Comparative Evaluation of Flexural Strength of Four Different Types of Provisional Restoration Materials: An In Vitro Pilot Study
Abstract
1. Introduction
2. Materials and Methods
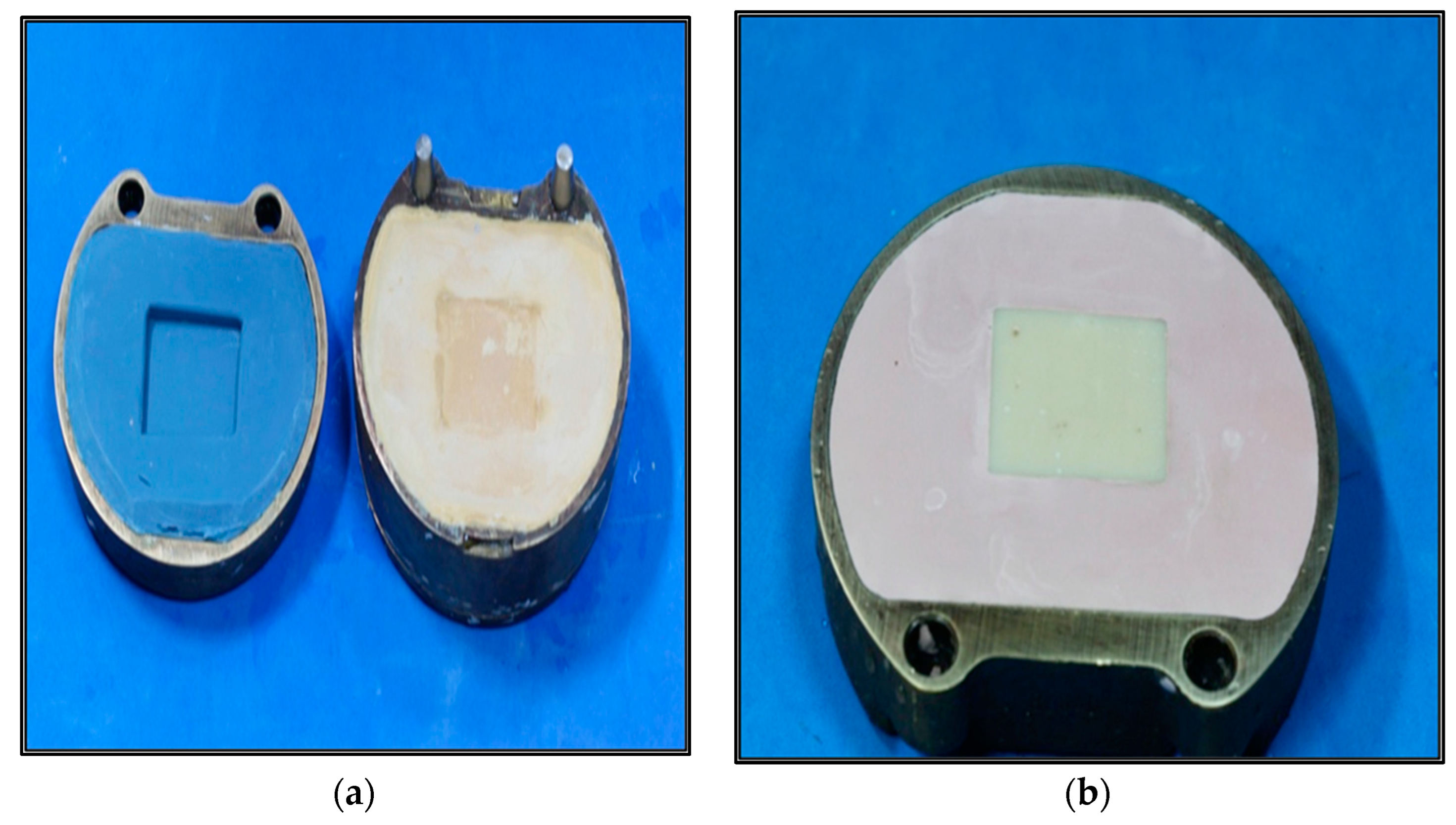
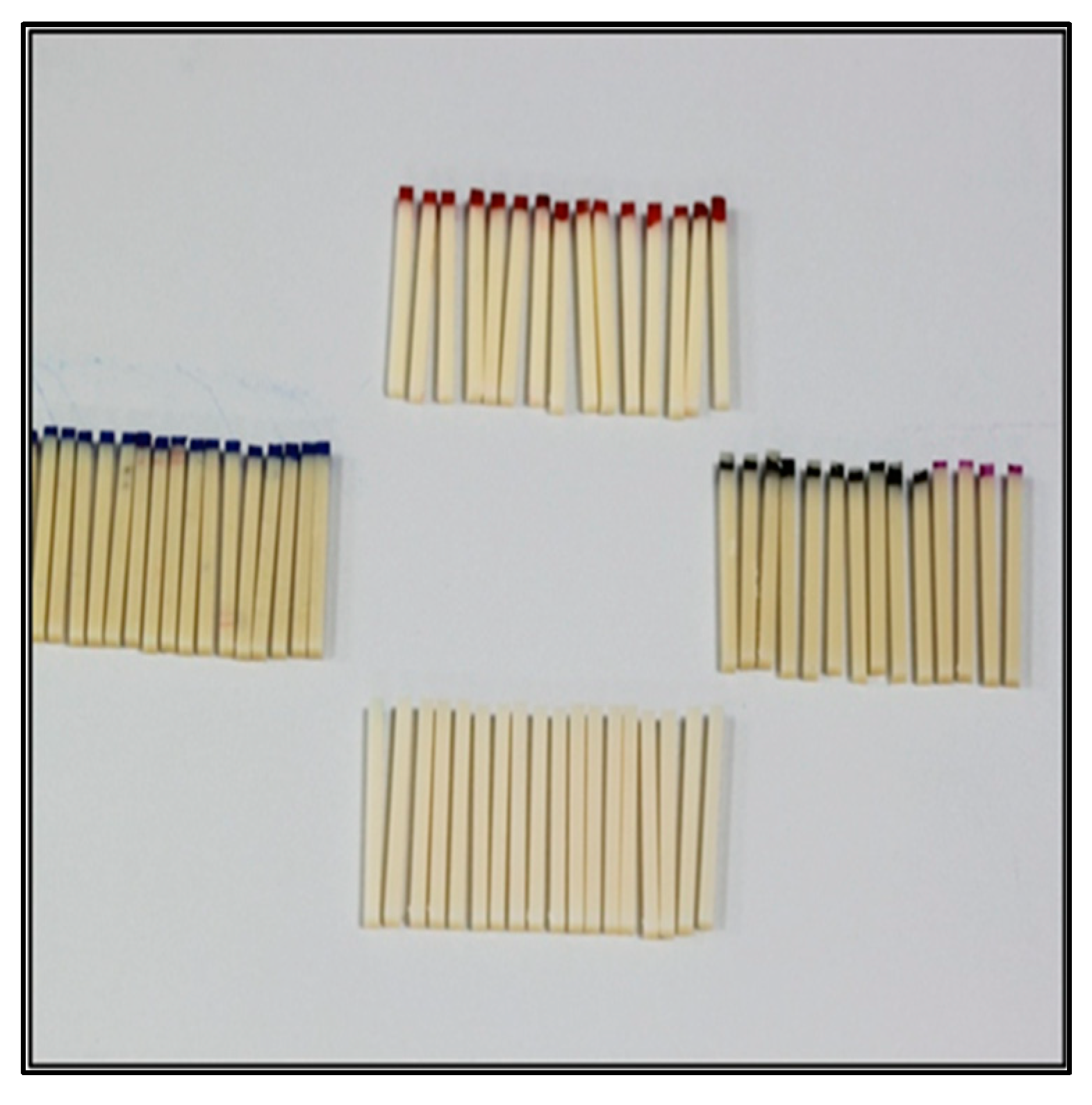
2.1. Methodology: (Figure 1)

2.1.1. Group 1–SR Ivocron Cold-Polymerized PMMA
2.1.2. Group–2 SR Ivocron Heat-Polymerized PMMA
2.1.3. Group–3 Protemp 4
2.1.4. Group 4–Revotek LC
2.1.5. Preparing Final Specimens for Testing
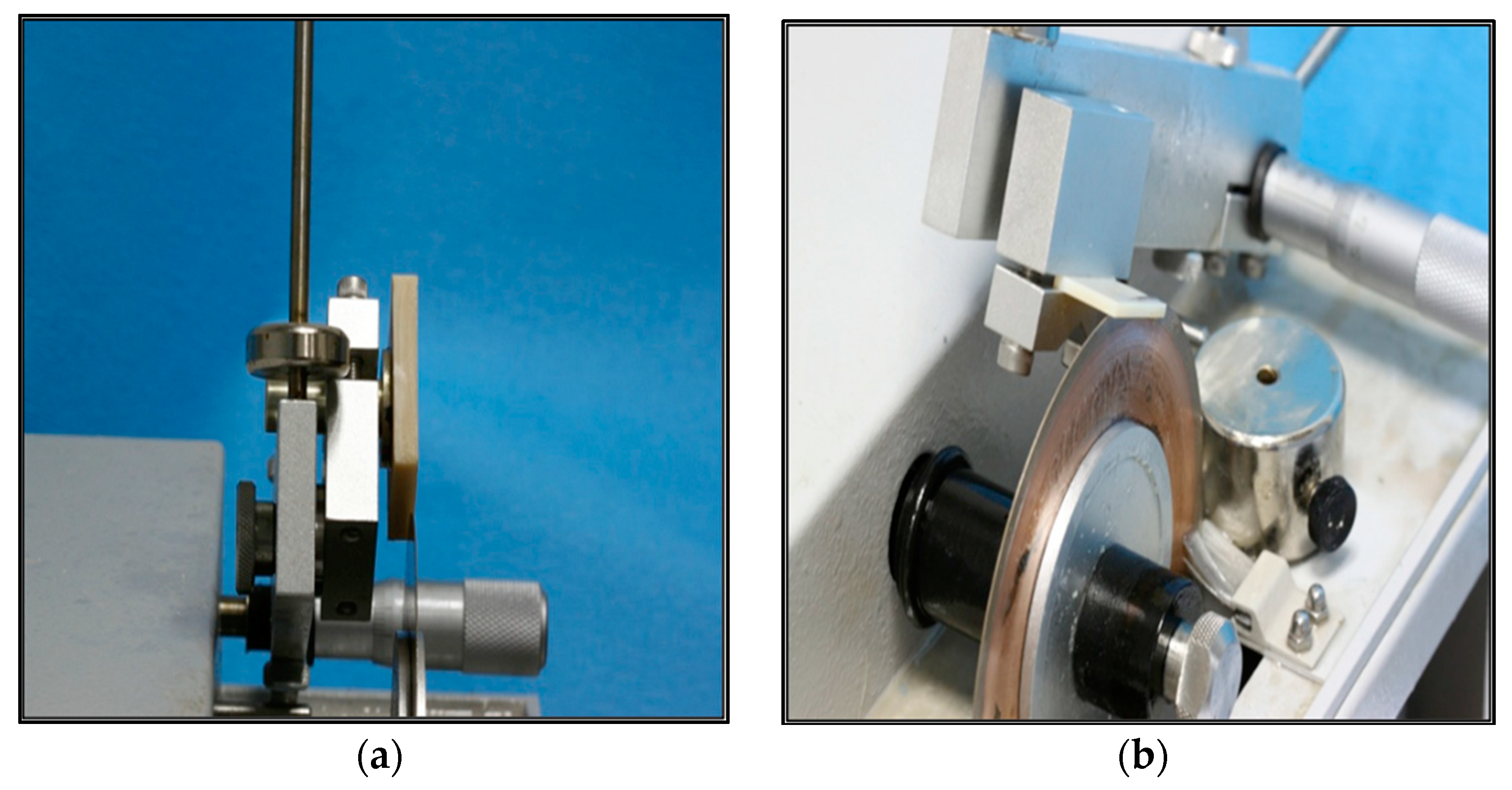
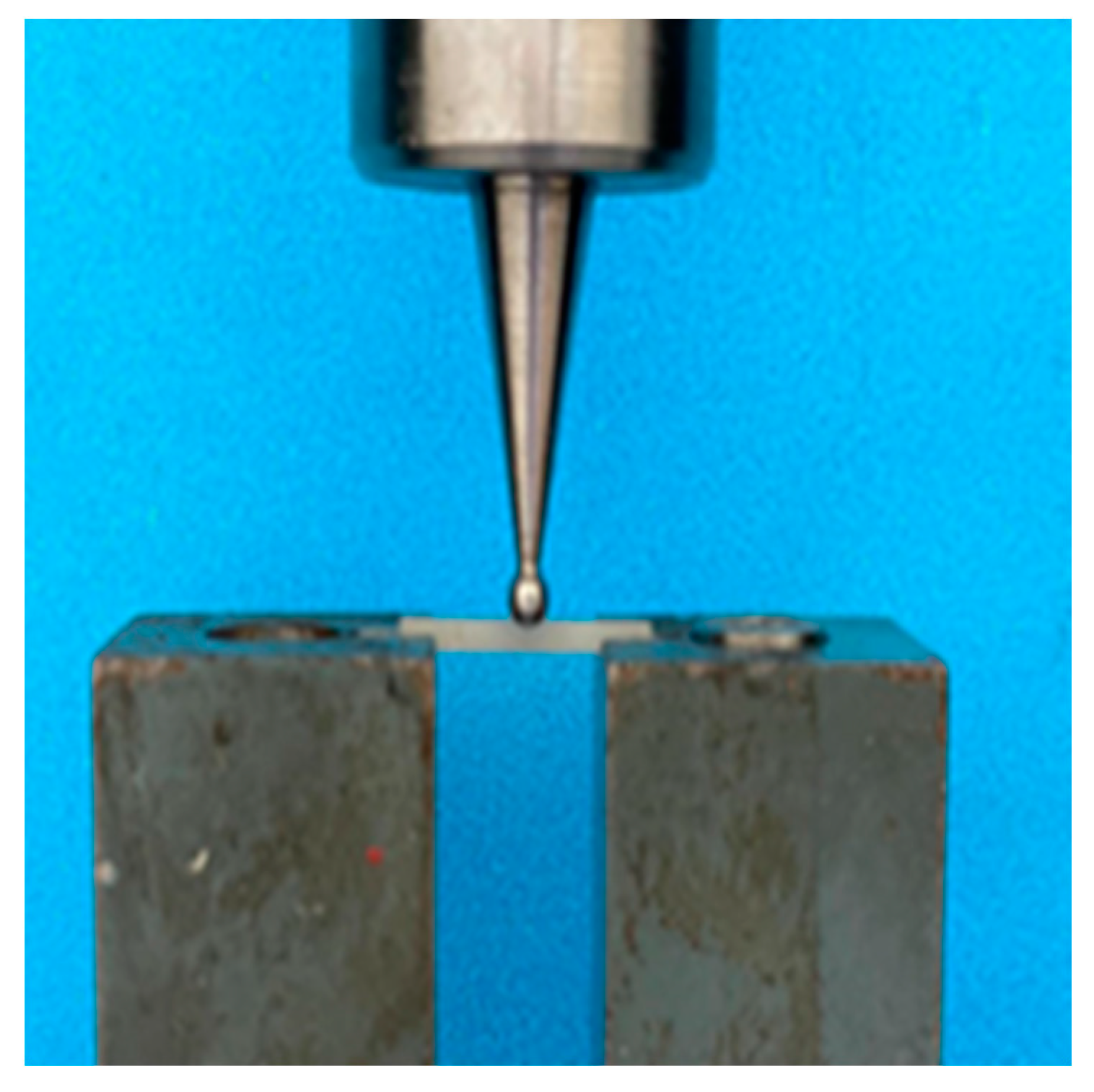
2.2. Flexure Strength Testing
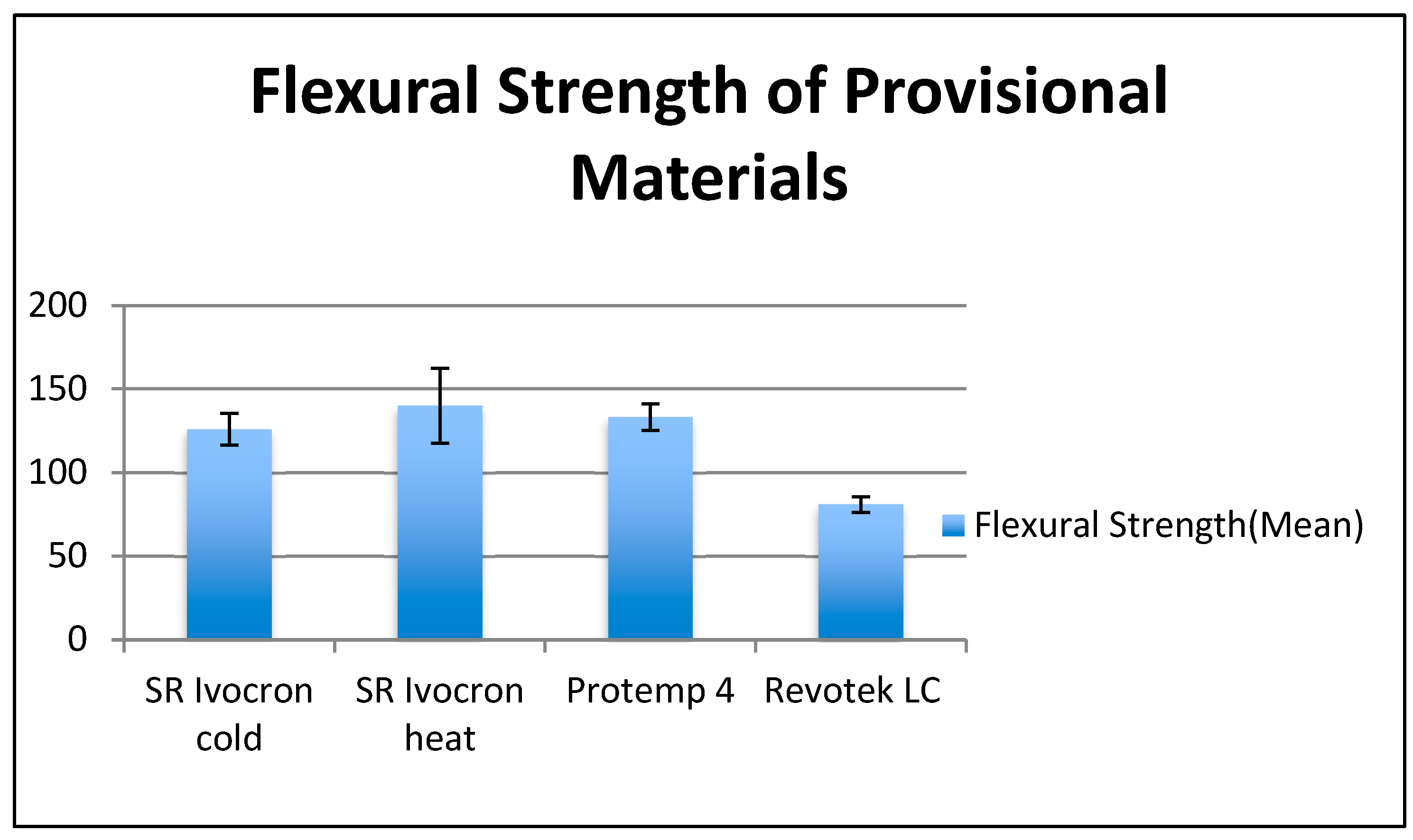
3. Results
Statistical Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rosenstiel, S.F.; Land, M.F.; Fujimoto, J. Contemporary Fixed Prosthodontics, 4th ed.; Mosby: St. Louis, MO, USA, 2006. [Google Scholar]
- Wang, R.L.; Moore, B.K.; Goodacre, C.J.; Swartz, M.L.; Andres, C.J. A Comparison of Resins for Fabricating Provisional Fixed Restorations. Int. J. Prosthodont. 1989, 2, 173–184. [Google Scholar]
- Hamza, T.A.; Rosenstiel, S.F.; Elhosary, M.M.; Ibraheem, R.M. The Effect of Fiber Reinforcement on the Fracture Toughness and Flexural Strength of Provisional Restorative Resins. J. Prosthet. Dent. 2004, 91, 258–264. [Google Scholar] [CrossRef]
- Abdullah, A.O.; Tsitrou, E.A.; Pollington, S. Comparative in Vitro Evaluation of CAD/CAM vs Conventional Provisional Crowns. J. Appl. Oral Sci. 2016, 24, 258–263. [Google Scholar] [CrossRef]
- Nejatidanesh, F.; Momeni, G.; Savabi, O. Flexural Strength of Interim Resin Materials for Fixed Prosthodontics. J. Prosthodont. 2009, 18, 507–511. [Google Scholar] [CrossRef]
- Christensen, G.J. Tooth Preparation and Pulp Degeneration. J. Am. Dent. Assoc. 1997, 128, 353–354. [Google Scholar] [CrossRef]
- Hazelton, L.R.; Nicholls, J.I.; Brudvik, J.S.; Daly, C.H. Influence of Reinforcement Design on the Loss of Marginal Seal of Provisional Fixed Partial Dentures. Int. J. Prosthodont. 1995, 8, 572–579. [Google Scholar]
- Vahidi, F. The Provisional Restoration. Dent. Clin. N. Am. 1987, 31, 363–381. [Google Scholar] [CrossRef]
- Skurow, H.M.; Nevins, M. The Rationale of the Preperiodontal Provisional Biologic Trial Restoration. Int. J. Periodontics Restor. Dent. 1988, 8, 8–29. [Google Scholar]
- Nejatidanesh, F.; Lotfi, H.R.; Savabi, O. Marginal Accuracy of Interim Restorations Fabricated from Four Interim Autopolymerizing Resins. J. Prosthet. Dent. 2006, 95, 364–367. [Google Scholar] [CrossRef]
- Haselton, D.R.; Diaz-Arnold, A.M.; Vargas, M.A. Flexural Strength of Provisional Crown and Fixed Partial Denture Resins. J. Prosthet. Dent. 2002, 87, 225–228. [Google Scholar] [CrossRef]
- Yannikakis, S.A.; Zissis, A.J.; Polyzois, G.L.; Caroni, C. Color Stability of Provisional Resin Restorative Materials. J. Prosthet. Dent. 1998, 80, 533–539. [Google Scholar] [CrossRef]
- Galindo, D.; Soltys, J.L.; Graser, G.N. Long-Term Reinforced Fixed Provisional Restorations. J. Prosthet. Dent. 1998, 79, 698–701. [Google Scholar] [CrossRef]
- Lang, R.; Rosentritt, M.; Behr, M.; Handel, G. Fracture Resistance of PMMA and Resin Matrix Composite-Based Interim FPD Materials. Int. J. Prosthodont. 2003, 16, 381–384. [Google Scholar]
- Akova, T.; Ozkomur, A.; Uysal, H. Effect of Food-Simulating Liquids on the Mechanical Properties of Provisional Restorative Materials. Dent. Mater. 2006, 22, 1130–1134. [Google Scholar] [CrossRef]
- Oshida, Y.; Hashem, A.; Elsalawy, R. Some Mechanistic Observation on Water-Deteriorated Dental Composite Resins. Biomed. Mater. Eng. 1995, 5, 93–115. [Google Scholar] [CrossRef]
- Donovan, T.E.; Hurst, R.G.; Campagni, W.V. Physical Properties of Acrylic Resin Polymerized by Four Different Techniques. J. Prosthet. Dent. 1985, 54, 522–524. [Google Scholar] [CrossRef]
- Diaz-Arnold, A.M.; Dunne, J.T.; Jones, A.H. Microhardness of Provisional Fixed Prosthodontic Materials. J. Prosthet. Dent. 1999, 82, 525–528. [Google Scholar] [CrossRef]
- Kaiser, D.A.; Cavazos, E. Temporization Techniques in Fixed Prosthodontics. Dent. Clin. N. Am. 1985, 29, 403–412. [Google Scholar] [CrossRef]
- Young, H.M.; Smith, C.T.; Morton, D. Comparative in Vitro Evaluation of Two Provisional Restorative Materials. J. Prosthet. Dent. 2001, 85, 129–132. [Google Scholar] [CrossRef]
- Rosentritt, M.; Behr, M.; Lang, R.; Handel, G. Flexural Properties of Prosthetic Provisional Polymers. Eur. J. Prosthodont. Restor. Dent. 2004, 12, 75–79. [Google Scholar]
- Emtiaz, S.; Tarnow, D.P. Processed Acrylic Resin Provisional Restoration with Lingual Cast Metal Framework. J. Prosthet. Dent. 1998, 79, 484–488. [Google Scholar] [CrossRef]
- Prestipino, V. Visible Light Cured Resins: A Technique for Provisional Fixed Restorations. Quintessence Int. 1989, 20, 241–248. [Google Scholar]
- Passon, C.; Goldfogel, M. Direct Technique for the Fabrication of a Visible Light-Curing Resin Provisional Restoration. Quintessence Int. 1990, 21, 699–703. [Google Scholar]
- Haddix, J.E. A Technique for Visible Light-Cured Provisional Restorations. J. Prosthet. Dent. 1988, 59, 512–514. [Google Scholar] [CrossRef]
- Moulding, M.B.; Teplitsky, P.E. Intrapulpal Temperature during Direct Fabrication of Provisional Restorations. Int. J. Prosthodont. 1989, 3, 299–304. [Google Scholar]
- Dahl, B.L.; Tronstad, L.; Spågberg, L. Biological Tests of a Temporary Crown and Bridge Material. J. Oral Rehabil. 1974, 1, 299–309. [Google Scholar] [CrossRef]
- Khan, Z.; Razavi, R.; von Fraunhofer, J.A. The Physical Properties of a Visible Light-Cured Temporary Fixed Partial Denture Material. J. Prosthet. Dent. 1988, 60, 543–545. [Google Scholar] [CrossRef]
- Ogle, R.E.; Sorensen, S.E.; Lewis, E.A. A New Visible Light-Cured Resin System Applied to Removable Prosthodontics. J. Prosthet. Dent. 1986, 56, 497–506. [Google Scholar] [CrossRef]
- Burns, D.R.; Beck, D.A.; Nelson, S.K. A Review of Selected Dental Literature on Contemporary Provisional Fixed Prosthodontic Treatment: Report of the Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. J. Prosthet. Dent. 2003, 90, 474–497. [Google Scholar] [CrossRef]
- Kc, V.; Kandaswamy, E.; Ms, M. A Comparative Evaluation of Fracture Toughness of Composite Resin vs Protemp 4 for Use in Strip Crowns: An In Vitro Study. Int. J. Clin. Pediatr. Dent. 2020, 13, 57–60. [Google Scholar] [CrossRef]
- Jathar, P.; Panse, A.; Desai, A.R. Acrylic Crowns for Esthetic Rehabilitation of Primary Teeth. Int. J. Pedod. Rehabil. 2018, 3, 42. [Google Scholar] [CrossRef]
| Group | Product Name | Manufacturer | Resin Type |
|---|---|---|---|
| 1 | SR Ivocron | Ivoclar Vivadent, Liechtenstein | Cold-polymerized polymethyl methacrylate |
| 2 | SR Ivocron | Ivoclar Vivadent, Liechtenstein | Heat-polymerized polymethyl methacrylate |
| 3 | Protemp 4 | 3M Germany-ESPE | Auto-polymerized bis-acryl composite |
| 4 | Revotek LC | GC Corp, Tokyo | Light-polymerized urethane dimethacrylate resin |
| 95% Confidence Interval | |||||||
|---|---|---|---|---|---|---|---|
| (I) Group | (J) Group | Mean Difference (I−J) | Std. Error | Sig. | Lower Bound | Upper Bound | Remark |
| Cold | Heat | −14.09556 | 6.11505 | 0.118 | −30.6634 | 2.4723 | NS |
| Protemp | −7.27667 | 6.11505 | 0.637 | −23.8446 | 9.2912 | NS | |
| Revotek | 45.05778 * | 6.11505 | <0.01 | 28.4899 | 61.6257 | S | |
| Heat | Cold | 14.09556 | 6.11505 | 0.118 | −2.4723 | 30.6634 | NS |
| Protemp | 6.81889 | 6.11505 | 0.683 | −9.7490 | 23.3868 | NS | |
| Revotek | 59.15333 * | 6.11505 | <0.01 | 42.5854 | 75.7212 | S | |
| Protemp | Cold | 7.27667 | 6.11505 | 0.637 | −9.2912 | 23.8446 | NS |
| Heat | −6.81889 | 6.11505 | 0.683 | −23.3868 | 9.7490 | NS | |
| Revotek | 52.33444 * | 6.11505 | <0.01 | 35.7666 | 68.9023 | S | |
| Revotek | Cold | −45.05778 * | 6.11505 | <0.01 | −61.6257 | −28.4899 | S |
| Heat | −59.15333 * | 6.11505 | <0.01 | −75.7212 | −42.5854 | S | |
| Protemp | −52.33444 * | 6.11505 | <0.01 | −68.9023 | −35.7666 | S | |
| Sum of Squares | df | Mean Square | F | Sig. | |
|---|---|---|---|---|---|
| Between Groups | 19,274.279 | 3 | 6424.760 | 38.181 | <0.01 |
| Within Groups | 5384.720 | 32 | 168.272 | ||
| Total | 24,658.998 | 35 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Idrissi, H.A.; Annamma, L.M.; Sharaf, D.; Jaghsi, A.A.; Abutayyem, H. Comparative Evaluation of Flexural Strength of Four Different Types of Provisional Restoration Materials: An In Vitro Pilot Study. Children 2023, 10, 380. https://doi.org/10.3390/children10020380
Idrissi HA, Annamma LM, Sharaf D, Jaghsi AA, Abutayyem H. Comparative Evaluation of Flexural Strength of Four Different Types of Provisional Restoration Materials: An In Vitro Pilot Study. Children. 2023; 10(2):380. https://doi.org/10.3390/children10020380
Chicago/Turabian StyleIdrissi, Hafsa Al, Lovely Muthiah Annamma, Dalya Sharaf, Ahmad Al Jaghsi, and Huda Abutayyem. 2023. "Comparative Evaluation of Flexural Strength of Four Different Types of Provisional Restoration Materials: An In Vitro Pilot Study" Children 10, no. 2: 380. https://doi.org/10.3390/children10020380
APA StyleIdrissi, H. A., Annamma, L. M., Sharaf, D., Jaghsi, A. A., & Abutayyem, H. (2023). Comparative Evaluation of Flexural Strength of Four Different Types of Provisional Restoration Materials: An In Vitro Pilot Study. Children, 10(2), 380. https://doi.org/10.3390/children10020380







