Organizational Health Literacy as a Tool for Health Equity: Application in a High-Risk Infant Follow-Up Program
Abstract
:1. Introduction
2. Materials and Methods
2.1. Information Items
2.2. Environment Locations
2.3. Data Collection
2.3.1. Information Assessments
2.3.2. Environmental Assessments
2.4. Data Analysis
2.4.1. Information Assessments
| Assessment Tool | |||||||
|---|---|---|---|---|---|---|---|
| SMOG * | PMOSE/ IKIRSCH | SAM | CDC CCI | PEMAT Understandability | PEMAT Actionability | Numeracy ^ | |
| Print Material | |||||||
| Family Feedback Form | 12 | Low Level 2 Grade 8 | - | - | 11/17 (64.7%) | 4/6 (66.7%) | - |
| Clinic Welcome Packet | 14 (13) 1 | Very Low Level 1 Grade 5 | 22/44 (50%) | 10/17 (58.8%) | 10/15 (66.7%) | 2/5 (40%) | ✓ |
| MCHAT-R | 8 (6) 2 | - | - | - | 7/11 (63.6%) | 3/5 (60%) | - |
| ASQ-42 Month | 7 | Moderate Level 3 Grade 9 | - | - | 15/16 (93.8%) | 4/5 (80%) | - |
| Turning Three | 11 | - | 19/44 (43.2%) | 6/18 (33.3%) | 7/16 (43.8%) | 3/6 (50%) | ✓ |
| Average Score: | 10.4 −9.5 | Low Level 2 Grade 8 | 46.6% | 46.1% | 66.5% | 59.3% | - |
| Website Material (clinic) | |||||||
| Retinopathy of Prematurity Overview | 14 (13) 3 | - | 16/36 (44.4%) | 3/11 (27.3%) | 10/13 (76.9%) | 0/0 (0%) | ✓ |
| Hearing Loss Overview | 12 | - | 16/36 (44.4%) | 4/11 (36.4%) | 7/12 (58.3%) | 1/5 (20%) | ✓ |
| Cerebral Palsy Overview | 13 (12) 4 | - | 16/36 (44.4%) | 2/11 (18.2%) | 8/12 (66.7%) | 0/0 (0%) | - |
| Your Visit | 11 (11) 5 | - | 21/36 (58.3%) | 6/17 (35.3%) | 9/13 (69.2%) | 2/5 (40%) | - |
| Average Score: Website | 12.5 −12 | - | 47.9% | 29.3% | 67.8% | 15% | - |
| Average Score: Total (Print & Website) | 11.3 −11 | Low Level 2 Grade 8 (print) | 47.5% | 34.9% | 67.1% | 39.6% | - |
2.4.2. Environmental Assessments
3. Results
3.1. Information Assessment
3.2. Environmental Assessment
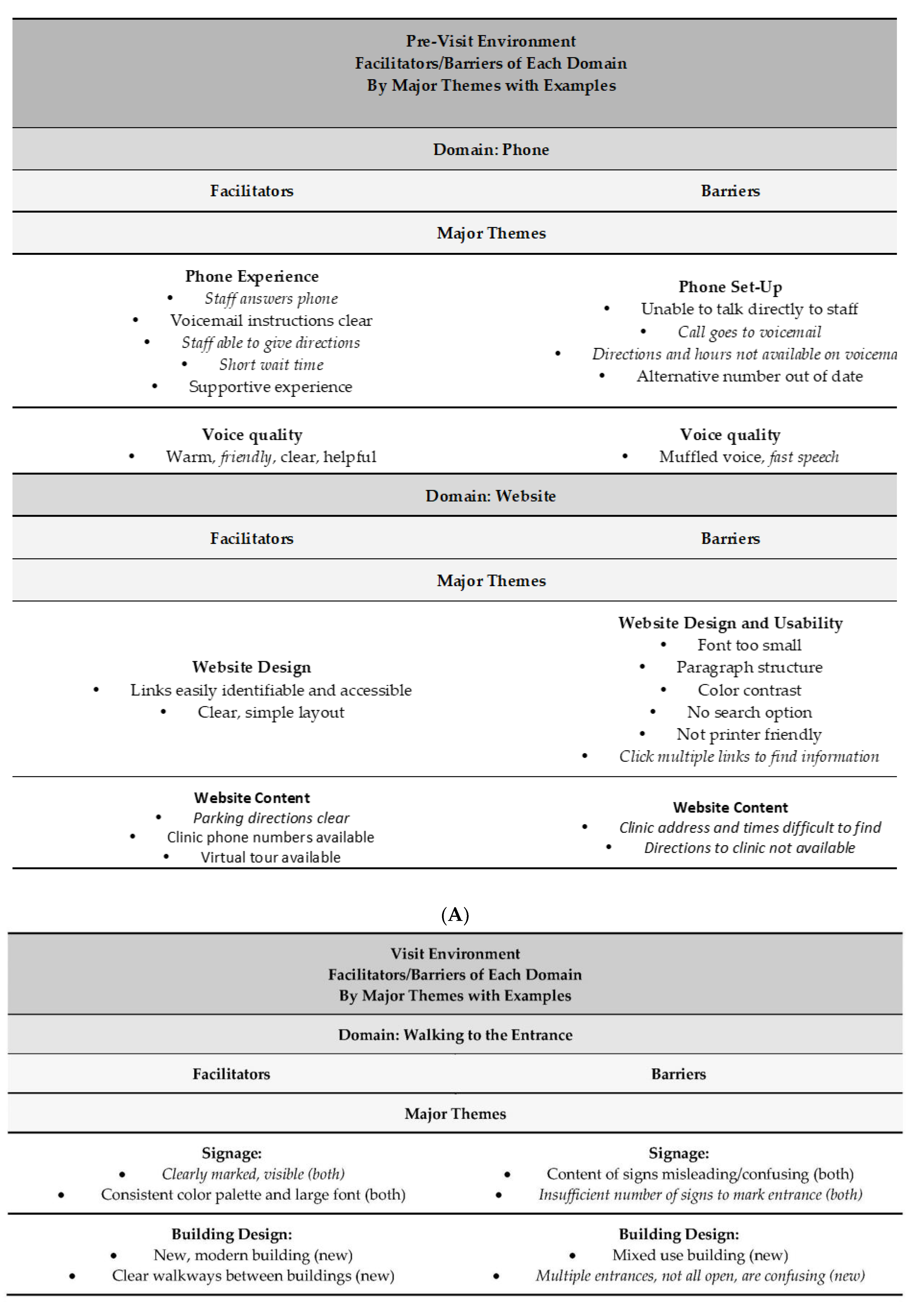
Pre-Visit Environment
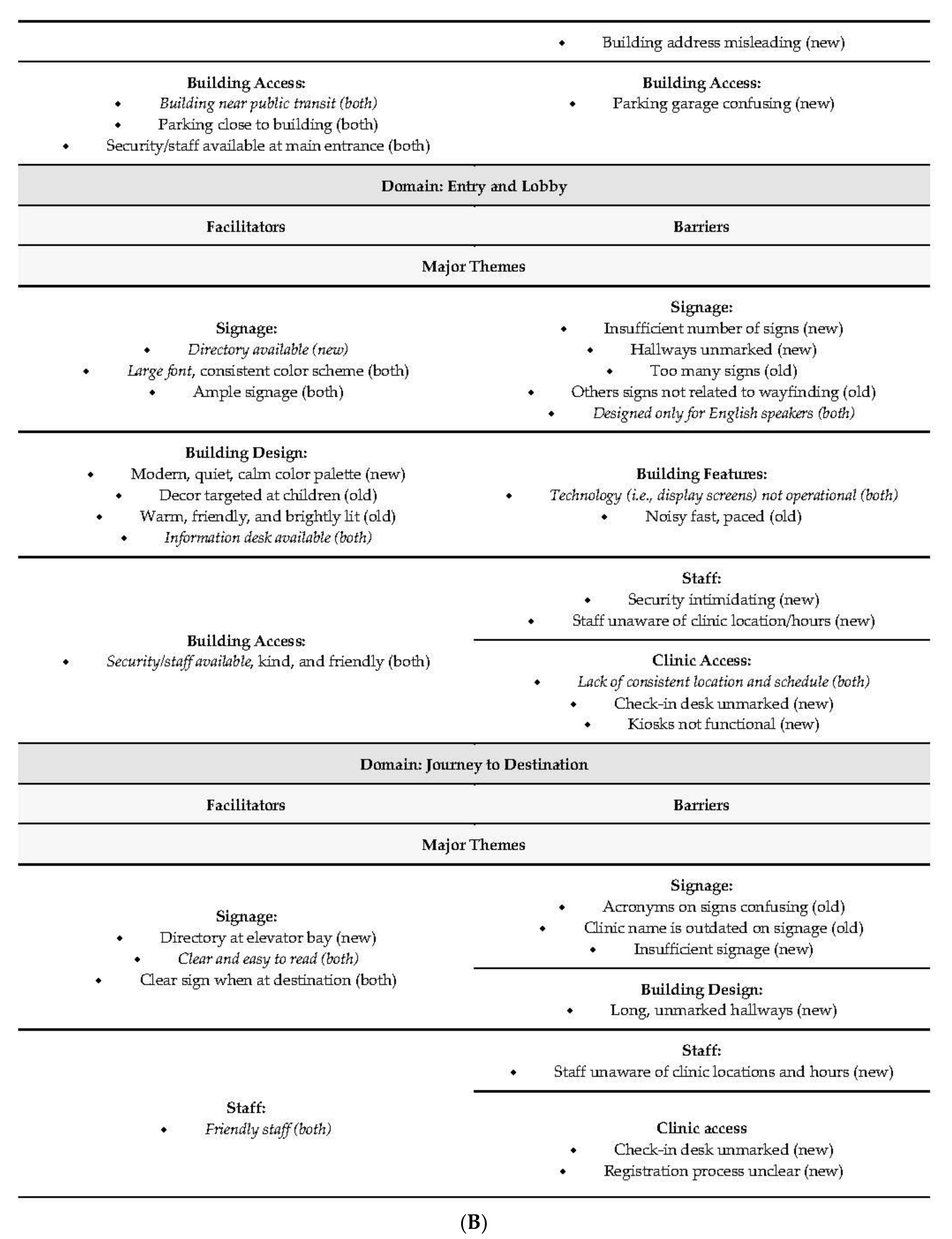
3.3. Visit Environment
4. Discussion
4.1. Moving Forward
4.2. Lessons Reinforced
4.3. Five Recommended Next Steps (Figure 2): These Results Suggest a Need for Evidence-Based Practice as Follows
4.3.1. Prioritize Plain Language in Written Text, Conversations, and Signage
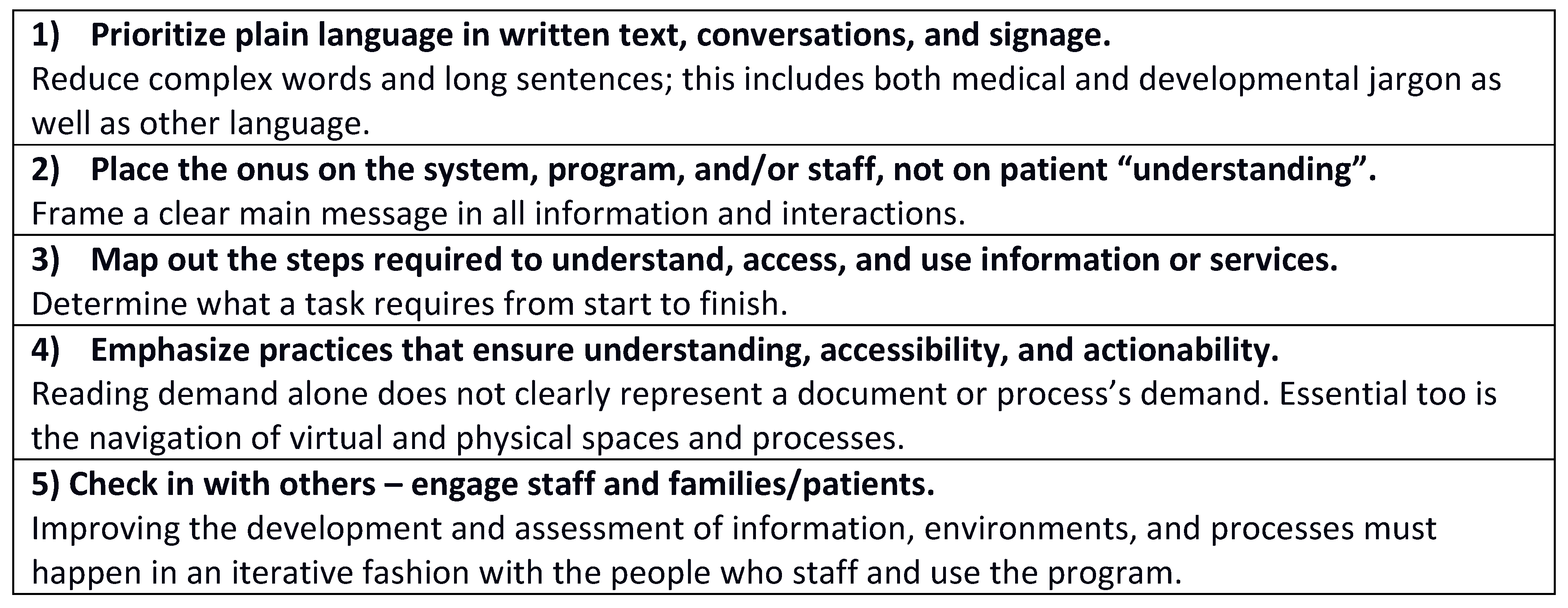
4.3.2. Place the Onus on the System, Program, and/or Staff, Not on Patient “Understanding” or Individual Skills
4.3.3. Map Out the Steps Required to Understand, Access, and Use Information or Services
4.3.4. Emphasize Practices That Ensure Understanding, Accessibility, and Actionability
4.3.5. Check In with Others—Engage Staff and Families/Patients
4.4. Implications
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bailey, Z.D.; Krieger, N.; Agénor, M.; Graves, J.; Linos, N.; Bassett, M.T. Structural racism and health inequities in the USA: Evidence and interventions. Lancet 2017, 389, 1453–1463. [Google Scholar] [CrossRef] [PubMed]
- Crear-Perry, J.; Correa-de-Araujo, R.; Johnson, T.L.; McLemore, M.R.; Neilson, E.; Wallace, M. Social and Structural Determinants of Health Inequities in Maternal Health. J. Women’s Health 2021, 30, 230–235. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, J.N.; Geller, A.; Negussie, Y.; Baciu, A. (Eds.) Communities in Action: Pathways to Health Equity; National Academies Press: Washington, DC, USA, 2017. [Google Scholar] [CrossRef]
- Whitman, A.; De Lew, N.; Chappel, A.; Aysola, V.; Zuckerman, R.; Sommers, B.D. Addressing Social Determinants of Health: Examples of Successful Evidence-Based Strategies and Current Federal Efforts; ASPE—Office of Health Policy: Washington, DC, USA, 2022. [Google Scholar]
- CDC’s Patient Navigation. Centers for Disease Control and Prevention, Cancer Resources for Clinics and Communities. 10 July 2023. Available online: https://www.cdc.gov/cancer/community-resources/interventions/patient-navigation.htm (accessed on 20 July 2023).
- Bolan, M. Housing and Employment Navigator Program Evaluation. Department of Labor Workforce Innovation Fund Grant, June 2017. Available online: https://buildingchanges.org/wp-content/uploads/2017/07/2017_HousingandEmploymentNavigator_Findings.pdf (accessed on 19 September 2023).
- Lopez, C.; Kim, B.; Sacks, K. Health Literacy in the United States: Enhancing Assessments and Reducing Disparities. Milken Institute, 2022. Available online: https://milkeninstitute.org/sites/default/files/2022-05/Health_Literacy_United_States_Final_Report.pdf (accessed on 19 September 2023).
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Helpern, D.J.; Viera, A.; Cortty, K.; Holland, A.; Brasure, M.; Lohr, K.N.; Harden, E.; et al. Health literacy interventions and outcomes: An updated systematic review. Evid. Report/Technol. Assess. 2011, 199, 1–941. [Google Scholar]
- Institute of Medicine (US) Committee on Health Literacy. Health Literacy: A Prescription to End Confusion; National Academies Press (US): Washington, DC, USA, 2004. Available online: http://www.ncbi.nlm.nih.gov/books/NBK216032/ (accessed on 24 July 2023).
- Rowlands, G.; Protheroe, J.; Winkley, J.; Richardson, M.; Seed, P.T.; Rudd, R. A mismatch between population health literacy and the complexity of health information: An observational study. Br. J. Gen. Pract. 2015, 65, e379–e386. [Google Scholar] [CrossRef]
- Baumeister, A.; Chakraverty, D.; Aldin, A.; Seven, Ü.S.; Skoetz, N.; Kalbe, E.; Woopen, C. ‘The system has to be health literate, too’—Perspectives among healthcare professionals on health literacy in transcultural treatment settings. BMC Health Serv. Res. 2021, 21, 716. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeld, L.; Miller, A.; Garverich, S.; Guyer, M.; Steiner, R.; Lincoln, A.K. Performing an Organizational Health Literacy Assessment in a Shelter Serving People with Mental Illness. HLRP Health Lit. Res. Pract. 2022, 6, e167–e174. [Google Scholar] [CrossRef]
- Braveman, P.; Gottlieb, L. The Social Determinants of Health: It’s Time to Consider the Causes of the Causes. Public Health Rep. 2014, 129, 19–31. [Google Scholar] [CrossRef]
- McCormick, M.C.; Litt, J.S.; Smith, V.C.; Zupancic, J.A.F. Prematurity: An Overview and Public Health Implications. Annu. Rev. Public Health 2011, 32, 367–379. [Google Scholar] [CrossRef]
- Healthy People 2030. Available online: https://health.gov/healthypeople (accessed on 24 July 2023).
- CDC’s Health Literacy. Centers for Disease Control and Prevention. 10 July 2023. Available online: https://www.cdc.gov/healthliteracy/index.html (accessed on 20 July 2023).
- Commission, T.J. ‘What Did the Doctor Say?’: Improving Health Literacy to Protect Patient Safety. 2007. Available online: https://swselfmanagement.ca/uploads/ResourceDocuments/The%20Joint%20Commission%20(2007)%20Improving%20Health%20Literacy%20for%20Patient%20Safety.pdf (accessed on 19 September 2023).
- FY 2021 Grant Awards—The Office of Minority Health. Available online: https://www.minorityhealth.hhs.gov/omh/browse.aspx?lvl=2&lvlid=88 (accessed on 20 July 2023).
- Health Literacy in Healthy People 2030—Healthy People 2030. Available online: https://health.gov/healthypeople/priority-areas/health-literacy-healthy-people-2030 (accessed on 24 July 2023).
- Batool, S.H.; Safdar, M.; Eman, S. Relationship between parents’ health literacy and child health: Systematic review. Libr. Hi Tech, 2022; ahead-of-print. [Google Scholar] [CrossRef]
- Keim-Malpass, J.; Letzkus, L.C.; Kennedy, C. Parent/caregiver health literacy among children with special health care needs: A systematic review of the literature. BMC Pediatr. 2015, 15, 92. [Google Scholar] [CrossRef]
- Sanders, L.M.; Federico, S.; Klass, P.; Abrams, M.A.; Dreyer, B. Literacy and Child Health: A Systematic Review. Arch. Pediatr. Adolesc. Med. 2009, 163, 131–140. [Google Scholar] [CrossRef]
- DeWalt, D.A.; Hink, A. Health literacy and child health outcomes: A systematic review of the literature. Pediatrics 2009, 124 (Suppl. 3), S265–S274. [Google Scholar] [CrossRef] [PubMed]
- Kumar, D.; Sanders, L.; Perrin, E.M.; Lokker, N.; Patterson, B.; Gunn, V.; Finkle, J.; Franco, V.; Choi, L.; Rothman, R.L. Parental Understanding of Infant Health Information: Health Literacy, Numeracy, and the Parental Health Literacy Activities Test (PHLAT). Acad. Pediatr. 2010, 10, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Leslie, C.; Crehan, J. Impact of Health Literacy on Early Intervention (EI) Access and Utilization: A Scoping Review. Am. J. Occup. Ther. 2020, 74 (Suppl. 1), 7411510280p1. [Google Scholar] [CrossRef]
- So, M.; Franks, J.L.; Cree, R.A.; Leeb, R.T. An Evaluation of the Literacy Demands of Online Natural Disaster Preparedness Materials for Families. Disaster Med. Public Health Prep. 2020, 14, 449–458. [Google Scholar] [CrossRef]
- Świątkiewicz-Mośny, M.; Prokop-Dorner, A.; Ślusarczyk, M.; Ożegalska-Łukasik, N.; Piłat-Kobla, A.; Zając, J.; Bala, M.M. When Peppa Pig and Confucius meet, joining forces on the battlefield of health literacy–a qualitative analysis of COVID-19 educational materials for children and adolescents from China, the USA, and Europe. PLoS ONE 2022, 17, e0278554. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Roundtable on Health Literacy. Developing Health Literacy Skills in Children and Youth: Proceedings of a Workshop. In The National Academies Collection: Reports Funded by National Institutes of Health; National Academies Press (US): Washington, DC, USA, 2020. Available online: http://www.ncbi.nlm.nih.gov/books/NBK562692/ (accessed on 18 August 2023).
- Naccarella, L.; Guo, S. A Health Equity Implementation Approach to Child Health Literacy Interventions. Children 2022, 9, 1284. [Google Scholar] [CrossRef] [PubMed]
- Fairbrother, H.; Curtis, P.; Goyder, E. Making health information meaningful: Children’s health literacy practices. SSM Popul. Health 2016, 2, 476–484. [Google Scholar] [CrossRef]
- Rosenfeld, L.; Litt, J.S. To Achieve Equitable, Integrated Care for Children, Family-centered Work Must Focus on Systems. Fam. Syst. Health, 2023; in press. [Google Scholar]
- Morrison, A.K.; Glick, A.; Yin, H.S. Health Literacy: Implications for Child Health. Pediatr. Rev. 2019, 40, 263–277. [Google Scholar] [CrossRef]
- Abrams, M.A.; Klass, P.; Dreyer, B.P. Health Literacy and Children: Recommendations for Action. Pediatrics 2009, 124 (Suppl. 3), S327–S331. [Google Scholar] [CrossRef]
- Groene, R.O.; Rudd, R.E. Results of a feasibility study to assess the health literacy environment: Navigation, written, and oral communication in 10 hospitals in Catalonia, Spain. J. Commun. Healthc. 2011, 4, 227–237. [Google Scholar] [CrossRef]
- Horowitz, A.M.; Maybury, C.; Kleinman, D.V.; Radice, S.D.; Wang, M.Q.; Child, W.; Rudd, R.E. Health Literacy Environmental Scans of Community-Based Dental Clinics in Maryland. Am. J. Public Health 2014, 104, e85–e93. [Google Scholar] [CrossRef]
- Ownby, R.L.; Waldrop-Valverde, D.; Caballero, J.; Jacobs, R.J. Baseline medication adherence and response to an electronically delivered health literacy intervention targeting adherence. Neurobehav. HIV Med. 2012, 4, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeld, L.; Shepherd, A.; Agunwamba, A.A.; McCray, A.T. Iterative evaluation of a web-based health information resource. J. Health Commun. 2013, 18, 974–990. [Google Scholar] [CrossRef] [PubMed]
- Sudore, R.L.; Schillinger, D. Interventions to Improve Care for Patients with Limited Health Literacy. J. Clin. Outcomes Manag. 2009, 16, 20–29. [Google Scholar] [PubMed]
- Rudd, R.E. Health Literacy: Insights and Issues. Stud. Health Technol. Inform. 2017, 240, 60–78. [Google Scholar]
- Litt, J.S.; Edwards, E.; Lainwala, S.; Mercier, C.; Montgomery, A.; O’Reilly, D.; Rhein, L.; Woythaler, M.; Hartman, T.; on behalf of the New England Follow-up Network. Optimizing High-risk Infant Follow-up in Nonresearch-based Paradigms: The New England Follow-up Network. Pediatr. Qual. Saf. 2020, 5, e287. [Google Scholar] [CrossRef]
- Litt, J.S.; McCormick, M.C. Preterm infants are less likely to have a family-centered medical home than term-born peers. J. Perinatol. Off. J. Calif. Perinat. Assoc. 2018, 38, 1391–1397. [Google Scholar] [CrossRef]
- Follow-up Care of High-Risk Infants. Pediatrics 2004, 114 (Suppl. 5), 1377–1397. [CrossRef]
- Fraiman, Y.S.; Edwards, E.M.; Horbar, J.D.; Mercier, C.E.; Soll, R.F.; Litt, J.S. Racial Inequity in High-Risk Infant Follow-Up Among Extremely Low Birth Weight Infants. Pediatrics 2023, 151, e2022057865. [Google Scholar] [CrossRef]
- Fraiman, Y.S.; Stewart, J.E.; Litt, J.S. Race, language, and neighborhood predict high-risk preterm Infant Follow Up Program participation. J. Perinatol. Off. J. Calif. Perinat. Assoc. 2022, 42, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Laughlin, G.H.M. SMOG Grading—A New Readability Formula. J. Read. 1969, 12, 639–646. [Google Scholar]
- Doak, C.C.; Doak, L.G.; Root, J.H. Teaching Patients with Low Literacy Skills; JB Lippincott Company: Philadelphia, PA, USA, 1996. [Google Scholar]
- Mosenthal, P.B.; Kirsch, I.S. A New Measure of Assessing Document Complexity: The PMOSE/IKIRSCH Document Readability Formula. J. Adolesc. Adult Lit. 1998, 41, 638–657. [Google Scholar]
- Shoemaker, S.J.; Wolf, M.S.; Brach, C. Development of the Patient Education Materials Assessment Tool (PEMAT): A new measure of understandability and actionability for print and audiovisual patient information. Patient Educ. Couns. 2014, 96, 395–403. [Google Scholar] [CrossRef] [PubMed]
- CDC. The CDC Clear Communication Index. Centers for Disease Control and Prevention. 28 June 2023. Available online: https://www.cdc.gov/ccindex/index.html (accessed on 18 August 2023).
- Apter, A.J.; Paasche-Orlow, M.K.; Remillard, J.T.; Bennett, I.M.; Ben-Joseph, E.P.; Batista, R.M.; Hyde, J.; Rudd, R.E. Numeracy and Communication with Patients: They Are Counting on Us. J. Gen. Intern. Med. 2008, 23, 2117–2124. [Google Scholar] [CrossRef]
- Rudd, R. Health Literacy Environment Activity Packet: First Impressions and Walking Interview. 2010. Available online: https://www.hsph.harvard.edu/wp-content/uploads/sites/135/2012/09/activitypacket.pdf (accessed on 19 September 2023).
- Labra, O.; Castro, C.; Wright, R.; Chamblas, I. Thematic Analysis in Social Work: A Case Study. In Global Social Work—Cutting Edge Issues and Critical Reflections; IntechOpen: London, UK, 2019. [Google Scholar] [CrossRef]
- Madill, A.; Jordan, A.; Shirley, C. Objectivity and reliability in qualitative analysis: Realist, contextualist and radical constructionist epistemologies. Br. J. Psychol. 2000, 91, 1–20. [Google Scholar] [CrossRef]
- Liamputtong, P.; Ezzy, D. Qualitative Research Methods; Oxford University Press: Melbourne, Australia, 2005. Available online: http://catdir.loc.gov/catdir/enhancements/fy0637/2005276163-t.html (accessed on 18 August 2023).
- Rudd, R.; Oelschlegel, S.; Tester, E.; Heidel, E.; The Health Literacy Task Force of the University of Tennessee Medical Center. The Health Literacy Environment of Hospitals and Health Centers. 2019. Available online: https://www.hsph.harvard.edu/wp-content/uploads/sites/135/2019/05/april-30-FINAL_The-Health-Literacy-Environment2_Locked.pdf (accessed on 19 September 2023).
- Harrington, K.F.; Haven, K.M.; Bailey, W.C.; Gerald, L.B. Provider Perceptions of Parent Health Literacy and Effect on Asthma Treatment Recommendations and Instructions. Pediatr. Allergy Immunol. Pulmonol. 2013, 26, 69–75. [Google Scholar] [CrossRef]
- Schappin, R.; Wijnroks, L.; Uniken Venema, M.M.A.T.; Jongmans, M.J. Rethinking stress in parents of preterm infants: A meta-analysis. PLoS ONE 2013, 8, e54992. [Google Scholar] [CrossRef]
- Rudd, R. Background and Overview. In Implications of Health Literacy for Public Health: Workshop Summary; National Academies Press (US): Washington, DC, USA, 2014. Available online: https://www.ncbi.nlm.nih.gov/books/NBK242431/ (accessed on 18 August 2023).
- Strategies to Improve Organizational Health Literacy. Sep. 2021. Available online: https://psnet.ahrq.gov/primer/strategies-improve-organizational-health-literacy (accessed on 18 August 2023).
- AHRQ Health Literacy Universal Precautions Toolkit. Available online: https://www.ahrq.gov/health-literacy/improve/precautions/index.html (accessed on 18 August 2023).
- The Roles of Trust and Health Literacy in Achieving Health Equity A Workshop Series. National Academies. Available online: https://www.nationalacademies.org/our-work/the-roles-of-trust-and-health-literacy-in-achieving-health-equity-a-workshop-series (accessed on 18 August 2023).
- Rothwell, J. Assessing the Economic Gains of Eradicating Illiteracy Nationally and Regionally in the United States. Barbara Bush Foundation for Family Literacy, 2020. Available online: https://www.barbarabush.org/wp-content/uploads/2020/09/BBFoundation_GainsFromEradicatingIlliteracy_9_8.pdf (accessed on 19 September 2023).
- Brach, C.; Keller, D.; Hernandez, L.M.; Baur, C.; Parker, R.; Dreyer, B.; Schyve, P.; Lemerise, A.J.; Schillinger, D. Ten Attributes of Health Literate Health Care Organizations; National Academy of Sciences: Washington, DC, USA, 2012. [Google Scholar]
- Coleman, C.; Birk, S.; DeVoe, J. Health Literacy and Systemic Racism-Using Clear Communication to Reduce Health Care Inequities. JAMA Intern. Med. 2023, 183, 753–754. [Google Scholar] [CrossRef]
| Material | Description |
|---|---|
| Family Feedback Form (2021) | A two-page handout given to parents/guardians of children seen in the clinic. The document outlines the major findings and recommendations from the visit and common referrals and resources. |
| Clinic Welcome Packet (2021) | A comprehensive letter distributed to parents/guardians of the clinic. It summarizes the program goals and objectives, answers common questions, and provides a referral form. |
| MCHAT-R (2021) | The Modified Checklist for Autism in Toddlers–Revised. A parent-reported screening checklist to assess the risk of an autism spectrum disorder diagnosis among young children. |
| ASQ-42 Month (2021) | The Ages & Stages Questionnaires, 42 Month. A parent-reported assessment to screen for developmental delays or other crucial milestones when a child is 42 months old. The questionnaires are completed by parents and scored by professionals. |
| Clinic Website|Retinopathy of Prematurity Overview (2021) | A web page connected to the clinic on the hospital website. It aims to educate parents/guardians on retinopathy of prematurity in children. |
| Clinic Website|Hearing Loss Overview (2021) | A web page connected to the clinic on the hospital website. It aims to educate parents/guardians on hearing loss in children. |
| Clinic Website|Cerebral Palsy Overview (2021) | A web page connected to the clinic on the hospital website. It aims to educate parents/guardians on cerebral palsy in children. |
| Clinic Website|Your Visit (2021) | A web page connected to the clinic on the hospital website. It aims to educate parents/guardians on the details of each visit to the clinic. |
| Turning Three (2021) | A presentation offered to parents/guardians of the clinic, developed by the Federation for Children with Special Needs Parent Training and Information Center, to help educate parents/guardians on the intricacies of Early Intervention and Special Education starting at age 3. |
| Material | Numeric Demand | ||
|---|---|---|---|
| Describe | Interpret | Decision | |
| Clinic Welcome Packet | 0% | 33.30% | 66.70% |
| Clinic Website—Retinopathy of Prematurity Overview | 60% | 40% | 0% |
| Clinic Website—Hearing Loss Overview | 40% | 80% | 0% |
| Turning Three | 0% | 33.30% | 66.70% |
| Domain ** | Sub-Domain, Part | Score % + |
|---|---|---|
| Institutional Practices | -- | 66% |
| Part 1: Resources | 100% | |
| Part 2: Orientation, Development, | 55% | |
| and Expectations | ||
| Orientation | 69% | |
| Development | 30% | |
| Expectations | 67% | |
| Navigation | -- | 68% |
| Part 1: Arrival | 22% | |
| Arrival and Departure | 0% | |
| Entry and Lobby Access | 40% | |
| Part 2: Wayfinding | 89% | |
| Staff Assistance | 94% | |
| Hallways and Navigation Ease | 83% | |
| Services and Specialty Areas | 100% | |
| Culture and Language | -- | 66% |
| Communication | -- | 52% |
| Print Materials | 46% | |
| Forms | 42% | |
| Websites | 51% | |
| Patient Portals | 71% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosenfeld, L.E.; McCullagh, K.; King, C.J.; Torres, M.; Litt, J.S. Organizational Health Literacy as a Tool for Health Equity: Application in a High-Risk Infant Follow-Up Program. Children 2023, 10, 1658. https://doi.org/10.3390/children10101658
Rosenfeld LE, McCullagh K, King CJ, Torres M, Litt JS. Organizational Health Literacy as a Tool for Health Equity: Application in a High-Risk Infant Follow-Up Program. Children. 2023; 10(10):1658. https://doi.org/10.3390/children10101658
Chicago/Turabian StyleRosenfeld, Lindsay E., Kelly McCullagh, Carolyn J. King, Micaela Torres, and Jonathan S. Litt. 2023. "Organizational Health Literacy as a Tool for Health Equity: Application in a High-Risk Infant Follow-Up Program" Children 10, no. 10: 1658. https://doi.org/10.3390/children10101658
APA StyleRosenfeld, L. E., McCullagh, K., King, C. J., Torres, M., & Litt, J. S. (2023). Organizational Health Literacy as a Tool for Health Equity: Application in a High-Risk Infant Follow-Up Program. Children, 10(10), 1658. https://doi.org/10.3390/children10101658





