Links between Childhood Obesity, High-Fat Diet, and Central Precocious Puberty
Abstract
1. Introduction
2. Methods
3. Obesity and Precocious Puberty
3.1. Childhood Obesity
3.2. Precocious Puberty
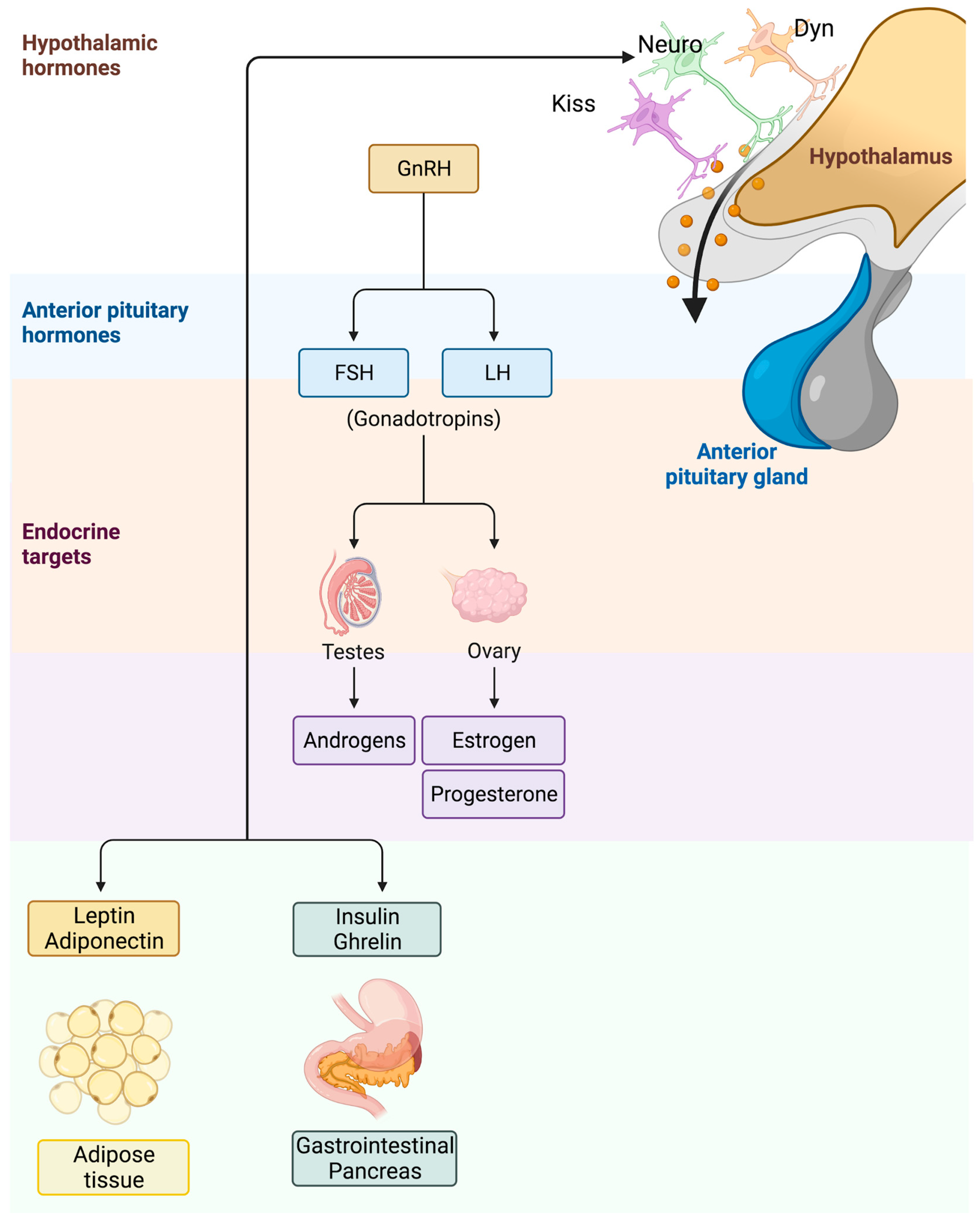
3.3. Precocious Puberty in Children with Obesity
4. High-Fat Diet in Children with Obesity
High-Fat Diet and Obesity
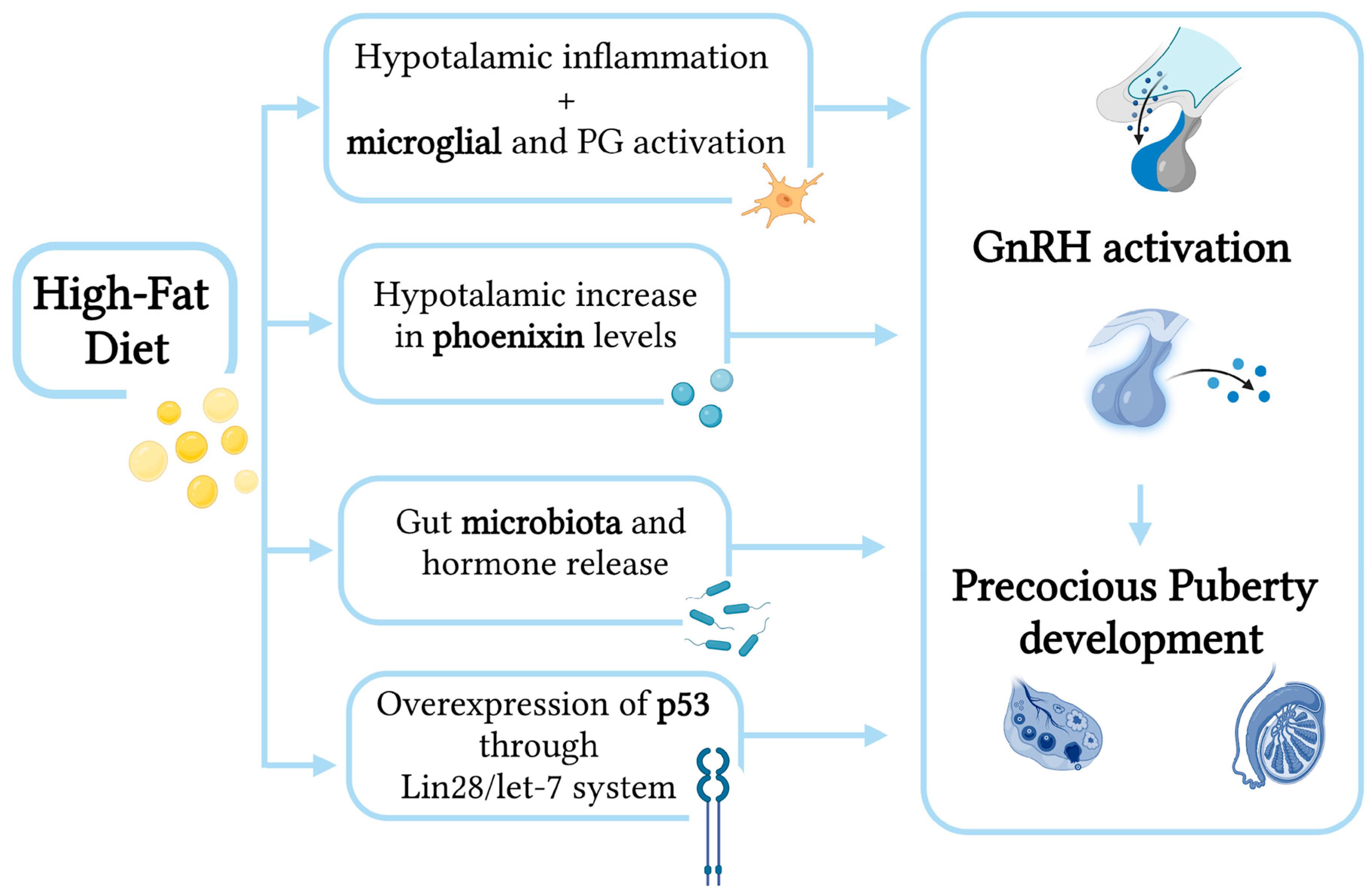
5. High-Fat Diet and Precocious Puberty
5.1. Epidemiological Evidence
5.2. Mechanisms Involved
5.2.1. Activation of GnRH via Hypothalamic Microglial Cells
5.2.2. Activation of GnRH via Diet-induced Phoenixin Action
5.2.3. Modification of Gut Microbiota and Hormones
5.2.4. Overexpression of p53 through Lin28/let-7 System
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- UNICEF/WHO/The World Bank Group Joint Child Malnutrition Estimates: Levels and Trends in Child Malnutrition: Key Findings of the 2020 Edition [Internet]. Available online: https://www.who.int/publications-detail-redirect/jme-2020-edition (accessed on 15 September 2021).
- Giordano, P.; Del Vecchio, G.C.; Cecinati, V.; Delvecchio, M.; Altomare, M.; De Palma, F.; De Mattia, D.; Cavallo, L.; Faienza, M.F. Metabolic, inflammatory, endothelial and haemostatic markers in a group of Italian obese children and adolescents. Eur. J. Pediatr. 2011, 170, 845–850. [Google Scholar] [CrossRef] [PubMed]
- Simmonds, M.; Burch, J.; Llewellyn, A.; Griffiths, C.; Yang, H.; Owen, C.; Duffy, S.; Woolacott, N. The use of measures of obesity in childhood for predicting obesity and the development of obesity-related diseases in adulthood: A systematic review and meta-analysis. Health Technol. Assess. 2015, 19, 1–336. [Google Scholar] [CrossRef] [PubMed]
- Faienza, M.F.; Francavilla, R.; Goffredo, R.; Ventura, A.; Marzano, F.; Panzarino, G.; Marinelli, G.; Cavallo, L.; Di Bitonto, G. Oxidative stress in obesity and metabolic syndrome in children and adolescents. Horm. Res. Paediatr. 2012, 78, 158–164. [Google Scholar] [CrossRef]
- Faienza, M.F.; Acquafredda, A.; Tesse, R.; Luce, V.; Ventura, A.; Maggialetti, N.; Monteduro, M.; Giordano, P.; Cavallo, L. Risk factors for subclinical atherosclerosis in diabetic and obese children. Int. J. Med. Sci. 2013, 10, 338–343. [Google Scholar] [CrossRef]
- Daniels, S.R.; Arnett, D.K.; Eckel, R.H.; Gidding, S.S.; Hayman, L.L.; Kumanyika, S.; Robinson, T.N.; Scott, B.J.; Jeor, S.S.; Williams, C.L. Overweight in children and adolescents: Pathophysiology, consequences, prevention, and treatment. Circulation 2005, 111, 1999–2012. [Google Scholar] [CrossRef] [PubMed]
- Plachta-Danielzik, S.; Kehden, B.; Landsberg, B.; Schaffrath Rosario, A.; Kurth, B.-M.; Arnold, C.; Graf, C.; Hense, S.; Ahrens, W.; Müller, M.J. Attributable risks for childhood overweight: Evidence for limited effectiveness of prevention. Pediatrics 2012, 130, e865–e871. [Google Scholar] [CrossRef]
- Shi, L.; Jiang, Z.; Zhang, L. Childhood obesity and central precocious puberty. Front. Endocrinol. 2022, 13, 1056871. [Google Scholar] [CrossRef]
- Lehrke, M.; Lazar, M.A. Inflamed about obesity. Nat. Med. 2004, 10, 126–127. [Google Scholar] [CrossRef]
- Hotamisligil, G.S. Inflammation and metabolic disorders. Nature 2006, 444, 860–867. [Google Scholar] [CrossRef]
- Petersen, K.F.; Shulman, G. Etiology of insulin resistance. Am. J. Med. 2006, 119 (Suppl. S1), S10–S16. [Google Scholar] [CrossRef]
- Sutherland, J.P.; McKinley, B.; Eckel, R.H. The metabolic syndrome and inflammation. Metab. Syndr. Relat. Disord. 2004, 2, 82–104. [Google Scholar] [CrossRef]
- Posey, K.A.; Clegg, D.J.; Printz, R.L.; Byun, J.; Morton, G.J.; Vivekanandan-Giri, A.; Pennathur, S.; Baskin, D.G.; Heinecke, J.W.; Woods, S.C.; et al. Hypothalamic proinflammatory lipid accumulation, inflammation, and insulin resistance in rats fed a high-fat diet. Am. J. Physiol. Endocrinol. Metab. 2009, 296, E1003–E1012. [Google Scholar] [CrossRef] [PubMed]
- Cai, D. NFkappaB-mediated metabolic inflammation in peripheral tissues versus central nervous system. Cell Cycle 2009, 8, 2542–2548. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, J.; Ben-Shlomo, Y.; Cole, T.J.; Holly, J.; Davey Smith, G. The impact of childhood body mass index on timing of puberty, adult stature and obesity: A follow-up study based on adolescent anthropometry recorded at Christ’s Hospital (1936–1964). Int. J. Obes. 2006, 30, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Calcaterra, V.; Verduci, E.; Magenes, V.C.; Pascuzzi, M.C.; Rossi, V.; Sangiorgio, A.; Bosetti, A.; Zuccotti, G.; Mameli, C. The Role of Pediatric Nutrition as a Modifiable Risk Factor for Precocious Puberty. Life 2021, 11, 1353. [Google Scholar] [CrossRef]
- Euling, S.Y.; Herman-Giddens, M.E.; Lee, P.A.; Selevan, S.G.; Juul, A.; Sørensen, T.I.A.; Dunkel, L.; Himes, J.H.; Teilmann, G.; Swan, S.H. Examination of US Puberty-Timing Data from 1940 to 1994 for Secular Trends: Panel Findings. Pediatrics 2008, 121 (Suppl. S3), S172–S191. [Google Scholar] [CrossRef]
- Valsamakis, G.; Arapaki, A.; Balafoutas, D.; Charmandari, E.; Vlahos, N.F. Diet-Induced Hypothalamic Inflammation, Phoenixin, and Subsequent Precocious Puberty. Nutrients 2021, 13, 3460. [Google Scholar] [CrossRef]
- Bo, T.; Liu, M.; Tang, L.; Lv, J.; Wen, J.; Wang, D. Effects of High-Fat Diet During Childhood on Precocious Puberty and Gut Microbiota in Mice. Front. Microbiol. 2022, 13, 930747. [Google Scholar] [CrossRef]
- Li, Y.; Shen, L.; Huang, C.; Li, X.; Chen, J.; Li, S.C.; Shen, B. Altered nitric oxide induced by gut microbiota reveals the connection between central precocious puberty and obesity. Clin. Transl. Med. 2021, 11, e299. [Google Scholar] [CrossRef]
- Chen, T.; Chen, C.; Wu, H.; Chen, X.; Xie, R.; Wang, F.; Sun, H.; Chen, L. Overexpression of p53 accelerates puberty in high-fat diet–fed mice through Lin28/let-7 system. Exp. Biol. Med. 2021, 246, 66–71. [Google Scholar] [CrossRef]
- Valdearcos, M.; Robblee, M.M.; Benjamin, D.I.; Nomura, D.K.; Xu, A.W.; Koliwad, S.K. Microglia Dictate the Impact of Saturated Fat Consumption on Hypothalamic Inflammation and Neuronal Function. Cell Rep. 2014, 9, 2124–2138. [Google Scholar] [CrossRef] [PubMed]
- Fujioka, H.; Kakehashi, C.; Funabashi, T.; Akema, T. Immunohistochemical evidence for the relationship between microglia and GnRH neurons in the preoptic area of ovariectomized rats with and without steroid replacement. Endocr. J. 2013, 60, 191–196. [Google Scholar] [CrossRef]
- Kiess, W.; Hoppmann, J.; Gesing, J.; Penke, M.; Körner, A.; Kratzsch, J.; Pfaeffle, R. Puberty—Genes, environment and clinical issues. J. Pediatr. Endocrinol. Metab. 2016, 29, 1229–1231. [Google Scholar] [CrossRef]
- Przybył, B.J.; Szlis, M.; Wójcik-Gładysz, A. Brain-derived neurotrophic factor (BDNF) affects the activity of the gonadotrophic axis in sheep. Horm. Behav. 2021, 131, 104980. [Google Scholar] [CrossRef]
- Styne, D.M.; Arslanian, S.A.; Connor, E.L.; Farooqi, I.S.; Murad, M.H.; Silverstein, J.H.; Yanovski, J.A. Pediatric Obesity—Assessment, Treatment, and Prevention: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2017, 102, 709–757. [Google Scholar] [CrossRef]
- Di Cesare, M.; Sorić, M.; Bovet, P.; Miranda, J.J.; Bhutta, Z.; Stevens, G.A.; Laxmaiah, A.; Kengne, A.P.; Bentham, J. The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med. 2019, 17, 212. [Google Scholar] [CrossRef]
- Dollman, J.; Norton, K.; Norton, L. Evidence for secular trends in children’s physical activity behaviour. Br. J. Sports Med. 2005, 39, 892–897, discussion 897. [Google Scholar] [CrossRef] [PubMed]
- Güngör, N.K. Overweight and obesity in children and adolescents. J. Clin. Res. Pediatr. Endocrinol. 2014, 6, 129–143. [Google Scholar] [CrossRef] [PubMed]
- Littleton, S.; Berkowitz, R.I.; Grant, S.F.A. Genetic Determinants of Childhood Obesity. Mol. Diagn. Ther. 2020, 24, 653. [Google Scholar] [CrossRef] [PubMed]
- Morales Camacho, W.J.; Molina Díaz, J.M.; Plata Ortiz, S.; Plata Ortiz, J.E.; Morales Camacho, M.A.; Calderón, B.P. Childhood obesity: Aetiology, comorbidities, and treatment. Diabetes/Metab. Res. Rev. 2019, 35, e3203. [Google Scholar] [CrossRef]
- Obradovic, M.; Sudar-Milovanovic, E.; Soskic, S.; Essack, M.; Arya, S.; Stewart, A.J.; Gojobori, T.; Isenovic, E.R. Leptin and Obesity: Role and Clinical Implication. Front. Endocrinol. 2021, 12, 585887. [Google Scholar] [CrossRef]
- Yeo, G.S.; Chao, D.H.M.; Siegert, A.M.; Koerperich, Z.M.; Ericson, M.D.; Simonds, S.E.; Larson, C.M.; Luquet, S.; Clarke, I.; Sharma, S.; et al. The melanocortin pathway and energy homeostasis: From discovery to obesity therapy. Mol. Metab. 2021, 48, 101206. [Google Scholar] [CrossRef] [PubMed]
- Hutny, M.; Hofman, J.; Zachurzok, A.; Matusik, P. MicroRNAs as the promising markers of comorbidities in childhood obesity—A systematic review. Pediatr. Obes. 2022, 17, e12880. [Google Scholar] [CrossRef] [PubMed]
- Voerman, E.; Santos, S.; Golab, B.P.; Amiano, P.; Ballester, F.; Barros, H.; Bergström, A.; Charles, M.-A.; Chatzi, L.; Chevrier, C.; et al. Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: An individual participant data meta-analysis. PLoS Med. 2019, 16, e1002744. [Google Scholar] [CrossRef] [PubMed]
- Alfano, R.; Robinson, O.; Handakas, E.; Nawrot, T.S.; Vineis, P.; Plusquin, M. Perspectives and challenges of epigenetic determinants of childhood obesity: A systematic review. Obes. Rev. 2022, 23 (Suppl. S1), e13389. [Google Scholar] [CrossRef] [PubMed]
- Sharp, G.C.; Lawlor, D.A.; Richmond, R.C.; Fraser, A.; Simpkin, A.; Suderman, M.; Shihab, H.A.; Lyttleton, O.; McArdle, W.; Ring, S.M.; et al. Maternal pre-pregnancy BMI and gestational weight gain, offspring DNA methylation and later offspring adiposity: Findings from the Avon Longitudinal Study of Parents and Children. Int. J. Epidemiol. 2015, 44, 1288–1304. [Google Scholar] [CrossRef]
- Rhee, K.E.; Phelan, S.; McCaffery, J. Early Determinants of Obesity: Genetic, Epigenetic, and In Utero Influences. Int. J. Pediatr. 2012, 2012, 463850. [Google Scholar] [CrossRef]
- Altaba, I.I.; Larqué, E.; Mesa, M.D.; Blanco-Carnero, J.E.; Gomez-Llorente, C.; Rodríguez-Martínez, G.; Moreno, L.A. Early Nutrition and Later Excess Adiposity during Childhood: A Narrative Review. Horm. Res. Paediatr. 2022, 95, 112–119. [Google Scholar] [CrossRef]
- Trandafir, L.M.; Temneanu, O.R. Pre and post-natal risk and determination of factors for child obesity. J. Med. Life 2016, 9, 386–391. [Google Scholar]
- Marcus, C.; Danielsson, P.; Hagman, E. Pediatric obesity—Long-term consequences and effect of weight loss. J. Intern. Med. 2022, 292, 870–891. [Google Scholar] [CrossRef]
- Calcaterra, V.; Rossi, V.; Mari, A.; Casini, F.; Bergamaschi, F.; Zuccotti, G.V.; Fabiano, V. Medical treatment of weight loss in children and adolescents with obesity. Pharmacol. Res. 2022, 185, 106471. [Google Scholar] [CrossRef] [PubMed]
- Cheuiche, A.V.; da Silveira, L.G.; de Paula, L.C.P.; Lucena, I.R.S.; Silveiro, S.P. Diagnosis and management of precocious sexual maturation: An updated review. Eur. J. Pediatr. 2021, 180, 3073–3087. [Google Scholar] [CrossRef] [PubMed]
- Klein, D.A.; Emerick, J.E.; Sylvester, J.; Vogt, K.S. Disorders of Puberty: An Approach to Diagnosis and Management. Am. Fam. Physician 2017, 96, 590–599. [Google Scholar] [PubMed]
- Tanner, J.M. Trend towards earlier menarche in London, Olso, Copenhagen, the Netherlands and Hungary. Nature 1973, 243, 95–96. [Google Scholar] [CrossRef]
- Bordini, B.; Rosenfield, R.L. Normal pubertal development: Part II: Clinical aspects of puberty. Pediatr. Rev. 2011, 32, 281–292. [Google Scholar] [CrossRef]
- Sun, S.S.; Schubert, C.M.; Chumlea, W.C.; Roche, A.F.; Kulin, H.E.; Lee, P.A.; Himes, J.H.; Ryan, A.S. National estimates of the timing of sexual maturation and racial differences among US children. Pediatrics 2002, 110, 911–919. [Google Scholar] [CrossRef]
- Sørensen, K.; Mouritsen, A.; Aksglaede, L.; Hagen, C.P.; Mogensen, S.S.; Juul, A. Recent secular trends in pubertal timing: Implications for evaluation and diagnosis of precocious puberty. Horm. Res. Paediatr. 2012, 77, 137–145. [Google Scholar] [CrossRef]
- Brito, V.N.; Spinola-Castro, A.M.; Kochi, C.; Kopacek, C.; da Silva, P.C.A.; Guerra-Júnior, G. Central precocious puberty: Revisiting the diagnosis and therapeutic management. Arch. Endocrinol. Metab. 2016, 60, 163–172. [Google Scholar] [CrossRef]
- Cao, R.; Liu, J.; Fu, P.; Zhou, Y.; Li, Z.; Liu, P. The Diagnostic Utility of the Basal Luteinizing Hormone Level and Single 60-Minute Post GnRH Agonist Stimulation Test for Idiopathic Central Precocious Puberty in Girls. Front. Endocrinol. 2021, 12, 713880. [Google Scholar] [CrossRef]
- Lee, S.Y.; Kim, J.M.; Kim, Y.M.; Lim, H.H. Single random measurement of urinary gonadotropin concentration for screening and monitoring girls with central precocious puberty. Ann. Pediatr. Endocrinol. Metab. 2021, 26, 178–184. [Google Scholar] [CrossRef]
- Wei, C.; Davis, N.; Honour, J.; Crowne, E. The investigation of children and adolescents with abnormalities of pubertal timing. Ann. Clin. Biochem. 2017, 54, 20–32. [Google Scholar] [CrossRef]
- Kliegman, R.; Nelson, W.E. Nelson Textbook of Pediatrics [Internet], 19th ed.; Elsevier/Saunders: Philadelphia, PA, USA, 2011; p. 2610. [Google Scholar]
- Eugster, E.A. Treatment of Central Precocious Puberty. J. Endocr. Soc. 2019, 3, 965–972. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Cao, B.; Luo, Q.; Wang, Q.; Liu, M.; Liang, X.; Wu, D.; Li, W.; Su, C.; Chen, J.; et al. The critical BMI hypothesis for puberty initiation and the gender prevalence difference: Evidence from an epidemiological survey in Beijing, China. Front. Endocrinol. 2022, 13, 1009133. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Ma, T.; Ma, Y.; Gao, D.; Chen, L.; Chen, M.; Liu, J.; Dong, B.; Dong, Y.; Ma, J. Adiposity Status, Trajectories, and Earlier Puberty Onset: Results From a Longitudinal Cohort Study. J. Clin. Endocrinol. Metab. 2022, 107, 2462–2472. [Google Scholar] [CrossRef] [PubMed]
- Frisch, R.E.; Revelle, R. Height and weight at menarche and a hypothesis of menarche. Arch. Dis. Child. 1971, 46, 695–701. [Google Scholar] [CrossRef]
- Bruno, C.; Vergani, E.; Giusti, M.; Oliva, A.; Cipolla, C.; Pitocco, D.; Mancini, A. The “Adipo-Cerebral” Dialogue in Childhood Obesity: Focus on Growth and Puberty. Physiopathol. Nutr. Aspects. Nutr. 2021, 13, 3434. [Google Scholar]
- Shimizu, H.; Mori, M. The brain-adipose axis: A review of involvement of molecules. Nutr. Neurosci. 2005, 8, 7–20. [Google Scholar] [CrossRef]
- de Luis, D.A.; Perez Castrillón, J.L.; Dueñas, A. Leptin and obesity. Minerva Med. 2009, 100, 229–236. [Google Scholar]
- Tng, E. Kisspeptin signalling and its roles in humans. Singap. Med. J. 2015, 56, 649–656. [Google Scholar] [CrossRef]
- Casanueva, F.F.; Dieguez, C. Neuroendocrine regulation and actions of leptin. Front. Neuroendocrinol. 1999, 20, 317–363. [Google Scholar] [CrossRef]
- Roemmich, J.N.; Clark, P.A.; Berr, S.S.; Mai, V.; Mantzoros, C.S.; Flier, J.S.; Weltman, A.; Rogol, A. Gender differences in leptin levels during puberty are related to the subcutaneous fat depot and sex steroids. Am. J. Physiol. 1998, 275, E543–E551. [Google Scholar] [CrossRef]
- Rutters, F.; Nieuwenhuizen, A.G.; Verhoef, S.P.M.; Lemmens, S.G.T.; Vogels, N.; Westerterp-Plantenga, M.S. The relationship between leptin, gonadotropic hormones, and body composition during puberty in a Dutch children cohort. Eur. J. Endocrinol. 2009, 160, 973–978. [Google Scholar] [CrossRef]
- Matkovic, V.; Ilich, J.Z.; Skugor, M.; Badenhop, N.E.; Goel, P.; Clairmont, A.; Klisovic, D.; Nahhas, R.W.; Landoll, J.D. Leptin is inversely related to age at menarche in human females. J. Clin. Endocrinol. Metab. 1997, 82, 3239–3245. [Google Scholar]
- Bianco, S.D.C. A potential mechanism for the sexual dimorphism in the onset of puberty and incidence of idiopathic central precocious puberty in children: Sex-specific kisspeptin as an integrator of puberty signals. Front. Endocrinol. 2012, 3, 149. [Google Scholar] [CrossRef]
- Mathew, H.; Castracane, V.D.; Mantzoros, C. Adipose tissue and reproductive health. Metabolism 2018, 86, 18–32. [Google Scholar] [CrossRef]
- Arita, Y.; Kihara, S.; Ouchi, N.; Takahashi, M.; Maeda, K.; Miyagawa, J.I.; Hotta, K.; Shimomura, I.; Nakamura, T.; Miyaoka, K.; et al. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem. Biophys. Res. Commun. 1999, 257, 79–83. [Google Scholar] [CrossRef]
- Sørensen, K.; Aksglaede, L.; Munch-Andersen, T.; Aachmann-Andersen, N.J.; Petersen, J.H.; Hilsted, L.; Helge, J.W.; Juul, A. Sex hormone-binding globulin levels predict insulin sensitivity, disposition index, and cardiovascular risk during puberty. Diabetes Care 2009, 32, 909–914. [Google Scholar] [CrossRef]
- Yüce, Ö.; Sevinç, D. Ultrasonographic assessment of pubertal breast development in obese children: Compliance with the clinic. J. Pediatr. Endocrinol. Metab. 2018, 31, 137–141. [Google Scholar] [CrossRef]
- Zhao, C.; Tang, Y.; Cheng, L. Diagnostic Value of LH Peak Value of the GnRH Stimulation Test for Girls with Precocious Puberty and Its Correlation with Body Mass Index. Comput. Math. Methods Med. 2022, 2022, 4118911. [Google Scholar] [CrossRef] [PubMed]
- Tenedero, C.B.; Oei, K.; Palmert, M.R. An Approach to the Evaluation and Management of the Obese Child with Early Puberty. J. Endocr. Soc. 2022, 6, bvab173. [Google Scholar] [CrossRef]
- Klein, K.O.; Newfield, R.S.; Hassink, S.G. Bone maturation along the spectrum from normal weight to obesity: A complex interplay of sex, growth factors and weight gain. J. Pediatr. Endocrinol. Metab. 2016, 29, 311–318. [Google Scholar] [CrossRef]
- Reinehr, T.; de Sousa, G.; Wabitsch, M. Relationships of IGF-I and andrrogens to skeletal maturation in obese children and adolescents. J. Pediatr. Endocrinol. Metab. 2006, 19, 1133–1140. [Google Scholar] [CrossRef]
- Aris, I.M.; Rifas-Shiman, S.L.; Zhang, X.; Yang, S.; Switkowski, K.; Fleisch, A.F.; Hivert, M.; Martin, R.M.; Kramer, M.S.; Oken, E. Association of BMI with Linear Growth and Pubertal Development. Obesity 2019, 27, 1661–1670. [Google Scholar] [CrossRef]
- De Leonibus, C.; Marcovecchio, M.L.; Chiarelli, F. Update on statural growth and pubertal development in obese children. Pediatr. Rep. 2012, 4, e35. [Google Scholar] [CrossRef]
- Imamura, F.; Micha, R.; Khatibzadeh, S.; Fahimi, S.; Shi, P.; Powles, J.; Mozaffarian, D. Dietary quality among men and women in 187 countries in 1990 and 2010: A systematic assessment. Lancet Glob. Health 2015, 3, e132–e142. [Google Scholar] [CrossRef]
- National Research Council (US) Committee on Diet and Health. Diet and Health: Implications for Reducing Chronic Disease Risk; National Academies Press: Washington, DC, USA, 1989. [Google Scholar]
- Obeid, C.A.; Gubbels, J.S.; Jaalouk, D.; Kremers, S.P.J.; Oenema, A. Adherence to the Mediterranean diet among adults in Mediterranean countries: A systematic literature review. Eur. J. Nutr. 2022, 61, 3327–3344. [Google Scholar] [CrossRef]
- García Cabrera, S.; Herrera Fernández, N.; Rodríguez Hernández, C.; Nissensohn, M.; Román-Viñas, B.; Serra-Majem, L. Kidmed test; prevalence of low adherence to the mediterranean diet in children and young; a systematic review. Nutr. Hosp. 2015, 32, 2390–2399. [Google Scholar]
- El-Behadli, A.F.; Sharp, C.; Hughes, S.O.; Obasi, E.M.; Nicklas, T.A. Maternal depression, stress and feeding styles: Towards a framework for theory and research in child obesity. Br. J. Nutr. 2015, 113, S55–S71. [Google Scholar] [CrossRef]
- Maffeis, C.; Talamini, G.; Tatò, L. Influence of diet, physical activity and parents’ obesity on children’s adiposity: A four-year longitudinal study. Int. J. Obes. Relat. Metab. Disord. 1998, 22, 758–764. [Google Scholar] [CrossRef]
- Dashti, H.S.; Scheer, F.A.; Jacques, P.F.; Lamon-Fava, S.; Ordovás, J.M. Short sleep duration and dietary intake: Epidemiologic evidence, mechanisms, and health implications. Adv. Nutr. 2015, 6, 648–659. [Google Scholar] [CrossRef]
- Weiss, A.; Xu, F.; Storfer-Isser, A.; Thomas, A.; Ievers-Landis, C.E.; Redline, S. The association of sleep duration with adolescents’ fat and carbohydrate consumption. Sleep 2010, 33, 1201–1209. [Google Scholar] [CrossRef] [PubMed]
- Córdova, F.V.; Barja, S.; Brockmann, P.E. Consequences of short sleep duration on the dietary intake in children: A systematic review and metanalysis. Sleep Med. Rev. 2018, 42, 68–84. [Google Scholar] [CrossRef] [PubMed]
- Johnson, L.; Mander, A.P.; Jones, L.R.; Emmett, P.M.; Jebb, S.A. Energy-dense, low-fiber, high-fat dietary pattern is associated with increased fatness in childhood. Am. J. Clin. Nutr. 2008, 87, 846–854. [Google Scholar] [CrossRef] [PubMed]
- Rennie, K.L.; Johnson, L.; Jebb, S.A. Behavioural determinants of obesity. Best Pract. Res. Clin. Endocrinol. Metab. 2005, 19, 343–358. [Google Scholar] [CrossRef] [PubMed]
- Robertson, S.M.; Cullen, K.W.; Baranowski, J.; Baranowski, T.; Hu, S.; de Moor, C. Factors related to adiposity among children aged 3 to 7 years. J. Am. Diet. Assoc. 1999, 99, 938–943. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, C.M.; McGillicuddy, F.C.; Harford, K.A.; Finucane, O.M.; Mills, K.H.G.; Roche, H.M. Dietary saturated fatty acids prime the NLRP3 inflammasome via TLR4 in dendritic cells-implications for diet-induced insulin resistance. Mol. Nutr. Food Res. 2012, 56, 1212–1222. [Google Scholar] [CrossRef] [PubMed]
- Souza, C.O.; Teixeira, A.A.; Biondo, L.A.; Silveira, L.S.; de Souza Breda, C.N.; Braga, T.T.; Camara, N.O.; Belchior, T.; Festuccia, W.T.; Diniz, T.A.; et al. Palmitoleic acid reduces high fat diet-induced liver inflammation by promoting PPAR-γ-independent M2a polarization of myeloid cells. Biochim. Biophys. Acta Mol. Cell. Biol. Lipids 2020, 1865, 158776. [Google Scholar] [CrossRef]
- Chan, K.L.; Pillon, N.J.; Sivaloganathan, D.M.; Costford, S.R.; Liu, Z.; Théret, M.; Chazaud, B.; Klip, A. Palmitoleate Reverses High Fat-induced Proinflammatory Macrophage Polarization via AMP-activated Protein Kinase (AMPK). J. Biol. Chem. 2015, 290, 16979–16988. [Google Scholar] [CrossRef]
- Pickup, J.C. Inflammation and activated innate immunity in the pathogenesis of type 2 diabetes. Diabetes Care 2004, 27, 813–823. [Google Scholar] [CrossRef]
- Ross, R. Atherosclerosis--an inflammatory disease. N. Engl. J. Med. 1999, 340, 115–126. [Google Scholar] [CrossRef]
- Nigro, E.; Scudiero, O.; Monaco, M.L.; Palmieri, A.; Mazzarella, G.; Costagliola, C.; Bianco, A.; Daniele, A. New insight into adiponectin role in obesity and obesity-related diseases. Biomed. Res. Int. 2014, 2014, 658913. [Google Scholar] [CrossRef]
- Thaler, J.P.; Schwartz, M.W. Minireview: Inflammation and obesity pathogenesis: The hypothalamus heats up. Endocrinology 2010, 151, 4109–4115. [Google Scholar] [CrossRef]
- Festa, A.; D’Agostino, R.; Tracy, R.P.; Haffner, S.M.; Insulin Resistance Atherosclerosis Study. Elevated levels of acute-phase proteins and plasminogen activator inhibitor-1 predict the development of type 2 diabetes: The insulin resistance atherosclerosis study. Diabetes 2002, 51, 1131–1137. [Google Scholar] [CrossRef] [PubMed]
- Duncan, B.B.; Schmidt, M.I.; Pankow, J.S.; Ballantyne, C.M.; Couper, D.; Vigo, A.; Hoogeveen, R.; Folsom, A.R.; Heiss, G. Low-grade systemic inflammation and the development of type 2 diabetes: The atherosclerosis risk in communities study. Diabetes 2003, 52, 1799–1805. [Google Scholar] [CrossRef] [PubMed]
- Coll, A.P.; Farooqi, I.S.; O’Rahilly, S. The hormonal control of food intake. Cell 2007, 129, 251–262. [Google Scholar] [CrossRef]
- Lam, T.K.T.; Schwartz, G.J.; Rossetti, L. Hypothalamic sensing of fatty acids. Nat. Neurosci. 2005, 8, 579–584. [Google Scholar] [CrossRef]
- Morton, G.J.; Cummings, D.E.; Baskin, D.G.; Barsh, G.S.; Schwartz, M.W. Central nervous system control of food intake and body weight. Nature 2006, 443, 289–295. [Google Scholar] [CrossRef]
- Gropp, E.; Shanabrough, M.; Borok, E.; Xu, A.W.; Janoschek, R.; Buch, T.; Plum, L.; Balthasar, N.; Hampel, B.; Waisman, A.; et al. Agouti-related peptide-expressing neurons are mandatory for feeding. Nat. Neurosci. 2005, 8, 1289–1291. [Google Scholar] [CrossRef]
- Luquet, S.; Perez, F.A.; Hnasko, T.S.; Palmiter, R.D. NPY/AgRP neurons are essential for feeding in adult mice but can be ablated in neonates. Science 2005, 310, 683–685. [Google Scholar] [CrossRef]
- Yi, C.X.; Tschöp, M.H. Brain-gut-adipose-tissue communication pathways at a glance. Dis. Model. Mech. 2012, 5, 583–587. [Google Scholar] [CrossRef]
- Cowley, M.A.; Smart, J.L.; Rubinstein, M.; Cerdán, M.G.; Diano, S.; Horvath, T.L.; Cone, R.D.; Low, M.J. Leptin activates anorexigenic POMC neurons through a neural network in the arcuate nucleus. Nature 2001, 411, 480–484. [Google Scholar] [CrossRef] [PubMed]
- Uysal, K.T.; Wiesbrock, S.M.; Marino, M.W.; Hotamisligil, G.S. Protection from obesity-induced insulin resistance in mice lacking TNF-alpha function. Nature 1997, 389, 610–614. [Google Scholar] [CrossRef] [PubMed]
- Arruda, A.P.; Milanski, M.; Coope, A.; Torsoni, A.S.; Ropelle, E.; Carvalho, D.P.; Carvalheira, J.B.; Velloso, L.A. Low-grade hypothalamic inflammation leads to defective thermogenesis, insulin resistance, and impaired insulin secretion. Endocrinology 2011, 152, 1314–1326. [Google Scholar] [CrossRef] [PubMed]
- Oh-I, S.; Thaler, J.P.; Ogimoto, K.; Wisse, B.E.; Morton, G.J.; Schwartz, M.W. Central administration of interleukin-4 exacerbates hypothalamic inflammation and weight gain during high-fat feeding. Am. J. Physiol. Endocrinol. Metab. 2010, 299, E47–E53. [Google Scholar] [CrossRef] [PubMed]
- Yan, J.; Zhang, H.; Yin, Y.; Li, J.; Tang, Y.; Purkayastha, S.; Li, L.; Cai, D. Obesity- and aging-induced excess of central transforming growth factor-β potentiates diabetic development via an RNA stress response. Nat. Med. 2014, 20, 1001–1008. [Google Scholar] [CrossRef]
- Wang, N.; Wang, H.; Yao, H.U.A.; Wei, Q.I.N.; Mao, X.M.; Jiang, T.A.O.; Xiang, J.; Dila, N.A. Expression and activity of the TLR4/NF-κB signaling pathway in mouse intestine following administration of a short-term high-fat diet. Exp. Ther. Med. 2013, 6, 635–640. [Google Scholar] [CrossRef]
- Zhou, Y.-D. Glial Regulation of Energy Metabolism. Adv. Exp. Med. Biol. 2018, 1090, 105–121. [Google Scholar]
- Cai, D.; Khor, S. Hypothalamic Microinflammation» Paradigm in Aging and Metabolic Diseases. Cell Metab. 2019, 30, 19–35. [Google Scholar] [CrossRef]
- Fessler, M.B.; Rudel, L.L.; Brown, J.M. Toll-like receptor signaling links dietary fatty acids to the metabolic syndrome. Curr. Opin. Lipidol. 2009, 20, 379–385. [Google Scholar] [CrossRef]
- Myers, M.G.; Cowley, M.A.; Münzberg, H. Mechanisms of leptin action and leptin resistance. Annu. Rev. Physiol. 2008, 70, 537–556. [Google Scholar] [CrossRef]
- Schenk, S.; Saberi, M.; Olefsky, J.M. Insulin sensitivity: Modulation by nutrients and inflammation. J. Clin. Investig. 2008, 118, 2992–3002. [Google Scholar] [CrossRef] [PubMed]
- David, L.A.; Maurice, C.F.; Carmody, R.N.; Gootenberg, D.B.; Button, J.E.; Wolfe, B.E.; Ling, A.V.; Devlin, A.S.; Varma, Y.; Fischbach, M.A.; et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature 2014, 505, 559–563. [Google Scholar] [CrossRef] [PubMed]
- Turnbaugh, P.J.; Bäckhed, F.; Fulton, L.; Gordon, J.I. Diet-induced obesity is linked to marked but reversible alterations in the mouse distal gut microbiome. Cell Host Microbe 2008, 3, 213–223. [Google Scholar] [CrossRef] [PubMed]
- Ley, R.E.; Turnbaugh, P.J.; Klein, S.; Gordon, J.I. Microbial ecology: Human gut microbes associated with obesity. Nature 2006, 444, 1022–1023. [Google Scholar] [CrossRef] [PubMed]
- Turnbaugh, P.J.; Ridaura, V.K.; Faith, J.J.; Rey, F.E.; Knight, R.; Gordon, J.I. The effect of diet on the human gut microbiome: A metagenomic analysis in humanized gnotobiotic mice. Sci. Transl. Med. 2009, 1, 6ra14. [Google Scholar] [CrossRef]
- Malesza, I.J.; Malesza, M.; Walkowiak, J.; Mussin, N.; Walkowiak, D.; Aringazina, R.; Bartkowiak-Wieczorek, J.; Mądry, E. High-Fat, Western-Style Diet, Systemic Inflammation, and Gut Microbiota: A Narrative Review. Cells 2021, 10, 3164. [Google Scholar] [CrossRef]
- Sonnenburg, E.D.; Smits, S.A.; Tikhonov, M.; Higginbottom, S.K.; Wingreen, N.S.; Sonnenburg, J.L. Diet-induced extinctions in the gut microbiota compound over generations. Nature 2016, 529, 212–215. [Google Scholar] [CrossRef]
- Cani, P.D.; Delzenne, N.M. The gut microbiome as therapeutic target. Pharmacol. Ther. 2011, 130, 202–212. [Google Scholar] [CrossRef]
- Bisanz, J.E.; Upadhyay, V.; Turnbaugh, J.A.; Ly, K.; Turnbaugh, P.J. Meta-Analysis Reveals Reproducible Gut Microbiome Alterations in Response to a High-Fat Diet. Cell Host Microbe 2019, 26, 265–272.e4. [Google Scholar] [CrossRef]
- De Wit, N.; Derrien, M.; Bosch-Vermeulen, H.; Oosterink, E.; Keshtkar, S.; Duval, C.; de Vogel-van den Bosch, J.; Kleerebezem, M.; Müller, M.; van der Meer, R. Saturated fat stimulates obesity and hepatic steatosis and affects gut microbiota composition by an enhanced overflow of dietary fat to the distal intestine. Am. J. Physiol. Gastrointest. Liver Physiol. 2012, 303, G589–G599. [Google Scholar] [CrossRef]
- Derrien, M.; Vaughan, E.E.; Plugge, C.M.; de Vos, W.M. Akkermansia muciniphila gen. nov., sp. nov., a human intestinal mucin-degrading bacterium. Int. J. Syst. Evol. Microbiol. 2004, 54, 1469–1476. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Lv, L.; Shi, D.; Ye, J.; Fang, D.; Guo, F.; Li, Y.; He, X.; Li, L. Protective Effect of Akkermansia muciniphila against Immune-Mediated Liver Injury in a Mouse Model. Front. Microbiol. 2017, 8, 1804. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; An, Y.; Hao, F.; Wang, Y.; Tang, H. Correlations of Fecal Metabonomic and Microbiomic Changes Induced by High-fat Diet in the Pre-Obesity State. Sci. Rep. 2016, 6, 21618. [Google Scholar] [CrossRef]
- Lam, Y.Y.; Ha, C.W.Y.; Storlien, L.H.; Hoffmann, J.M.A.; Oscarsson, J.; Dinudom, A.; Mather, T.J.; Cook, D.I.; Hunt, N.H.; Caterson, I.D.; et al. Effects of dietary fat profile on gut permeability and microbiota and their relationships with metabolic changes in mice. Obesity 2015, 23, 1429–1439. [Google Scholar]
- Derrien, M.; van Passel, M.W.; van de Bovenkamp, J.H.; Schipper, R.G.; de Vos, W.M.; Dekker, J. Mucin-bacterial interactions in the human oral cavity and digestive tract. Gut Microbes 2010, 1, 254–268. [Google Scholar] [CrossRef] [PubMed]
- Lam, Y.Y.; Ha, C.W.Y.; Campbell, C.R.; Mitchell, A.J.; Dinudom, A.; Oscarsson, J.; Cook, D.I.; Hunt, N.H.; Caterson, I.D.; Holmes, A.J.; et al. Increased gut permeability and microbiota change associate with mesenteric fat inflammation and metabolic dysfunction in diet-induced obese mice. PLoS ONE 2012, 7, e34233. [Google Scholar] [CrossRef] [PubMed]
- Cani, P.D.; Amar, J.; Iglesias, M.A.; Poggi, M.; Knauf, C.; Bastelica, D.; Neyrinck, A.M.; Fava, F.; Tuohy, K.M.; Chabo, C.; et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 2007, 56, 1761–1772. [Google Scholar] [CrossRef]
- Kim, K.-A.; Gu, W.; Lee, I.-A.; Joh, E.-H.; Kim, D.-H. High fat diet-induced gut microbiota exacerbates inflammation and obesity in mice via the TLR4 signaling pathway. PLoS ONE 2012, 7, e47713. [Google Scholar] [CrossRef]
- Chen, C.; Zhang, Y.; Sun, W.; Chen, Y.; Jiang, Y.; Song, Y.; Lin, Q.; Zhu, L.; Zhu, Q.; Wang, X.; et al. Investigating the relationship between precocious puberty and obesity: A cross-sectional study in Shanghai, China. BMJ Open 2017, 7, e014004. [Google Scholar] [CrossRef]
- Mendes, N.F.; Kim, Y.-B.; Velloso, L.A.; Araújo, E.P. Hypothalamic Microglial Activation in Obesity: A Mini-Review. Front. Neurosci. 2018, 12, 846. [Google Scholar] [CrossRef]
- Gao, Y.; Ottaway, N.; Schriever, S.C.; Legutko, B.; García-Cáceres, C.; de la Fuente, E.; Mergen, C.; Bour, S.; Thaler, J.P.; Seeley, R.J.; et al. Hormones and diet, but not body weight, control hypothalamic microglial activity: Hypothalamic Microglia in Obesity. Glia 2014, 62, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Rosenfield, R.L.; Lipton, R.B.; Drum, M.L. Thelarche, pubarche, and menarche attainment in children with normal and elevated body mass index. Pediatrics 2009, 123, 84–88. [Google Scholar] [CrossRef] [PubMed]
- de Roux, N.; Genin, E.; Carel, J.C.; Matsuda, F.; Chaussain, J.L.; Milgrom, E. Hypogonadotropic hypogonadism due to loss of function of the KiSS1-derived peptide receptor GPR54. Proc. Natl. Acad. Sci. USA 2003, 100, 10972–10976. [Google Scholar] [CrossRef]
- Szamreta, E.A.; Qin, B.; Rivera-Núñez, Z.; Parekh, N.; Barrett, E.S.; Ferrante, J.; Lin, Y.; Bandera, E.V. Greater adherence to a Mediterranean-like diet is associated with later breast development and menarche in peripubertal girls. Public Health Nutr. 2020, 23, 1020–1030. [Google Scholar] [CrossRef]
- Cheng, G.; Buyken, A.E.; Shi, L.; Karaolis-Danckert, N.; Kroke, A.; Wudy, S.A.; Degen, G.H.; Remer, T. Beyond overweight: Nutrition as an important lifestyle factor influencing timing of puberty. Nutr. Rev. 2012, 70, 133–152. [Google Scholar] [CrossRef] [PubMed]
- Koo, M.M.; Rohan, T.E.; Jain, M.; McLaughlin, J.R.; Corey, P.N. A cohort study of dietary fibre intake and menarche. Public Health Nutr. 2002, 5, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Berkey, C.S.; Gardner, J.D.; Frazier, A.L.; Colditz, G. Relation of childhood diet and body size to menarche and adolescent growth in girls. Am. J. Epidemiol. 2000, 152, 446–452. [Google Scholar] [CrossRef] [PubMed]
- Mervish, N.A.; Gardiner, E.W.; Galvez, M.P.; Kushi, L.H.; Windham, G.C.; Biro, F.M.; Pinney, S.M.; Rybak, M.E.; Teitelbaum, S.L.; Wolff, M.S. Dietary flavonol intake is associated with age of puberty in a longitudinal cohort of girls. Nutr. Res. 2013, 33, 534–542. [Google Scholar] [CrossRef]
- Aksglaede, L.; Sørensen, K.; Petersen, J.H.; Skakkebæk, N.E.; Juul, A. decline in age at breast development: The Copenhagen Puberty Study. Pediatrics 2009, 123, 932–939. [Google Scholar] [CrossRef]
- Jansen, E.C.; Marín, C.; Mora-Plazas, M.; Villamor, E. Higher Childhood Red Meat Intake Frequency Is Associated with Earlier Age at Menarche. J. Nutr. 2015, 146, 792–798. [Google Scholar] [CrossRef]
- Mueller, N.T.; Jacobs, D.R.; MacLehose, R.F.; Demerath, E.W.; Kelly, S.P.; Dreyfus, J.G.; Pereira, M.A. Consumption of caffeinated and artificially sweetened soft drinks is associated with risk of early menarche. Am. J. Clin. Nutr. 2015, 102, 648–654. [Google Scholar] [CrossRef] [PubMed]
- Gunther, A.L.B.; Karaolis-Danckert, N.; Kroke, A.; Remer, T.; Buyken, A.E. Dietary protein intake throughout childhood is associated with the timing of puberty. J. Nutr. 2010, 140, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, C.; Udam, T.; Lauritzen, L.; Mølgaard, C.; Juul, A.; Michaelsen, K. Animal protein intake, serum insulin-like growth factor I, and growth in healthy 2.5-y-old Danish children. Am. J. Clin. Nutr. 2004, 80, 447–452. [Google Scholar] [CrossRef] [PubMed]
- Wiley, A. Milk intake and total dairy consumption: Associations with early menarche in NHANES 1999–2004. PLoS ONE 2011, 6, e14685. [Google Scholar] [CrossRef] [PubMed]
- Rogers, I.; Northstone, K.; Dunger, D.; Cooper, A.; Ness, A.; Emmett, P. Diet throughout childhood and age at menarche in a contemporary cohort of British girls. Public Health Nutr. 2010, 13, 2052–2063. [Google Scholar] [CrossRef]
- Merzenich, H.; Boeing, H.; Wahrendorf, J. Dietary fat and sports activity as determinants for age at menarche. Am. J. Epidemiol. 1993, 138, 217–224. [Google Scholar] [CrossRef]
- Carwile, J.L.; Willett, W.C.; Wang, M.; Rich-Edwards, J.; Frazier, A.L.; Michels, K.B. Milk Consumption after Age 9 Years Does Not Predict Age at Menarche. J. Nutr. 2015, 145, 1900–1908. [Google Scholar] [CrossRef]
- Barbieri, R.L. The Endocrinology of the Menstrual Cycle. In Human Fertility; Rosenwaks, Z., Wassarman, P.M., Eds.; Springer: New York, NY, USA, 2014; pp. 145–169. [Google Scholar]
- Beltramo, M.; Dardente, H.; Cayla, X.; Caraty, A. Cellular mechanisms and integrative timing of neuroendocrine control of GnRH secretion by kisspeptin. Mol. Cell. Endocrinol. 2014, 382, 387–399. [Google Scholar] [CrossRef]
- Yosten, G.L.C.; Lyu, R.-M.; Hsueh, A.J.W.; Avsian-Kretchmer, O.; Chang, J.-K.; Tullock, C.W.; Dun, S.L.; Dun, N.; Samson, W.K. A Novel Reproductive Peptide, Phoenixin. J. Neuroendocrinol. 2013, 25, 206–215. [Google Scholar] [CrossRef]
- Billert, M.; Rak, A.; Nowak, K.; Skrzypski, M. Phoenixin: More than Reproductive Peptide. Int. J. Mol. Sci. 2020, 21, 8378. [Google Scholar] [CrossRef]
- Suszka-Świtek, A.; Pałasz, A.; Filipczyk, Ł.; Menezes, I.C.; Mordecka-Chamera, K.; Angelone, T.; Bogus, K.; Bacopoulou, F.; Worthington, J.J.; Wiaderkiewicz, R. The Gn RH analogues affect novel neuropeptide SMIM 20/phoenixin and GPR 173 receptor expressions in the female rat hypothalamic–pituitary–gonadal (HPG) axis. Clin. Exp. Pharmacol. Physiol. 2019, 46, 350–359. [Google Scholar] [CrossRef] [PubMed]
- Seminara, S.B.; Messager, S.; Chatzidaki, E.E.; Thresher, R.R.; Acierno, J.S.J.; Shagoury, J.K.; Bo-Abbas, Y.; Kuohung, W.; Schwinof, K.M.; Hendrick, A.G.; et al. The GPR54 Gene as a Regulator of Puberty. N. Engl. J. Med. 2003, 349, 1614–1627. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, X.P.; Nakamura, T.; Osuka, S.; Bayasula, B.; Nakanishi, N.; Kasahara, Y.; Muraoka, A.; Hayashi, S.; Nagai, T.; Murase, T.; et al. Effect of the neuropeptide phoenixin and its receptor GPR173 during folliculogenesis. Reproduction 2019, 158, 25–34. [Google Scholar] [CrossRef] [PubMed]
- McIlwraith, E.K.; Loganathan, N.; Belsham, D.D. Phoenixin Expression Is Regulated by the Fatty Acids Palmitate, Docosahexaenoic Acid and Oleate, and the Endocrine Disrupting Chemical Bisphenol A in Immortalized Hypothalamic Neurons. Front. Neurosci. 2018, 12, 838. [Google Scholar] [CrossRef]
- Shi, H.; Kokoeva, M.V.; Inouye, K.; Tzameli, I.; Yin, H.; Flier, J.S. TLR4 links innate immunity and fatty acid–induced insulin resistance. J. Clin. Investig. 2006, 116, 3015–3025. [Google Scholar] [CrossRef]
- Calcaterra, V.; Rossi, V.; Massini, G.; Regalbuto, C.; Hruby, C.; Panelli, S.; Bandi, C.; Zuccotti, G. Precocious puberty and microbiota: The role of the sex hormone–gut microbiome axis. Front. Endocrinol. 2022, 13, 1000919. [Google Scholar] [CrossRef]
- Qi, X.; Yun, C.; Pang, Y.; Qiao, J. The impact of the gut microbiota on the reproductive and metabolic endocrine system. Gut Microbes 2021, 13, 1894070. [Google Scholar] [CrossRef]
- Morrison, D.J.; Preston, T. Formation of short chain fatty acids by the gut microbiota and their impact on human metabolism. Gut Microbes 2016, 7, 189–200. [Google Scholar] [CrossRef]
- Silva, Y.P.; Bernardi, A.; Frozza, R.L. The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Front. Endocrinol. 2020, 11, 25. [Google Scholar] [CrossRef]
- Kimura, I.; Ichimura, A.; Ohue-Kitano, R.; Igarashi, M. Free Fatty Acid Receptors in Health and Disease. Physiol. Rev. 2020, 100, 171–210. [Google Scholar] [CrossRef]
- Evans, J.M.; Morris, L.S.; Marchesi, J.R. The gut microbiome: The role of a virtual organ in the endocrinology of the host. J. Endocrinol. 2013, 218, R37–R47. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Wu, H.; Chen, X.; Xie, R.; Wang, F.; Sun, H.; Chen, L. p53 Mediates GnRH Secretion via Lin28/let-7 System in GT1-7 Cells. DMSO 2020, 13, 4681–4688. [Google Scholar] [CrossRef] [PubMed]
- Johnson, W.; Choh, A.C.; Curran, J.E.; Czerwinski, S.A.; Bellis, C.; Dyer, T.D.; Blangero, J.; Towne, B.; Demerath, E.W. Genetic risk for earlier menarche also influences peripubertal body mass index. Am. J. Phys. Anthropol. 2013, 150, 10–20. [Google Scholar] [CrossRef]
- Perry, J.R.B.; Stolk, L.; Franceschini, N.; Lunetta, K.L.; Zhai, G.; McArdle, P.F.; Smith, A.V.; Aspelund, T.; Bandinelli, S.; Boerwinkle, E.; et al. Meta-analysis of genome-wide association data identifies two loci influencing age at menarche. Nat. Genet. 2009, 41, 648–650. [Google Scholar] [CrossRef]
- Wang, Y. Is obesity associated with early sexual maturation? A comparison of the association in American boys versus girls. Pediatrics 2002, 110, 903–910. [Google Scholar] [CrossRef] [PubMed]
- Clarkson, J.; Boon, W.C.; Simpson, E.R.; Herbison, A.E. Postnatal development of an estradiol-kisspeptin positive feedback mechanism implicated in puberty onset. Endocrinology 2009, 150, 3214–3220. [Google Scholar] [CrossRef] [PubMed]
- Kauffman, A.S.; Navarro, V.M.; Kim, J.; Clifton, D.K.; Steiner, R.A. Sex differences in the regulation of Kiss1/NKB neurons in juvenile mice: Implications for the timing of puberty. Am. J. Physiol. Endocrinol. Metab. 2009, 297, E1212–E1221. [Google Scholar] [CrossRef]
| Authors | Journal/Year | Study Design | Population Involved (Sample Size and Age) | Main Results |
|---|---|---|---|---|
| Sandhu J, et al. [15] | Int. J. Obes. (Lond). 2006 | A retrospective school-based cohort follow-up study | 1520 men born between 1927 and 1956 with serial height and weight measurements from the age of 9 to 18, followed up in adulthood at a mean age of 63 years | Boys with a later puberty tended to be taller and less adipose as adults. Boys with a higher childhood BMI tended to have an earlier puberty. |
| Euling SY, et al. [17] | Pediatrics. 2008 | Comparative study | Examination of US puberty timing data from 1940 to 1994 | Trend toward an earlier breast development onset and menarche in girls, even if a minority of panelists concluded that the current data on girls puberty timing for any marker are insufficient. Current data for boys are, instead, insufficient to evaluate secular trends in male pubertal development. |
| Chen C, et al. [132] | Erratum in: BMJ Open. 2017 | Population-based cross-sectional study | 17,620 Chinese children aged 6–12 years. | 25.98% and 38.58% of boys with precocious puberty were, respectively, accompanied by obesity or central obesity. 13.86% and 29.42% of girls with precocious puberty were, respectively, accompanied by obesity or central obesity. |
| Rosenfield RL, et al. [135] | Pediatrics. 2009 | Population-based study | Comparison of stage 2 breasts, stage 3 (sexual) pubic hair, and menarche in the Third National Health and Nutrition Examination Survey sample of children with normal BMI with those with excessive BMI | Girls with excessive BMI had a significantly higher prevalence of breast appearance from ages 8.0 through 9.6 years and pubarche from ages 8.0 through 10.2 years than those with normal BMI. |
| Szamreta EA, et al. [137] | Public. Health Nutr. 2020 | Population-based study | 202 girls aged 9 or 10 years at baseline (2006–2014) | High Mediterranean-like diet adherence was associated with a later onset of thelarche and menarche. |
| Koo MM, et al. [139] | Public Health Nutr. 2002 | Prospective cohort study | 637 pre-menarcheal girls, 6 to 14 years of age | A higher intake of dietary fiber was associated with a later age at menarche. |
| Berkey CS, et al. [140] | Am J Epidemiol. 2000 | Longitudinal study | 67 Caucasian girls, birth to 10 years of age | Girls who consumed more animal protein and less vegetable protein at ages 3–5 years had earlier menarche Girls aged 1–2 years with higher dietary fat intakes and girls aged 6–8 years with higher animal protein intakes became adolescents with earlier peak growth. |
| Mervish NA, et al. [141] | Nutr Res. 2013 | Longitudinal study | 1178 girls, aged 6–8 years | Highest flavonol consumption was associated with later breast development (even if there are different limitations of the study). |
| Jansen EC, et al. [143] | J Nutr. 2015 | Prospective study | 456 girls aged 8.4 ± 1.7 years, followed for a median 5.6 years | Higher red meat intake is associated with an earlier age at menarche. Higher fatty fish intake is associated with a later menarcheal age. |
| Mueller NT, et al. [144] | Am J Clin Nutr. 2015 | Prospective study | 2379 girls (1213 African American, 1166 Caucasian) aged 9–10 years, followed for 10 years | Consumption of caffeinated and artificially sweetened soft drinks was positively associated with risk of early menarche. |
| Günther AL, et al. [145] | J Nutr. 2010 | Data collected from the longitudinal Dortmund Nutritional and Anthropometric Longitudinally Designed Study | 112 participants between 6 and 13 years | A higher total animal protein intake at 5–6 y was related to an earlier pubertal growth spurt. A higher vegetable protein intake at 3–4 and 5–6 y was related to later pubertal growth spurt. |
| Hoppe C, et al. [146] | Am J Clin Nutr. 2004 | Data analysis | 90 children (54 boys), aged 2.5 years | Milk intake was positively associated with a stimulating effect on sIGF-I concentrations and, thereby, on growth. |
| Wiley AS [147] | PLoS ONE. 2011 | Regression analysis from data collected in NHANES 1999–2004 | 2657 women age 20–49 years; 1008 girls age 9–12 years | Greater milk intake is associated with an increased risk of early menarche or a lower age at menarche. |
| Carwile JL, et al. [150] | J Nutr. 2015 | Prospective study | 5583 US girls aged 9–14 years | Frequency of milk consumption seems not to be correlated with the onset of menarche. |
| Merzenich H, et al. [149] | Am J Epidemiol. 1993 | Prospective study | 261 girls, aged 8–15 years | Increased fat intake was associated with accelerated menarche. Increased sports activity was associated with a delay in menarche. |
| Rogers IS, et al. [148] | Public Health Nutr. 2010 | Avon Longitudinal Study of Parents and Children | 3298 girls aged 3–10 years | Higher intakes of protein and meat in early to mid-childhood may lead to earlier menarche. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calcaterra, V.; Magenes, V.C.; Hruby, C.; Siccardo, F.; Mari, A.; Cordaro, E.; Fabiano, V.; Zuccotti, G. Links between Childhood Obesity, High-Fat Diet, and Central Precocious Puberty. Children 2023, 10, 241. https://doi.org/10.3390/children10020241
Calcaterra V, Magenes VC, Hruby C, Siccardo F, Mari A, Cordaro E, Fabiano V, Zuccotti G. Links between Childhood Obesity, High-Fat Diet, and Central Precocious Puberty. Children. 2023; 10(2):241. https://doi.org/10.3390/children10020241
Chicago/Turabian StyleCalcaterra, Valeria, Vittoria Carlotta Magenes, Chiara Hruby, Francesca Siccardo, Alessandra Mari, Erika Cordaro, Valentina Fabiano, and Gianvincenzo Zuccotti. 2023. "Links between Childhood Obesity, High-Fat Diet, and Central Precocious Puberty" Children 10, no. 2: 241. https://doi.org/10.3390/children10020241
APA StyleCalcaterra, V., Magenes, V. C., Hruby, C., Siccardo, F., Mari, A., Cordaro, E., Fabiano, V., & Zuccotti, G. (2023). Links between Childhood Obesity, High-Fat Diet, and Central Precocious Puberty. Children, 10(2), 241. https://doi.org/10.3390/children10020241








