Affiliation to a Social Group as a Preventive Factor in Suicidal Behaviors in Children and Adolescents during the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
3. Risk and Protective Factors for Suicide Behaviors
4. Suicide vs. Group Affiliation
4.1. Origin
4.2. Indigenous Children
4.3. Religion
4.4. Family and Peer Group
4.5. Immigration
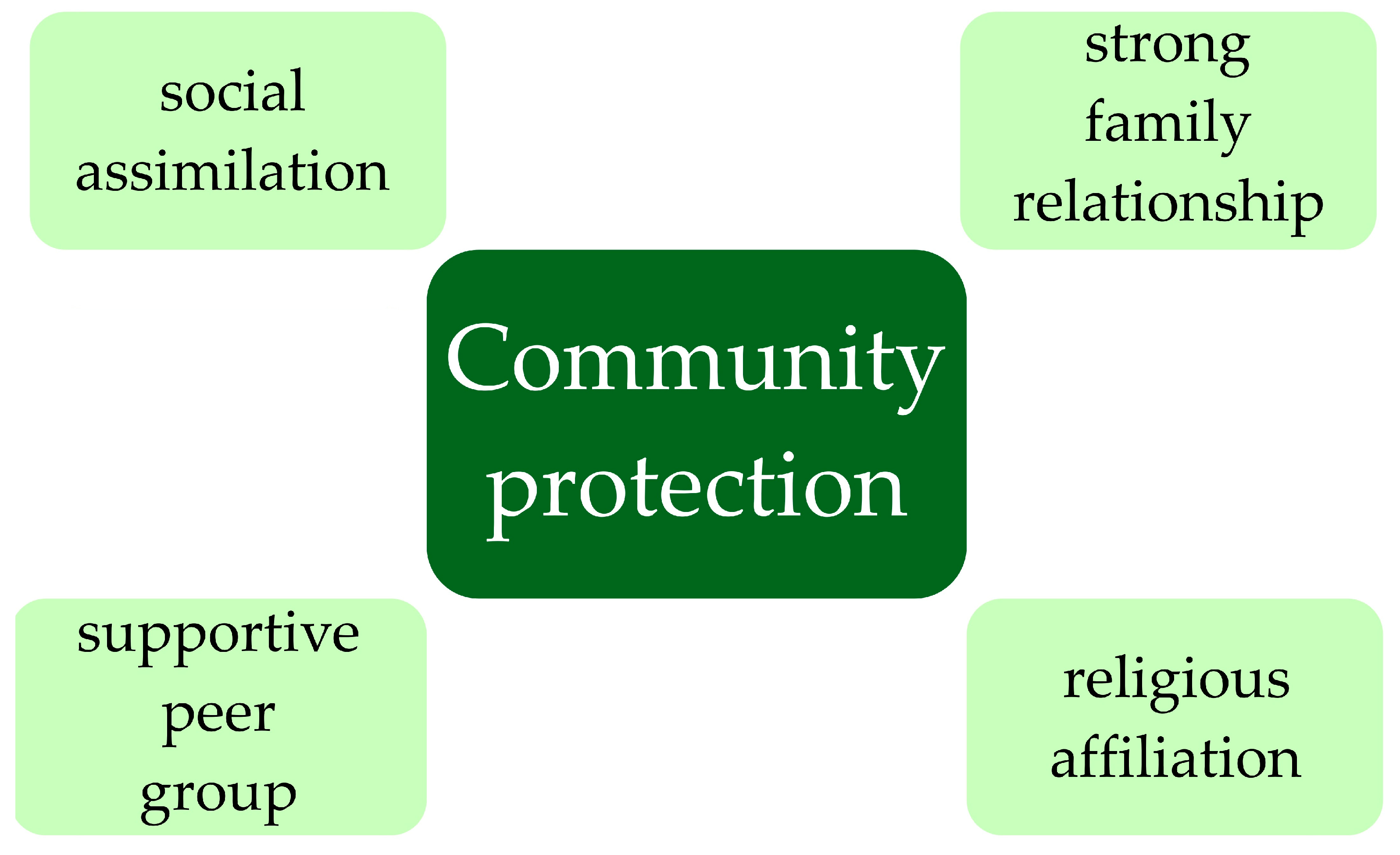
5. Community as a Protective Factor
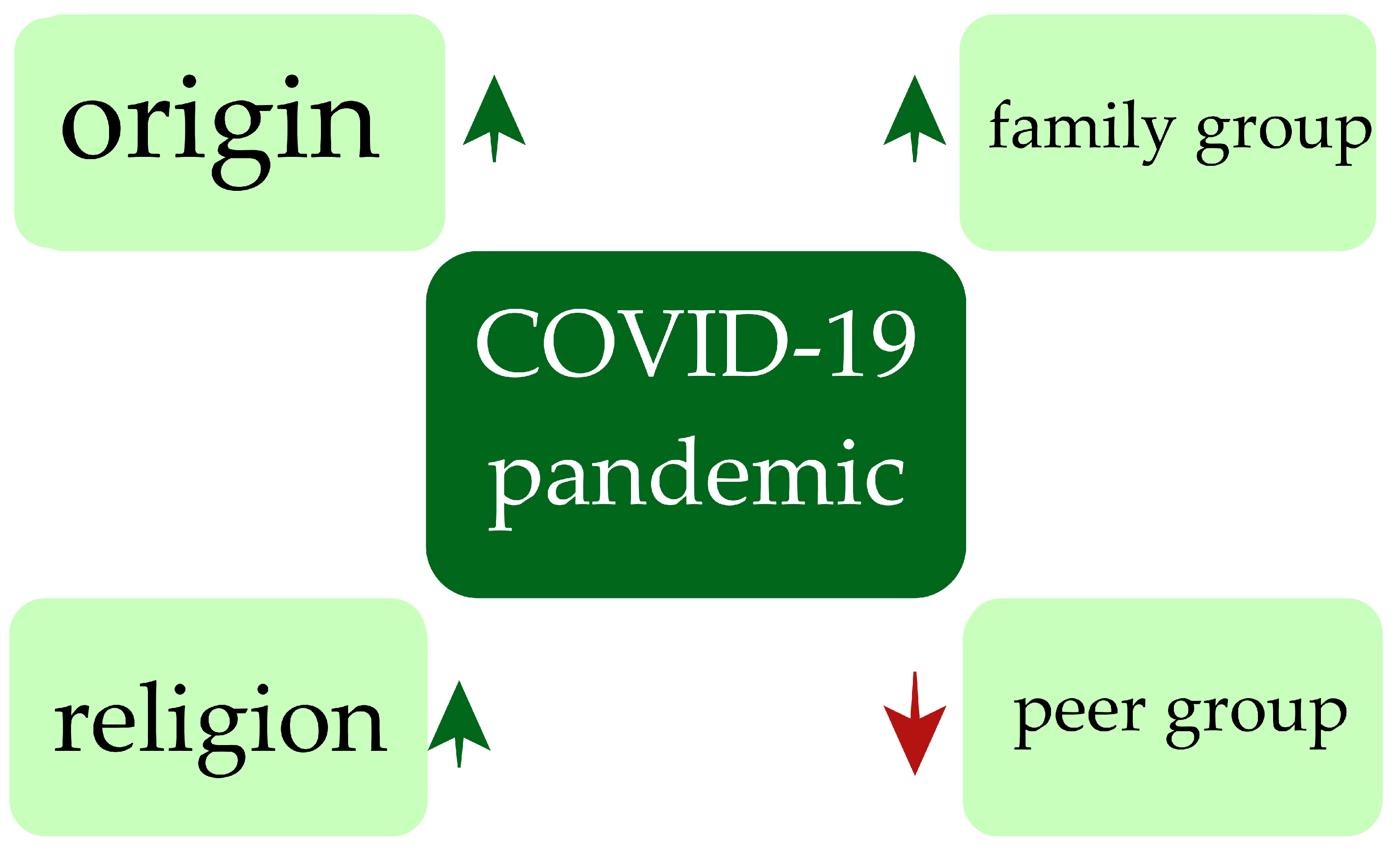
6. Suicide Behaviors during the COVID-19 Pandemic
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- John, A.; Glendenning, A.C.; Marchant, A.; Montgomery, P.; Stewart, A.; Wood, S.; Lloyd, K.; Hawton, K. Self-Harm, Suicidal Behaviours, and Cyberbullying in Children and Young People: Systematic Review. J. Med. Internet Res. 2018, 20, e129. [Google Scholar] [CrossRef] [PubMed]
- Astrup, H.; Myhre, M.; Kildahl, A.T.; Walby, F.A. Suicide After Contact With Child and Adolescent Mental Health Services—A National Registry Study. Front. Psychiatry 2022, 13, 886070. [Google Scholar] [CrossRef] [PubMed]
- Breslin, K.; Balaban, J.; Shubkin, C.D. Adolescent suicide: What can pediatricians do? Curr. Opin. Pediatr. 2020, 32, 595–600. [Google Scholar] [CrossRef]
- Ruch, D.A.; Heck, K.M.; Sheftall, A.H.; Fontanella, C.A.; Stevens, J.; Zhu, M.; Horowitz, L.M.; Campo, J.V.; Bridge, J.A. Characteristics and Precipitating Circumstances of Suicide Among Children Aged 5 to 11 Years in the United States, 2013–2017. JAMA Netw. Open 2021, 4, e2115683. [Google Scholar] [CrossRef]
- Hawton, K.; Hill, N.T.M.; Gould, M.; John, A.; Lascelles, K.; Robinson, J. Clustering of suicides in children and adolescents. Lancet Child Adolesc. Health 2020, 4, 58–67. [Google Scholar] [CrossRef]
- Carli, V.; Hoven, C.W.; Wasserman, C.; Chiesa, F.; Guffanti, G.; Sarchiapone, M.; Apter, A.; Balazs, J.; Brunner, R.; Corcoran, P.; et al. A newly identified group of adolescents at “invisible” risk for psychopathology and suicidal behavior: Findings from the SEYLE study. World Psychiatry 2014, 13, 78–86. [Google Scholar] [CrossRef]
- Wasserman, D.; Carli, V.; Iosue, M.; Javed, A.; Herrman, H. Suicide prevention in childhood and adolescence: A narrative review of current knowledge on risk and protective factors and effectiveness of interventions. Asia-Pac. Psychiatry 2021, 13, e12452. [Google Scholar] [CrossRef]
- Charpignon, M.-L.; Ontiveros, J.; Sundaresan, S.; Puri, A.; Chandra, J.; Mandl, K.D.; Majumder, M.S. Evaluation of Suicides Among US Adolescents During the COVID-19 Pandemic. JAMA Pediatr. 2022, 176, 724. [Google Scholar] [CrossRef]
- Gould, M.S.; Wallenstein, S.; Kleinman, M.H.; O’Carroll, P.; Mercy, J. Suicide clusters: An examination of age-specific effects. Am. J. Public Health 1990, 80, 211–212. [Google Scholar] [CrossRef]
- Swedo, E.A.; Beauregard, J.L.; de Fijter, S.; Werhan, L.; Norris, K.; Montgomery, M.P.; Rose, E.B.; David-Ferdon, C.; Massetti, G.M.; Hillis, S.D.; et al. Associations Between Social Media and Suicidal Behaviors During a Youth Suicide Cluster in Ohio. J. Adolesc. Health 2021, 68, 308–316. [Google Scholar] [CrossRef]
- Cho, Y.-J. Are Korean children free from suicide? Risk and protective factors within a transactional–ecological perspective. J. Child Health Care 2020, 24, 473–485. [Google Scholar] [CrossRef] [PubMed]
- Ong, M.; Lakoma, M.; Bhosrekar, S.G.; Hickok, J.; McLean, L.; Murphy, M.; Poland, R.E.; Purtell, N.; Ross-Degnan, D. Risk factors for suicide attempt in children, adolescents, and young adults hospitalized for mental health disorders. Child Adolesc. Ment. Health 2021, 26, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Ati, N.A.L.; Paraswati, M.D.; Windarwati, H.D. What are the risk factors and protective factors of suicidal behavior in adolescents? A systematic review. J. Child Adolesc. Psychiatr. Nurs. 2021, 34, 7–18. [Google Scholar] [CrossRef]
- Turecki, G.; Brent, D.A. Suicide and suicidal behaviour. Lancet 2016, 387, 1227–1239. [Google Scholar] [CrossRef] [PubMed]
- Kõlves, K.; de Leo, D. Suicide methods in children and adolescents. Eur. Child Adolesc. Psychiatry 2017, 26, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, R.E.; Oquendo, M.A.; Stanley, B. Religion and Suicide Risk: A Systematic Review. Arch. Suicide Res. 2016, 20, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Sedgwick, R.; Epstein, S.; Dutta, R.; Ougrin, D. Social media, internet use and suicide attempts in adolescents. Curr. Opin. Psychiatry 2019, 32, 534–541. [Google Scholar] [CrossRef]
- Filho, O.C.D.S.; Minayo, M.C.D.S. Triplo tabu: Sobre o suicídio na infância e na adolescência. Cien Saude Colet 2021, 26, 2693–2698. [Google Scholar] [CrossRef]
- Janiri, D.; Doucet, G.E.; Pompili, M.; Sani, G.; Luna, B.; Brent, D.A.; Frangou, S. Risk and protective factors for childhood suicidality: A US population-based study. Lancet Psychiatry 2020, 7, 317–326. [Google Scholar] [CrossRef]
- Hirsch, J.L.; Clark, M.S. Multiple Paths to Belonging That We Should Study Together. Perspect. Psychol. Sci. 2019, 14, 238–255. [Google Scholar] [CrossRef]
- García, F.E.; Villagrán, L.; Ahumada, M.C.; Inzunza, N.; Schuffeneger, K.; Garabito, S. Sense of Ethnic Belonging: Relation With Well-Being and Psychological Distress in Inhabitants of the Mapuche Conflict Area, Chile. Front. Psychol. 2021, 11, 617465. [Google Scholar] [CrossRef] [PubMed]
- Busolo, D.S.; Woodgate, R.L. Palliative care experiences of adult cancer patients from ethnocultural groups: A qualitative systematic review protocol. JBI Database Syst. Rev. Implement. Rep. 2015, 13, 99–111. [Google Scholar] [CrossRef] [PubMed]
- Savolainen, I.; Kaakinen, M.; Sirola, A.; Oksanen, A. Addictive behaviors and psychological distress among adolescents and emerging adults: A mediating role of peer group identification. Addict. Behav. Rep. 2018, 7, 75–81. [Google Scholar] [CrossRef] [PubMed]
- McLaren, S.; Schurmann, J.; Jenkins, M. The Relationships Between Sense of Belonging to a Community GLB Youth Group; School, Teacher, and Peer Connectedness; and Depressive Symptoms: Testing of a Path Model. J. Homosex. 2015, 62, 1688–1702. [Google Scholar] [CrossRef]
- Daigle, M.S.; Labelle, R.J. Pilot Evaluation of a Group Therapy Program for Children Bereaved by Suicide. Crisis 2012, 33, 350–357. [Google Scholar] [CrossRef]
- Journot-Reverbel, K.; Raynaud, J.-P.; Bui, E.; Revet, A. Support groups for children and adolescents bereaved by suicide: Lots of interventions, little evidence. Psychiatry Res. 2017, 250, 253–255. [Google Scholar] [CrossRef]
- Cerel, J.; Padgett, J.H.; Reed, G.A. Support Groups for Suicide Survivors: Results of a Survey of Group Leaders. Suicide Life Threat. Behav. 2009, 39, 588–598. [Google Scholar] [CrossRef]
- Walker, R.S. After suicide: Coming together in kindness and support. Death Stud. 2017, 41, 635–638. [Google Scholar] [CrossRef]
- Weinstein, S.M.; Cruz, R.A.; Isaia, A.R.; Peters, A.T.; West, A.E. Child- and Family-Focused Cognitive Behavioral Therapy for Pediatric Bipolar Disorder: Applications for Suicide Prevention. Suicide Life Threat. Behav. 2018, 48, 797–811. [Google Scholar] [CrossRef] [PubMed]
- Pfeffer, C.R.; Jiang, H.; Kakuma, T.; Hwang, J.; Metsch, M. Group Intervention for Children Bereaved by the Suicide of a Relative. J. Am. Acad. Child Adolesc. Psychiatry 2002, 41, 505–513. [Google Scholar] [CrossRef]
- Miller, A.B.; Esposito-Smythers, C.; Leichtweis, R.N. Role of Social Support in Adolescent Suicidal Ideation and Suicide Attempts. J. Adolesc. Health 2015, 56, 286–292. [Google Scholar] [CrossRef] [PubMed]
- Barreau, P. Les groupes de parole: Une manière de dire pour se dire. Soins 2019, 64, 25–27. [Google Scholar] [CrossRef] [PubMed]
- Ali, B.; Rockett, I.R.H.; Miller, T.R.; Leonardo, J.B. Racial/Ethnic Differences in Preceding Circumstances of Suicide and Potential Suicide Misclassification Among US Adolescents. J. Racial Ethn. Health Disparities 2022, 9, 296–304. [Google Scholar] [CrossRef]
- Balis, T.; Postolache, T.T. Ethnic Differences in Adolescent Suicide in the United States. Int. J. Child Health Hum. Dev. 2008, 1, 281–296. [Google Scholar] [PubMed]
- Lee, C.S.; Wong, Y.J. Racial/ethnic and gender differences in the antecedents of youth suicide. Cult. Divers. Ethn. Minor. Psychol. 2020, 26, 532–543. [Google Scholar] [CrossRef]
- Wong, S.S.; Sugimoto-Matsuda, J.J.; Chang, J.Y.; Hishinuma, E.S. Ethnic Differences in Risk Factors For Suicide Among American High School Students, 2009: The Vulnerability of Multiracial and Pacific Islander Adolescents. Arch. Suicide Res. 2012, 16, 159–173. [Google Scholar] [CrossRef]
- Van Bergen, D.; Smit, J.; Van Balkom, A.; Van Ameijden, E.; Saharso, S. Suicidal Ideation in Ethnic Minority and Majority Adolescents in Utrecht, The Netherlands. Crisis 2008, 29, 202–208. [Google Scholar] [CrossRef]
- Kołodziej-Sarzyńska, M.; Majewska, M.; Juchnowicz, D.; Karakuła-Juchnowicz, H. Risk factors of suicide with reference to the theory of social integration by Émile Durkheim. Psychiatr. Pol. 2019, 53, 865–881. [Google Scholar] [CrossRef]
- Claassen, C.A.; Yip, P.S.; Corcoran, P.; Bossarte, R.M.; Lawrence, B.A.; Currier, G.W. National Suicide Rates a Century after Durkheim: Do We Know Enough to Estimate Error? Suicide Life Threat. Behav. 2010, 40, 193–223. [Google Scholar] [CrossRef]
- Choo, C.C.; Harris, K.M.; Chew, P.K.H.; Ho, R.C. Does ethnicity matter in risk and protective factors for suicide attempts and suicide lethality? PLoS ONE 2017, 12, e0175752. [Google Scholar] [CrossRef]
- Caqueo-Urízar, A.; Urzúa, A.; De Munter, K. Mental health of indigenous school children in Northern Chile. BMC Psychiatry 2014, 14, 11. [Google Scholar] [CrossRef]
- Young, C.; Hanson, C.; Craig, J.C.; Clapham, K.; Williamson, A. Psychosocial factors associated with the mental health of indigenous children living in high income countries: A systematic review. Int. J. Equity Health 2017, 16, 153. [Google Scholar] [CrossRef] [PubMed]
- Clifford, A.C.; Doran, C.M.; Tsey, K. A systematic review of suicide prevention interventions targeting indigenous peoples in Australia, United States, Canada and New Zealand. BMC Public Health 2013, 13, 463. [Google Scholar] [CrossRef] [PubMed]
- Stoor, J.P.A.; Berntsen, G.; Hjelmeland, H.; Silviken, A. “If you do not birget [manage] then you don’t belong here”: A qualitative focus group study on the cultural meanings of suicide among Indigenous Sámi in arctic Norway. Int. J. Circumpolar Health 2019, 78, 1565861. [Google Scholar] [CrossRef]
- Canetto, S.S. Language, culture, gender, and intersectionalities in suicide theory, research, and prevention: Challenges and changes. Suicide Life Threat. Behav. 2021, 51, 1045–1054. [Google Scholar] [CrossRef] [PubMed]
- Barker, B.; Goodman, A.; DeBeck, K. Reclaiming Indigenous identities: Culture as strength against suicide among Indigenous youth in Canada. Can. J. Public Health 2017, 108, e208–e210. [Google Scholar] [CrossRef]
- Hackett, C.; Feeny, D.; Tompa, E. Canada’s residential school system: Measuring the intergenerational impact of familial attendance on health and mental health outcomes. J. Epidemiol. Community Health 2016, 70, 1096–1105. [Google Scholar] [CrossRef]
- Elias, B.; Mignone, J.; Hall, M.; Hong, S.P.; Hart, L.; Sareen, J. Trauma and suicide behaviour histories among a Canadian indigenous population: An empirical exploration of the potential role of Canada’s residential school system. Soc. Sci. Med. 2012, 74, 1560–1569. [Google Scholar] [CrossRef]
- Soole, R.; Kõlves, K.; De Leo, D. Suicides in Aboriginal and Torres Strait Islander children: Analysis of Queensland Suicide Register. Aust. N. Z. J. Public Health 2014, 38, 574–578. [Google Scholar] [CrossRef]
- Hämäläinen, S.; Musial, F.; Salamonsen, A.; Graff, O.; Olsen, T.A. Sami yoik, Sami history, Sami health: A narrative review. Int. J. Circumpolar Health 2018, 77, 1454784. [Google Scholar] [CrossRef]
- Eckhoff, C.; Sørvold, M.T.; Kvernmo, S. Adolescent self-harm and suicidal behavior and young adult outcomes in indigenous and non-indigenous people. Eur. Child Adolesc. Psychiatry 2020, 29, 917–927. [Google Scholar] [CrossRef] [PubMed]
- Norko, M.A.; Freeman, D.; Phillips, J.; Hunter, W.; Lewis, R.; Viswanathan, R. Can Religion Protect Against Suicide? J. Nerv. Ment. Dis. 2017, 205, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Rezaeian, M. Suicide Among Young Middle Eastern Muslim Females. Crisis 2010, 31, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Ritter, K.; Zitterl, W.; Stompe, T. Religion and suicide-part 2: Confessions, religiousness, secularisation and national suicide rates. Neuropsychiatrie 2011, 25, 127–134. [Google Scholar]
- Bullock, M.; Nadeau, L.; Renaud, J. Spirituality and Religion in Youth Suicide Attempters’ Trajectories of Mental Health Service Utilization: The Year before a Suicide Attempt. J. Can. Acad. Child Adolesc. Psychiatry 2012, 21, 186–193. [Google Scholar]
- Gearing, R.E.; Alonzo, D. Religion and Suicide: New Findings. J. Relig. Health 2018, 57, 2478–2499. [Google Scholar] [CrossRef]
- Hilario, C.T.; Kamanzi, J.; Kennedy, M.; Gilchrist, L.; Richter, S. Peer support for youth suicide prevention: A scoping review protocol. BMJ Open 2021, 11, e048837. [Google Scholar] [CrossRef]
- Cui, S.; Cheng, Y.; Xu, Z.; Chen, D.; Wang, Y. Peer relationships and suicide ideation and attempts among Chinese adolescents. Child Care Health Dev. 2011, 37, 692–702. [Google Scholar] [CrossRef]
- Thomas, A.L.; Brausch, A.M. Family and peer support moderates the relationship between distress tolerance and suicide risk in black college students. J. Am. Coll. Health 2022, 70, 1138–1145. [Google Scholar] [CrossRef]
- Hybholt, L.; Higgins, A.; Buus, N.; Berring, L.L.; Connolly, T.; Erlangsen, A.; Morrissey, J. The Spaces of Peer-Led Support Groups for Suicide Bereaved in Denmark and the Republic of Ireland: A Focus Group Study. Int. J. Environ. Res. Public Health 2022, 19, 9898. [Google Scholar] [CrossRef]
- Oppenheimer, C.W.; Stone, L.B.; Hankin, B.L. The influence of family factors on time to suicidal ideation onsets during the adolescent developmental period. J. Psychiatr. Res. 2018, 104, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Grzejszczak, J.; Gabryelska, A.; Gmitrowicz, A.; Kotlicka-Antczak, M.; Strzelecki, D. Are Children Harmed by Being Locked up at Home? The Impact of Isolation during the COVID-19 Pandemic on the Phenomenon of Domestic Violence. Int. J. Environ. Res. Public Health 2022, 19, 13958. [Google Scholar] [CrossRef] [PubMed]
- Merrilees, C.E.; Taylor, L.K.; Goeke-Morey, M.C.; Shirlow, P.; Cummings, E.M.; Cairns, E. The protective role of group identity: Sectarian antisocial behavior and adolescent emotion problems. Child Dev. 2014, 85, 412–420. [Google Scholar] [CrossRef]
- Calear, A.L.; Christensen, H.; Freeman, A.; Fenton, K.; Grant, J.B.; van Spijker, B.; Donker, T. A systematic review of psychosocial suicide prevention interventions for youth. Eur. Child Adolesc. Psychiatry 2016, 25, 467–482. [Google Scholar] [CrossRef] [PubMed]
- Antia, K.; Boucsein, J.; Deckert, A.; Dambach, P.; Račaitė, J.; Šurkienė, G.; Jaenisch, T.; Horstick, O.; Winkler, V. Effects of International Labour Migration on the Mental Health and Well-Being of Left-Behind Children: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2020, 17, 4335. [Google Scholar] [CrossRef]
- Kusi-Mensah, K.; Omigbodun, O. Children left behind by parental migration in sub-Saharan Africa. Lancet Child Adolesc. Health 2020, 4, 261–262. [Google Scholar] [CrossRef] [PubMed]
- Valtolina, G.G.; Colombo, C. Psychological Well-Being, Family Relations, and Developmental Issues of Children Left Behind. Psychol. Rep. 2012, 111, 905–928. [Google Scholar] [CrossRef]
- Chang, H.; Yan, Q.; Tang, L.; Huang, J.; Ma, Y.; Ye, X.; Yu, Y. A comparative analysis of suicide attempts in left-behind children and non-left-behind children in rural China. PLoS ONE 2017, 12, e0178743. [Google Scholar] [CrossRef]
- Qu, G.; Shu, L.; Zhang, J.; Wu, Y.; Ma, S.; Han, T.; Zhang, H.; Wang, J.; Sun, Y. Suicide ideation, suicide plan, and suicide attempt among left-behind children and adolescents: A systematic review and meta-analysis. Suicide Life Threat. Behav. 2021, 51, 515–527. [Google Scholar] [CrossRef]
- Hou, X.; Wang, J.; Guo, J.; Zhang, X.; Liu, J.; Qi, L.; Zhou, L. Methods and efficacy of social support interventions in preventing suicide: A systematic review and meta-analysis. Evid. Based Ment. Health 2022, 25, 29–35. [Google Scholar] [CrossRef]
- Xiao, Y.; Chen, Y.; Chang, W.; Pu, Y.; Chen, X.; Guo, J.; Li, Y.; Yin, F. Perceived social support and suicide ideation in Chinese rural left-behind children: A possible mediating role of depression. J. Affect. Disord. 2020, 261, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Lapierre, S.; Erlangsen, A.; Waern, M.; De Leo, D.; Oyama, H.; Scocco, P.; Gallo, J.; Szanto, K.; Conwell, Y.; Draper, B.; et al. A Systematic Review of Elderly Suicide Prevention Programs. Crisis 2011, 32, 88–98. [Google Scholar] [CrossRef] [PubMed]
- Viola, T.W.; Nunes, M.L. Social and environmental effects of the COVID-19 pandemic on children. J. Pediatr. 2022, 98, S4–S12. [Google Scholar] [CrossRef] [PubMed]
- de Figueiredo, C.S.; Sandre, P.C.; Portugal, L.C.L.; Mázala-De-Oliveira, T.; da Silva Chagas, L.; Raony, Í.; Ferreira, E.S.; Giestal-De-Araujo, E.; dos Santos, A.A.; Bomfim, P.O.-S. COVID-19 pandemic impact on children and adolescents’ mental health: Biological, environmental, and social factors. Prog. Neuropsychopharmacol. Biol. Psychiatr. 2021, 106, 110171. [Google Scholar] [CrossRef]
- Zalsman, G.; Stanley, B.; Szanto, K.; Clarke, D.E.; Carli, V.; Mehlum, L. Suicide in the Time of COVID-19: Review and Recommendations. Arch. Suicide Res. 2020, 24, 477–482. [Google Scholar] [CrossRef]
- Bersia, M.; Koumantakis, E.; Berchialla, P.; Charrier, L.; Ricotti, A.; Grimaldi, P.; Dalmasso, P.; Comoretto, R.I. Suicide spectrum among young people during the COVID-19 pandemic: A systematic review and meta-analysis. EClinicalMedicine 2022, 54, 101705. [Google Scholar] [CrossRef]
- Hill, R.M.; Rufino, K.; Kurian, S.; Saxena, J.; Saxena, K.; Williams, L. Suicide Ideation and Attempts in a Pediatric Emergency Department Before and During COVID-19. Pediatrics 2021, 147, e2020029280. [Google Scholar] [CrossRef]
- Merayo-Cano, J.M.; Porras-Segovia, A.A.; Baca-García, E. COVID-19 impact vs. suicide impact in Spain. Rev. Psiquiatr. Salud Ment. 2022. [Google Scholar] [CrossRef]
- Isumi, A.; Doi, S.; Yamaoka, Y.; Takahashi, K.; Fujiwara, T. Do suicide rates in children and adolescents change during school closure in Japan? The acute effect of the first wave of COVID-19 pandemic on child and adolescent mental health. Child Abus. Negl. 2020, 110, 104680. [Google Scholar] [CrossRef]
- Tanaka, T.; Okamoto, S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat. Hum. Behav. 2021, 5, 229–238. [Google Scholar] [CrossRef]
- Mourouvaye, M.; Bottemanne, H.; Bonny, G.; Fourcade, L.; Angoulvant, F.; Cohen, J.F.; Ouss, L. Association between suicide behaviours in children and adolescents and the COVID-19 lockdown in Paris, France: A retrospective observational study. Arch. Dis. Child 2021, 106, 918–919. [Google Scholar] [CrossRef]
- Yard, E.; Radhakrishnan, L.; Ballesteros, M.F.; Sheppard, M.; Gates, A.; Stein, Z.; Hartnett, K.; Kite-Powell, A.; Rodgers, L.; Adjemian, J.; et al. Emergency Department Visits for Suspected Suicide Attempts Among Persons Aged 12–25 Years Before and During the COVID-19 Pandemic-United States, January 2019–May 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 888–894. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.J.; Kloess, J.A.; Gill, C.; Michail, M. Assessing and Responding to Suicide Risk in Children and Young People: Understanding Views and Experiences of Helpline Staff. Int. J. Environ. Res. Public Health 2022, 19, 10887. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Noh, Y.; Seo, J.Y.; Park, S.H.; Kim, M.H.; Won, S. Impact of the COVID-19 Pandemic on the Mental Health of Adolescent Students in Daegu, Korea. J. Korean Med. Sci. 2021, 36, e321. [Google Scholar] [CrossRef] [PubMed]
- Valdez-Santiago, R.; Villalobos, A.; Arenas-Monreal, L.; González-Forteza, C.; Hermosillo-De-La-Torre, A.E.; Benjet, C.; Wagner, F.A. Comparison of suicide attempts among nationally representative samples of Mexican adolescents 12 months before and after the outbreak of the Covid-19 pandemic. J. Affect. Disord. 2022, 298, 65–68. [Google Scholar] [CrossRef]
- Haw, C.; Hawton, K.; Gunnell, D.; Platt, S. Economic recession and suicidal behaviour: Possible mechanisms and ameliorating factors. Int. J. Soc. Psychiatry 2015, 61, 73–81. [Google Scholar] [CrossRef]
- Uphoff, E.P.; Lombardo, C.; Johnston, G.; Weeks, L.; Rodgers, M.; Dawson, S.; Seymour, C.; Kousoulis, A.A.; Churchill, R. Mental health among healthcare workers and other vulnerable groups during the COVID-19 pandemic and other coronavirus outbreaks: A rapid systematic review. PLoS ONE 2021, 16, e0254821. [Google Scholar] [CrossRef]
- Chiang, Y.-C.; Lin, Y.-J.; Li, X.; Lee, C.-Y.; Zhang, S.; Lee, T.S.-H.; Chang, H.-Y.; Wu, C.-C.; Yang, H.-J. Parents’ right strategy on preventing youngsters’ recent suicidal ideation: A 13-year prospective cohort study. J. Ment. Health 2022, 31, 374–382. [Google Scholar] [CrossRef]
- Ishimoto, Y.; Yamane, T.; Matsumoto, Y.; Takizawa, Y.; Kobayashi, K. The impact of gender differences, school adjustment, social interactions, and social activities on emotional and behavioral reactions to the COVID-19 pandemic among Japanese school children. SSM-Ment. Health 2022, 2, 100077. [Google Scholar] [CrossRef]
- Kandula, U.R.; Wake, A.D. Magnitude and Factors Affecting Parental Stress and Effective Stress Management Strategies among Family Members During COVID-19. Psychol. Res. Behav. Manag. 2022, 15, 83–93. [Google Scholar] [CrossRef]
- Karim, S.; Choukas-Bradley, S.; Radovic, A.; Roberts, S.R.; Maheux, A.J.; Escobar-Viera, C.G. Support over Social Media among Socially Isolated Sexual and Gender Minority Youth in Rural U.S. during the COVID-19 Pandemic: Opportunities for Intervention Research. Int. J. Environ. Res. Public Health 2022, 19, 15611. [Google Scholar] [CrossRef] [PubMed]
- Que, J.; Yuan, K.; Gong, Y.; Meng, S.; Bao, Y.; Lu, L. Raising awareness of suicide prevention during the COVID-19 pandemic. Neuropsychopharmacol. Rep. 2020, 40, 392–395. [Google Scholar] [CrossRef] [PubMed]
- Roe, J. Ethnicity and children’s mental health: Making the case for access to urban parks. Lancet Planet Health 2018, 2, e234–e235. [Google Scholar] [CrossRef] [PubMed]
- Pickett, K.E.; Wilkinson, R.G. People like us: Ethnic group density effects on health. Ethn. Health 2008, 13, 321–334. [Google Scholar] [CrossRef]
- Campo, M.; Mackie, D.M.; Sanchez, X. Emotions in Group Sports: A Narrative Review From a Social Identity Perspective. Front. Psychol. 2019, 10, 666. [Google Scholar] [CrossRef] [PubMed]
- Hefner, J.; Eisenberg, D. Social support and mental health among college students. Am. J. Orthopsychiatry 2009, 79, 491–499. [Google Scholar] [CrossRef] [PubMed]
- Meherali, S.; Punjani, N.; Louie-Poon, S.; Abdul Rahim, K.; Das, J.K.; Salam, R.A.; Lassi, Z.S. Mental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 3432. [Google Scholar] [CrossRef]
- Ye, J. Pediatric Mental and Behavioral Health in the Period of Quarantine and Social Distancing With COVID-19. JMIR Pediatr. Parent. 2020, 3, e19867. [Google Scholar] [CrossRef]
- Becker, M.; Correll, C.U. Suicidality in Childhood and Adolescence. Dtsch. Arztebl. Int. 2020, 117, 261–267. [Google Scholar] [CrossRef]
- Morthorst, B.R.; Harder, L.C.; Nylandsted, A.B.; Pagsberg, A.K. Suicide prevention clinics for children and adolescents in The Capital Region of Denmark. Ugeskr. Laeger 2021, 183, V09200693. [Google Scholar]
- Hardwick, T. Our Children are Killing Themselves: An Examination of Risk Factors, Protective Factors, and Best Practices for Addressing Suicidality Among African-American Youth. J. Natl. Black Nurses Assoc. 2021, 32, 49–55. [Google Scholar]
- Fleming, T.M.; Merry, S.N.; Robinson, E.M.; Denny, S.J.; Watson, P.D. Self-reported Suicide Attempts and Associated Risk and Protective Factors Among Secondary School Students in New Zealand. Aust. New Zealand J. Psychiatry 2007, 41, 213–221. [Google Scholar] [CrossRef]
- Hajek, A.; König, H.-H. Social Isolation and Loneliness of Older Adults in Times of the COVID-19 Pandemic: Can Use of Online Social Media Sites and Video Chats Assist in Mitigating Social Isolation and Loneliness? Gerontology 2021, 67, 121–124. [Google Scholar] [CrossRef] [PubMed]
- Graham, M.; Weale, V.; Lambert, K.A.; Kinsman, N.; Stuckey, R.; Oakman, J. Working at Home. J. Occup. Environ. Med. 2021, 63, 938–943. [Google Scholar] [CrossRef]
- Berk, M.S. Editorial: Suicide prevention in youth. Child Adolesc. Ment. Health 2022, 27, 325–327. [Google Scholar] [CrossRef]
- Busby, D.R.; Hatkevich, C.; McGuire, T.C.; King, C.A. Evidence-Based Interventions for Youth Suicide Risk. Curr. Psychiatry Rep. 2020, 22, 5. [Google Scholar] [CrossRef]
- Forte, A.; Sarli, G.; Polidori, L.; Lester, D.; Pompili, M. The Role of New Technologies to Prevent Suicide in Adolescence: A Systematic Review of the Literature. Medicina 2021, 57, 109. [Google Scholar] [CrossRef]
| Risk Factors | Protective Factors |
|---|---|
|
|
| Country | Suicidal Behavior in the COVID-19 Pandemic | Reference |
|---|---|---|
| Italy (Torino) | Children under the age of 19 showed a 15% increase | [73] |
| US (Texas) | Higher rates of SA in February, March, April, and July 2020 (1.58, 2.34, 1.75, and 1.77 times higher, respectively, for each month) compared to the same months in 2019 | [74] |
| Spain | People took their own lives in Spain in 2020, an increase of 7.4% over 2019 | [75] |
| Japan | Significant increase in suicide rates (by as much as 49%) during the second wave of the pandemic (July to October 2020) | [77] |
| Korea | More than 35% of students in this group have experienced an emotional crisis, possibly leading to SA | [81] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grzejszczak, J.; Strzelecki, D.; Gabryelska, A.; Kotlicka-Antczak, M. Affiliation to a Social Group as a Preventive Factor in Suicidal Behaviors in Children and Adolescents during the COVID-19 Pandemic. Children 2023, 10, 333. https://doi.org/10.3390/children10020333
Grzejszczak J, Strzelecki D, Gabryelska A, Kotlicka-Antczak M. Affiliation to a Social Group as a Preventive Factor in Suicidal Behaviors in Children and Adolescents during the COVID-19 Pandemic. Children. 2023; 10(2):333. https://doi.org/10.3390/children10020333
Chicago/Turabian StyleGrzejszczak, Jagoda, Dominik Strzelecki, Agata Gabryelska, and Magdalena Kotlicka-Antczak. 2023. "Affiliation to a Social Group as a Preventive Factor in Suicidal Behaviors in Children and Adolescents during the COVID-19 Pandemic" Children 10, no. 2: 333. https://doi.org/10.3390/children10020333
APA StyleGrzejszczak, J., Strzelecki, D., Gabryelska, A., & Kotlicka-Antczak, M. (2023). Affiliation to a Social Group as a Preventive Factor in Suicidal Behaviors in Children and Adolescents during the COVID-19 Pandemic. Children, 10(2), 333. https://doi.org/10.3390/children10020333





