Abstract
Originating in the 1970s, magnetic compression anastomosis (MCA) has lately been revisited with a focus on minimal invasive surgery (MIS). The aim of this report is to reappraise our earlier experience with MCA with the intention of facilitating future MCA advancement. A retrospective review was conducted regarding preclinical experiments and clinical trials at a single institution from 1980 to 1995. The reviewed information was compiled and appraised to generate proposals for future MCA use. The experimental studies, including 250 MCA cases in gastrointestinal and urinary tract animal models, demonstrated the technical versatility of MCA as well as the superior biomechanical characteristics in comparison to hand-sewn anastomoses. Clinical trials encompassed 87 MCA procedures in 86 children, 2 to 10 years of age, involving the following techniques: non-operative esophageal recanalization (n = 15), non-operative ileostomy undiversion (n = 46), Swenson pull-through (n = 10), non-operative urethral recanalization (n = 5), and extravesical ureterocystoneostomy (n = 11). Clinical MCA was found to be successful in over 87% of cases. MCA limitations concerning anastomotic failure and scarring were thought to be mostly due to inadequate magnetic compression. Based on our historic experience, we propose further research on the technical aspects of MCA, along with the biological aspects of anastomotic tissue remodeling. Magnets should be designed and manufactured for a wide spectrum of pediatric surgical indications, particularly in combination with novel MIS techniques.
1. Introduction
First introduced in adult colorectal surgery in the Netherlands some 40 years ago [1], magnetic compression anastomosis (MCA) has lately been revisited under the term “magnamosis”, particularly in the context of pediatric minimally invasive surgery (MIS) [2,3,4,5,6].
Remarkably, the number of publications and presentations on the topic has been increasing over the past decade, especially in pediatric surgery. While this is indicative of a greater interest in the potential use of MCA, the more recent clinical applications are still limited to case presentations and small patient series [4,5,6,7,8,9,10,11,12,13].
Following the historical Dutch report [1], a pilot project on MCA use in pediatric surgery, including pre-clinical animal experiments and clinical trials, was implemented at the Department of Pediatric Surgery, N.I. Pirogov Russian National Research Medical University the Moscow, N.F. Filatov Children’s Hospital, Moscow, starting from the 1980s and continuing well into the early 1990s. Most of these data, however, have not been published in the English literature.
After the described experiments, magnetic compression anastomosis was not pursued for various reasons, but it experienced a renaissance recently. The goal of this article is to bridge the knowledge gap between the historic experience and current studies on magnetic compression anastomosis. Therefore, the aim of this report is to reappraise our earlier and relatively extensive experience with MCA, and to evaluate the results that may be pertinent to contemporary proposals for MCA advancement.
2. Materials and Methods
A retrospective review of the above-mentioned single-institution materials, dated from 1980 to 1995, was conducted on MCA in preclinical experiments on animal models and subsequent clinical trials. The originally designed MCA techniques for specific pediatric surgical and urological applications were assessed from historic records. The sources of the reviewed information included literature publications, summaries of PhD theses, certified patents documentation (all in Russian language), and some personal records of the authors.
Specifically, the analysis of the information focused on the aspects of the safety and technical feasibility of MCA, considering the biological formation and biomechanical characteristics of the newly formed anastomoses with a focus on potential prospective and innovative clinical applications.
The extrapolated information was used to propose ideas for MCA advancement in pediatric surgery in accord with recent reports on contemporary applications of MCA, as identified in a literature search.
3. Results
3.1. General Aspects and Preclinical Experiments
There was a total of 250 preclinical, experimental MCA cases of different types in various locations in the digestive and urinary tracts, primarily performed in canine and rabbit models (Table 1). All experiments were performed with the use of Samarium Cobalt (SaCo) magnets with a variable geometrical shape, size, and coercivity force.

Table 1.
Overview of preclinical MCA experiments.
Technical and biomechanical characteristics were evaluated in comparison with corresponding hand-sewn anastomoses as controls in animal models [14,15,16,17,18,19,20,21,22,23].
Performing MCA was simple, effectively facilitating the formation of sutureless anastomoses via an endoluminal approach [14,15,16,17,18,19,20,21].
The results of biomechanical and histomorphological studies on all animal models showed that, at various postoperative intervals from 1 day to 1 month, the MCA in general had characteristically superior anastomotic properties compared to the hand-sewn controls (Figure 1).
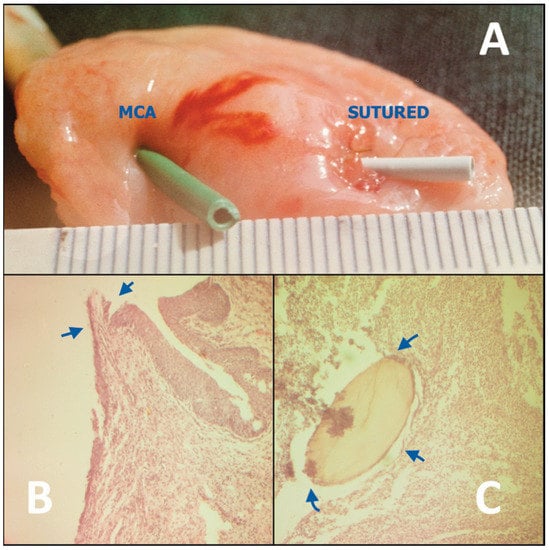
Figure 1.
Canine model of an MCA constructed between the ureter and urinary bladder (left) in comparison with a hand-sewn control (right), shown on postoperative day 14. (A) Compared to the hand-sewn anastomosis, which shows swelling and granulation tissue, the MCA more closely resembles the native ureteric orifice. (B) Histological image of the MCA, showing complete epithelization at the compression/anastomotic line (arrows). (C) Histological image of the sutured anastomosis with intramural suppurative changes around the suture material (arrows).
In particular, MCA demonstrated high tensile strength, most likely due to the healing by primary intention with no resultant leakage or excessive scarring or strictures [16,17,18,19,20,21].
Tensile strength tests on the intestinal rabbit models at 1, 5, 7–10, 14, and 21 postoperative days demonstrated bursting pressures that were 1.5 to 2-fold greater than after hand-sewn anastomoses in a control series (n = 35) [15,16].
Histological examinations of the MCA at 1, 5, 7–10, 14, 21, and 30 days postoperatively confirmed seamless healing in both the gastrointestinal (n = 96) and urinary (n = 84) tract models. We also found primary epithelization within 7–10 days (Figure 1B). In contrast, healing of hand-sewn analogues in all control groups was associated with ongoing suppurative inflammation with intramural micro-abscesses around the absorbable suture material (polyglactin or catgut), which were identifiable up to 1 month postoperatively, and resulted in fibrous tissue proliferation (Figure 1C) [15,17,18,20].
In seven cases of experimental colorectal MCA, anastomotic perforation and dehiscence was noted when using magnets with high coercivity force and small compression surfaces. A combination of these mechanical factors led to focal tissue overload with subsequent tissue tearing and perforation [15]. Therefore, a limitation for MCA was postulated as using strong magnets with minimally rounded edges and small compression surface.
In summary, the following factors were identified for successful MCA formation.
- At the anastomotic line, epithelization and connective tissue matrix proliferation dynamically develop at the so called “zone of moderate compression”, where the compression forces decrease gradually towards the periphery. This is effectively modulated by the rounded edges of magnetic compression surfaces. Flat magnets should not be used for MCA because they are associated with a higher degree of scarring and, thus, stricture formation.
- In the demarcated central zone, maximal compression is required to ensure reliable anastomotic coaptation, and to exponentially compress the subjected tissue to the point of desiccation and necrosis, preventing suppurative necrosis with inflammation within the anastomosis itself, which may lead to inadequate anastomosis formation and increased proliferation of granulation tissue.
- At the demarcation zone that constitutes the inner anastomotic line, epithelization steadily progresses and bridges the rim of the thinned desiccated central tissue. The magnet thereby gradually becomes detached and passes distally within 7 to 10 days; thus, the anastomotic healing by primary intention is completed (Figure 2) [15,17,18,20].
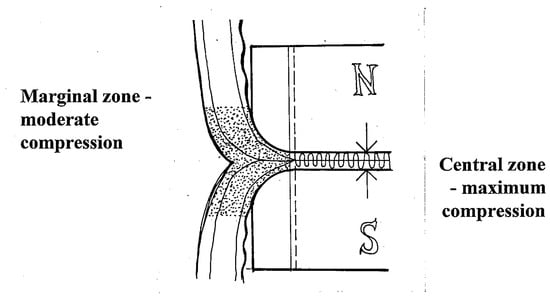 Figure 2. Diagram of optimal MCA formation. The central tissues are highly compressed to produce desiccation and necrosis, while gradient compression in the periphery allows healing and promotes trans-anastomotic mucosal bridging (N: magnetic north, S: magnetic south).
Figure 2. Diagram of optimal MCA formation. The central tissues are highly compressed to produce desiccation and necrosis, while gradient compression in the periphery allows healing and promotes trans-anastomotic mucosal bridging (N: magnetic north, S: magnetic south).
3.2. Review of Clinical Trials
A review of the records revealed a total of 87 MCA procedures performed in 86 selected patients, 2 to 10 years of age. The MCA clinical applications involved using SaCo magnets of specific geometric configuration, size, and compressing force, based on the preclinical experimental evaluations detailed above. Indications comprised various pathological conditions of the gastrointestinal and urinary tracts in pediatric surgical practice [15,16,17,18,19,22,23,24], detailed as follows.
3.2.1. Non-Operative MCA Esophageal Recanalization
The original technique was developed to treat short-length esophageal strictures using magnetic cylinders by means of compressing and ablating the underlying scar tissue (Figure 3). The technique was applied in fifteen patients (n = 15) with esophageal strictures 3 to 15 mm in length [14,16,22,23].
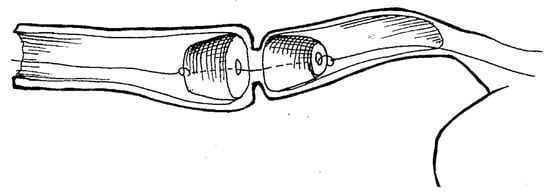
Figure 3.
Schematic principle of non-operative endoluminal esophageal recanalization of strictures using magnetic cylinders.
Under rigid esophagoscopy, specially designed magnetic cylinders 10, 12, or 14 mm in diameter were deployed to the stricture site via the gastrostomy and perorally over a guide string, which was passed through the stricture narrowing after previous bougienage. Under fluoroscopy, the magnets were then brought together into coaptation.
The magnets were followed by daily repeat X-rays for the next 3 to 5 days. The resultant MCA formation usually occurred within 7 days, when the magnets detached from the anastomosis. They were subsequently removed under fluoroscopic control and endoscopic assistance by retracting them by the attached strings [22,23].
Complete esophageal recanalization was achieved in nine cases, five of which were congeital membranous stenoses and four of which were postoperative anastomotic strictures. Adverse outcomes included esophageal perforation in one case and esophageal re-stenosis in five [22,23].
3.2.2. Non-Operative MCA Ileostomy Undiversion
A technique for enterostomy undiversion was developed using flexible silicon-coated segmented block-shaped magnets in a side-to-side configuration (Figure 4). The technique was used in forty-six patients with double barrel ileostomy when undiversion was clinically indicated [24].
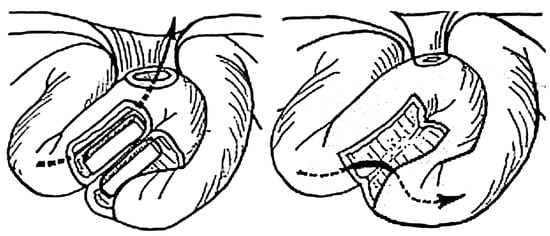
Figure 4.
Schematic drawing of endoluminal loop ileostomy undiversion using magnetic blocks. The arrow marks the flow of stool.
Technically, the magnets were fashioned with attached strings for easy retrieval after successful MCA formation. They were manually placed into each stomal limb and brought to proper coaptation under fluoroscopic guidance. Subsequent MCA formation usually occurred between 7 and 10 days [24].
Successful MCA enterostomy undiversion was achieved in forty-four patients. There were no cases of leakage, and the intestinal passage was restored in all patients. In two cases, magnet placement was aborted intraoperatively due to gross tissue interposition between the stomal limbs because it was deemed unsafe to bring magnets into the coaptation [24].
3.2.3. Swenson Type MCA-Based Pull-through for Hirschsprung Disease
A modified MCA-based Swenson pull-through technique using flexible silicon-coated segmented magnetic rings of 20 to 40 mm diameter was designed to treat rectosigmoid Hirschsprung disease in 10 patients (Figure 5) [14,15,16].
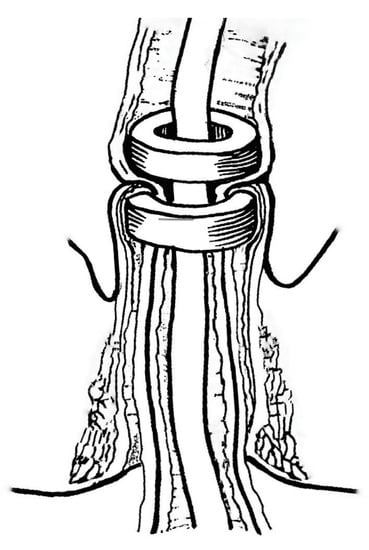
Figure 5.
Principle of MCA-based Swenson pull-through for Hirschsprung disease.
Technically, the procedure entailed an open approach via conventional laparotomy. The affected bowel segment was conventionally mobilized with deep pelvic dissection to the lower rectal level. The proximal magnetic ring was delivered intra-luminally through the anus to the upper limit of the intended resection, which was followed by eversion of the mobilized bowel portion trans-anally. The distal magnetic ring was then placed over the everted recto-sigmoidal cylinder. The magnetic rings were brought into coaptation at the level above the anal verge, creating an end-to-end colorectal MCA. A rectal tube was inserted intra-luminally through the magnetic rings proximally to the anastomosis and the everted bowel cylinder was then excised.
Magnet coaptation was verified intraoperatively using fluoroscopy and monitored postoperatively by serial radiographs. The MCA usually formed within 8 to 12 days. Once the anastomosis had formed, the magnets detached and were manually removed through the anus [14,15,16].
An intact colorectal MCA with no leakage or subsequent stenosis was achieved in six patients. Adverse outcomes included post-anastomotic stenosis in two patients (n = 2) with bulky-thickness bowel wall interposed between the magnetic rings [16].
3.2.4. Non-Operative Urethral Recanalization
Small diameter magnetic cylinders were used to treat short-length post-traumatic urethral strictures (Figure 6). The technique was applied in five patients with short strictures that were less than 5 mm in length [17,19,25].
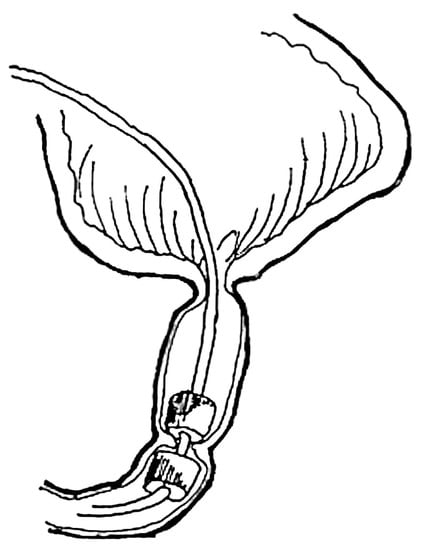
Figure 6.
Schematic drawing of endoluminal urethral recanalization using magnetic cylinders.
The upper magnetic cylinder of 4 to 6 mm diameter was delivered via rigid cystoscopy through a temporary cystostomy. The lower magnetic cylinder was delivered via cystoscopy through the meatus. Both magnets were introduced over a guide string that had been previously placed across the stricture. Fluoroscopy was used to verify good coaptation of the magnets.
Urethral MCA formation usually occurred within 7 to 10 days. After anastomosis formation, the magnets were removed by retracting them by the attached string using cystoscopy and fluoroscopic control [17,19,25].
Complete restoration of urethral patency and normal voiding patterns were achieved in four patients with membranous type strictures (n = 4). Post-anastomotic restenosis was noted in one patient with a more extensive stricture of 5 mm in length [17,19].
3.2.5. Extravesical Ureterocystoneostomy
A technique of ureteric reimplantation using small magnetic rings of 4 to 5 mm in diameter was designed to create an extravesical MCA between the ureter and urinary bladder (Figure 7). It was employed on a total of 11 ureters in 10 patients with grade 3 to 4 vesicoureteral reflux (VUR) [18,26].
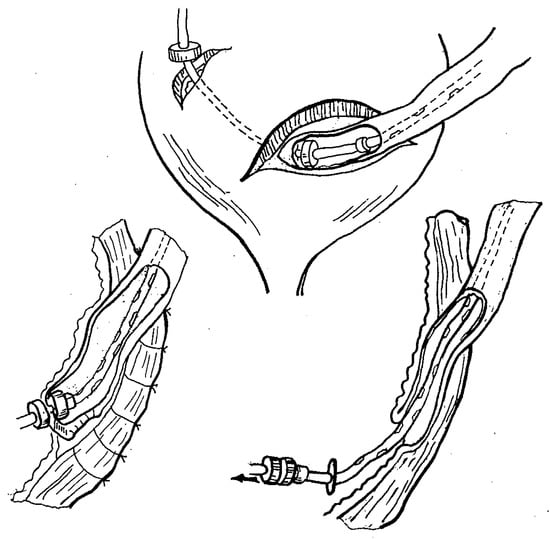
Figure 7.
Principle of extravesical ureterocystoneostomy using magnetic rings.
The procedure involved an open preperitoneal approach via a Pfannenstiel-type incision. The uretero-vesical segment was mobilized, the distal ureter was resected, and a Lich-Gregoir detrusorotomy was performed in a conventional fashion. The ureterocystoneostomy was accomplished by placing the proximal magnetic ring over a stent into the lumen of the ureter. At the point of intended anastomosis, the distal tip of the stent (with the curl cut off) was brought into the bladder by using an attached stylet piercing through both the ureteric wall and the distal corner of the denuded submucosal surface of the bladder wall. The ureteric lumen was then closed with continuous absorbable sutures. The distal magnetic ring was introduced into the bladder over the distal tip of the stent brought out via a mini-cystotomy, followed by a cystostomy tube placed over the stent. The magnets were then approximated, creating a side-to-side MCA between the full-thickness ureteric wall and the submucosal layer of the bladder wall. Ureterocystoneostomy was completed by closing the tunnel in a Lich-Gregoir fashion using interrupted absorbable sutures.
MCA formation occurred within 7 to 10 days. The magnets detached from the anastomosis once it was formed and were removed via the cystostomy by retracting the stent and cystostomy tube [18,26].
The procedure was successfully completed in all 10 patients. No recurrent VUR or anastomotic strictures were noted in the postoperative follow-up [18].
3.3. Clinical Success for MCA
A summary of clinical outcomes is presented in Table 2, demonstrating that across all indications, MCA was successful in over 87% of cases [17,18,19,22,23,24].

Table 2.
Summary of MCA clinical outcomes.
3.4. Recognized Adverse Effects Associated with MCA
Adverse outcomes encountered in our experience are listed in Table 2. In detail, they comprised:
- Inability to safely perform ileostomy undiversion in two patients due to interposing of excessively thick tissue, so that the procedure was aborted due to safety concerns [24];
- Recurrent strictures after esophageal recanalization in five patients with corrosive strictures of irregular shape and more than 10 mm in length [22,23];
- Recurrent strictures after urethral recanalization in a patient with a stricture approximately 5.0 mm in length (n = 1) [17,19];
- Restenosis after Swenson colorectal MCA in two patients with a bulky bowel wall [15,16] that impeded proper mating of the magnets.
The pathomechanism of postoperative restenosis or stenosis (esophageal and urethral, as well as colorectal) was thought to be related to a relatively insufficient magnetic compression force, which appeared to occur in circumstances of excessive distance between magnets due to disproportionately bulky tissue interposition. Conversely, esophageal perforation was possibly due to forceful compression applied to extensive stricture scar tissue and its inability to exhibit normal healthy tissue healing.
The above scenarios should be considered limitations for clinical MCA applications [15,16,18,20,21,22].
4. Discussion
Contrary to what many believe is a recent, novel development, MCA has previously been explored in both animal experiments and clinical trials in our institution in Moscow several decades ago. Our historic experience with MCA, reported for the first time in the English literature, dates as far back as the 1980s and early 1990s. Nonetheless, many of the issues regarding MCA and its challenges resonate with contemporary reports. Our experience spans a large spectrum of indications, ranging from pediatric upper gastrointestinal, colorectal, and urological applications.
Recently, other groups have been reviving MCA for use in various pediatric surgical indications [13], including esophageal atresia repair [11,12,27], rectal atresia [9], duodenal stenosis [10], vascular anastomosis [28], and for re-cannulation of the hypopharynx [29]. Several experimental studies have been conducted in swine [30,31], rabbits, and dogs [32]. The studies confirm the above findings from decades ago and also seem to suggest that magnets can be used for creating the anastomosis, but that simultaneous approximation of pouches or structures under tension will lead to increased rates of anastomotic stricture [12].
In the field of adult surgery, magnets have also been used for a wide spectrum of applications, including duodeno–ileal anastomosis [33,34], ureterostenosis after kidney transplantation [35], hepaticojejunostomy [36,37], biliary strictures [38,39,40], as well as for foregut issues, such as strictures after esophageal cancer surgery [41] and sleeve gastrectomy [42].
Given the retrospective review nature of our historic experience with MCA, we acknowledge that this report lacks a certain grade of evidenced-based robustness. The technical aspects of each individual study are described according to our laboratory notes, scientific reports in Russian language, and doctoral theses that resulted from the experiments and clinical studies. Nonetheless, for those interested, further details and copies of the original materials are available from the corresponding authors upon specific request.
The first-hand information presented here accurately conveys our initial experience on the biological basis and applicability of MCA. To our knowledge, these are some of the first clinical applications reported, and constitute a pioneering effort to employ MCA in pediatric surgery. Particularly, the MCA experience described here were carried out in relatively large numbers, whereas many recent articles report much smaller case numbers of similar techniques.
Considering our earlier experience, we outline the rationale for the potential MCA application in gastro-intestinal and urinary tract surgery on the grounds of its superior biomechanical properties versus hand-sewn anastomosis and technical versatility allowing a greater scope for creating anastomoses, especially, in settings of the non-operative endoluminal approach and challenging surgical access in difficult anatomical areas.
The reasons for using MCA rather than a handsewn anastomosis include purely endoscopic applicability and technical simplicity, which may decrease operative times. These aspects are particularly important in multimorbid infants, which do not tolerate long operative times. In addition, MCA produces an even circular anastomosis, with less variability compared to the variability of individually placed sutures. The drawback of MCA is the timeframe in which the anastomosis forms. Compared to a hand-sewn anastomosis, the MCA is not immediately patent after placing the magnets but needs 7 to 10 days to mature. This delayed patency may postpone enteral feedings for several days, compared to a hand-sewn anastomosis. Nevertheless, we believe that MCA should be considered for minimally invasive applications in small infants that do not tolerate long operative times.
We hope that this information will provide a stimulus for the current working groups on MCA to incorporate our findings and ideas for relevant future innovative development in pediatric surgery, in particular, in conjunction with a MIS approach. Combining MCA and MIS techniques create synergy and seem like a worthwhile future direction.
At this point, we propose that further research and development of MCA is undertaken to rationalize its formation, confirm efficacy for the described indications, and explore new fields of application, particularly in pediatric surgery. Optimally, these endeavors should be conducted with interdisciplinary medical, bioscientific, and engineering input. Some of the work packages we propose are:
- Designing and industrially manufacturing biocompatible and safe rare earth magnetic devices for specific anastomotic indications with optimal parameters of compression, size, and specific geometrical shape for creating MCA in pediatric gastrointestinal and urinary structures.
- Designing and industrially manufacturing an auxiliary magnetic driving device with computerized technology that would facilitate intraluminal magnet positioning and coaptation, ensuring efficient MCA creation while electronically monitoring and securing optimal tissue compression. This should be facilitated by measuring the distance and the resulting effective magnetic coercivity force, thereby detecting possible undue anastomotic tissue tension and/or bulky tissue interposition between magnets in real-time.
- Push for further research into the development and standardization of MCA in conjuncture with pediatric MIS with a focus on the following procedures:
- ▪
- Endoluminal recanalization in short-length obstructive lesions with a various pathogenesis and localization;
- ▪
- Non-operative undiversion of intestinal stomas;
- ▪
- Laparoscopic pull-through;
- ▪
- Laparoscopic extravesical ureteric reimplantation;
- ▪
- Laparoscopic biliary-digestive reconstruction;
- ▪
- Laparoscopic duodenal atresia repair;
- ▪
- Laparoscopic-assisted repair of certain anorectal malformations;
- ▪
- Thoracoscopic esophageal atresia repair with and without a fistula.
Our proposals for designing and industrially manufacturing magnets as a specific anastomosing device along with an auxiliary computerized magnetic driving device are intended to standardize MCA technical performance and to ensure its optimal biological formation while avoiding risks of the MCA limitations, as identified in our past experience. We feel that this is paramount to ensure safe and effective MCA for neonatal and older pediatric patients. In summary, following our past experience with MCA, we believe that future research on MCA should be combined with pediatric MIS techniques that were not available when we performed our experiments and clinical studies.
5. Conclusions
This is the first comprehensive report of our historic MCA experience in the English language. The experience described in this report can be considered a true pioneering effort, which unfortunately has not been as visible as it merits so far. Our studies show that MCA should be considered as a valid alternative to hand-sewn anastomoses in a wide spectrum of pediatric surgical problems, particularly for future MIS applications. Our report underlines the surgical versatility of MCA, particularly for endoluminal applications using endoscopic delivery techniques. It also shows the importance of finding the optimal compression pressure and other biophysical properties, with the goal of producing high-quality anastomoses. Based on our findings, novel devices should be designed for specific indications, taking into consideration biological healing of the particular tissues and the required magnetic force to form the anastomosis.
Author Contributions
Conceptualization, A.M.K. and O.J.M.; Methodology, A.M.K.; Formal Analysis, A.M.K. and V.V.N.; Validation, A.M.K., V.V.N. and A.Y.R.; Writing—original draft, A.M.K.; Writing—review and editing, O.J.M. and A.M.K. All images are images and personal drawings by A.M.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Our clinical experimental studies on magnetic compression anastomosis (MCA) during 1980 to 1995 were conducted in accordance with the Declaration of Helsinki Ethical Principles for Medical Research involving human subjects (WMA General Assembly 1964, 1975, 1983) as an internationally agreed justificatory framework for human medical research. Accordingly, the approval for both preclinical animal experiments and subsequent clinical trials were granted by the Scientific Council and its Ethics Branch/Committee of the of 2nd Moscow Medical Institution named after N.I.Pirogov (now N.I.Pirogov Russian National Research Medical University). All animal experiments were carried out at the Experimental Medical Research Centre of the same institution. The welfare of animals used was fully respected. In clinical trials, the informed consents were obtained from patients’ parents as the risks, burdens, and benefits of the originally designed and first used in human procedures with MCA application were explained in detail.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data on which this publication is based are available from the corresponding author O.J.M. upon reasonable request.
Acknowledgments
We acknowledge our senior colleagues and former mentors Geraskin V.I., Isakov Y.F., Stepanov E.A., and Sharipov N.A., for their leading role in initiating the MCA pilot projects, for their involvement, and for pioneering MCA applications in pediatric surgery by devising a number of original ideas.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Jansen, A.; Keeman, J.N.; Davies, G.A.; Klopper, P.J. Early experiences with magnetic rings in resection of the distal colon. Neth. J. Surg. 1980, 32, 20–27. Available online: https://pubmed.ncbi.nlm.nih.gov/7366876/ (accessed on 28 July 2023).
- Jamshidi, R.; Stephenson, J.T.; Clay, J.G.; Pichakron, K.O.; Harrison, M.R. Magnamosis: Magnetic compression anastomosis with comparison to suture and staple techniques. J. Pediatr. Surg. 2009, 44, 222–228. [Google Scholar] [CrossRef]
- Gonzales, K.D.; Douglas, G.; Pichakron, K.O.; Kwiat, D.A.; Gallardo, S.G.; Encinas, J.L.; Hirose, S.; Harrison, M.R. Magnamosis III: Delivery of a magnetic compression anastomosis device using minimally invasive endoscopic techniques. J. Pediatr. Surg. 2012, 47, 1291–1295. [Google Scholar] [CrossRef] [PubMed]
- Wall, J.; Diana, M.; Leroy, J.; DeRuijter, V.; Gonzales, K.D.; Lindner, V.; Harrison, M.; Marescaux, J. Magnamosis IV: Magnetic compression anastomosis for minimally invasive colorectal surgery. Endoscopy 2013, 45, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Dorman, R.M.; Vali, K.; Harmon, C.M.; Zaritzky, M.; Bass, K.D. Repair of esophageal atresia with proximal fistula using endoscopic magnetic compression anastomosis (Magnamosis) after staged lengthening. Pediatr. Surg. Int. 2016, 32, 525–528. [Google Scholar] [CrossRef] [PubMed]
- Toselli, L.; Martinez-Ferro, M.; Cervio, G.; Kwiat, D.; Imamura-Ching, J.; Graves, C.E.; Gaston, B.; Harrison, M. Magnetic Compression Anastomosis (Magnamosis) for Functional Undiversion of Ileostomy in Pediatric Patients. J. Laparoendosc. Adv. Surg. Technol. 2017, 27, 1314–1317. [Google Scholar] [CrossRef] [PubMed]
- Woo, R.; Wong, C.M.; Trimble, Z.; Puapong, D.; Koehler, S.; Miller, S.; Johnson, S. Magnetic compression stricturoplasty for treatment of refractory esophageal strictures in children: Technique and lessons learned. Surg. Innov. 2017, 24, 432–439. [Google Scholar] [CrossRef]
- Liu, S.Q.; Lv, Y.; Fang, Y.; Luo, R.X.; Zhao, J.R.; Luo, R.G.; Li, Y.M.; Zhang, J.; Zhang, P.F.; Guo, J.Z.; et al. Magnetic compression for anastomosis in treating an infant born with long-gap oesophageal atresia: A case report. Medicine 2020, 99, e22472. [Google Scholar] [CrossRef]
- Liu, S.Q.; Li, Q.F.; Lv, Y.; Zhao, J.R.; Luo, R.X.; Zhang, P.F.; Guo, J.Z.; Zhang, A.P.; Li, Q.H. Magnetic compression anastomosis for rectal atresia following necrotizing enterocolitis: A case report. Medicine 2020, 99, e23613. [Google Scholar] [CrossRef]
- Liu, S.; Fang, Y.; Lv, Y.; Zhao, J.; Luo, R.; Luo, R.; Cheng, J.; Yang, H.; Zhang, A.; Shen, Y.; et al. Magnetic compression stricturoplasty in patients with severe stricture after simultaneous esophageal atresia and duodenal obstruction repair: A case report. Exp. Ther. Med. 2022, 23, 93. [Google Scholar] [CrossRef]
- Muensterer, O.J.; Evans, L.L.; Sterlin, A.; Sahlabadi, M.; Aribindi, V.; Lindner, A.; König, T.; Harrison, M.R. Novel device for endoluminal esophageal atresia repair: First-in-human experience. Pediatrics 2021, 148, e2020049627. [Google Scholar] [CrossRef]
- Holler, A.-S.; König, T.T.; Chen, C.; Harrison, M.R.; Muensterer, O.J. Esophageal magnetic compression anastomosis in esophageal atresia repair: A PRISMA-compliant systematic review and comparison with a novel approach. Children 2022, 9, 1113. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.G.; Evans, L.L.; Johnson, S.M.; Woo, R.K. The evolving use of magnets in surgery: Biomedical considerations and a review of their current applications. Bioengineering 2023, 10, 442. [Google Scholar] [CrossRef] [PubMed]
- Isakov, Y.F.; Geras’kin, V.I.; Vasil’ev, G.S.; Sharipov, N.A. Using permanent magnets in pediatric surgery. Klin. Khir. 1981, 6, 36–39. Available online: https://pubmed.ncbi.nlm.nih.gov/7024620/ (accessed on 28 July 2023).
- Sharipov, N.A. Colorectal Resections with the Use of Permanent Magnets in Children. Ph.D. Thesis, N.I. Pirogov National Medical University, Moscow, Russia, 1982. [Google Scholar]
- Stepanov, E.A.; Vasil’Ev, G.S.; Sharipov, N.A.; Rudakov, S.S.; Romakhin, I.A. Use of permanent magnets in digestive tract surgery in children. Vestn. Akad. Med. Nauk SSSR 1984, 9, 6–11. Available online: https://pubmed.ncbi.nlm.nih.gov/6388182/ (accessed on 28 July 2023).
- Nikolaev, V.V. Treatment of Urethral Strictures with the Use of Permanent Magnets in Children. Ph.D. Thesis, N.I. Pirogov National Medical University, Moscow, Russia, 1987. [Google Scholar]
- Kotlovsky, A.M. Ureteric Reimplantation with the Use of Permanent Magnets in Children. Ph.D. Thesis, N.I. Pirogov National Medical University, Moscow, Russia, 1987. [Google Scholar]
- Isakov, I.F.; Stepanov, E.A.; Erokhin, A.P.; Nikolaev, V.V.; Vasi’Lev, G.S. Surgical treatment of urethral strictures in children. Vestn. Khir. Im. I I Grek. 1989, 142, 61–66. Available online: https://pubmed.ncbi.nlm.nih.gov/2800174/ (accessed on 28 July 2023).
- Lubashevskiĭ, V.T.; Shabanov, A.M.; Vasil’ev, G.S. The inflammatory-reparative processes in the implantation of the ureter into the bladder by using the mechanical forces of permanent magnets. Bull. Exp. Biol. Med. 1993, 116, 550–552. Available online: https://pubmed.ncbi.nlm.nih.gov/8312560/ (accessed on 28 July 2023). [CrossRef]
- Nikolaev, V.V. Technical principles of urethral compression anastomoses. Bull. Exp. Biol. Med. 1998, 126, 855–858. [Google Scholar] [CrossRef]
- Stepanov, E.A.; Vasilév, G.S.; Nikolaev, V.V.; Guz, V.I.; Sharipov, N.A.; Romanov, A.V.; Goritskaia, T.A.; Vasilév, K.G. Treatment of short esophageal stricture in children. Vestn. Ross. Akad. Med. Nauk. 1994, 3, 15–19. Available online: https://pubmed.ncbi.nlm.nih.gov/7516212/ (accessed on 28 July 2023).
- Sharipov, N.A. Treatment of Esophageal Strictures. Ph.D. Thesis, N.I. Pirogov National Medical University, Moscow, Russia, 1996. [Google Scholar]
- Stepanov, E.A.; Vasil’ev, G.S.; Nikolaev, V.V. The treatment of intestinal fistulas in children by applying a by-pass anastomosis using magnetic devices. Khirurgiia (Mosk) 1992, 11, 93–95. Available online: https://pubmed.ncbi.nlm.nih.gov/1294807/ (accessed on 28 July 2023).
- Stepanov, E.A.; Nikolaev, V.V.; Kotlovsky, A.M.; Vasilév, G.S. Method of Correction of Urethral Strictures; Patent for Invention—Authors’ copyright No. 1361753; Bulletin Inventions and Discoveries, 49; USSR: Moscow, Russia, 1987. [Google Scholar]
- Isakov, Y.F.; Stepanov, E.A.; Kotlovsky, A.M.; Vasilév, G.S. Method of Ureterocystoneostomy; Patent for Invention—Authors’ copyright No. 1277452; Bulletin Inventions and Discoveries, 46; USSR: Moscow, Russia, 1986. [Google Scholar]
- Evans, L.L.; Chen, C.S.; Muensterer, O.J.; Sahlabadi, M.; Lovvorn, H.N.; Novotny, N.M.; Upperman, J.S.; Martinez, J.A.; Bruzoni, M.; Dunn, J.C.; et al. The novel application of an emerging device for salvage of primary repair in high-risk complex esophageal atresia. J. Pediatr. Surg. 2022, 57, 810–818. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Liu, S.; Lei, P.; Lv, Y.; Wu, R.; Ma, F.; Wang, H.; Luo, R. Fast and Effective Nonsuture Anastomosis of Magnetic Artificial Blood Vessel Transplantation for Caval Reconstruction in Canines. Ann. Vasc. Surg. 2020, 68, 487–496. [Google Scholar] [CrossRef]
- Mascagni, P.; Tringali, A.; Boškoski, I.; Bove, V.; Schepis, T.; Perri, V.; Costamagna, G. Magnetic kissing for the endoscopic treatment of a complete iatrogenic stenosis of the hypopharynx. Endoscopy 2023, 55, E499–E500. [Google Scholar] [CrossRef]
- Sterlin, A.; Evans, L.; Mahler, S.; Lindner, A.; Dickmann, J.; Heimann, A.; Sahlabadi, M.; Aribindi, V.; Harrison, M.R.; Muensterer, O.J. An experimental study on long term outcomes after magnetic esophageal compression anastomosis in piglets. J. Pediatr. Surg. 2022, 57, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Hornok, Z.; Kubiak, R.; Csukas, D.; Ferencz, A.; Cserni, T. Esophageal Magnetic Anastomosis Device (EMAD) to simplify and improve outcome of thoracoscopic repair for esophageal atresia with tracheoesophageal fistula: A proof of concept study. J. Pediatr. Surg. 2023, 58, 1489–1493. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.-H.; Lv, Y.; Liu, S.-Q.; Cui, X.-H.; Suo, R.-Y. Esophageal magnetic compression anastomosis in dogs. World J. Gastroenterol. 2022, 28, 5313–5323. [Google Scholar] [CrossRef]
- Gagner, M.; Krinke, T.; Lapointe-Gagner, M.; Buchwald, J.N. Side-to-side duodeno-ileal magnetic compression anastomosis: Design and feasibility of a novel device in a porcine model. Surg. Endosc. 2023, 37, 6197–6207. [Google Scholar] [CrossRef]
- Gagner, M.; Abuladze, D.; Koiava, L.; Buchwald, J.N.; Van Sante, N.; Krinke, T. First-in-Human Side-to-Side Magnetic Compression Duodeno-ileostomy with the Magnet Anastomosis System. Obes. Surg. 2023, 33, 2282–2292. [Google Scholar] [CrossRef]
- Zhang, J.; Xue, W.; Tian, P.; Yan, H.; Zheng, J.; Li, X.; Wang, Y.; Ding, X.; Lyu, Y. Clinical effect of magnetic compression anastomosis on ureterostenosis after kidney transplantation. Chin. Med. J. 2023, 136, 1006–1008. [Google Scholar] [CrossRef]
- Gökçe, D.T.; Ödemiş, B.; Erdoğan, Ç. Magnetic compression anastomosis using a double-balloon enteroscope for complete obstruction of Roux-en-Y hepaticojejunostomy anastomosis. Endoscopy 2022, 54, E945–E947. [Google Scholar] [CrossRef]
- Suyama, K.; Takamori, H.; Yamanouchi, E.; Tanaka, H.; Sakamoto, Y.; Ikuta, Y.; Maki, Y.; Sakurai, K.; Hirota, M.; Baba, H.; et al. Recanalization of Obstructed Choledochojejunostomy Using the Magnet Compression Anastomosis Technique. Am. J. Gastroenterol. 2010, 105, 230–231. [Google Scholar] [CrossRef] [PubMed]
- Ödemiş, B.; Başpınar, B.; Tola, M.; Torun, S. Magnetic Compression Anastomosis Is a Good Treatment Option for Patients with Completely Obstructed Benign Biliary Strictures: A Case Series Study. Dig. Dis. Sci. 2022, 67, 4906–4918. [Google Scholar] [CrossRef] [PubMed]
- Akita, H.; Hikita, H.; Yamanouchi, E.; Marubashi, S.; Nagano, H.; Umeshita, K.; Dono, K.; Tsutsui, S.; Hayashi, N.; Monden, M. Use of a metallic-wall stent in the magnet compression anastomosis technique for bile duct obstruction after liver transplantation. Liver Transplant. 2007, 14, 118–120. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Scientific Committee of the Third International Conference of Magnetic Surgery; Zhang, N.; Lv, Y. Expert consensus on magnetic recanalization technique for biliary anastomotic strictures after liver transplantation. HepatoBiliary Surg. Nutr. 2021, 10, 401–404. [Google Scholar] [CrossRef]
- Isozaki, T.; Murakami, K.; Yamanouchi, E.; Uesato, M.; Toyozumi, T.; Koide, Y.; Tsukamoto, S.; Sakata, H.; Hayano, K.; Kano, M.; et al. Magnetic compression anastomosis is effective in treating stenosis after esophageal cancer surgery: A case report. Surg. Case Rep. 2020, 6, 213. [Google Scholar] [CrossRef]
- Liu, K.; Lu, Q.; Huang, G.-B.; Zhou, J.-W.; Wang, X.-Y.; Chang, P.-K.; Zhang, W.; Yu, J.-W.; Lyu, Y.; Wang, S.-P. Use of the magnetic compression technique in sleeve gastrectomy. Chin. Med. J. 2020, 133, 2768–2770. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).