Abstract
This study aimed to identify predictors for successful post-treatment outcomes in early orthopedic class III malocclusion treatment with a facemask and hyrax expander appliance. The study was performed on lateral cephalograms from 37 patients at the start of treatment (T0), post-treatment (T1), and a minimum of three years after treatment (T2). The patients were grouped as stable or unstable according to the existence of a 2-mm overjet at T2. For statistical analysis, independent t-tests were used to compare the baseline characteristics and measurements of the two groups, considering a significance level of < 0.05. Thirty variables of pretreatment cephalograms were considered during logistic regression analysis to identify predictors. A discriminant equation was established using a stepwise method. The success rate and area under the curve were calculated, with AB to the mandibular plane, ANB, ODI, APDI, and A–B plane angles as predictors. The A–B plane angle was the most significantly different between the stable and unstable groups. In terms of the A–B plane angle, the success rate of early class III treatment with a facemask and hyrax expander appliance was 70.3%, and the area under the curve indicated a fair grade.
1. Introduction
Class III malocclusion is among the most challenging conditions to address with orthodontic treatment [1]. The prevalence of skeletal class III malocclusion varies widely among ethnic groups and different geographic regions. As reported in a previous review, prevalence rates are less than 8.3% in the United States, 3–5% in Brazil, 5% in the south of Italy, 2.8% in Germany, 2.3–14% in Japan, and 9–19% in South Korea [2]. These reports suggest a much higher rate of class III malocclusion among Asians than other ethnic groups.
The etiology of class III malocclusion is varied and complex, and this condition is associated with both genetic and environmental factors [3,4]. Moreover, several environmental factors can be involved in exacerbating class III malocclusion: oral habits, respiratory problems (enlarged tonsils and mouth breathing), incorrect posture, and congenital anatomic defects [5,6,7]. A previous study suggested that patients with unilateral cleft lip and palate exhibit delayed maxillary development similar to individuals with class III malocclusion [8]. Because of these many different factors, accurately predicting the possibility of success or failure after early orthopedic class III treatment is challenging, but it is necessary to facilitate the selection of the appropriate treatment protocols for good long-term outcomes.
Previous studies only evaluated early treatment of class III malocclusion in mixed dentition for a short-term period. Although recent systematic reviews suggested that the early treatment of class III malocclusion is effective in the short term, there is a lack of evidence on long-term benefits [9,10]. Another systematic review predicted the success of early treatment of class III malocclusion with different appliances, such as a chin cup, a facemask, a combination of chin cup and facemask, a facemask in combination with rapid maxillary expansion, cervical headgear, and functional appliances. It concluded that the accurate prediction of the orthopedic treatment outcomes of class III malocclusion was dubious because of the quality of the papers reviewed [11]. In addition, because of the large variety of predictors and differences among the developed prediction models, they doubted the existence of a universal predictor of the outcome of treatment of class III malocclusions [11].
Several prediction models have been suggested for short-term or long-term stability after early orthopedic class III treatment. For each prediction model, a variety of cephalometric predictors have been reported, such as the AB-mandibular plane angle, Wits appraisal, articular angle, N-perpendicular to point A, length of mandibular ramus, angulation of cranial base, inclination of mandibular plane to cranial base, lower face height, gonial angle, the position of the condyle with reference to cranial base, ramal length, and mandibular length [12,13,14,15,16,17,18,19,20,21,22,23]. However, some prediction models have low prediction accuracy [12,21]. In fact, use of fewer predictors in discriminant analysis is more useful in clinical practice, because it simplifies the treatment prediction and minimizes measurement errors. This leads to a null hypothesis: a model with a universal predictor would be established to improve predictive accuracy in patients with early orthopedic class III treatment.
This retrospective study aimed to identify predictors of initial skeletal morphology in patients with class III malocclusion and to establish a novel model with a universal predictor for successful post-treatment outcomes of a facemask and hyrax expander appliance using discriminant analysis.
2. Materials and Methods
In this study, patients seen between April 2004 and April 2015 at the Department of Pediatric Dentistry, Jeonbuk National University Dental Hospital, were considered. The following inclusion criteria were applied: (1) skeletal class Ⅲ malocclusion in the primary and permanent dentition characterized by an anterior crossbite and a Wits appraisal of –2.0 mm or less; (2) lateral cephalograms available for pretreatment (T0), post-treatment (T1), and a minimum of three years after treatment (T2); and (3) orthopedic treatment with a facemask and hyrax expander appliance, including maxilla protraction by semi-rapid expansion (one-quarter turn every other day) and the wearing of a facemask for at least 14 h per day. In the T1–T2 period, the patients wore a class III activator as a retainer at night for one year. The exclusion criteria were the existence of craniofacial syndrome and the application of orthopedic treatment using other modalities. This study was conducted following approval by the Institutional Review Board of Jeonbuk National University Hospital (No. CUH 2019-05-012, approved 1 June 2019).
Initially, a sample of 171 patients with class III malocclusion in the primary and mixed dentition was included. After screening the inclusion and exclusion criteria, a final total of 37 patients (mean age: 6.6 years) was selected for this study. According to the existence of an overjet of 2 mm after the completion of treatment (T2), the subjects were divided into stable (overjet > 2 mm) and unstable (overjet < 2 mm) groups. The following clinical data were collected through a chart review: sex (male or female), family history (is there a family history of mandibular prognathism?), rhinitis (is there rhinitis?), mouth breathing (is there chronic oral ventilation?), adenoid and tonsil hypertrophy (are there enlarged tonsils and adenoids?), oral habits (are there bad oral habits?), and cooperation (good or bad).
Cephalometric analysis was performed at T0 and computed using V-Ceph software (version 6.0; Osstem, Seoul, South Korea), including 18 landmarks and 30 variables (linear and angular measurements). In this study, a third-year dental resident traced each lateral cephalogram. Before performing cephalometric analysis, the intra-rater reliability was evaluated. Eight lateral cephalograms were randomly selected from patients included in the study and were analyzed at two different times within one week. In both instances, the measurements obtained for each patient were analyzed through intraclass coefficient correlation (ICC). The ICC oscillated between 0.933 for the SNA angle and 0.991 for the SN to FH plane. These values indicated a high level of intra-rater concordance. Landmark positions and linear and angular measurements are presented in Figure 1, Figure 2 and Figure 3, respectively. The details of cephalometric landmarks and linear and angular measurements are described in Table 1. In addition, the analyses of lateral cephalograms were stratified according to six skeletal aspects: the cranial base (SN to FH, anterior cranial base, posterior cranial base, and saddle), maxilla (midfacial length), mandible (mandibular body length, mandibular ramus height, mandibular plane angle, mandibular length, and gonial angle), anteroposterior relationships (SNA, A point to N perpendicular, SNB, pogonion to N perpendicular, ANB, Wits, articular angle, and APDI), vertical relationships (sum, SN-GoGn, Y-axis to FH, ODI, AB to the mandibular plane, A–B plane angle, facial axis, FMA, and AB to the occlusal plane), and dental relationships (U1 to SN, L1 to NB, and IMPA).
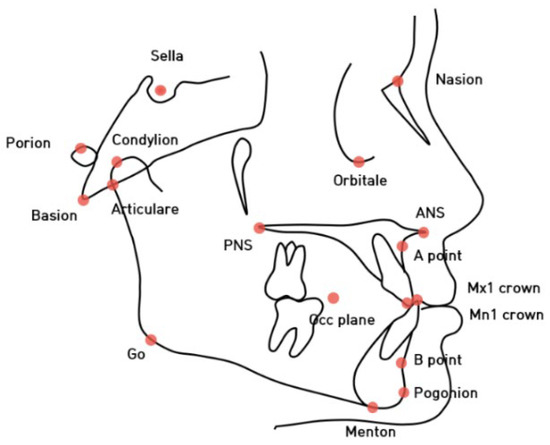
Figure 1.
The cephalometric landmarks used in this study.
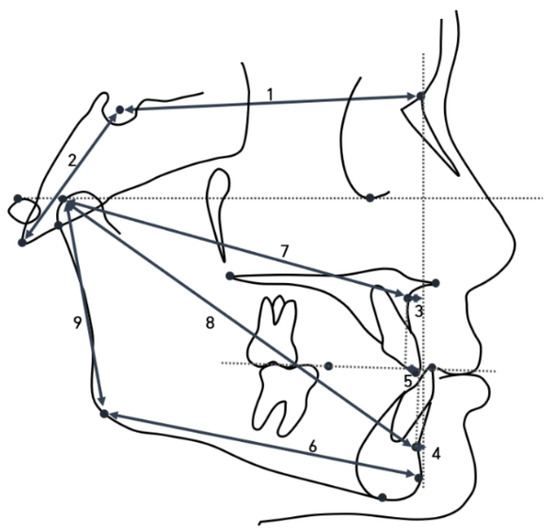
Figure 2.
Linear measurements used in this study. 1, anterior cranial base; 2, posterior cranial base; 3, A point to N perpendicular; 4, pogonion to N perpendicular; 5, intermaxillary position to occlusal plane; 6, mandibular body length; 7, midfacial length; 8, mandibular length; and 9, mandibular ramus height.
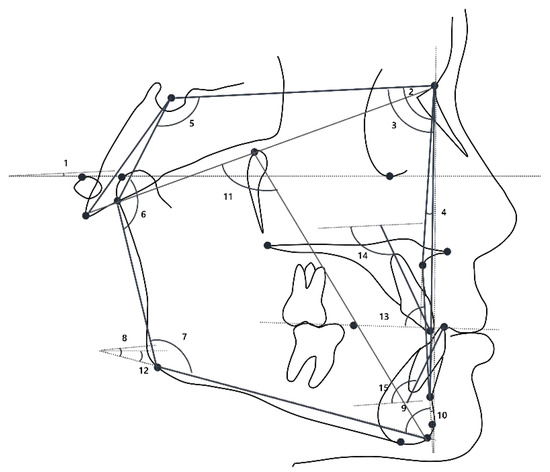
Figure 3.
Angular measurements used in this study. 1, SN to the FH plane; 2, SNA angle; 3, SNB angle; 4, ANB angle; 5, saddle angle; 6, articular angle; 7, gonial angle; 8, SN-GoGn; 9, AB to the mandibular plane; 10, A–B plane angle; 11, facial axis; 12, mandibular plane angle; 13, A-B to the occlusal plane; 14, inclination of upper incisor; and 15, inclination of lower incisor.

Table 1.
Descriptions of cephalometric landmarks, linear, and angular measurements.
Statistical Analyses
All data were statistically analyzed using SPSS software (version 23.0, IBM, Chicago, CA, USA) with a significance level of p < 0.05. Independent t-tests were performed to compare baseline characteristics and cephalometric measurements between the stable and unstable groups. In addition, 30 variables of the lateral cephalograms at T0 were used in logistic regression analysis to identify key variables to distinguish between the stable and unstable groups. A stepwise method was applied to establish a discriminant equation with a universal variable. Using the discriminant equation, we stratified study participants into stable and unstable groups and calculated the success rate of prognosis. The success rate was based on accurate predictions of stable and unstable groups at T0 and T2.
For the evaluation of a predictive model, the area under the curve (AUC) was analyzed. In addition, the AUC value was classified as excellent (0.9–1.0), good (0.8–0.9), fair (0.7–0.8), poor (0.6–0.7), and failed (0.5–0.6) [24].
3. Results
3.1. Study Participant Characteristics
The mean age of the included patients at T0, T1, and T2 was 6.6 ± 1.7 years, 8.4 ± 1.8 years, and 13.7 ± 2.9 years, respectively, while the mean length of the treatment period (T0–T1) was 13.8 ± 5.2 months (Table 2). In addition, there were no significant differences between the stable and unstable groups in terms of sex, family history, rhinitis, mouth breathing, adenoid or tonsil hypertrophy, oral habits, or cooperation (Table 3).

Table 2.
Demographic characteristics of the study participants.

Table 3.
Comparison of baseline characteristics between the stable and unstable groups.
3.2. Cephalometric Analysis
Differences between the stable and the unstable groups across the six skeletal aspects, including the cranial base, maxilla, mandible, vertical relationships, anteroposterior relationships, and dental relationships, were evaluated (Table 4).

Table 4.
Comparison of the two study groups in the initial stage.
The stable group had a larger ANB angle, smaller APDI angle, larger ODI angle, larger AB to mandibular plane angle, and smaller A–B plane angle compared with the unstable group (p < 0.05). Other variables were not significantly different (p > 0.05).
3.3. Discriminant and AUC Analysis
Five variables including AB to the mandibular plane, ANB, ODI, APDI, and A–B plane angles were used for discriminant analysis. In a stepwise manner, one variable suitable for distinguishing between the two groups (the most significant variable) was extracted, which was the A–B plane angle.
As shown in Table 5, unstandardized discriminant function coefficients of the selected predictive variable with a calculated constant established the following equation, which yields individual scores for assigning new patients to the stable or unstable group:
Individual score = 0.454 (A–B plane angle) − 0.013

Table 5.
Stepwise discriminant analysis.
The critical score (mean value distinguishing between stable and unstable groups) was set to 0.000662. If a new patient with class III malocclusion showed that the individual score was lower than 0.000662, then the prognosis of early orthopedic treatment with a facemask and hyrax expander appliance was considered stable.
The success rate of the predictive model was 70.3%, as shown in Table 6. Regarding the predictability of treatment of skeletal class III malocclusion, the sensitivity and specificity values were 0.68 and 0.72, respectively. Furthermore, fair prediction performance (AUC of 0.724) of the discriminant function was achieved (Table 7).

Table 6.
Classification results of discriminant analysis.

Table 7.
The AUC values of the discriminant function.
4. Discussion
In this study, AB to the mandibular plane, ANB, ODI, APDI, and A–B plane angles were predictors of short-term prognosis in early orthopedic class III treatment. This suggested that the presence of increased vertical proportions and reduced overjet are indicators that early intervention might be less successful in the short term. A previous systematic review of 14 studies reported 35 cephalometric predictors of treatment outcome (20 linear, 13 angular, and two ratios) [11]. Apart from ODI, our predictors were reported in this review and in recent studies [12,25].
Among the five variables, the A–B plane angle showed the most significant difference between the stable and unstable groups and was the first variable to enter the stepwise discriminant model, suggesting that the A–B plane angle could be the best skeletal measurement for the prediction of class III early treatment. In addition, two previous studies established predictive models for Koreans [12,13], which were compared with our predictive model. Due to differences in subject age, follow-up duration, the method of early orthopedic treatment, and success criteria, the significant variables assigned to the equations were different among the studies.
The prediction model demonstrated moderate accuracy for the prognosis of early class III treatment in the short-term follow-up (70.3%). This discriminant will be helpful to clinicians and can be used to evaluate early orthopedic treatment, especially in skeletal Class III malocclusion in growing children. It may also help determine whether additional orthopedic treatment is needed before or during peak pubertal growth.
Although there are differences in patient characteristics, treatment protocols, success criteria, and evaluation time, the success rate of our study was higher than that reported in previous studies [12,13,15,16]. The success rate in some previous studies might have been lower because the treatment outcome was assessed after the confirmation of the completion of facial growth. There could have been late mandibular growth in some patients. Ghiz et al. collected data 3 years after treatment [16], Choi et al. collected data when their patients were approximately 19 years of age [12], and the authors of the remaining two studies collected data when their patients were approximately 17 years old [13,15]. In addition, our model had an AUC value of 0.724, which was a fair grade for prediction. The sensitivity and specificity values between our study and the previous investigations did not indicate a significant difference. Therefore, in comparison with other studies, our model demonstrated stability for predicting short-term outcomes in class III patients receiving early orthopedic treatment with a facemask and hyrax expander appliance.
Regarding early treatment protocols for class III malocclusion, facemasks and rapid maxillary expanders have been shown to be effective for enhancing maxillary growth and improving the overjet [26]. In a previous study, it was suggested that rapid maxillary expansion (two-quarter turns per day) and semi-rapid maxillary expansion (one-quarter turn every other day) have similar effects on dentofacial structure both in the transverse, vertical, and sagittal planes [27]. In combination with expansion therapy, a facemask is also used to improve the effectiveness of maxillary protraction. From a systematic review, clinicians suggested that a facemask should be used for 14–16 h a day [28]. In addition, a retainer with an activator is extremely important following orthopedic class III treatment to prevent relapse. Class III is not considered fully treated until growth is complete. Relapse is related to changes in dental tipping and maxillary rotation following the first month of facemask interruption [14,29,30].
Although our model with a universal predictor will help clinicians to simplify and improve prognosis prediction, some limitations influenced the success rate in this study. The first limitation of this retrospective study was that it was a short-term follow-up study conducted when the patient’s growth was not complete. Previous studies conducted in Korea showed that the mean age at T2 was 17.4 and 19.1 years, respectively [12,13]. However, the mean age at T2 was 13.7 ± 2.9 years in this study. The mean skeletal maturity index (SMI) for a 13-year-old male is SMI 6 [31], which means that skeletal growth is at the peak stage and therefore a remarkable amount of mandibular growth is expected. The patients who were classified into the stable group may eventually be classified into the unstable group in the long term. The final success of class III treatment should be evaluated after the completion of craniofacial growth.
The second limitation of this study was that the criteria used for determining the stable or unstable outcomes of treatment may be ambiguous. In our study, successful treatment was defined based on a 2-mm overjet at T2, for a total follow-up period of at least 3 years. However, overcorrection should be performed at T1 due to considering the relapse of anterior crossbite. Many clinicians recommended that the criterion for the successful orthopedic treatment of class III malocclusion should be more than 2 mm [32]. In previous studies, researchers used various criteria from 0 mm to 2 mm at T2 [12,16,18,21,33]. Since various criteria are observed in many class III malocclusion patients undergoing early orthodontic treatment, future studies will be needed to define clinical treatment outcomes.
Third, only hard tissue measurements were analyzed in this study. In further studies, it will be necessary to consider soft tissue measurements that may predict the treatment outcomes of skeletal class III cases. Finally, although we extracted information on major risk factors related to class III malocclusion, such as family history, oral habits, and patient medical history, we included only cephalometric variables in the analysis. We aimed to compare these findings with existing studies that created prediction models using only cephalometric variables. The performance of the predictive model should be improved by including important clinical information. Moreover, to achieve a higher performance for predicting the long-term outcomes of early orthopedic class III treatment, advanced methods such as machine learning or deep learning should be employed.
5. Conclusions
In early class III malocclusion treatment with a facemask and hyrax expander appliance, AB to the mandibular plane, ANB, ODI, APDI, and A–B plane angles were predictors of post-treatment outcomes. Furthermore, our prediction model using the A–B plane angle showed quite high accuracy. This model might be helpful for clinicians in terms of prognosis prediction and treatment decision making for growing patients with skeletal class Ⅲ malocclusion.
Author Contributions
Conceptualization, M.-S.L., V.N.T.L. and D.-W.L.; methodology, D.-W.L.; software, J.-G.K.; validation, J.-G.K., Y.-M.Y. and D.-W.L.; formal analysis, V.N.T.L.; investigation, M.-S.L.; resources, D.-W.L.; data curation, Y.-M.Y.; writing—original draft preparation, M.-S.L., V.N.T.L. and D.-W.L.; writing—review and editing, M.-S.L., V.N.T.L., J.-G.K. and D.-W.L.; visualization, Y.-M.Y.; supervision, D.-W.L.; project administration, D.-W.L.; funding acquisition, D.-W.L. All authors have read and agreed to the published version of the manuscript.
Funding
This paper was supported by research funds of Jeonbuk National University in 2022. Moreover, this work was supported by the Biomedical Research Institute, Jeonbuk National University Hospital.
Institutional Review Board Statement
This study was approved by the Institutional Review Board of Jeonbuk National University Hospital (No. CUH 2019-05-012).
Informed Consent Statement
The requirement for patient consent was waived since the present study was not a human subject research project specified in the Bioethics and Safety Act. Moreover, it was practically impossible to obtain the consent of the research subjects and the risk to these subjects was extremely low, since existing data were used in this retrospective study.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no conflicts of interest to declare.
References
- Al-Mozany, S.A.; Dalci, O.; Almuzian, M.; Gonzalez, C.; Tarraf, N.E.; Ali Darendeliler, M. A novel method for treatment of Class III malocclusion in growing patients. Prog. Orthod. 2017, 18, 40. [Google Scholar]
- Zere, E.; Chaudhari, P.K.; Sharan, J.; Dhingra, K.; Tiwari, N. Developing Class III malocclusions: Challenges and solutions. Clin. Cosmet. Investig. Dent. 2018, 10, 99–116. [Google Scholar]
- Moreno Uribe, L.M.; Miller, S.F. Genetics of the dentofacial variation in human malocclusion. Orthod. Craniofac. Res. 2015, 18 (Suppl. 1), 91–99. [Google Scholar]
- Weaver, C.A.; Miller, S.F.; da Fontoura, C.S.; Wehby, G.L.; Amendt, B.A.; Holton, N.E.; Allareddy, V.; Southard, T.E.; Moreno Uribe, L.M. Candidate gene analyses of 3-dimensional dentoalveolar phenotypes in subjects with malocclusion. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 539–558. [Google Scholar]
- William, R.; Proffit, H.W.F.; Larson, S.; Sarver, D.M. Contemporary Orthodontics, 6th ed.; Elsevier: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Harari, D.; Redlich, M.; Miri, S.; Hamud, T.; Gross, M. The effect of mouth breathing versus nasal breathing on dentofacial and craniofacial development in orthodontic patients. Laryngoscope 2010, 120, 2089–2093. [Google Scholar]
- Iwasaki, T.; Sato, H.; Suga, H.; Takemoto, Y.; Inada, E.; Saitoh, I.; Kakuno, E.; Kanomi, R.; Yamasaki, Y. Relationships among nasal resistance, adenoids, tonsils, and tongue posture and maxillofacial form in Class II and Class III children. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 929–940. [Google Scholar]
- Dogan, E.; Ergican, G.O.; Dogan, S. Maxillary Development in Patients with Unilateral Cleft Lip and Palate Compared with Individuals Having Skeletal Class I and Class III Malocclusion. J. Clin. Pediatr. Dent. 2021, 45, 140–145. [Google Scholar]
- Woon, S.C.; Thiruvenkatachari, B. Early orthodontic treatment for Class III malocclusion: A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 28–52. [Google Scholar]
- DiBiase, A.T.; Seehra, J.; Papageorgiou, S.N.; Cobourne, M.T. Do we get better outcomes from early treatment of Class III discrepancies? Br. Dent. J. 2022, 233, 197–201. [Google Scholar]
- Fudalej, P.; Dragan, M.; Wedrychowska-Szulc, B. Prediction of the outcome of orthodontic treatment of Class III malocclusions--a systematic review. Eur. J. Orthod. 2011, 33, 190–197. [Google Scholar]
- Choi, Y.J.; Chang, J.E.; Chung, C.J.; Tahk, J.H.; Kim, K.H. Prediction of long-term success of orthopedic treatment in skeletal Class III malocclusions. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 193–203. [Google Scholar]
- Moon, Y.M.; Ahn, S.J.; Chang, Y.I. Cephalometric predictors of long-term stability in the early treatment of Class III malocclusion. Angle Orthod. 2005, 75, 747–753. [Google Scholar]
- Baccetti, T.; Franchi, L.; McNamara, J.A., Jr. Cephalometric variables predicting the long-term success or failure of combined rapid maxillary expansion and facial mask therapy. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 16–22. [Google Scholar]
- Yoshida, I.; Yamaguchi, N.; Mizoguchi, I. Prediction of post-treatment outcome after combined treatment with maxillary protraction and chincap appliances. Eur. J. Orthod. 2006, 28, 89–96. [Google Scholar]
- Ghiz, M.A.; Ngan, P.; Gunel, E. Cephalometric variables to predict future success of early orthopedic Class III treatment. Am J Orthod Dentofac. Orthop 2005, 127, 301–306. [Google Scholar]
- Ferro, A.; Nucci, L.P.; Ferro, F.; Gallo, C. Long-term stability of skeletal Class III patients treated with splints, Class III elastics, and chincup. Am. J. Orthod Dentofac. Orthop 2003, 123, 423–434. [Google Scholar]
- Ko, Y.I.; Baek, S.H.; Mah, J.; Yang, W.S. Determinants of successful chincup therapy in skeletal class III malocclusion. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 33–41. [Google Scholar]
- Schuster, G.; Lux, C.J.; Stellzig-Eisenhauer, A. Children with class III malocclusion: Development of multivariate statistical models to predict future need for orthognathic surgery. Angle Orthod. 2003, 73, 136–145. [Google Scholar]
- Tahmina, K.; Tanaka, E.; Tanne, K. Craniofacial morphology in orthodontically treated patients of class III malocclusion with stable and unstable treatment outcomes. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 681–690. [Google Scholar]
- Wells, A.P.; Sarver, D.M.; Proffit, W.R. Long-term efficacy of reverse pull headgear therapy. Angle Orthod. 2006, 76, 915–922. [Google Scholar]
- Zentner, A.; Doll, G.M. Size discrepancy of apical bases and treatment success in angle Class III malocclusion. J. Orofac. Orthop. 2001, 62, 97–106. [Google Scholar]
- Zentner, A.; Doll, G.M.; Peylo, S.M. Morphological parameters as predictors of successful correction of Class III malocclusion. Eur. J. Orthod. 2001, 23, 383–392. [Google Scholar]
- Obuchowski, N.A. Receiver operating characteristic curves and their use in radiology. Radiology 2003, 229, 3–8. [Google Scholar]
- Souki, B.Q.; Nieri, M.; Pavoni, C.; Pavan Barros, H.M.; Junqueira Pereira, T.; Giuntini, V.; Cozza, P.; Franchi, L. Development and validation of a prediction model for long-term unsuccess of early treatment of Class III malocclusion. Eur. J. Orthod. 2020, 42, 200–205. [Google Scholar]
- Baccetti, T.; Rey, D.; Angel, D.; Oberti, G.; McNamara, J.A., Jr. Mandibular cervical headgear vs rapid maxillary expander and facemask for orthopedic treatment of Class III malocclusion. Angle Orthod. 2007, 77, 619–624. [Google Scholar]
- Ramoglu, S.I.; Sari, Z. Maxillary expansion in the mixed dentition: Rapid or semi-rapid? Eur. J. Orthod. 2010, 32, 11–18. [Google Scholar]
- Yepes, E.; Quintero, P.; Rueda, Z.V.; Pedroza, A. Optimal force for maxillary protraction facemask therapy in the early treatment of class III malocclusion. Eur. J. Orthod. 2014, 36, 586–594. [Google Scholar]
- Baccetti, T.; McGill, J.S.; Franchi, L.; McNamara, J.A., Jr.; Tollaro, I. Skeletal effects of early treatment of Class III malocclusion with maxillary expansion and face-mask therapy. Am. J. Orthod. Dentofac. Orthop. 1998, 113, 333–343. [Google Scholar]
- Cha, K.S. Skeletal changes of maxillary protraction in patients exhibiting skeletal class III malocclusion: A comparison of three skeletal maturation groups. Angle Orthod. 2003, 73, 26–35. [Google Scholar]
- Lee, Y.; Mah, Y. Skeletal Age Assessment of SMI and MP3 Stages to Predict the Pubertal Growth Spurt. J. Korean Acad. Pediatr. Dent. 2019, 46, 233–238. [Google Scholar]
- Tejedor, N.; Martin, C.; Alarcon, J.A.; Oteo-Calatayud, M.D.; Palma-Fernandez, J.C. Sexual dimorphism in the long-term stability (10 years) of skeletal Class III treatment. Prog. Orthod. 2021, 22, 13. [Google Scholar]
- Ngan, P.; Wei, S.H.Y. Early Treatment of Class III Patients To Improve Facial Aesthetics and Predict Future Growth. Hong Kong Dent. J. 2004, 1, 28–34. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).