The Effectiveness of a Physical Literacy-Based Intervention for Increasing Physical Activity Levels and Improving Health Indicators in Overweight and Obese Adolescents (CAPACITES 64)
Abstract
1. Introduction
- −
- Develop PL among adolescents;
- −
- Increase MVPA and improve health indicators (body composition and CRF) among overweight and obese adolescents.
2. Materials and Methods
2.1. Study Design and Procedure
2.2. Participant Recruitment Process
- −
- Overweight or obese status (BMI > International Obesity Task Force (IOTF 25) cutoff) [54] and PA levels in among the lowest 25% (1st quartile) and/or CRF in the lowest 25% (first quartile);
- −
- A %BF in the highest 25% (4th quartile) and PA levels in the lowest 25% (1st quartile) and/or a CRF in the lowest 25% (first quartile);
- −
- Consent from the adolescent and his/her parents or legal guardians.
- −
- Motor, mental, cognitive, or psychic disabilities in adolescents;
- −
- An injury.
2.3. Description of the Intervention CAPACITES 64
- −
- In school;
- −
- Out-of-school (e.g., a sports gymnasium);
- −
- In adolescents’ household environments [30].
2.3.1. Specific Actions to Develop PL and Increase PA
- (a)
- For the out-of-school activities, two weekly sessions of adapted exercise were programmed every Wednesday (3:00–5:00 pm) and Friday (5:00–6:00 pm) during the whole intervention. A total of 69 sessions were made. These sessions took place in a sports gymnasium and were supervised by an adapted exercise professional. The sessions were based on an exercise plan that respected the main criteria of adaptation, respect for the load, and progression [57].
- −
- The positive influence of peers (e.g., creating a homogeneous group with similar physical characteristics);
- −
- setting short-, medium-, and long-term goals (e.g., regular review of goals);
- −
- making it possible to achieve success (e.g., adapting practice to the level of each individual);
- −
- sessions based on fun and non-structured play rather than sport competition;
- −
- positive feedback on the gain of intrinsic skills (e.g., showing the new success of an exercise).
- (b)
- At the school level, two main actions were implemented:
- (c)
- At the family and household level:
2.3.2. Specific Dietary Actions
- −
- Hands-on educational cooking workshops in the school kitchens;
- −
- Educational workshops on nutrition (similar to those on PA);
- −
- Individual consultation with the adolescent and their family based on the dietary diagnosis;
- −
- An individual follow-up on the diet of the adolescent and their family in the form of monthly exchanges (setting and reaching objectives);
- −
- Awareness-raising of the adolescent’s teachers (similar to the awareness-raising on PA).
2.4. Anthropometric Data
- −
- Underweight is characterized by a BMI < the IOTF threshold 17;
- −
- Normal weight corresponds to a BMI between the IOTF 17 and 25 thresholds;
- −
- Being overweight corresponds to a BMI between the IOTF of 25 and 30;
- −
- Obesity corresponds to a BMI > the IOTF 30 threshold and severe obesity to a BMI > the IOTF 35 threshold.
2.5. Body Composition Measurement
2.6. Measurement of CRF by the 20 m Shuttle Walk/Run Test (TMNA-20)
2.7. Measurement of PA Levels
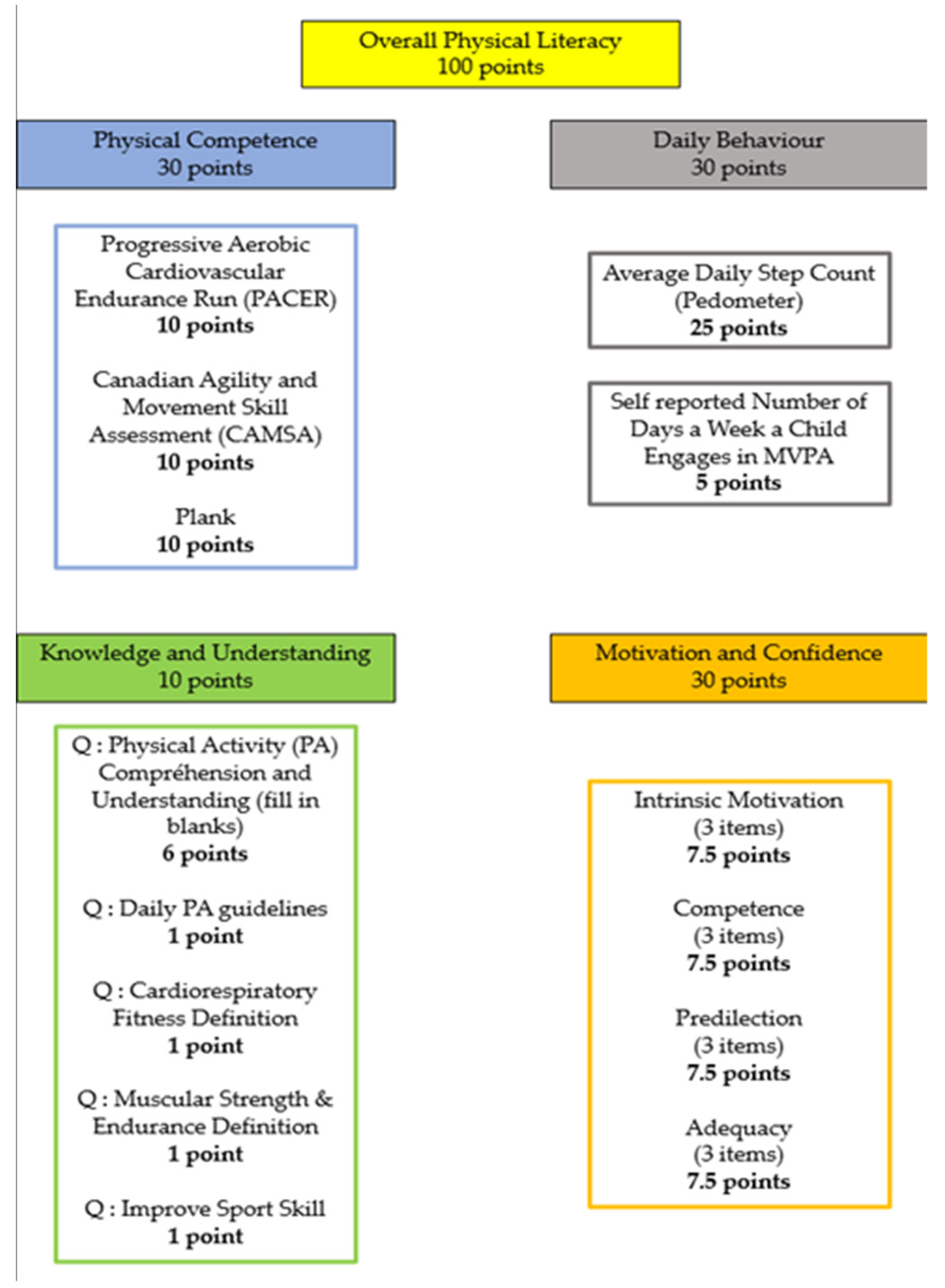
2.8. Measurement of PL
2.9. Statistical Analysis
3. Results
3.1. Baseline Results (T0) and Impact of the Intervention at 9 Months on the Group of Adolescents (T1)
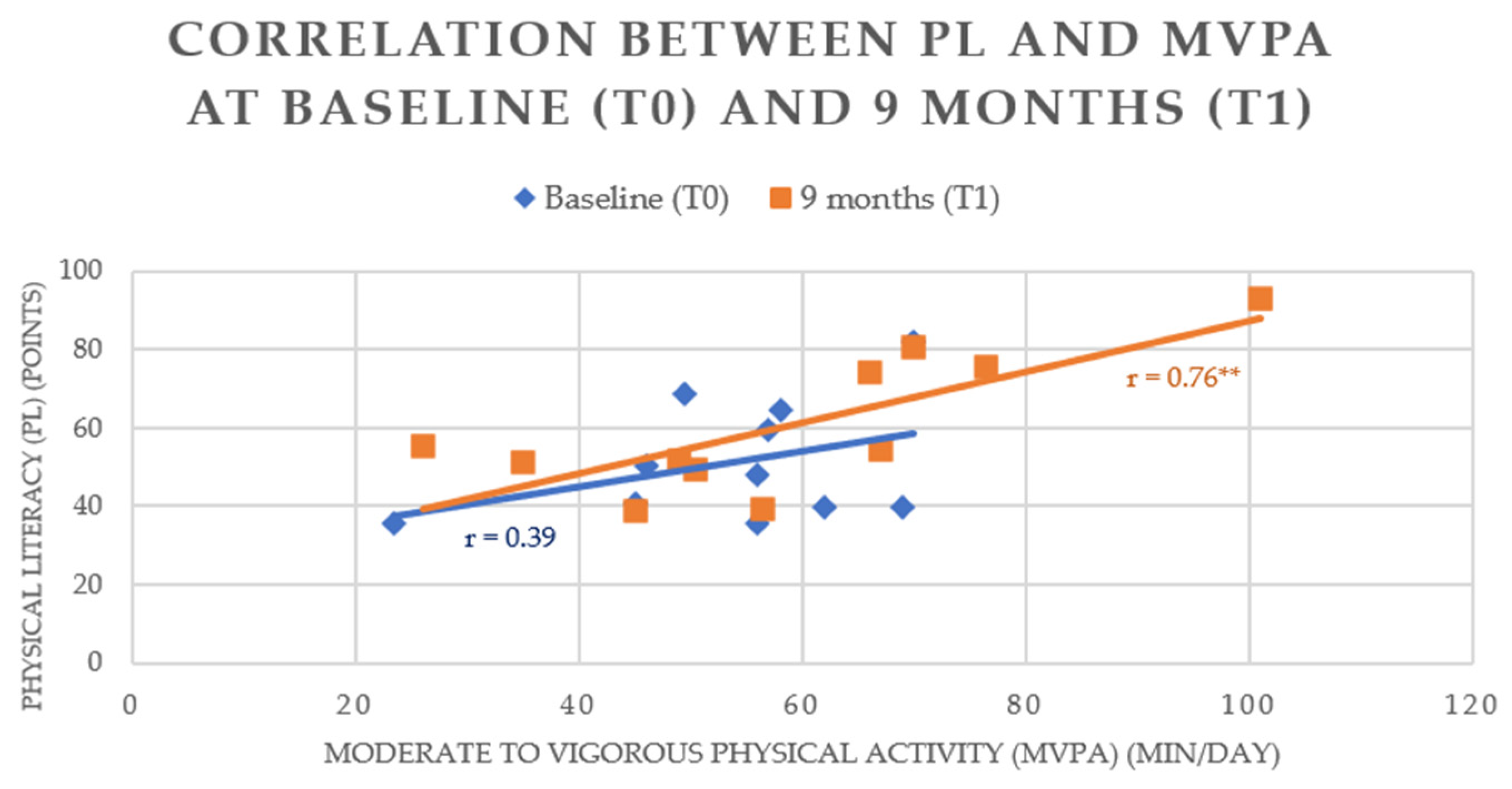
3.2. Correlation Matrix between Variables at T0 and T1
4. Discussion
4.1. Development of PL
4.2. Effect of PL Development on Body Composition and Anthropometric Data
4.3. Effect of PL Development on CRF
4.4. Effect of PL Development on MVPA
4.5. Correlation between PL and MVPA
4.6. Strengths and Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fleary, S.A.; Joseph, P.; Pappagianopoulos, J.E. Adolescent Health Literacy and Health Behaviors: A Systematic Review. J. Adolesc. 2018, 62, 116–127. [Google Scholar] [CrossRef]
- Varma, V.R.; Dey, D.; Leroux, A.; Di, J.; Urbanek, J.; Xiao, L.; Zipunnikov, V. Re-Evaluating the Effect of Age on Physical Activity over the Lifespan. Prev. Med. 2017, 101, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Mijalković, S.; Stanković, D.; Tomljanović, M.; Batez, M.; Grle, M.; Grle, I.; Brkljačić, I.; Jularić, J.; Sporiš, G.; Fišer, S.Ž. School-Based Exercise Programs for Promoting Cardiorespiratory Fitness in Overweight and Obese Children Aged 6 to 10. Children 2022, 9, 1323. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.F.; Bustamante, E.E.; Waller, J.L.; Davis, C.L. Exercise Effects on Quality of Life, Mood, and Self-Worth in Overweight Children: The SMART Randomized Controlled Trial. Transl. Behav. Med. 2019, 9, 451–459. [Google Scholar] [CrossRef]
- de Greeff, J.W.; Bosker, R.J.; Oosterlaan, J.; Visscher, C.; Hartman, E. Effects of Physical Activity on Executive Functions, Attention and Academic Performance in Preadolescent Children: A Meta-Analysis. J. Sci. Med. Sport 2018, 21, 501–507. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Global Trends in Insufficient Physical Activity among Adolescents: A Pooled Analysis of 298 Population-Based Surveys with 1·6 Million Participants. Lancet Child. Adolesc. Health 2020, 4, 23–35. [Google Scholar] [CrossRef] [PubMed]
- Carson, V.; Hunter, S.; Kuzik, N.; Gray, C.E.; Poitras, V.J.; Chaput, J.-P.; Saunders, T.J.; Katzmarzyk, P.T.; Okely, A.D.; Connor Gorber, S.; et al. Systematic Review of Sedentary Behaviour and Health Indicators in School-Aged Children and Youth: An Update. Appl. Physiol. Nutr. Metab. 2016, 41, S240–S265. [Google Scholar] [CrossRef]
- Faigenbaum, A.D.; MacDonald, J.P.; Stracciolini, A.; Rebullido, T.R. Making a Strong Case for Prioritizing Muscular Fitness in Youth Physical Activity Guidelines. Curr. Sport. Med. Rep. 2020, 19, 530–536. [Google Scholar] [CrossRef]
- WHO. WHO European Regional Obesity: Report 2022; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 2022; ISBN 978-92-890-5773-8. [Google Scholar]
- Larqué, E.; Labayen, I.; Flodmark, C.-E.; Lissau, I.; Czernin, S.; Moreno, L.A.; Pietrobelli, A.; Widhalm, K. From Conception to Infancy—Early Risk Factors for Childhood Obesity. Nat. Rev. Endocrinol. 2019, 15, 456–478. [Google Scholar] [CrossRef]
- Ang, Y.N.; Wee, B.S.; Poh, B.K.; Ismail, M.N. Multifactorial Influences of Childhood Obesity. Curr. Obes. Rep. 2013, 2, 10–22. [Google Scholar] [CrossRef]
- Poitras, V.J.; Gray, C.E.; Borghese, M.M.; Carson, V.; Chaput, J.-P.; Janssen, I.; Katzmarzyk, P.T.; Pate, R.R.; Connor Gorber, S.; Kho, M.E.; et al. Systematic Review of the Relationships between Objectively Measured Physical Activity and Health Indicators in School-Aged Children and Youth. Appl. Physiol. Nutr. Metab. 2016, 41, S197–S239. [Google Scholar] [CrossRef]
- Raistenskis, J.; Sidlauskiene, A.; Strukcinskiene, B.; Baysal, S.U.; Buckus, R. Physical Activity and Physical Fitness in Obese, Overweight, and Normal-Weight Children. Turk. J. Med. Sci. 2016, 46, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Vicencio, S.; Coudeyre, E.; Kluka, V.; Cardenoux, C.; Jegu, A.-G.; Fourot, A.-V.; Ratel, S.; Martin, V. The Bigger, the Stronger? Insights from Muscle Architecture and Nervous Characteristics in Obese Adolescent Girls. Int. J. Obes. 2015, 40, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.K.; Sim, Y.K.; Lee, J.-H.; Yook, J.S.; Ha, S.-M.; Seo, E.C.; So, W.-Y.; Kim, H.R.; Jeong, W.-M.; Goo, B.O.; et al. The Relationship between Body Composition and Physical Fitness and the Effect of Exercise According to the Level of Childhood Obesity Using the MGPA Model. Int. J. Environ. Res. Public Health 2022, 19, 487. [Google Scholar] [CrossRef] [PubMed]
- Mendelson, M.; Michallet, A.-S.; Estève, F.; Perrin, C.; Levy, P.; Wuyam, B.; Flore, P. Ventilatory Responses to Exercise Training in Obese Adolescents. Respir. Physiol. Neurobiol. 2012, 184, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Vega-Ramirez, L.; Pérez-Cañaveras, R.M.; De Juan Herrero, J. There Is an Inverse Correlation between Basic Motor Skills and Overweight in Schoolchildren Aged 8 to 12. Children 2021, 8, 1198. [Google Scholar] [CrossRef]
- Gilic, B.; Malovic, P.; Sunda, M.; Maras, N.; Zenic, N. Adolescents with Higher Cognitive and Affective Domains of Physical Literacy Possess Better Physical Fitness: The Importance of Developing the Concept of Physical Literacy in High Schools. Children 2022, 9, 796. [Google Scholar] [CrossRef]
- Mendoza-Muñoz, M.; Barrios-Fernández, S.; Adsuar, J.C.; Pastor-Cisneros, R.; Risco-Gil, M.; García-Gordillo, M.Á.; Carlos-Vivas, J. Influence of Body Composition on Physical Literacy in Spanish Children. Biology 2021, 10, 482. [Google Scholar] [CrossRef]
- Power, T.G.; Ullrich-French, S.C.; Steele, M.M.; Daratha, K.B.; Bindler, R.C. Obesity, Cardiovascular Fitness, and Physically Active Adolescents’ Motivations for Activity: A Self-Determination Theory Approach. Psychol. Sport. Exerc. 2011, 12, 593–598. [Google Scholar] [CrossRef]
- Tully, L.; Arthurs, N.; Wyse, C.; Browne, S.; Case, L.; McCrea, L.; O’Connell, J.M.; O’Gorman, C.S.; Smith, S.M.; Walsh, A.; et al. Guidelines for Treating Child and Adolescent Obesity: A Systematic Review. Front. Nutr. 2022, 9, 902865. [Google Scholar] [CrossRef]
- Cesa, C.C.; Molino, G.O.G.; Lima, J.; Pereira, R.B.; Eibel, B.; Barbiero, S.M.; Schaan, B.D.; Pellanda, L.C. Physical Activity and Cardiovascular Risk Factors in Children: A Meta-Analysis Update. Int. J. Cardiovasc. Sci. 2021, 35, 304–315. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Ramírez-Campillo, R.; Izquierdo, M. Is Muscular Fitness Associated with Future Health Benefits in Children and Adolescents? A Systematic Review and Meta-Analysis of Longitudinal Studies. Sports Med. 2019, 49, 1079–1094. [Google Scholar] [CrossRef]
- O’Malley, G.; Thivel, D. Physical Activity and Play in Children Who Are Obese; European Childhood Obesity Group: Bruxelles, Belgium, 2015; p. 20. [Google Scholar]
- Kornet-van der Aa, D.A.; Altenburg, T.M.; van Randeraad-van der Zee, C.H.; Chinapaw, M.J.M. The Effectiveness and Promising Strategies of Obesity Prevention and Treatment Programmes among Adolescents from Disadvantaged Backgrounds: A Systematic Review: Preventing and Treating Adolescent Obesity. Obes. Rev. 2017, 18, 581–593. [Google Scholar] [CrossRef] [PubMed]
- Mead, E.; Brown, T.; Rees, K.; Azevedo, L.B.; Whittaker, V.; Jones, D.; Olajide, J.; Mainardi, G.M.; Corpeleijn, E.; O’Malley, C.; et al. Diet, Physical Activity and Behavioural Interventions for the Treatment of Overweight or Obese Children from the Age of 6 to 11 Years. Cochrane Database Syst. Rev. 2017, 2017, CD012651. [Google Scholar] [CrossRef]
- Psaltopoulou, T.; Tzanninis, S.; Ntanasis-Stathopoulos, I.; Panotopoulos, G.; Kostopoulou, M.; Tzanninis, I.-G.; Tsagianni, A.; Sergentanis, T.N. Prevention and Treatment of Childhood and Adolescent Obesity: A Systematic Review of Meta-Analyses. World J. Pediatr. 2019, 15, 350–381. [Google Scholar] [CrossRef] [PubMed]
- Bauman, A.E.; Reis, R.S.; Sallis, J.F.; Wells, J.C.; Loos, R.J.; Martin, B.W. Correlates of Physical Activity: Why Are Some People Physically Active and Others Not? Lancet 2012, 380, 258–271. [Google Scholar] [CrossRef]
- Brandes, B.; Busse, H.; Sell, L.; Christianson, L.; Brandes, M. A Scoping Review on Characteristics of School-Based Interventions to Promote Physical Activity and Cardiorespiratory Fitness among 6- to 10-Year-Old Children. Prev. Med. 2022, 155, 106920. [Google Scholar] [CrossRef]
- Simon, C.; Kellou, N.; Dugas, J.; Platat, C.; Copin, N.; Schweitzer, B.; Hausser, F.; Bergouignan, A.; Lefai, E.; Blanc, S. A Socio-Ecological Approach Promoting Physical Activity and Limiting Sedentary Behavior in Adolescence Showed Weight Benefits Maintained 2.5 Years after Intervention Cessation. Int. J. Obes. 2014, 38, 936–943. [Google Scholar] [CrossRef]
- Foster, C.; Moore, J.B.; Singletary, C.R.; Skelton, J.A. Physical Activity and Family-based Obesity Treatment: A Review of Expert Recommendations on Physical Activity in Youth. Clin. Obes. 2018, 8, 68–79. [Google Scholar] [CrossRef]
- Hatfield, D.P.; Chomitz, V.R.; Chui, K.K.H.; Sacheck, J.M.; Brown, A.A.; Economos, C.D. Impact of a Community-Based Physical Activity Program on Fitness and Adiposity Among Overweight and Obese Children. Health Promot. Pract. 2017, 18, 75–83. [Google Scholar] [CrossRef]
- Ash, T.; Agaronov, A.; Young, T.; Aftosmes-Tobio, A.; Davison, K.K. Family-Based Childhood Obesity Prevention Interventions: A Systematic Review and Quantitative Content Analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 113. [Google Scholar] [CrossRef] [PubMed]
- Lambrinou, C.-P.; Androutsos, O.; Karaglani, E.; Cardon, G.; Huys, N.; Wikström, K.; Kivelä, J.; Ko, W.; Karuranga, E.; Tsochev, K.; et al. Effective Strategies for Childhood Obesity Prevention via School Based, Family Involved Interventions: A Critical Review for the Development of the Feel4Diabetes-Study School Based Component. BMC Endocr. Disord. 2020, 20, 52. [Google Scholar] [CrossRef] [PubMed]
- Nathan, N.; Hall, A.; McCarthy, N.; Sutherland, R.; Wiggers, J.; Bauman, A.E.; Rissel, C.; Naylor, P.-J.; Cradock, A.; Lane, C.; et al. Multi-Strategy Intervention Increases School Implementation and Maintenance of a Mandatory Physical Activity Policy: Outcomes of a Cluster Randomised Controlled Trial. Br. J. Sport. Med. 2022, 56, 385–393. [Google Scholar] [CrossRef]
- Nooijen, C.F.J.; Galanti, M.R.; Engström, K.; Möller, J.; Forsell, Y. Effectiveness of Interventions on Physical Activity in Overweight or Obese Children: A Systematic Review and Meta-Analysis Including Studies with Objectively Measured Outcomes: Physical Activity Interventions. Obes. Rev. 2017, 18, 195–213. [Google Scholar] [CrossRef]
- Whitehead, M. The Concept of Physical Literacy. Eur. J. Phys. Educ. 2001, 6, 127–138. [Google Scholar] [CrossRef]
- Whitehead, M. Physical Literacy and Physical Education: Conceptual Mapping. Phys. Educ. Matters 2006, 1, 6–9. [Google Scholar]
- Cairney, J.; Dudley, D.; Kwan, M.; Bulten, R.; Kriellaars, D. Physical Literacy, Physical Activity and Health: Toward an Evidence-Informed Conceptual Model. Sports Med. 2019, 49, 371–383. [Google Scholar] [CrossRef]
- Edwards, L.C.; Bryant, A.S.; Keegan, R.J.; Morgan, K.; Jones, A.M. Definitions, Foundations and Associations of Physical Literacy: A Systematic Review. Sports Med. 2017, 47, 113–126. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Park, J.; Kim, J.-E.; Kang, D.; Cho, S.; Chung, I.-J.; Shin, A.; Lee, M.; Choi, J.-Y. Socioecological Approach for Identifying the Determinants of Objectively Measured Physical Activity: A Prospective Study of the UK Biobank. Prev. Med. 2022, 155, 106949. [Google Scholar] [CrossRef]
- Ma, R.-S.; Sum, R.K.-W.; Li, M.-H.; Huang, Y.; Niu, X.-L. Association between Physical Literacy and Physical Activity: A Multilevel Analysis Study among Chinese Undergraduates. Int. J. Environ. Res. Public Health 2020, 17, 7874. [Google Scholar] [CrossRef]
- Belanger, K.; Barnes, J.D.; Longmuir, P.E.; Anderson, K.D.; Bruner, B.; Copeland, J.L.; Gregg, M.J.; Hall, N.; Kolen, A.M.; Lane, K.N.; et al. The Relationship between Physical Literacy Scores and Adherence to Canadian Physical Activity and Sedentary Behaviour Guidelines. BMC Public. Health 2018, 18, 1042. [Google Scholar] [CrossRef] [PubMed]
- Lang, J.J.; Chaput, J.-P.; Longmuir, P.E.; Barnes, J.D.; Belanger, K.; Tomkinson, G.R.; Anderson, K.D.; Bruner, B.; Copeland, J.L.; Gregg, M.J.; et al. Cardiorespiratory Fitness Is Associated with Physical Literacy in a Large Sample of Canadian Children Aged 8 to 12 Years. BMC Public Health 2018, 18, 1041. [Google Scholar] [CrossRef]
- Caldwell, H.A.T.; Di Cristofaro, N.A.; Cairney, J.; Bray, S.R.; MacDonald, M.J.; Timmons, B.W. Physical Literacy, Physical Activity, and Health Indicators in School-Age Children. Int. J. Environ. Res. Public Health 2020, 17, 5367. [Google Scholar] [CrossRef] [PubMed]
- Kozera, T.R. Physical Literacy in Children and Youth. Ph.D. Thesis, University of Manitoba, Winnipeg, MB, Canada, 2017. [Google Scholar]
- Carl, J.; Barratt, J.; Töpfer, C.; Cairney, J.; Pfeifer, K. The Effectiveness of Physical Literacy Interventions: A Systematic Review with Meta-Analysis. Sport Med 2022, 52, 2965–2999. [Google Scholar] [CrossRef] [PubMed]
- Coyne, P.; Vandenborn, E.; Santarossa, S.; Milne, M.M.; Milne, K.J.; Woodruff, S.J. Physical Literacy Improves with the Run Jump Throw Wheel Program among Students in Grades 4-6 in Southwestern Ontario. Appl. Physiol. Nutr. Metab. 2019, 44, 645–649. [Google Scholar] [CrossRef]
- Kwan, M.Y.W.; Li, Y.-C.; Cairney, J. Theory-Based Correlates of Physical Activity Among Children with Developmental Coordination Disorder: A Scoping Review. Curr. Dev. Disord. Rep. 2022, 9, 105–109. [Google Scholar] [CrossRef]
- Paponetti, M.K.; Zwolski, C.; Porter, R.; Paterno, M.V. Leveraging the Construct of Physical Literacy to Promote Physical Activity for Youth with Obesity—A Qualitative Analysis of Physical Therapists’ Perceptions. Obes. Pillars 2023, 5, 100054. [Google Scholar] [CrossRef]
- Nezondet, C.; Gandrieau, J.; Nguyen, P.; Zunquin, G. Perceived Physical Literacy Is Associated with Cardiorespiratory Fitness, Body Composition and Physical Activity Levels in Secondary School Students. Children 2023, 10, 712. [Google Scholar] [CrossRef]
- Quinart, S. Validation d’outils Adaptés pour L’évaluation de L’endurance Cardiorespiratoire chez L’adolescent Obèse. Ph.D. Thesis, Universite de Franche-Comte, Besançon, France, 2015. [Google Scholar]
- Guedes, D.P.; Lopes, C.C. Validação da versão brasileira do Youth Risk Behavior Survey 2007. Rev. Saúde Pública 2010, 44, 840–850. [Google Scholar] [CrossRef]
- Cole, T.J.; Lobstein, T. Extended International (IOTF) Body Mass Index Cut-Offs for Thinness, Overweight and Obesity: Extended International BMI Cut-Offs. Pediatric Obesity 2012, 7, 284–294. [Google Scholar] [CrossRef]
- Haute Autorité de Santé. Guide du Parcours de Soins: Surpoids et Obésité de L’enfant et de L’adolescent(e); HAS: Saint-Denis, France, 2022; p. 151. [Google Scholar]
- Higgs, C.; Cairney, J.; Jurbala, P.; Dudley, D.; Way, R.; Mitchell, D.; Grove, J.; Verbeek, M.; Carey, A.; Ross-McManus, H.; et al. Développer La Littératie Physique; Sport pour la vie: Fort St John, BC, Canada, 2019; p. 108. [Google Scholar]
- Liguori, G. ACSM’s Guidelines for Exercise Testing and Prescription, 11th ed.; Wolters Kluwer Santé: Sydney, Australia, 2022; ISBN 978-1-975150-18-1. [Google Scholar]
- Stearns, J.; Wohlers, B.; Mchugh, T.-L.; Kuzik, N.; Spence, J. Reliability and Validity of the PLAY Fun Tool with Children and Youth in Northern Canada. Meas. Phys. Educ. Exerc. Sci. 2018, 23, 1–11. [Google Scholar] [CrossRef]
- Borg, G.A. Psychophysical Bases of Perceived Exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Howlett, N.; Trivedi, D.; Troop, N.A.; Chater, A.M. Are Physical Activity Interventions for Healthy Inactive Adults Effective in Promoting Behavior Change and Maintenance, and Which Behavior Change Techniques Are Effective? A Systematic Review and Meta-Analysis. Transl. Behav. Med. 2019, 9, 147–157. [Google Scholar] [CrossRef]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically Clustered Techniques: Building an International Consensus for the Reporting of Behavior Change Interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef] [PubMed]
- James, J.; Kerr, D. Prevention of Childhood Obesity by Reducing Soft Drinks. Int. J. Obes. 2005, 29, S54–S57. [Google Scholar] [CrossRef] [PubMed]
- Neri, D.; Steele, E.M.; Khandpur, N.; Cediel, G.; Zapata, M.E.; Rauber, F.; Marrón-Ponce, J.A.; Machado, P.; Costa Louzada, M.L.; Andrade, G.C.; et al. Ultraprocessed Food Consumption and Dietary Nutrient Profiles Associated with Obesity: A Multicountry Study of Children and Adolescents. Obes. Rev. 2022, 23. [Google Scholar] [CrossRef]
- Hoelscher, D.M.; Brann, L.S.; O’Brien, S.; Handu, D.; Rozga, M. Prevention of Pediatric Overweight and Obesity: Position of the Academy of Nutrition and Dietetics Based on an Umbrella Review of Systematic Reviews. J. Acad. Nutr. Diet. 2022, 122, 410–423.e6. [Google Scholar] [CrossRef]
- Léger, L.A.; Mercier, D.; Gadoury, C.; Lambert, J. The Multistage 20 Metre Shuttle Run Test for Aerobic Fitness. J. Sport. Sci. 1988, 6, 93–101. [Google Scholar] [CrossRef]
- Kwon, S.; Menezes, A.M.B.; Ekelund, U.; Wehrmeister, F.C.; Gonçalves, H.; da Silva, B.G.C.; Janz, K.F. Longitudinal Change in Physical Activity and Adiposity in the Transition from Adolescence to Early Adulthood: The 1993 Pelotas Cohort Study. Int. J. Behav. Nutr. Phys. Act. 2022, 19, 83. [Google Scholar] [CrossRef]
- Romanzini, M.; Petroski, E.L.; Ohara, D.; Dourado, A.C.; Reichert, F.F. Calibration of ActiGraph GT3X, Actical and RT3 Accelerometers in Adolescents. Eur. J. Sport. Sci. 2014, 14, 91–99. [Google Scholar] [CrossRef]
- Troiano, R.P. Large-Scale Applications of Accelerometers: New Frontiers and New Questions. Med. Sci. Sport. Exerc. 2007, 39, 1501. [Google Scholar] [CrossRef]
- Rich, C.; Geraci, M.; Griffiths, L.; Sera, F.; Dezateux, C.; Cortina-Borja, M. Quality Control Methods in Accelerometer Data Processing: Defining Minimum Wear Time. PLoS ONE 2013, 8, e67206. [Google Scholar] [CrossRef]
- Evenson, K.R.; Catellier, D.J.; Gill, K.; Ondrak, K.S.; McMurray, R.G. Calibration of Two Objective Measures of Physical Activity for Children. J. Sport. Sci. 2008, 26, 1557–1565. [Google Scholar] [CrossRef]
- Longmuir, P.E.; Gunnell, K.E.; Barnes, J.D.; Belanger, K.; Leduc, G.; Woodruff, S.J.; Tremblay, M.S. Canadian Assessment of Physical Literacy Second Edition: A Streamlined Assessment of the Capacity for Physical Activity among Children 8 to 12 Years of Age. BMC Public Health 2018, 18, 1047. [Google Scholar] [CrossRef] [PubMed]
- Soare, R.; Brasil, I.; Monteiro, W.; Farinatti, P. Effects of Physical Activity on Body Mass and Composition of School-Age Children and Adolescents with Overweight or Obesity: Systematic Review Focusing on Intervention Characteristics. J. Bodyw. Mov. Ther. 2022, 33, 154–163. [Google Scholar] [CrossRef] [PubMed]
- Carl, J.; Barratt, J.; Töpfer, C.; Cairney, J.; Pfeifer, K. How Are Physical Literacy Interventions Conceptualized? – A Systematic Review on Intervention Design and Content. Psychol. Sport Exerc. 2022, 58, 102091. [Google Scholar] [CrossRef]
- Li, M.H.; Kaioglou, V.; Ma, R.S.; Choi, S.M.; Venetsanou, F.; Sum, R.K.W. Exploring Physical Literacy in Children Aged 8 to 12 Years Old: A Cross-Cultural Comparison between China and Greece. BMC Public Health 2022, 22, 2102. [Google Scholar] [CrossRef] [PubMed]
- Chung, Y.L.; Rhie, Y.-J. Severe Obesity in Children and Adolescents: Metabolic Effects, Assessment, and Treatment. J. Obes. Metab. Syndr. 2021, 30, 326–335. [Google Scholar] [CrossRef]
- Ogden, C.L.; Li, Y.; Freedman, D.S.; Borrud, L.G.; Flegal, K.M. Smoothed Percentage Body Fat Percentiles for U.S. Children and Adolescents, 1999–2004. Natl. Health Stat. Rep. 2011, 43, 1–7. [Google Scholar]
- Guerra, P.H.; Nobre, M.R.C.; da Silveira, J.A.C.; de Aguiar Carrazedo Taddei, J.A. The Effect of School-Based Physical Activity Interventions on Body Mass Index: A Meta-Analysis of Randomized Trials. Clinics 2013, 68, 1263–1273. [Google Scholar] [CrossRef]
- Stoner, L.; Pontzer, H.; Barone Gibbs, B.; Moore, J.B.; Castro, N.; Skidmore, P.; Lark, S.; Williams, M.A.; Hamlin, M.J.; Faulkner, J. Fitness and Fatness Are Both Associated with Cardiometabolic Risk in Preadolescents. J. Pediatr. 2020, 217, 39–45.e1. [Google Scholar] [CrossRef]
- Brand, C.; Sehn, A.P.; Fochesatto, C.F.; de Castro Silveira, J.F.; Mota, J.; Gomez, D.M.; Gaya, A.R.; Reuter, C.P.; Renner, J.D.P. Body Fat Percentage, Cardiorespiratory Fitness and Arterial Blood Pressure in Children and Adolescents: A Longitudinal Analysis. BMC Cardiovasc. Disord. 2022, 22, 267. [Google Scholar] [CrossRef]
- Lätt, E.; Mäestu, J.; Rääsk, T.; Jürimäe, T.; Jürimäe, J. Cardiovascular Fitness, Physical Activity, and Metabolic Syndrome Risk Factors among Adolescent Estonian Boys: A Longitudinal Study. Am. J. Hum. Biol. 2016, 28, 782–788. [Google Scholar] [CrossRef]
- Telford, R.M.; Olive, L.S.; Keegan, R.J.; Keegan, S.; Barnett, L.M.; Telford, R.D. Student Outcomes of the Physical Education and Physical Literacy (PEPL) Approach: A Pragmatic Cluster Randomised Controlled Trial of a Multicomponent Intervention to Improve Physical Literacy in Primary Schools. Phys. Educ. Sport. Pedagog. 2021, 26, 97–110. [Google Scholar] [CrossRef]
- Cain, K.L.; Sallis, J.F.; Conway, T.L.; Van Dyck, D.; Calhoon, L. Using Accelerometers in Youth Physical Activity Studies: A Review of Methods. J. Phys. Act. Health 2013, 10, 437–450. [Google Scholar] [CrossRef] [PubMed]
- Currie, C.; Zanotti, C.; Morgan, A.; Currie, D.; de Looze, M.; Roberts, C.; Samdal, O.; Smith, O.R.; Barnekow, V. Social Determinants of Health and Well-Being among Young People: Health Behaviour in School-Aged Children (HBSC) Study: International Report from the 2009/2010 Survey; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 2012; ISBN 978-92-890-1423-6. [Google Scholar]
- Belton, S.; McCarren, A.; McGrane, B.; Powell, D.; Issartel, J. The Youth-Physical Activity Towards Health (Y-PATH) Intervention: Results of a 24 Month Cluster Randomised Controlled Trial. PLoS ONE 2019, 14, e0221684. [Google Scholar] [CrossRef] [PubMed]
- Vermeiren, E.; Bruyndonckx, L.; De Winter, B.; Verhulst, S.; Van Eyck, A.; Van Hoorenbeeck, K. The Effect of Weight Regain on Cardiometabolic Health in Children with Obesity: A Systematic Review of Clinical Studies. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2575–2586. [Google Scholar] [CrossRef]
- Delisle Nyström, C.; Traversy, G.; Barnes, J.D.; Chaput, J.-P.; Longmuir, P.E.; Tremblay, M.S. Associations between Domains of Physical Literacy by Weight Status in 8-to 12-Year-Old Canadian Children. BMC Public. Health 2018, 18, 1043. [Google Scholar] [CrossRef] [PubMed]
- Martins, J.; Costa, J.; Sarmento, H.; Marques, A.; Farias, C.; Onofre, M.; Valeiro, M.G. Adolescents’ Perspectives on the Barriers and Facilitators of Physical Activity: An Updated Systematic Review of Qualitative Studies. Int. J. Env. Res. Public. Health 2021, 18, 4954. [Google Scholar] [CrossRef] [PubMed]
- Yen, C.-F.; Hsiao, R.C.; Ko, C.-H.; Yen, J.-Y.; Huang, C.-F.; Liu, S.-C.; Wang, S.-Y. The Relationships between Body Mass Index and Television Viewing, Internet Use and Cellular Phone Use: The Moderating Effects of Socio-Demographic Characteristics and Exercise. Int. J. Eat. Disord. 2010, 43, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Verney, J.; Metz, L.; Chaplais, E.; Cardenoux, C.; Pereira, B.; Thivel, D. Bioelectrical Impedance Is an Accurate Method to Assess Body Composition in Obese but Not Severely Obese Adolescents. Nutr. Res. 2016, 36, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Kuruvilla, S.; Bustreo, F.; Kuo, T.; Mishra, C.; Taylor, K.; Fogstad, H.; Gupta, G.R.; Gilmore, K.; Temmerman, M.; Thomas, J.; et al. The Global Strategy for Women’s, Children’s and Adolescents’ Health (2016–2030): A Roadmap Based on Evidence and Country Experience. Bull. World Health Organ. 2016, 94, 398–400. [Google Scholar] [CrossRef] [PubMed]
- Malina, R.M.; Beunen, G.; Lefevre, J.; Woynarowska, B. Maturity-Associated Variation in Peak Oxygen Uptake in Active Adolescent Boys and Girls. Ann. Hum. Biol. 1997, 24, 19–31. [Google Scholar] [CrossRef] [PubMed]

| Age | Type | Time | Benefits |
|---|---|---|---|
| 5 to 17 years old |
|
|
|
| Organization of a Adapted Exercise Session | |
|---|---|
| Warm-up | Modalities: Time: 5 to 10 min—intensity between 50 and 70% maximum Heart Rate (HR max) Construction: 100% in the form of games with intensity progression (from 50% to 70% HRmax). Guidance according to work in the body of the session (aerobic, muscular…) |
| Session | Modalities: Time: 40 to 50 min—Intensity: between 50 and 90% HR max. Principle of intermittent exercise with high periods at 90% HRmax and low periods at 50% HRmax. The work at the target HR zones is controlled with a heart rate monitor. Construction:
|
| Rest | Modalities: 5 to 10 min Construction: Time for exchange on the session: perception, feelings, and transmission of information |
| Characteristics (n = 13) | Baseline (T0) | Post Intervention 9 Months (T1) | Gross Difference | Difference in % | p-Value (p ≤ 0.05) |
|---|---|---|---|---|---|
| BMI (kg/m²) | 26.4 (±5.5) | 25.5 (±5.1) | −0.9 (±1.5) | 96.7 | 0.07 |
| BMI z score | 2.0 (±0.8) | 1.7 (±0.9) | −0.3 (±0.3) | 83.6 | ≤0.01 ** |
| SMM (%) | 39.5 (±4.9) | 41.7 (±4.4) | 2.2 (±2.8) | 105.4 | ≤0.01 ** |
| BF (%) | 30.1 (±8.7) | 26.3 (±7.8) | −3.8 (±4.9) | 87.4 | ≤0.01 ** |
| Vmax (km/h) | 8.7 (±1.5) | 9.2 (±1.6) | 0.5 (±0.7) | 105.7 | 0.03 * |
| VO2peak (mL·min·kg−1) | 30.9 (±4.4) | 32.4 (±4.6) | 1.5 (±1.7) | 104.8 | ≤0.01 ** |
| MVPA (min/day) | 53.8 (±12.9) | 58.4 (20.8) | 4.6 (±13.7) | 108.5 | 0.4 |
| PL (CAPL-2) | |||||
| Total score PL | 51.5 (±14.1) | 59.8 (±18.2) | 8.3 (±9.3) | 116.2 | ≤0.01 ** |
| Score in the «physical competence» | 11.7 (±7.9) | 15.9 (±7.8) | 4.1 (±4.1) | 135.5 | ≤0.01 ** |
| Score in the «daily behavior» | 11.9 (±5.0) | 12.9 (±7.0) | 1.0 (±5.9) | 112.8 | 0.5 |
| Score in the «knowledge and understanding» | 5.6 (±2.0) | 8.2 (±1.9) | 2.5 (±2.3) | 145.0 | ≤0.01 * |
| Score in the «motivation and confidence» | 22.2 (±4.8) | 22.9 (±4.6) | 0.7 (±3.8) | 102.9 | 0.7 |
| Baseline T0 | PL | MVPA | VO2peak | %BF | %SMM |
|---|---|---|---|---|---|
| PL (points) | 0.39 | 0.83 ** | −0.41 | 0.41 | |
| MVPA (min/day) | 0.39 | 0.31 | −0.16 | 0.16 | |
| VO2peak (mL·min·kg−1) | 0.83 ** | 0.31 | −0.72 * | 0.72 * | |
| %BF | −0.41 | −0.16 | −0.72 * | −0.99 ** | |
| %SMM | 0.41 | 0.16 | 0.72 * | −0.99 ** | |
| T1 | PL | MVPA | VO2pic | %BF | %SMM |
| PL (points) | 0.76 ** | 0.91 ** | −0.37 | 0.37 | |
| MVPA (min/day) | 0.76 ** | 0.81 ** | −0.33 | 0.33 | |
| VO2peak (mL·min·kg−1) | 0.91 ** | 0.81 ** | −0.61 * | 0.61 * | |
| %BF | −0.37 | −0.33 | −0.61 * | −1.00 ** | |
| %SMM | 0.37 | 0.33 | 0.61 * | −1.00 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nezondet, C.; Gandrieau, J.; Bourrelier, J.; Nguyen, P.; Zunquin, G. The Effectiveness of a Physical Literacy-Based Intervention for Increasing Physical Activity Levels and Improving Health Indicators in Overweight and Obese Adolescents (CAPACITES 64). Children 2023, 10, 956. https://doi.org/10.3390/children10060956
Nezondet C, Gandrieau J, Bourrelier J, Nguyen P, Zunquin G. The Effectiveness of a Physical Literacy-Based Intervention for Increasing Physical Activity Levels and Improving Health Indicators in Overweight and Obese Adolescents (CAPACITES 64). Children. 2023; 10(6):956. https://doi.org/10.3390/children10060956
Chicago/Turabian StyleNezondet, Charlie, Joseph Gandrieau, Julien Bourrelier, Philippe Nguyen, and Gautier Zunquin. 2023. "The Effectiveness of a Physical Literacy-Based Intervention for Increasing Physical Activity Levels and Improving Health Indicators in Overweight and Obese Adolescents (CAPACITES 64)" Children 10, no. 6: 956. https://doi.org/10.3390/children10060956
APA StyleNezondet, C., Gandrieau, J., Bourrelier, J., Nguyen, P., & Zunquin, G. (2023). The Effectiveness of a Physical Literacy-Based Intervention for Increasing Physical Activity Levels and Improving Health Indicators in Overweight and Obese Adolescents (CAPACITES 64). Children, 10(6), 956. https://doi.org/10.3390/children10060956






