Pediatric Elbow Dislocations and Associated Fractures
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Population
2.3. Inclusion/Exclusion Criteria
2.4. Data Collection/Analysis
3. Results
3.1. Demographic Data
3.2. Mechanism of Injury
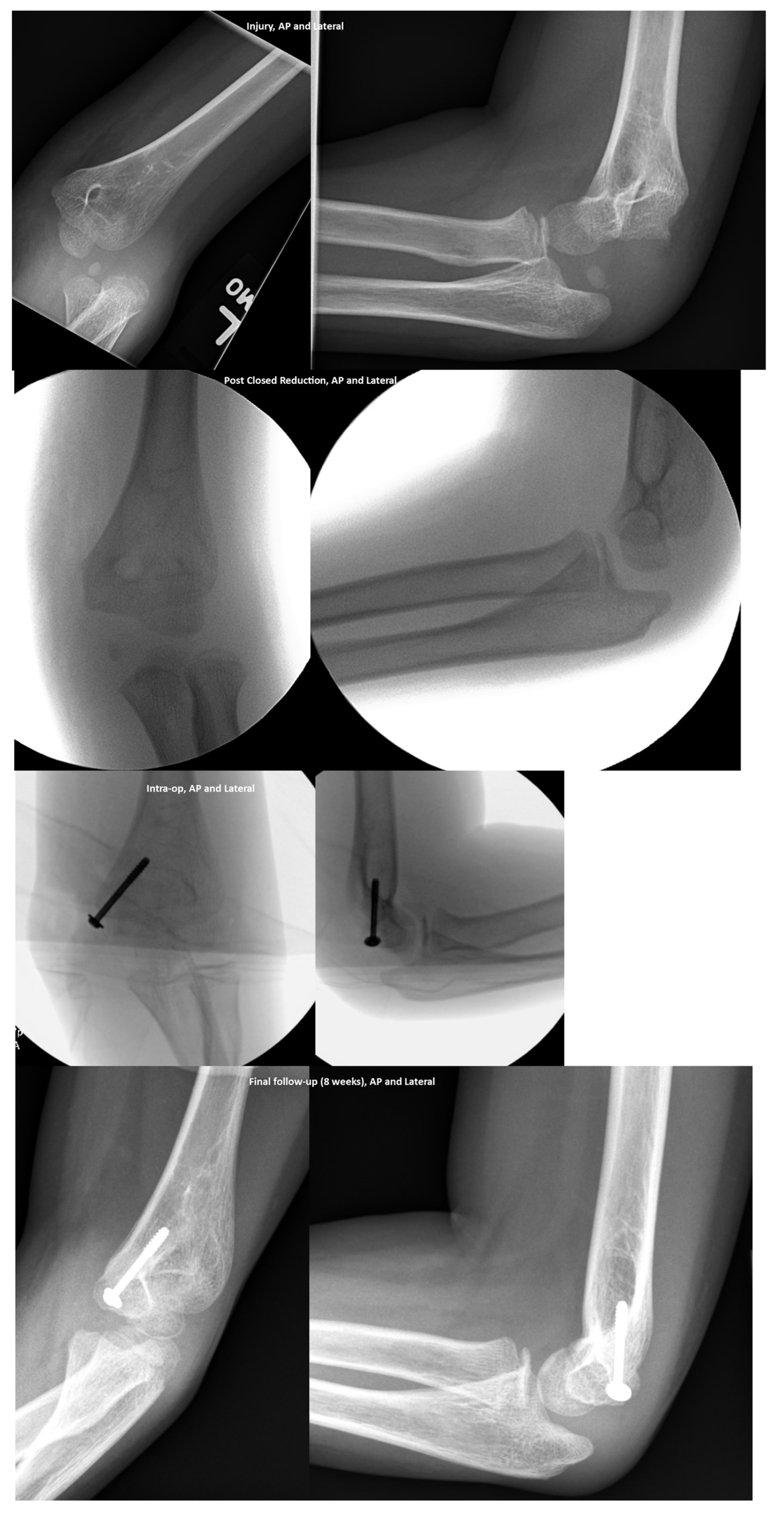
3.3. Treatment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sofu, H.; Gursu, S.; Camurcu, Y.; Yildirim, T.; Sahin, V. Pure elbow dislocation in the paediatric age group. Int. Orthop. 2016, 40, 541–545. [Google Scholar] [CrossRef] [PubMed]
- Murphy, R.F.; Vuillermin, C.; Naqvi, M.; Miller, P.E.; Bae, D.S.; Shore, B.J. Early outcomes of pediatric elbow dislocation-risk factors associated with morbidity. J. Pediatr. Orthop. 2017, 37, 440–446. [Google Scholar] [CrossRef] [PubMed]
- Bilgili, F.; Dikmen, G.; Baş, A.; Asma, A.; Batibay, S.G.; Şirikçi, M.; Atalar, A.C. Acute traumatic posterior fracture dislocation of the elbow in pediatric patients: Impact of surgery time and associated fractures on outcome. J. Pediatr. Orthop. B 2016, 25, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Tarallo, L.; Mugnai, R.; Fiacchi, F.; Adani, R.; Zambianchi, F.; Catani, F. Pediatric medial epicondyle fractures with intra-articular elbow incarceration. J. Orthop. Traumatol. 2015, 16, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Magee, L.C.B.; Baghdadi, S.; Gohel, S.B.; Sankar, W.N. Complex Fracture-Dislocations of the Elbow in the Pediatric Population. J. Pediatr. Orthop. 2021, 41, e470–e474. [Google Scholar] [CrossRef] [PubMed]
- Herring, J.A.; Tachdjian, M.O. Tachdjian’s Pediatric Orthopaedics: From the Texas Scottish Rite Hospital for Children, 5th ed.; Saunders: Philadelphia, PA, USA, 2014. [Google Scholar]
- Knapik, D.M.; Fausett, C.L.; Gilmore, A.; Liu, R.W. Outcomes of Nonoperative Pediatric Medial Humeral Epicondyle Fractures with and without Associated Elbow Dislocation. J. Pediatr. Orthop. 2017, 37, e224–e228. [Google Scholar] [CrossRef] [PubMed]
- Vuillermin, C.; Donohue, K.S.; Miller, P.; Bauer, A.S.; Kramer, D.E.; Yen, Y.-M. Incarcerated Medial Epicondyle Fractures with Elbow Dislocation: Risk Factors Associated with Morbidity. J. Pediatr. Orthop. 2019, 39, e647–e651. [Google Scholar] [CrossRef] [PubMed]
- Farsetti, P.; Potenza, V.; Caterini, R.; Ippolito, E. Long-Term Results of Treatment of Fractures of the Medial Humeral Epicondyle in Children. J. Bone Jt. Surg. 2001, 83, 1299–1305. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, J.T.R.; Patel, N.M.; Macknin, J.; Flynn, J.M.; Cameron, D.; Wolfgruber, H.C.; Ganley, T.J. Return to competitive sports after medial epicondyle fractures in adolescent athletes: Results of operative and nonoperative treatment. Am. J. Sports Med. 2013, 41, 1152–1157. [Google Scholar] [CrossRef] [PubMed]
- Hyvönen, H.; Korhonen, L.; Hannonen, J.; Serlo, W.; Sinikumpu, J.-J. Recent trends in children’s elbow dislocation with or without a concomitant fracture. BMC Musculoskelet. Disord. 2019, 20, 294. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.; Cooper, S.D.; Cha, A. Elbow dislocation with an associated lateral condyle fracture of the humerus: A rare occurrence in the pediatric population. J. Pediatr. Orthop. 2015, 35, 329–333. [Google Scholar] [CrossRef] [PubMed]
- Jevtovic-Todorovic, V.; Hartman, R.E.; Izumi, Y.; Benshoff, N.D.; Dikranian, K.; Zorumski, C.F.; Olney, J.W.; Wozniak, D.F. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J. Neurosci. 2003, 23, 876–882. [Google Scholar] [CrossRef] [PubMed]
- Paule, M.; Li, M.; Allen, R.; Liu, F.; Zou, X.; Hotchkiss, C.; Hanig, J.; Patterson, T.; Slikker, W.; Wang, C. Ketamine anesthesia during the first week of life can cause long-lasting cognitive deficits in rhesus monkeys. Neurotoxicol. Teratol. 2011, 33, 220–230. [Google Scholar] [CrossRef] [PubMed]
- Davidson, A.J.; Disma, N.; de Graaff, J.C.; Withington, D.E.; Dorris, L.; Bell, G.; Stargatt, R.; Bellinger, D.C.; Schuster, T.; Arnup, S.J.; et al. Neurodevelopmental outcome at 2 years of age after general anaesthesia and awake-regional anaesthesia in infancy (GAS): An international multicentre, randomised controlled trial. Lancet 2016, 387, 239–250, Erratum in Lancet 2016, 387, 228. [Google Scholar] [CrossRef] [PubMed]
- McCann, M.E.; de Graaff, J.C.; Dorris, L.; Disma, N.; Withington, D.; Bell, G.; Grobler, A.; Stargatt, R.; Hunt, R.W.; Sheppard, S.J.; et al. Neurodevelopmental outcome at 5 years of age after general anaesthesia or awake-regional anaesthesia in infancy (GAS): An international, multicentre, randomised, controlled equivalence trial. Lancet 2019, 393, 664–677. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.S.; Li, G.; Miller, T.L.K.; Salorio, C.; Byrne, M.W.; Bellinger, D.C.; Ing, C.; Park, R.; Radcliffe, J.; Hays, S.R.; et al. Association Between a Single General Anesthesia Exposure Before Age 36 Months and Neurocognitive Outcomes in Later Childhood. JAMA 2016, 315, 2312–2320. [Google Scholar] [CrossRef] [PubMed]
- Bjur, K.A.; Payne, E.T.; Nemergut, M.E.; Hu, D.; Flick, R.P. Anesthetic-Related Neurotoxicity and Neuroimaging in Children: A Call for Conversation. J. Child Neurol. 2017, 32, 594–602. [Google Scholar] [CrossRef] [PubMed]
- Warner, D.O.; Zaccariello, M.J.; Katusic, S.K.; Schroeder, D.R.; Hanson, A.C.; Schulte, P.J.; Buenvenida, S.L.; Gleich, S.J.; Wilder, R.T.; Sprung, J.; et al. Neuropsychological and Behavioral Outcomes after Exposure of Young Children to Procedures Requiring General Anesthesia: The Mayo Anesthesia Safety in Kids (MASK) Study. Anethesiology 2018, 129, 89–105. [Google Scholar] [CrossRef] [PubMed]
- Bartels, D.D.; McCann, M.E.; Davidson, A.J.; Polaner, D.M.; Whitlock, E.L.; Bateman, B.T. Estimating pediatric general anesthesia exposure: Quantifying duration and risk. Paediatr. Anaesth. 2018, 28, 520–527. [Google Scholar] [CrossRef] [PubMed]
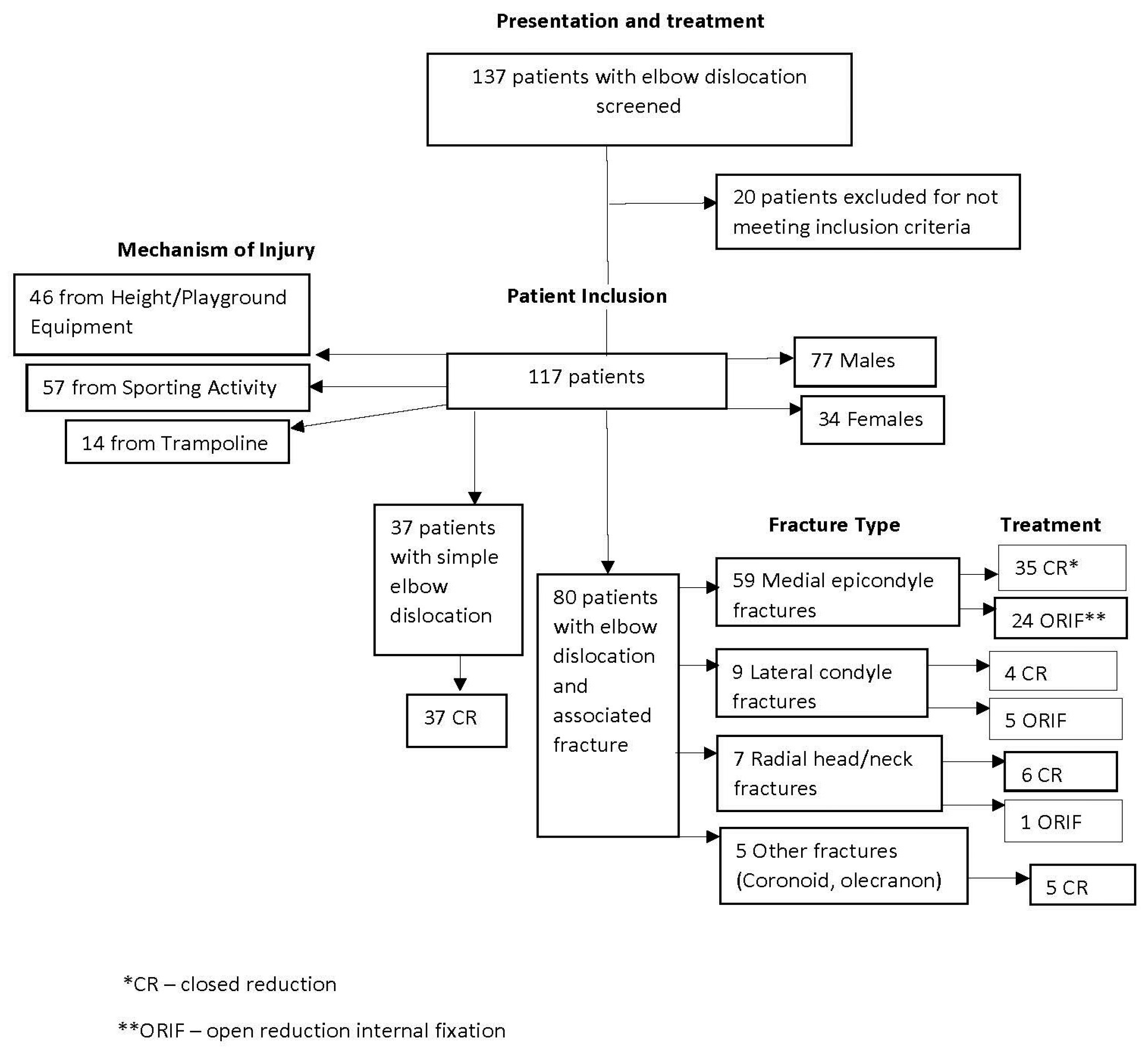

| n = 117 | ||
|---|---|---|
| Sex | Male | 73 |
| Female | 44 | |
| Mechanism of Injury | Fall from height/playground equipment | 46 |
| Sporting Activity | 57 | |
| Trampoline | 14 | |
| n | CR * Attempted? | CR * Successful? | ORIF ** | Indication for ORIF ** | |
|---|---|---|---|---|---|
| TOTAL INCLUDED | 117 | 117 | 85 | 30 | |
| Simple dislocation | 37 | 37 | 37 | 0 | |
| Associated fracture | 80 | 80 | 50 | 30 | |
| Medial epicondyle fracture | 59 | 59 | 35 | 24 (40.7%) | fracture displacement—19 (79.2%) |
| incarcerated fracture fragment—5 (20.8%) | |||||
| Lateral condyle fracture | 9 | 9 | 4 | 5 (55.6%) | fracture displacement—5 (100%) |
| Radial head/neck fracture | 7 | 7 | 6 | 1 (14.3%) | fracture displacement—1 |
| Other (coronoid, olecranon) | 5 | 5 | 5 | 0 |
| Variables | Overall | No-ORIF Group | ORIF Group | p-Value | |||
|---|---|---|---|---|---|---|---|
| n | Mean ± Std *, Med (Range) | n | Mean ± Std *, Med (Range) | n | Mean ± Std *, Med (Range) | ||
| Fracture displacement (mm) | 51 | 6.52 ± 5.28, 5.00 (0, 21.10) | 33 | 4.30 ± 3.50, 4.00 (0, 11.00) | 18 | 10.58 ± 5.66, 11.05 (1.50, 21.10) | 0.0004 |
| Fracture displacement (mm)—with medial epicondyle fracture | 47 | 6.85 ± 5.37, 6.80 (0, 21.10) | 33 | 4.30 ± 3.50, 4.00 (0, 11.00) | 14 | 12.85 ± 4.07, 12.75 (6.80, 21.10) | <0.0001 |
| Fracture displacement (mm)—with lateral condyle fracture | 4 | 2.63 ± 1.11, 2.50 (1.50, 4.00) | 0 | 4 | 2.63 ± 1.11, 2.50 (1.50, 4.00) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lewallen, L.; Elliott, M.E.; McIntosh, A.; Ho, C.A. Pediatric Elbow Dislocations and Associated Fractures. Children 2023, 10, 993. https://doi.org/10.3390/children10060993
Lewallen L, Elliott ME, McIntosh A, Ho CA. Pediatric Elbow Dislocations and Associated Fractures. Children. 2023; 10(6):993. https://doi.org/10.3390/children10060993
Chicago/Turabian StyleLewallen, Laura, Marilyn E. Elliott, Amy McIntosh, and Christine A. Ho. 2023. "Pediatric Elbow Dislocations and Associated Fractures" Children 10, no. 6: 993. https://doi.org/10.3390/children10060993
APA StyleLewallen, L., Elliott, M. E., McIntosh, A., & Ho, C. A. (2023). Pediatric Elbow Dislocations and Associated Fractures. Children, 10(6), 993. https://doi.org/10.3390/children10060993









