Uncommon Large and Bilateral Fibrous Cephalic Plaques in a Patient with TSC2-Related Tuberous Sclerosis Complex
Abstract
:1. Introduction
2. Case Report
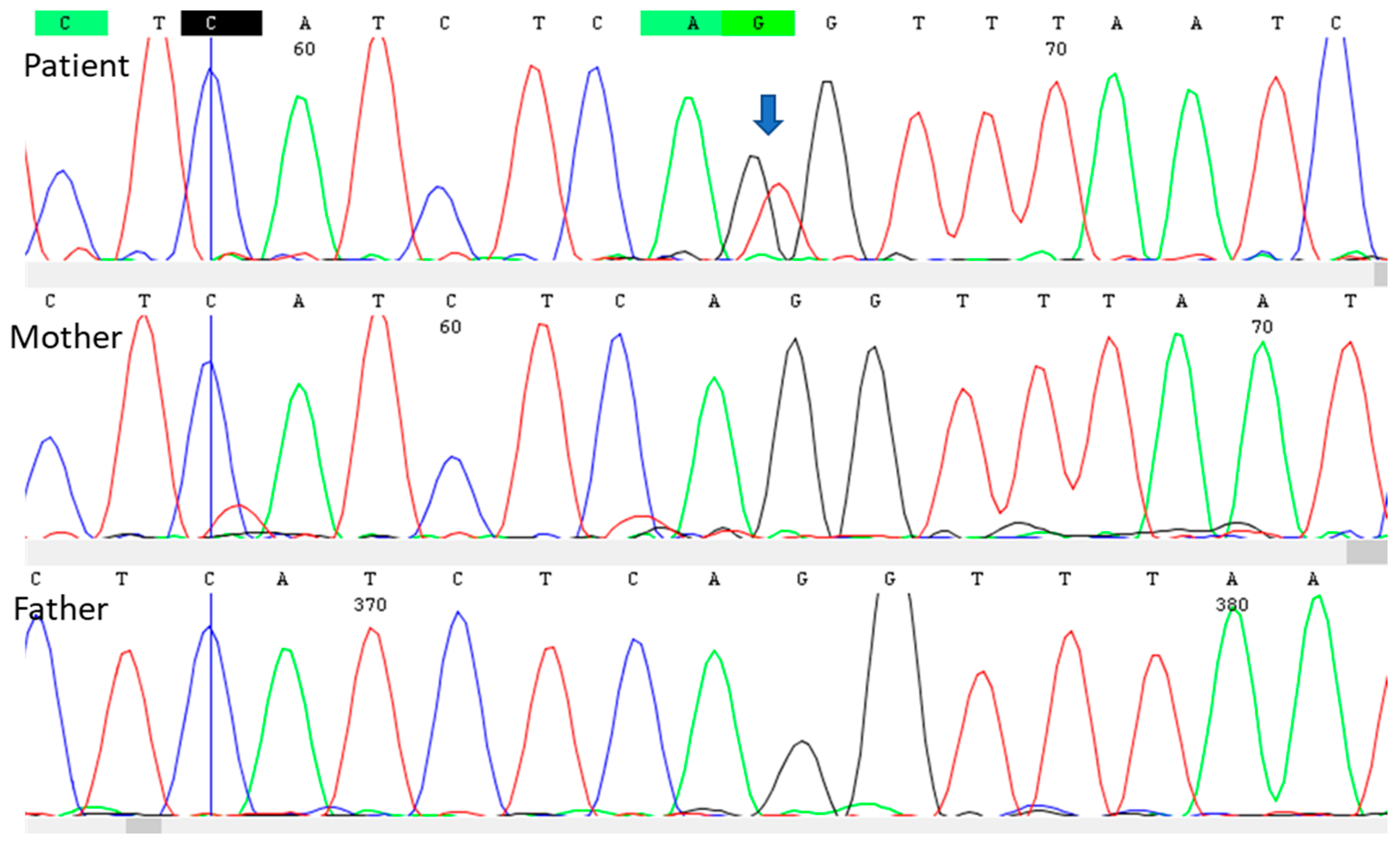
3. Genetic Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Oyerinde, O.; Buccine, D.; Treichel, A.; Hong, C.; Lee, C.R.; Moss, J.; Darling, T.N. Fibrous cephalic plaques in tuberous sclerosis complex. J. Am. Acad. Dermatol. 2018, 78, 717–724. [Google Scholar] [CrossRef] [PubMed]
- Northrup, H.; Aronow, M.E.; Bebin, E.M.; Bissler, J.; Darling, T.N.; de Vries, P.J.; Frost, M.D.; Fuchs, Z.; Gosnell, E.S.; Gupta, N.; et al. International Tuberous Sclerosis Complex Consensus Group. Updated International Tuberous Sclerosis Complex Diagnostic Criteria and Surveillance and Management Recommendations. Pediatr. Neurol. 2021, 123, 50–66. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, R.A.; Fernández, G.; Kotulska, K.; Jóźwiak, S. Tuberous sclerosis complex: Advances in diagnosis, genetics, and management. J. Am. Acad. Dermatol. 2007, 57, 189–202. [Google Scholar] [CrossRef] [PubMed]
- Nickel, W.R.; Reed, W.B. Tuberous sclerosis. Special reference to the microscopic alterations in the cutaneous hamartomas. Arch. Dermatol. 1962, 85, 209–226. [Google Scholar] [CrossRef] [PubMed]
- Dabora, S.L.; Jozwiak, S.; Franz, D.N.; Roberts, P.S.; Nieto, A.; Chung, J.; Choy, Y.S.; Reeve, M.P.; Thiele, E.; Egelhoff, J.C.; et al. Mutational analysis in a cohort of 224 tuberous sclerosis patients indicates increased severity of TSC2, compared with TSC1, disease in multiple organs. Am. J. Hum. Genet. 2001, 68, 64–80. [Google Scholar] [CrossRef] [PubMed]
- Apam-Garduño, D.; Cazarín-Barrientos, J.; Hernández-Martínez, N.L.; Reyna-Fabián, M.E.; Magaña, M.; Alcántara-Ortigoza, M.A.; González-Del Angel, A.; Rivera-Vega, M.R. Clinical, pathological, and molecular correlation of folliculocystic and collagen hamartoma: A new potential diagnostic criterion for tuberous sclerosis complex? J. Cutan. Pathol. 2023, 50, 481–486. [Google Scholar] [CrossRef] [PubMed]
- Reyna-Fabián, M.E.; Hernández-Martínez, N.L.; Alcántara-Ortigoza, M.A.; Ayala-Sumuano, J.T.; Enríquez-Flores, S.; Velázquez-Aragón, J.A.; Varela-Echavarría, A.; Todd-Quiñones, C.G.; González-Del Angel, A. First comprehensive TSC1/TSC2 mutational analysis in Mexican patients with Tuberous Sclerosis Complex reveals numerous novel pathogenic variants. Sci. Rep. 2020, 10, 6589. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, E.; Saskatchewan, R. Unusual cutaneous manifestations of tuberous sclerosis: Case report. Plast. Reconstr. Surg. 1967, 40, 153–156. [Google Scholar] [CrossRef] [PubMed]
- Pereira da Silva Neto, M.; Rodovalho de Assis, B.; Rodrigues Andrade, G. Sebaceous nevus of Jadassohn: Review and clinical-surgical approach. An. Bras. Dermatol. 2022, 97, 628–636. [Google Scholar] [CrossRef] [PubMed]
- Özdoğan, S.; Saymaz, C.; Yaltırık, C.K.; Düzkalır, H.G.; Kaya, M.; Demirel, N.; Düzkalır, A.H.; Sarıkaya, B.; Aktekin, B. Encephalocraniocutaneous Lipomatosis: Haberland Syndrome. Am. J. Case Rep. 2017, 18, 1271–1275. [Google Scholar] [CrossRef] [PubMed]
- Rama Rao, G.R.; Krishna Rao, P.V.; Gopal, K.V.; Kumar, Y.H.; Ramachandra, B.V. Forehead plaque: A cutaneous marker of CNS involvement in tuberous sclerosis. Indian. J. Dermatol. Venereol. Leprol. 2008, 74, 28–31. [Google Scholar] [CrossRef] [PubMed]
- Umeoka, S.; Koyama, T.; Miki, Y.; Akai, M.; Tsutsui, K.; Togashi, K. Pictorial review of tuberous sclerosis in various organs. Radiographics 2008, 28, e32. [Google Scholar] [CrossRef] [PubMed]
- Morris, B.S.; Garg, A.; Jadhav, P.J. Tuberous sclerosis: A presentation of less-commonly encountered stigmata. Australas. Radiol. 2002, 46, 426–430. [Google Scholar] [CrossRef] [PubMed]
- Sancak, O.; Nellist, M.; Goedbloed, M.; Elfferich, P.; Wouters, C.; Maat-Kievit, A.; Zonnenberg, B.; Verhoef, S.; Halley, D.; van den Ouweland, A. Mutational analysis of the TSC1 and TSC2 genes in a diagnostic setting: Genotype—Phenotype correlations and comparison of diagnostic DNA techniques in Tuberous Sclerosis Complex. Eur. J. Hum. Genet. 2005, 13, 731–741. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-del Angel, A.; Ruiz-Herrera, A.; Hernández-Martínez, N.L.; Todd-Quiñones, C.G.; Durán-McKinster, C.; Herrera-Mora, P.; Alcántara-Ortigoza, M.A. Uncommon Large and Bilateral Fibrous Cephalic Plaques in a Patient with TSC2-Related Tuberous Sclerosis Complex. Children 2023, 10, 1614. https://doi.org/10.3390/children10101614
González-del Angel A, Ruiz-Herrera A, Hernández-Martínez NL, Todd-Quiñones CG, Durán-McKinster C, Herrera-Mora P, Alcántara-Ortigoza MA. Uncommon Large and Bilateral Fibrous Cephalic Plaques in a Patient with TSC2-Related Tuberous Sclerosis Complex. Children. 2023; 10(10):1614. https://doi.org/10.3390/children10101614
Chicago/Turabian StyleGonzález-del Angel, Ariadna, Adriana Ruiz-Herrera, Nancy Leticia Hernández-Martínez, Carlos G. Todd-Quiñones, Carola Durán-McKinster, Patricia Herrera-Mora, and Miguel Angel Alcántara-Ortigoza. 2023. "Uncommon Large and Bilateral Fibrous Cephalic Plaques in a Patient with TSC2-Related Tuberous Sclerosis Complex" Children 10, no. 10: 1614. https://doi.org/10.3390/children10101614
APA StyleGonzález-del Angel, A., Ruiz-Herrera, A., Hernández-Martínez, N. L., Todd-Quiñones, C. G., Durán-McKinster, C., Herrera-Mora, P., & Alcántara-Ortigoza, M. A. (2023). Uncommon Large and Bilateral Fibrous Cephalic Plaques in a Patient with TSC2-Related Tuberous Sclerosis Complex. Children, 10(10), 1614. https://doi.org/10.3390/children10101614




