed]
- Gehrt, T.B.; Niziurski, J.A.; Frostholm, L.; Berntsen, D. Encoding and retrieval biases for health-related scenes in patients with severe health anxiety(.). Memory 2019, 27, 1110–1121. [Google Scholar] [CrossRef]
- Niziurski, J.A.; Berntsen, D. Involuntary versus voluntary episodic memories: The effects of encoding factors and emotion. Psychol. Conscious. Theory Res. Pract. 2019, in press. [Google Scholar] [CrossRef]
- Teh, E.J.; Yap, M.J.; Rickard Liow, S.J. Emotional Processing in Autism Spectrum Disorders: Effects of Age, Emotional Valence, and Social Engagement on Emotional Language Use. J. Autism Dev. Disord. 2018, 48, 4138–4154. [Google Scholar] [CrossRef] [PubMed]
- Wright, K.D.; Asmundson, G.J.G. Health Anxiety in Children: Development and Psychometric Properties of the Childhood Illness Attitude Scales. Cogn. Behav. Ther. 2003, 32, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Thorisdottir, A.S.; Villadsen, A.; LeBouthillier, D.M.; Rask, C.U.; Wright, K.D.; Walker, J.R.; Feldgaier, S.; Asmundson, G.J.G. Measurement invariance across Genders on the Childhood Illness Attitude Scales (CIAS). J. Psychosom. Res. 2017, 98, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Brysbaert, M.; Stevens, M. Power Analysis and Effect Size in Mixed Effects Models: A Tutorial. J. Cogn. 2018, 1, 9. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 17; StataCorp LLC: College Station, TX, USA, 2021. [Google Scholar]
- Williams, J.M.; Mathews, A.; MacLeod, C. The emotional Stroop task and psychopathology. Psychol. Bull. 1996, 120, 3–24. [Google Scholar] [CrossRef] [PubMed]
- Jack, F.; Leov, J.; Zajac, R. Age-related differences in the free-recall accounts of child, adolescent, and adult witnesses. Appl. Cogn. Psychol. 2014, 28, 30–38. [Google Scholar] [CrossRef]
- McManis, M.H.; Bradley, M.M.; Berg, W.K.; Cuthbert, B.N.; Lang, P.J. Emotional reactions in children: Verbal, physiological, and behavioral responses to affective pictures. Psychophysiology 2001, 38, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Belmon, J.; Noyer-Martin, M.; Jhean-Larose, S. Differences in young children’s emotional valence ratings of 180 stimuli. Personal. Individ. Differ. 2023, 206, 112121. [Google Scholar] [CrossRef]
- Sabater, L.; Guasch, M.; Ferré, P.; Fraga, I.; Hinojosa, J.A. Spanish affective normative data for 1,406 words rated by children and adolescents (SANDchild). Behav. Res. Methods 2020, 52, 1939–1950. [Google Scholar] [CrossRef] [PubMed]
- Heathcote, L.C.; Koopmans, M.; Eccleston, C.; Fox, E.; Jacobs, K.; Wilkinson, N.; Lau, J.Y.F. Negative Interpretation Bias and the Experience of Pain in Adolescents. J. Pain 2016, 17, 972–981. [Google Scholar] [CrossRef]
- Gomborone, J.E.; Dewsnap, P.A.; Libby, G.W.; Farthing, M.J. Selective affective biasing in recognition memory in the irritable bowel syndrome. Gut 1993, 34, 1230–1233. [Google Scholar] [CrossRef]
- Witthöft, M.; Kerstner, T.; Ofer, J.; Mier, D.; Rist, F.; Diener, C.; Bailer, J. Cognitive biases in pathological health anxiety: The contribution of attention, memory, and evaluation processes. Clin. Psychol. Sci. 2016, 4, 464–479. [Google Scholar] [CrossRef]
| Participants | Possible Range | Total | Children (8 to 12 Years) | Adolescents (13 to 17 Years) |
|---|---|---|---|---|
| N (% female) | 96 (47.92%) | 51 (49.02%) | 45 (46.67%) | |
| Age (mean (SD)) | 12.32 (2.56) | 10.27 (1.43) | 14.64 (1.23) | |
| Scores on questionnaires (median (IQR)) | ||||
| Children’s Somatic Symptoms Inventory 1 | 0–96 | 8.00 (11.00) | 8.00 (11.0) | 11.0 (10.00) |
| Childhood Illness Attitude Scale 2 | 11–33 | 15.00 (5.00) | 14.00 (6.00) | 16.00 (4.00) |
| Pediatric Quality of Life Inventory 1, Gastrointestinal Symptoms scale | 0–100 | 86.11 (19.44) | 91.66 (19.44) | 86.11 (16.66) |
| Parents | ||||
| Education | ||||
| High school, N (%) 3 | <5 | <5 | <5 | |
| Vocational education, N (%) | 13 (13.54) | 6 (11.76) | 7 (15.56) | |
| Continuing education, N (%) 3 | 8 (8.33) | <5 | 5 (11.11) | |
| Higher education, N (%) | 74 (77.08) | 42 (82.35) | 32 (71.11) | |
| Employment | ||||
| Full- or part-time employment, N (%) | 89 (92.71) | 45 (88.24) | 44 (97.78) | |
| Unemployed, N (%) 3 | <5 | <5 | <5 | |
| Other (e.g., sick leave, maternity leave), N (%) 3 | 6 (6.25) | 5 (9.80) | <5 | |
| Marital status | ||||
| Living together, N (%) | 85 (85.54) | 46 (90.20) | 39 (86.67) | |
| Living apart, N (%)3 | 10 (10.42) | <5 | 6 (13.33) | |
| Other, N (%) 3 | <5 | <5 | <5 | |
| Yearly household income | ||||
| Low income (<500,000 DKK), N (%)3 | 5 (5.21) | <5 | <5 | |
| Middle income (500,000–1,000,000 DKK), N (%) | 47 (48.96) | 24 (47.06) | 23 (51.11) | |
| High income (>1,000,000 DKK), N (%) | 44 (45.84) | 23 (45.10) | 21 (46.67) |
| Possible Range | Total (N = 96) | Girls (N = 46) | Boys (N = 50) | Test statistic | p | Children (N = 51) | Adolescents (N = 45) | Test Statistic | p | |
|---|---|---|---|---|---|---|---|---|---|---|
| Encoding | ||||||||||
| Healthy | 12.50 (5.00) | 13.00 (4.00) | 12.00 (6.00) | 0.45 b | 0.65 | 12.00 (6.00) | 13.00 (4.00) | −1.59 b | 0.11 | |
| No longer healthy | 7.50 (5.00) | 7.00 (4.00) | 8.00 (6.00) | −0.45 b | 0.65 | 8.00 (6.00) | 7.00 (4.00) | 1.59 b | 0.11 | |
| Free recall | ||||||||||
| Words recalled | 0–20 | 7.00 (6.00) | 8.00 (6.00) | 6.50 (5.00) | 0.85 b | 0.40 | 6.00 (4.00) | 8.00 (4.00) | −2.17 b | 0.03 |
| Gastrointestinal words recalled | 0–10 | 3.00 (3.00) | 3.00 (3.00) | 3.00 (3.00) | 0.28 b | 0.78 | 3.00 (3.00) | 3.00 (3.00) | −0.42 b | 0.67 |
| General words recalled | 0–10 | 4.00 (3.00) | 4.00 (4.00) | 3.00 (4.00) | 1.16 b | 0.25 | 3.00 (3.00) | 4.00 (5.00) | −3.31 b | <0.01 |
| Recognition | ||||||||||
| Words correctly recognized in total | 0–40 | 37.00 (2.00) | 37.00 (2.00) | 37.00 (2.00) | 1.01 a | 0.31 | 37.00 (2.00) | 37.00 (3.00) | −0.75 a | 0.45 |
| General words correctly recognized | 0–20 | 19.00 (2.00) | 19.00 (1.00) | 19.00 (2.00) | 1.60 a | 0.11 | 19.00 (1.00) | 19.00 (2.00) | 1.28 a | 0.20 |
| Difficulty | 1–7 | 2.00 (2.50) | 2.50 (2.00) | 2.00 (3.00) | 0.49 a | 0.63 | 2.00 (2.00) | 2.00 (3.00) | 0.59 a | 0.55 |
| Confidence | 1–7 | 5.00 (2.00) | 5.00 (2.00) | 5.00 (2.00) | −0.23 a | 0.82 | 5.00 (1.00) | 5.00 (2.00) | 1.91 a | 0.06 |
| Gastrointestinal words correctly recognized | 0–20 | 18.00 (2.00) | 18.00 (2.00) | 18.50 (2.00) | −0.16 a | 0.87 | 18.00 (3.00) | 19.00 (2.00) | −2.17 a | 0.03 |
| Difficulty | 1–7 | 3.00 (2.00) | 3.00 (1.00) | 3.00 (2.00) | −0.39 a | 0.70 | 3.00 (2.00) | 3.00 (1.00) | 1.14 a | 0.26 |
| Confidence | 1–7 | 5.00 (2.00) | 5.00 (2.00) | 5.00 (2.00) | −0.19 a | 0.85 | 5.00 (2.00) | 5.00 (2.00) | 0.53 a | 0.60 |
| Possible Range | Total (N= 96) | Girls (N = 46) | Boys (N = 50) | Test Statistic | p | Children (N = 51) | Adolescents (N = 45) | Test Statistic | p | |
|---|---|---|---|---|---|---|---|---|---|---|
| Encoding | ||||||||||
| Emotional valence | 1–100 | 69.00 (11.40) | 69.60 (10.06) | 68.50 (10.33) | −1.30 b | 0.20 | 67.93 (13.00) | 70.00 (8.80) | −1.02 b | 0.31 |
| Physical reaction | 1–7 | 1.27 (0.93) | 1.40 (1.07) | 1.20 (0.93) | 1.22 a | 0.22 | 1.47 (1.33) | 1.20 (0.46) | 2.05 a | 0.04 |
| Self-relevance | 1–7 | 4.37 (1.30) | 4.13 (1.27) | 4.43 (1.27) | −0.49 b | 0.63 | 4.20 (1.27) | 4.40 (1.33) | −1.01 b | 0.31 |
| Free recall | ||||||||||
| Pictures recalled | 0–15 | 3.00 (2.00) | 3.00 (2.00) | 3.00 (3.00) | 0.30 b | 0.76 | 3.00 (2.00) | 3.00 (2.00) | −0.74 b | 0.46 |
| Fun pictures recalled | 0–5 | 1.00 (2.00) | 1.00 (2.00) | 1.00 (2.00) | −0.43 b | 0.67 | 1.00 (2.00) | 1.00 (1.00) | 0.18 b | 0.86 |
| School pictures recalled | 0–5 | 1.00 (2.00) | 1.00 (2.00) | 1.00 (2.00) | 0.39 b | 0.70 | 1.00 (2.00) | 1.00 (2.00) | −1.11 b | 0.27 |
| Food pictures recalled | 0–5 | 1.00 (1.50) | 1.00 (1.00) | 1.00 (2.00) | 0.54 b | 0.59 | 1.00 (2.00) | 1.00 (1.00) | −0.33 b | 0.75 |
| Emotional valence of recalled picture | 1–100 | 68.20 (20.76) | 64.50 (16.25) | 74.38 (19.75) | −2.43 b | 0.01 | 68.40 (24.64) | 68.00 (20) | −0.41 b | 0.68 |
| Physical reaction of recalled pictures | 1–7 | 1.20 (1.00) | 1.45 (1.25) | 1.00 (1) | 1.43 a | 0.15 | 1.60 (1.71) | 1.10 (0.50) | 2.05 a | 0.04 |
| Recognition | ||||||||||
| Pictures correctly recognized | 0–15 | 15.00 (0) | 15.00 (0) | 15.00 (0) | 1.95 a | 0.05 | 15.00 (0) | 15.00 (0) | 0.11 a | 0.92 |
| Difficulty | 1–7 | 1.07 (0.27) | 1.07 (0.13) | 1.20 (0.33) | −1.34 a | 0.18 | 1.07 (0.33) | 1.07 (0.20) | 1.32 a | 0.19 |
| Confidence | 1–7 | 6.93 (3.00) | 6.97 (0.47) | 6.93 (0.20) | 0.02 a | 0.98 | 6.93 (0.73) | 6.93 (0.13) | −1.32 a | 0.19 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bjerre-Nielsen, E.; Kallesøe, K.H.; Nielsen, E.S.; Gehrt, T.B.; Frostholm, L.; Rask, C.U. A New Experimental Design to Examine Cognitive Biases for Gastrointestinal Related Stimuli in Children and Adolescents. Children 2023, 10, 1327. https://doi.org/10.3390/children10081327
Bjerre-Nielsen E, Kallesøe KH, Nielsen ES, Gehrt TB, Frostholm L, Rask CU. A New Experimental Design to Examine Cognitive Biases for Gastrointestinal Related Stimuli in Children and Adolescents. Children. 2023; 10(8):1327. https://doi.org/10.3390/children10081327
Chicago/Turabian StyleBjerre-Nielsen, Ellen, Karen Hansen Kallesøe, Eva Skovslund Nielsen, Tine Bennedsen Gehrt, Lisbeth Frostholm, and Charlotte Ulrikka Rask. 2023. "A New Experimental Design to Examine Cognitive Biases for Gastrointestinal Related Stimuli in Children and Adolescents" Children 10, no. 8: 1327. https://doi.org/10.3390/children10081327
APA StyleBjerre-Nielsen, E., Kallesøe, K. H., Nielsen, E. S., Gehrt, T. B., Frostholm, L., & Rask, C. U. (2023). A New Experimental Design to Examine Cognitive Biases for Gastrointestinal Related Stimuli in Children and Adolescents. Children, 10(8), 1327. https://doi.org/10.3390/children10081327







