Clinical Outcomes of Daytime Versus Nighttime Laparoscopic Appendectomy in Children
Abstract
1. Introduction
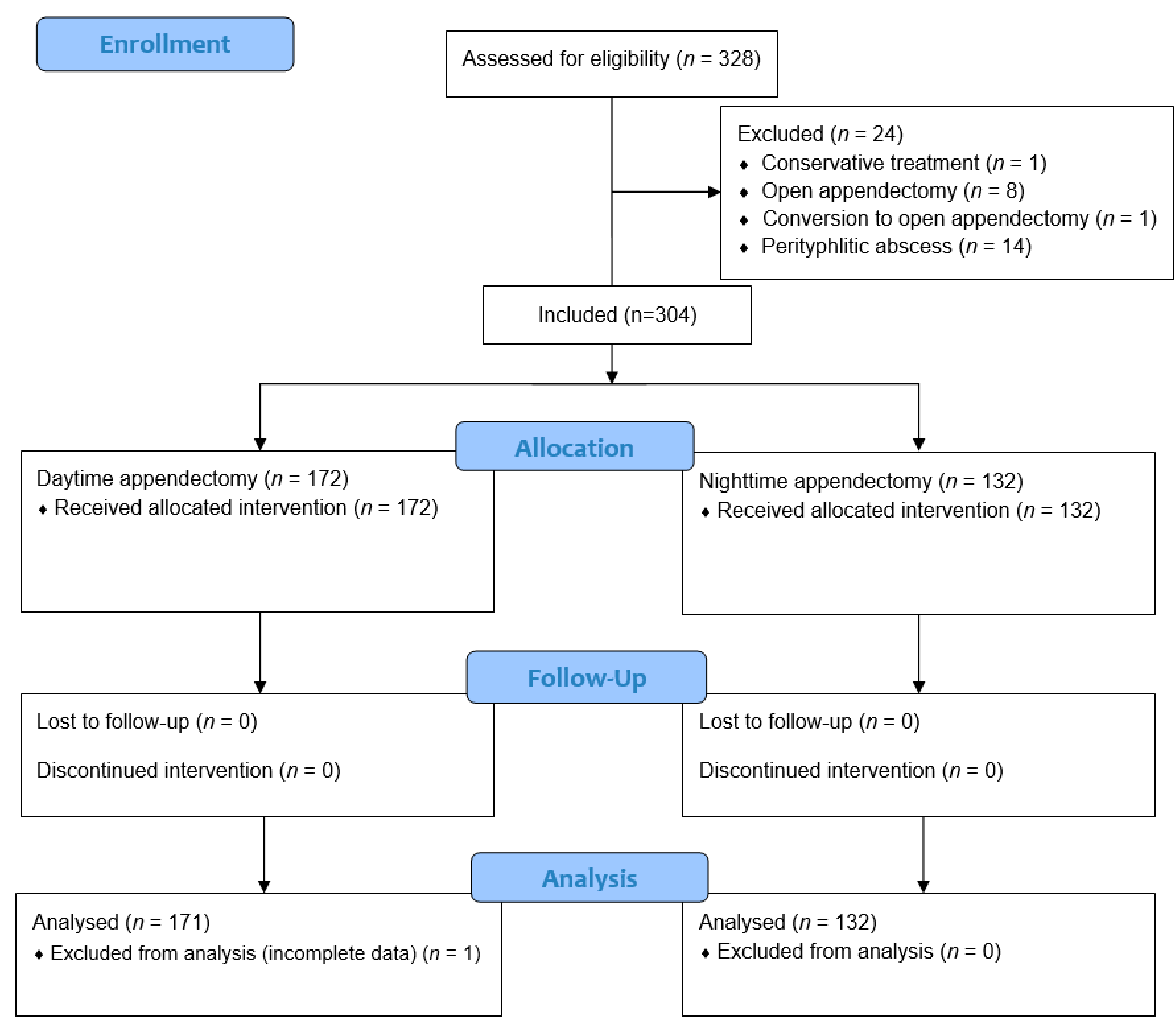
2. Materials and Methods
2.1. Patients
2.2. Outcomes of the Study
2.3. General Policy of Treatment of Acute Appendicitis and Indications for Emergency Surgery
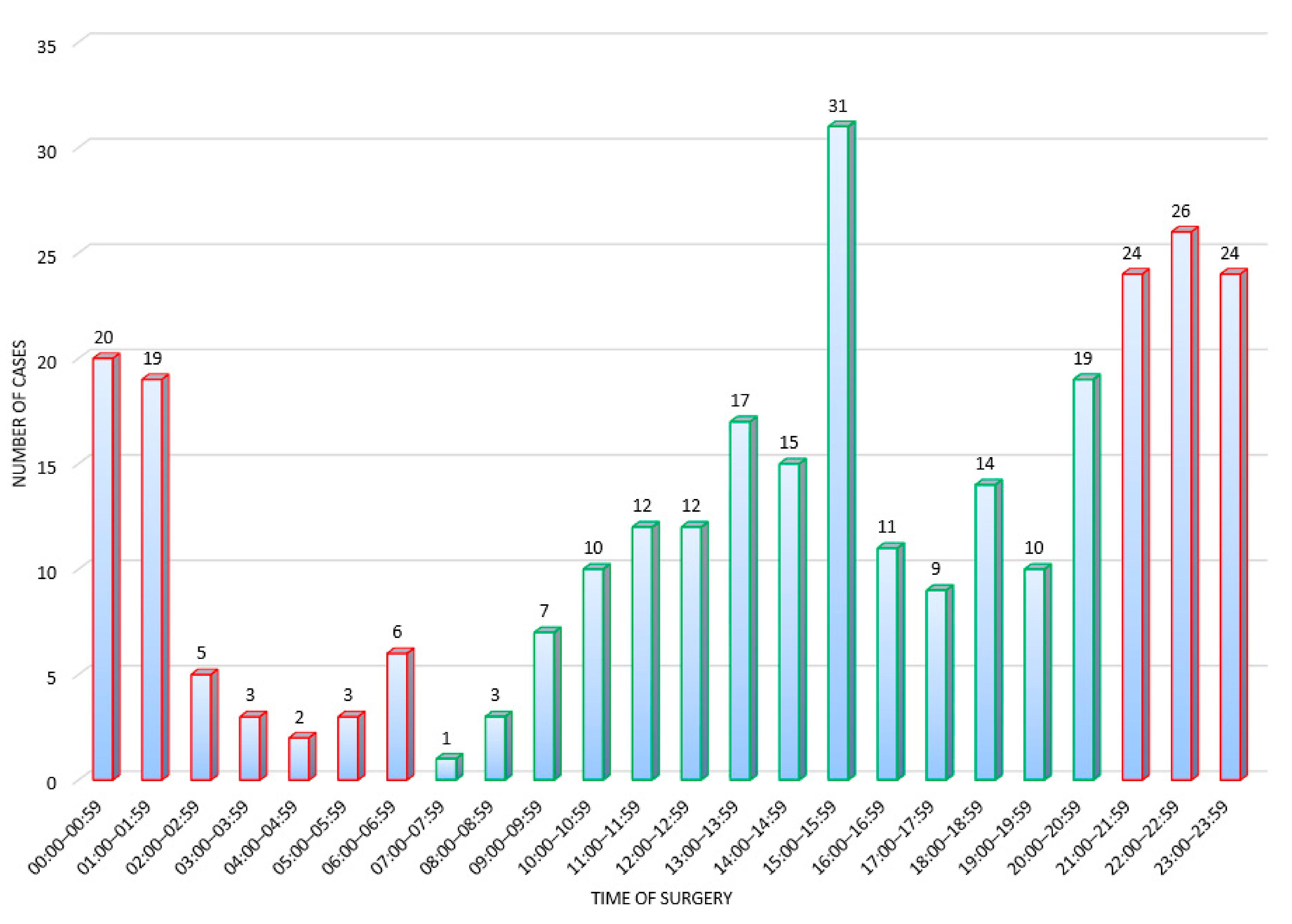
2.4. Study Design
2.5. Surgical Technique
2.6. Postoperative Protocol and Follow-Up
2.7. Ethical Aspects
2.8. Statistical Analysis
3. Results
3.1. Baseline Characteristics, Demographic and Clinical Data of the Study
3.2. Pathohistological Analysis
3.3. Comparison of Study Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shah, A.A.; Al-Zoubi, R.M.; Al-Qudimat, A.R.; Rejeb, M.A.; Ojha, L.K.; Abdulzem, S.; Qadir, K.; Sameer, S.; Zarour, A.; Ghali, M.S. Daytime versus nighttime laparoscopic appendectomy in term of complications and clinical outcomes: A retrospective study of 1001 appendectomies. Heliyon 2022, 8, e11911. [Google Scholar] [CrossRef] [PubMed]
- Jukić, M.; Tesch, A.; Todorić, J.; Šušnjar, T.; Milunović, K.P.; Barić, T.; Pogorelić, Z. Same-day discharge after laparoscopic appendectomy for simple appendicitis in pediatric patients—Is it possible? Children 2022, 9, 1220. [Google Scholar] [CrossRef] [PubMed]
- Basilio, M.S.; Delgado-Miguel, C.; Ramírez-Amorós, C.; Sarmiento, M.; Moratilla-Lapeña, L.; Almeyda, A.; Mejía, R.; Martínez, L. Does the timing of appendectomy affect outcomes and postoperative complications? Pediatr. Surg. Int. 2023, 39, 90. [Google Scholar] [CrossRef] [PubMed]
- Jackson, J.E.; Rajasekar, G.; Vukcevich, O.; Coakley, B.A.; Nuño, M.; Saadai, P. Association between race, gender, and pediatric postoperative outcomes: An updated retrospective review. J. Surg. Res. 2023, 281, 112–121. [Google Scholar] [CrossRef]
- Stringer, M.D. Acute appendicitis. J. Paediatr. Child Health 2017, 53, 1071–1076. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Čohadžić, T. A bizarre cause of acute appendicitis in a pediatric patient: An ingested tooth. Children 2023, 10, 108. [Google Scholar] [CrossRef]
- Jumah, S.; Wester, T. Non-operative management of acute appendicitis in children. Pediatr. Surg. Int. 2022, 39, 11. [Google Scholar] [CrossRef]
- Bai, S.; Hu, S.; Zhang, Y.; Guo, S.; Zhu, R.; Zeng, J. The value of the Alvarado score for the diagnosis of acute appendicitis in children: A systematic review and meta-analysis. J. Pediatr. Surg. 2023, in press. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Mihanović, J.; Ninčević, S.; Lukšić, B.; Baloević, S.E.; Polašek, O. Validity of appendicitis inflammatory response score in distinguishing perforated from non-perforated appendicitis in children. Children 2021, 8, 309. [Google Scholar] [CrossRef]
- Oztan, M.O.; Gokmen, A.A.; Ozdemir, T.; Müderris, T.; Kaya, S.; Koyluoglu, G. Pentraxin-3: A strong novel biochemical marker for appendicitis in children. Am. J. Emerg. Med. 2019, 37, 1912–1916. [Google Scholar] [CrossRef]
- Montero, J.A.; Antona, G.; Pascual, C.B.; Anaut, M.B.; Briones, R.R.; Fernández-Celis, A.; Marcotegui, A.R.; López-Andrés, N.; Martín-Calvo, N. Serum neutrophil gelatinase-associated lipocalin (NGAL) as a diagnostic tool in pediatric acute appendicitis: A prospective validation study. Pediatr. Surg. Int. 2022, 38, 1569–1576. [Google Scholar] [CrossRef]
- Montero, J.A.; Pascual, C.B.; Anaut, M.B.; López-Andrés, N.; Antona, G.; Martín-Calvo, N. Diagnostic performance of serum interleukin-6 in pediatric acute appendicitis: A systematic review. World J. Pediatr. 2022, 18, 91–99. [Google Scholar] [CrossRef]
- Wu, Z.; Zhao, L.; Feng, S.; Luo, J. Hyperfibrinogenemia and hyponatremia as predictors of perforated appendicitis in children: A retrospective cohort study. Int. J. Color. Dis. 2023, 38, 72. [Google Scholar] [CrossRef]
- Kakar, M.; Delorme, M.; Broks, R.; Asare, L.; Butnere, M.; Reinis, A.; Engelis, A.; Kroica, J.; Saxena, A.; Petersons, A. Determining acute complicated and uncomplicated appendicitis using serum and urine biomarkers: Interleukin-6 and neutrophil gelatinase-associated lipocalin. Pediatr. Surg. Int. 2020, 36, 629–636. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Lukšić, A.M.; Mihanović, J.; Đikić, D.; Balta, V. Hyperbilirubinemia as an indicator of perforated acute appendicitis in pediatric population: A prospective study. Surg. Infect. 2021, 22, 1064–1071. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Lukšić, B.; Ninčević, S.; Polašek, O. Hyponatremia as a predictor of perforated acute appendicitis in pediatric population: A prospective study. J. Pediatr. Surg. 2021, 56, 1816–1821. [Google Scholar] [CrossRef]
- Tintor, G.; Jukić, M.; Šupe-Domić, D.; Jerončić, A.; Pogorelić, Z. Diagnostic accuracy of leucine-rich α-2-glycoprotein 1 as a non-invasive salivary biomarker in pediatric appendicitis. Int. J. Mol. Sci. 2023, 24, 6043. [Google Scholar] [CrossRef]
- Tintor, G.; Jukić, M.; Šupe-Domić, D.; Jerončić, A.; Pogorelić, Z. Diagnostic utility of serum leucine-rich α-2-glycoprotein 1 for acute appendicitis in children. J. Clin. Med. 2023, 12, 2455. [Google Scholar] [CrossRef]
- Livingston, E.H.; Woodward, W.A.; Sarosi, G.A.; Haley, R.W. Disconnect between incidence of nonperforated and perforated appendicitis. Ann. Surg. 2007, 245, 886–892. [Google Scholar] [CrossRef]
- Poprom, N.; Wilasrusmee, C.; Attia, J.; McEvoy, M.; Thakkinstian, A.; Rattanasiri, S. Comparison of postoperative complications between open and laparoscopic appendectomy: An umbrella review of systematic reviews and meta-analyses. J. Trauma: Inj. Infect. Crit. Care 2020, 89, 813–820. [Google Scholar] [CrossRef] [PubMed]
- Wei, H.-B.; Huang, J.-L.; Zheng, Z.-H.; Wei, B.; Zheng, F.; Qiu, W.-S.; Guo, W.-P.; Chen, T.-F.; Wang, T.-B. Laparoscopic versus open appendectomy: A prospective randomized comparison. Surg. Endosc. 2009, 24, 266–269. [Google Scholar] [CrossRef] [PubMed]
- Vanhatalo, S.; Munukka, E.; Sippola, S.; Jalkanen, S.; Grönroos, J.; Marttila, H.; Eerola, E.; Hurme, S.; Hakanen, A.J.; APPAC Collaborative Study Group; et al. Prospective multicentre cohort trial on acute appendicitis and microbiota, aetiology and effects of antimicrobial treatment: Study protocol for the MAPPAC (Microbiology APPendicitis ACuta) trial. BMJ Open 2019, 9, e031137. [Google Scholar] [CrossRef] [PubMed]
- Van Dijk, S.T.; van Dijk, A.H.; Dijkgraaf, M.G.; Boermeester, M.A. Meta-analysis of in-hospital delay before surgery as a risk factor for complications in patients with acute appendicitis. Br. J. Surg. 2018, 105, 933–945. [Google Scholar] [CrossRef] [PubMed]
- Mönttinen, T.; Kangaspunta, H.; Laukkarinen, J.; Ukkonen, M. Nighttime appendectomy is safe and has similar outcomes as daytime appendectomy: A study of 1198 appendectomies. Scand. J. Surg. 2021, 110, 227–232. [Google Scholar] [CrossRef]
- Li, J.; Xu, R.; Hu, D.-M.; Zhang, Y.; Gong, T.-P.; Wu, X.-L. Effect of Delay to operation on outcomes in patients with acute appendicitis: A systematic review and meta-analysis. J. Gastrointest. Surg. 2019, 23, 210–223. [Google Scholar] [CrossRef]
- Teixeira, P.; Sivrikoz, E.; Inaba, K.; Talving, P.; Lam, L.; Demetriades, D. Appendectomy timing. Ann. Surg. 2012, 256, 538–543. [Google Scholar] [CrossRef]
- Bolmers, M.D.M.; de Jonge, J.; Bom, W.J.; van Rossem, C.C.; van Geloven, A.A.W.; Bemelman, W.A.; Snapshot Appendicitis Collaborative Study Group. In-hospital delay of appendectomy in acute, complicated appendicitis. J. Gastrointest. Surg. 2022, 26, 1063–1069. [Google Scholar] [CrossRef]
- Bom, W.J.; de Jonge, J.; Scheijmans, J.C.G.; van Geloven, A.A.W.; Gans, S.L.; Boermeester, M.A.; Bemelman, W.A.; van Rossem, C.C.; on behalf of the Snapshot. Daytime versus nighttime in acute appendicitis. Diagnostics 2022, 12, 788. [Google Scholar] [CrossRef]
- Jukić, M.; Antišić, J.; Pogorelić, Z. Incidence and causes of 30-day readmission rate from discharge as an indicator of quality care in pediatric surgery. Acta Chir. Belg. 2023, 123, 26–30. [Google Scholar] [CrossRef]
- Jukić, M.; Biuk, I.; Pogorelić, Z. The incidence and causes of unplanned reoperations as a quality indicator in pediatric surgery. Children 2022, 9, 106. [Google Scholar] [CrossRef]
- Dindo, D.; Demartines, N.; Clavien, P.-A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Mihanović, J.; Šikić, N.L.; Mrklić, I.; Katušić, Z.; Karlo, R.; Jukić, M.; Jerončić, A.; Pogorelić, Z. Comparison of new versus reused Harmonic scalpel performance in laparoscopic appendectomy in patients with acute appendicitis—A randomized clinical trial. Langenbeck’s Arch. Surg. 2021, 406, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Pogorelić, Z.; Kostovski, B.; Jerončić, A.; Šušnjar, T.; Mrklić, I.; Jukić, M.; Jurić, I. A Comparison of endoloop ligatures and nonabsorbable polymeric clips for the closure of the appendicular stump during laparoscopic appendectomy in children. J. Laparoendosc. Adv. Surg. Tech. 2017, 27, 645–650. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Beara, V.; Jukić, M.; Rashwan, H.; Šušnjar, T. A new approach to laparoscopic appendectomy in children—Clipless/sutureless Harmonic scalpel laparoscopic appendectomy. Langenbeck’s Arch. Surg. 2022, 407, 779–787. [Google Scholar] [CrossRef] [PubMed]
- Jaschinski, T.; Mosch, C.; Eikermann, M.; Neugebauer, E.A. Laparoscopic versus open appendectomy in patients with suspected appendicitis: A systematic review of meta-analyses of randomised controlled trials. BMC Gastroenterol. 2015, 15, 48. [Google Scholar] [CrossRef]
- Bailey, K.; Choynowski, M.; Kabir, S.M.U.; Lawler, J.; Badrin, A.; Sugrue, M. Meta-analysis of unplanned readmission to hospital post-appendectomy: An opportunity for a new benchmark. ANZ J. Surg. 2019, 89, 1386–1391. [Google Scholar] [CrossRef]
- Rolle, U.; Fahlenbach, C.; Heidecke, C.-D.; Heller, G.; Meyer, H.-J.; Schuler, E.; Waibel, B.; Jeschke, E.; Günster, C.; Maneck, M. Rates of complications after appendectomy in children and adolescents: Pediatric surgical compared to general surgical hospitals. J. Surg. Res. 2021, 260, 467–474. [Google Scholar] [CrossRef]
- Karakaya, A.E. The reasons for conversion from laparoscopic appendectomy to open surgery in children: The first experience on 100 cases in a single center. Dicle Tıp Dergisi 2021, 48, 65–71. [Google Scholar] [CrossRef]
- Johnson, K.N.; Linnaus, M.; Notrica, D.M. Conversion from laparoscopic to open appendectomy: Decreased risk at dedicated children’s hospitals. Pediatr. Surg. Int. 2018, 34, 873–877. [Google Scholar] [CrossRef]
- Lezama, M.M.; Casas, M.A.; Angeramo, C.A.; Harriott, C.B.; Schlottmann, F. Conversion from laparoscopic to open appendectomy: Trends, risk factors and outcomes. A 15-year single-center analysis of 2193 adult patients. World J. Surg. 2022, 46, 2642–2647. [Google Scholar] [CrossRef]
- Li, X.; Zhang, J.; Sang, L.; Zhang, W.; Chu, Z.; Li, X.; Liu, Y. Laparoscopic versus conventional appendectomy—A meta-analysis of randomized controlled trials. BMC Gastroenterol. 2010, 10, 1–8. [Google Scholar] [CrossRef]
- Jeon, B.G.; Kim, H.J.; Jung, K.H.; Kim, S.W.; Park, J.S.; Kim, K.H.; Kim, I.D.; Lee, S.-J. Prolonged operative time in laparoscopic appendectomy: Predictive factors and outcomes. Int. J. Surg. 2016, 36 Pt A, 225–232. [Google Scholar] [CrossRef]
- Souza-Gallardo, L.M.; Martínez-Ordaz, J.L. Apendicitis aguda. manejo quirúrgico y no quirúrgico [acute appendicitis. surgical and non-surgical treatment]. Rev. Med. Inst. Mex. Seguro Soc. 2017, 55, 76–81. [Google Scholar]
- Salminen, P.; Paajanen, H.; Rautio, T.; Nordström, P.; Aarnio, M.; Rantanen, T.; Tuominen, R.; Hurme, S.; Virtanen, J.; Mecklin, J.-P.; et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: The APPAC randomized clinical trial. JAMA 2015, 313, 2340–2348. [Google Scholar] [CrossRef]
- Leite, R.M.d.A.; Seo, D.J.; Gomez-Eslava, B.; Hossain, S.; Lesegretain, A.; de Souza, A.V.; Bay, C.P.; Zilberstein, B.; Marchi, E.; Machado, R.B.; et al. Nonoperative vs operative management of uncomplicated acute appendicitis: A systematic review and meta-analysis. JAMA Surg. 2022, 157, 828. [Google Scholar] [CrossRef]
- Patel, S.V.; Groome, P.A.; Merchant, S.J.; Lajkosz, K.; Nanji, S.; Brogly, S.B. Timing of surgery and the risk of complications in patients with acute appendicitis: A population-level case-crossover study. J. Trauma Acute Care Surg. 2018, 85, 341–347. [Google Scholar] [CrossRef]
- Tago, T.; Shimoda, M.; Imazato, R.; Udou, R.; Katsumata, K.; Tsuchida, A.; Suzuki, S. Possibility for avoidance of urgent nighttime operations for acute appendicitis in a regional core university hospital. Asian J. Endosc. Surg. 2022, 15, 22–28. [Google Scholar] [CrossRef]
- Koltka, A.K.; Ali, A.; Yanar, T.H.; Ilhan, M.; Gök, A.F.K.; Sivrikoz, N.; Günay, M.K.; Ertekin, C. Is nighttime laparoscopic general surgery under general anesthesia safe? Ulus Travma Acil Cerrahi Derg 2018, 24, 20–24. [Google Scholar] [CrossRef]
- Meschino, M.T.; Giles, A.E.; Rice, T.J.; Saddik, M.; Doumouras, A.G.; Nenshi, R.; Allen, L.; Vogt, K.; Engels, P.T. Operative timing is associated with increased morbidity and mortality in patients undergoing emergency general surgery: A multisite study of emergency general services in a single academic network. Can. J. Surg. 2020, 63, E321–E328. [Google Scholar] [CrossRef]
- Kelz, R.R.; Tran, T.T.; Hosokawa, P.; Henderson, W.; Paulson, C.E.; Spitz, F.; Hamilton, B.H.; Hall, B.L. Time-of-day effects on surgical outcomes in the private sector: A retrospective cohort study. J. Am. Coll. Surg. 2009, 209, 434–445e2. [Google Scholar] [CrossRef]
- Chen, C.; Zhang, X.; Gu, C.; Wang, Y.; Liu, K.; Pan, X.; Fu, S.; Fan, L.; Wang, R. Surgery performed at night by continuously working surgeons contributes to a higher incidence of intraoperative complications in video-assisted thoracoscopic pulmonary resection: A large monocentric retrospective study. Eur. J. Cardio-Thoracic Surg. 2020, 57, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Buget, M.I.; Canbolat, N.; Chousein, C.M.; Kizilkurt, T.; Ersen, A.; Koltka, K. Comparison of nighttime and daytime operation on outcomes of supracondylar humeral fractures: A prospective observational study. Medicine 2022, 101, e29382. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, S.; Carvalho, A.F.; Rodrigues, A.J.; Costa, P.; Sanz, M.; Goulart, A.; Rios, H.; Leão, P. Day and night surgery: Is there any influence in the patient postoperative period of urgent colorectal intervention? Int. J. Color. Dis. 2016, 31, 525–533. [Google Scholar] [CrossRef] [PubMed]
- Merati-Kashani, K.; Canal, C.; Birrer, D.L.; Clavien, P.-A.; Neuhaus, V.; Turina, M. Nighttime cholecystectomies are safe when controlled for individual patient risk factors–a nationwide case–control analysis. World J. Surg. 2021, 45, 2058–2065. [Google Scholar] [CrossRef]
- Yaghoubian, A.; Kaji, A.H.; Ishaque, B.; Park, J.; Rosing, D.K.; Lee, S.; Stabile, B.E.; de Virgilio, C. Acute care surgery performed by sleep deprived residents: Are outcomes affected? J. Surg. Res. 2010, 163, 192–196. [Google Scholar] [CrossRef]
- Wu, J.X.; Nguyen, A.T.; de Virgilio, C.; Plurad, D.S.; Kaji, A.H.; Nguyen, V.; Gifford, E.; de Virgilio, M.; Ayabe, R.; Saltzman, D.; et al. Can it wait until morning? A comparison of nighttime versus daytime cholecystectomy for acute cholecystitis. Am. J. Surg. 2014, 208, 911–918, Discussion 917–918. [Google Scholar] [CrossRef]
- Tomasko, J.M.; Pauli, E.M.; Kunselman, A.R.; Haluck, R.S. Sleep deprivation increases cognitive workload during simulated surgical tasks. Am. J. Surg. 2012, 203, 37–43. [Google Scholar] [CrossRef]
- Whelehan, D.F.; Alexander, M.; Connelly, T.M.; McEvoy, C.; Ridgway, P.F. Sleepy surgeons: A multi-method assessment of sleep deprivation and performance in surgery. J. Surg. Res. 2021, 268, 145–157. [Google Scholar] [CrossRef]
- Sikder, S.; Tuwairqi, K.; Selter, J. Assessment of surgeon fatigue by surgical simulators. Open Access Surg. 2015, 8, 43–50. [Google Scholar] [CrossRef]
- Whelehan, D.F.; McCarrick, C.A.; Ridgway, P.F. A systematic review of sleep deprivation and technical skill in surgery. Surgeon 2020, 18, 375–384. [Google Scholar] [CrossRef]
- Koda, N.; Oshima, Y.; Koda, K.; Shimada, H. Surgeon fatigue does not affect surgical outcomes: A systematic review and meta-analysis. Surg. Today 2020, 51, 659–668. [Google Scholar] [CrossRef]
- Sturm, L.; Dawson, D.; Vaughan, R.; Hewett, P.; Hill, A.; Graham, J.C.; Maddern, G.J. Effects of fatigue on surgeon performance and surgical outcomes: A systematic review. ANZ J. Surg. 2011, 81, 502–509. [Google Scholar] [CrossRef]
- Sun, E.C.; Mello, M.M.; Vaughn, M.T.; Kheterpal, S.; Hawn, M.T.; Dimick, J.B.; Jena, A.B. Assessment of perioperative outcomes among surgeons who operated the night before. JAMA Intern. Med. 2022, 182, 720–728. [Google Scholar] [CrossRef]
- Vinden, C.; Nash, D.M.; Rangrej, J.; Shariff, S.Z.; Dixon, S.N.; Jain, A.K.; Garg, A.X. Complications of daytime elective laparoscopic cholecystectomies performed by surgeons who operated the night before. JAMA 2013, 310, 1837–1841. [Google Scholar] [CrossRef]
| Group I (n = 171) Daytime Appendectomy | Group II (n = 132) Nighttime Appendectomy | p | |
|---|---|---|---|
| Demographic Characteristics of Patients; Median (IQR) or n (%) | |||
| Age (years) | 11 (9, 14) | 11 (8, 15) | 0.631 * |
| Gender | |||
| Male Female | 115 (67.3) 56 (32.7) | 81 (61.4) 51 (38.6) | 0.287 † |
| Weight (kg) | 45 (34, 60) | 44 (35, 65.5) | 0.865 * |
| Height (cm) | 159 (141, 174) | 156.5 (143, 174) | 0.703 * |
| Clinical data of patients; median (IQR); mean ± SD or n (%) | |||
| Duration of symptoms (h) | 22 (20, 44) | 24 (20, 48) | 0.667 * |
| Body temperature (°C) | 37.1 ± 0.7 | 37.2 ± 0.8 | 0.853 § |
| Vomiting | 97 (56.7) | 77 (58.3) | 0.778 † |
| Pain in RLQ | 171 (100) | 132 (100) | >0.999 ‡ |
| Rebound tenderness | 141 (82.5) | 105 (79.5) | 0.520 † |
| AIR score; median (IQR) | 7 (4, 8) | 7 (4, 8) | 0.833 * |
| Laboratory data of patients; median (IQR) or mean ± SD | |||
| Leukocytes (×109/L) | 14.4 ± 4.7 | 14.7 ± 5.5 | 0.700 § |
| C-reactive protein (mg/L) | 17.9 (6, 44.9) | 17.1 (5.6, 43.3) | 0.412 * |
| Neutrophil granulocytes (%) | 80.7 ± 10.3 | 80.0 ± 9.8 | 0.556 § |
| Variables n (%) | Group I (n = 167) Daytime Appendectomy | Group II (n = 129) Nighttime Appendectomy | p |
|---|---|---|---|
| Catarrhal appendicitis | 17 (10.2) | 13 (10.1) | 0.976 * |
| Phlegmonous appendicitis | 74 (44.3) | 51 (39.5) | 0.409 * |
| Gangrenous appendicitis | 62 (37.1) | 47 (36.4) | 0.902 * |
| Neuroendocrine tumor | 1 (0.6) | 2 (1.6) | 0.582 † |
| No appendicitis | 13 (7.8) | 16 (12.4) | 0.185 * |
| Variables Median (IQR) or n (%) | Group I (n = 171) | Group II (n = 132) | p |
|---|---|---|---|
| Daytime Appendectomy | Nighttime Appendectomy | ||
| Postoperative fever < 72 h | 11 (6.4) | 10 (7.6) | 0.697 * |
| Complications (total) | 11 (6.4) | 9 (6.8) | 0.893 * |
| Postoperative ileus | 2 (1.2) | 1 (0.8) | >0.999 † |
| Abscess | 7 (4.1) | 4 (3) | 0.761 † |
| Wound infection | 1 (0.6) | 2 (1.5) | 0.582 † |
| Bladder injury | 0 (0) | 1 (0.8) | 0.435 † |
| Bleeding—trocar insertion site | 1 (0.6) | 1 (0.8) | >0.999 † |
| Duration of surgery (min) | 26 (22, 40) | 37 (31, 46) | <0.001 ‡ |
| Re-admission | 5 (2.9) | 2 (1.5) | 0.703 † |
| Redo-surgery | 3 (1.7) | 0 (0) | 0.260 † |
| Conversion to laparotomy | 0 (0) | 1 (0.8) | 0.435 † |
| Duration of hospital stay (days) | 3 (1, 5) | 3 (2, 5) | 0.368 ‡ |
| Grade | Group I (n = 171) | Group II (n = 132) | p * |
|---|---|---|---|
| Daytime Appendectomy | Nighttime Appendectomy | ||
| I | 2 (1.2) | 1 (0.8) | >0.999 |
| II | 5 (2.9) | 3 (2.3) | >0.999 |
| III a | 1 (0.6) | 2 (1.5) | 0.581 |
| III b | 3 (1.8) | 3 (2.3) | >0.999 |
| IV a | 0 | 0 | - |
| IV b | 0 | 0 | - |
| V | 0 | 0 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pogorelić, Z.; Janković Marendić, I.; Čohadžić, T.; Jukić, M. Clinical Outcomes of Daytime Versus Nighttime Laparoscopic Appendectomy in Children. Children 2023, 10, 750. https://doi.org/10.3390/children10040750
Pogorelić Z, Janković Marendić I, Čohadžić T, Jukić M. Clinical Outcomes of Daytime Versus Nighttime Laparoscopic Appendectomy in Children. Children. 2023; 10(4):750. https://doi.org/10.3390/children10040750
Chicago/Turabian StylePogorelić, Zenon, Ivana Janković Marendić, Tin Čohadžić, and Miro Jukić. 2023. "Clinical Outcomes of Daytime Versus Nighttime Laparoscopic Appendectomy in Children" Children 10, no. 4: 750. https://doi.org/10.3390/children10040750
APA StylePogorelić, Z., Janković Marendić, I., Čohadžić, T., & Jukić, M. (2023). Clinical Outcomes of Daytime Versus Nighttime Laparoscopic Appendectomy in Children. Children, 10(4), 750. https://doi.org/10.3390/children10040750








