A Novel Nomogram Based on Quantitative MRI and Clinical Features for the Prediction of Neonatal Intracranial Hypertension
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Patients and Public Involvement
2.3. Details of MRI Acquisition
2.4. MR Image Processing
2.5. Model Development
2.6. Model Assessment
2.7. Statistical Analysis
3. Results
3.1. Clinical Characteristics and Volumetric Segmentation
3.2. Selected Predictors
3.3. Performance of the Prediction Model
Discrimination and Calibration
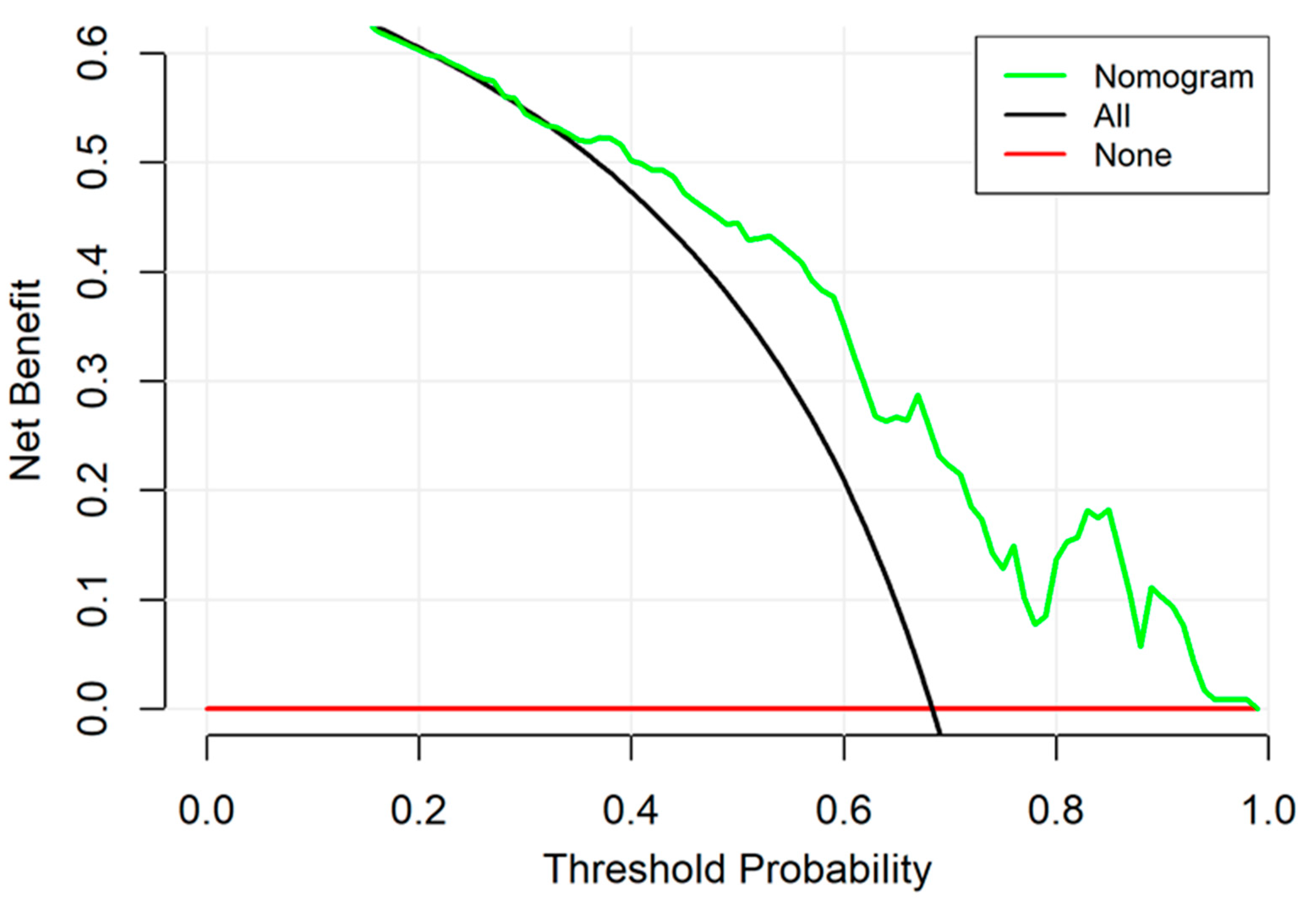
3.4. Clinical Utility
4. Discussion
Limitations and Further Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sands, R.; Shanmugavadivel, D.; Stephenson, T.; Wood, D. Medical problems presenting to paediatric emergency departments: 10 years on. Emerg. Med. J. 2012, 29, 379–382. [Google Scholar] [CrossRef]
- Gillson, N.; Jones, C.; Reem, R.E.; Rogers, D.L.; Zumberge, N.; Aylward, S.C. Incidence and Demographics of Pediatric Intracranial Hypertension. Pediatr. Neurol. 2017, 73, 42–47. [Google Scholar] [CrossRef]
- Tibussek, D.; Distelmaier, F.; Von Kries, R.; Mayatepek, E. Pseudotumor cerebri in childhood and adolescence—Results of a Germany-wide ESPED-survey. Klin. Padiatr. 2013, 225, 81–85. [Google Scholar] [CrossRef]
- Dessardo, N.S.; Dessardo, S.; Sasso, A.; Sarunic, A.V.; Dezulovic, M.S. Pediatric idiopathic intracranial hypertension: Clinical and demographic features. Coll. Antropol. 2010, 34 (Suppl. S2), 217–221. [Google Scholar] [PubMed]
- Gordon, K. Pediatric pseudotumor cerebri: Descriptive epidemiology. Can. J. Neurol. Sci. 1997, 24, 219–221. [Google Scholar] [PubMed]
- Kayhanian, S.; Young, A.M.H.; Piper, R.J.; Donnelly, J.; Scoffings, D.; Garnett, M.R.; Fernandes, H.M.; Smielewski, P.; Czosnyka, M.; Hutchinson, P.J.; et al. Radiological Correlates of Raised Intracranial Pressure in Children: A Review. Front. Pediatr. 2018, 6, 32. [Google Scholar] [CrossRef] [PubMed]
- Hu, R.; Holbrook, J.; Newman, N.J.; Biousse, V.; Bruce, B.B.; Qiu, D.; Oshinski, J.; Saindane, A.M. Cerebrospinal Fluid Pressure Reduction Results in Dynamic Changes in Optic Nerve Angle on Magnetic Resonance Imaging. J. Neuroophthalmol. 2019, 39, 35–40. [Google Scholar] [CrossRef]
- Sekhon, M.S.; Griesdale, D.E.; Robba, C.; McGlashan, N.; Needham, E.; Walland, K.; Shook, A.C.; Smielewski, P.; Czosnyka, M.; Gupta, A.K.; et al. Optic nerve sheath diameter on computed tomography is correlated with simultaneously measured intracranial pressure in patients with severe traumatic brain injury. Intensive Care Med. 2014, 40, 1267–1274. [Google Scholar] [CrossRef]
- Yuh, W.T.; Zhu, M.; Taoka, T.; Quets, J.P.; Maley, J.E.; Muhonen, M.G.; Schuster, M.E.; Kardon, R.H. MR imaging of pituitary morphology in idiopathic intracranial hypertension. J. Magn. Reson. Imaging 2000, 12, 808–813. [Google Scholar] [CrossRef]
- Paul, S.; Smith, J.; Green, J.; Smith-Collins, A.; Chinthapalli, R. Managing children with raised intracranial pressure: Part one (introduction and meningitis). Nurs. Child. Young People 2013, 25, 31–36. [Google Scholar] [CrossRef]
- Hawryluk, G.W.J.; Citerio, G.; Hutchinson, P.; Kolias, A.; Meyfroidt, G.; Robba, C.; Stocchetti, N.; Chesnut, R. Intracranial pressure: Current perspectives on physiology and monitoring. Intensive Care Med. 2022, 48, 1471–1481. [Google Scholar] [CrossRef] [PubMed]
- Hegendorfer, E.; Vaes, B.; Van Pottelbergh, G.; Mathei, C.; Verbakel, J.; Degryse, J.M. Predictive Accuracy of Frailty Tools for Adverse Outcomes in a Cohort of Adults 80 Years and Older: A Decision Curve Analysis. J. Am. Med. Dir. Assoc. 2020, 21, 440.e1–440.e8. [Google Scholar] [CrossRef] [PubMed]
- Van Calster, B.; Wynants, L.; Verbeek, J.F.; Verbakel, J.Y.; Christodoulou, E.; Vickers, A.J.; Roobol, M.J.; Steyerberg, E.W. Reporting and Interpreting Decision Curve Analysis: A Guide for Investigators. Eur. Urol. 2018, 74, 796–804. [Google Scholar] [CrossRef]
- Xiang, T.; Feng, D.; Zhang, X.; Chen, Y.; Wang, H.; Liu, X.; Gong, Z.; Yuan, J.; Liu, M.; Sha, Z.; et al. Effects of increased intracranial pressure on cerebrospinal fluid influx, cerebral vascular hemodynamic indexes, and cerebrospinal fluid lymphatic efflux. J. Cereb. Blood Flow. Metab. 2022, 42, 2287–2302. [Google Scholar] [CrossRef] [PubMed]
- Ganslandt, O.; Mourtzoukos, S.; Stadlbauer, A.; Sommer, B.; Rammensee, R. Evaluation of a novel noninvasive ICP monitoring device in patients undergoing invasive ICP monitoring: Preliminary results. J. Neurosurg. 2018, 128, 1653–1660. [Google Scholar] [CrossRef] [PubMed]
- Ackerman, K.; Mohammed, A.; Chinthala, L.; Davis, R.L.; Kamaleswaran, R.; Shafi, N.I. Features derived from blood pressure and intracranial pressure predict elevated intracranial pressure events in critically ill children. Sci. Rep. 2022, 12, 21473. [Google Scholar] [CrossRef] [PubMed]
- Dattilo, M. Noninvasive methods to monitor intracranial pressure. Curr. Opin. Neurol. 2023, 36, 1–9. [Google Scholar] [CrossRef]
- Roemer, S.N.; Friedrich, E.B.; Kettner, M.; Rauzi, M.; Schub, P.; Kulikovski, J.; Janitschke, D.; Stögbauer, J.; Lochner, P. Transorbital sonography and MRI reliability to assess optic nerve sheath diameter in idiopathic intracranial hypertension. J. Neuroimaging 2023, 33, 375–380. [Google Scholar] [CrossRef]
- Wolthers, S.A.; Engelholm, C.P.; Uslu, B.; Brandt, C.T. Noninvasive intracranial pressure monitoring in central nervous system infections. Minerva Anestesiol. 2023, 89, 206–216. [Google Scholar] [CrossRef]
- Potchen, M.; Kampondeni, S.; Birbeck, G.; Seydel, K.; Beare, N.; Glover, S.; Hammond, C.; Chilingulo, C.; Taylor, T. Noninvasive measures of brain edema predict outcome in pediatric cerebral malaria. Surg. Neurol. Int. 2018, 9, 53. [Google Scholar] [CrossRef]
- Dreier, J.P.; Lemale, C.L.; Kola, V.; Friedman, A.; Schoknecht, K. Spreading depolarization is not an epiphenomenon but the principal mechanism of the cytotoxic edema in various gray matter structures of the brain during stroke. Neuropharmacology 2018, 134, 189–207. [Google Scholar] [CrossRef] [PubMed]
- Yu, P.L. Fluid therapy of brain edema and intracranial hypertension in children. Transl. Pediatr. 2012, 1, 54–57. [Google Scholar] [PubMed]
- Leinonen, V.; Vanninen, R.; Rauramaa, T. Raised intracranial pressure and brain edema. Handb. Clin. Neurol. 2017, 145, 25–37. [Google Scholar] [PubMed]
- Shimony, N.; Martinez-Sosa, M.; Osburn, B.; Jallo, G.I. Non-traumatic pediatric intracranial hypertension: Key points for different etiologies, diagnosis, and treatment. Acta Neurol. Belg. 2021, 121, 823–836. [Google Scholar] [CrossRef] [PubMed]
- Raabe, V.N.; Shane, A.L. Group B Streptococcus (Streptococcus agalactiae). Microbiol. Spectr. 2019, 7, 10–1128. [Google Scholar] [CrossRef] [PubMed]
- Aberg, K.; Norman, M.; Pettersson, K.; Ekeus, C. Vacuum extraction in fetal macrosomia and risk of neonatal complications: A population-based cohort study. Acta Obstet. Gynecol. Scand. 2016, 95, 1089–1096. [Google Scholar] [CrossRef]
- Gardella, C.; Taylor, M.; Benedetti, T.; Hitti, J.; Critchlow, C. The effect of sequential use of vacuum and forceps for assisted vaginal delivery on neonatal and maternal outcomes. Am. J. Obstet. Gynecol. 2001, 185, 896–902. [Google Scholar] [CrossRef]
- Apperley, L.; Kumar, R.; Senniappan, S. Idiopathic intracranial hypertension in children with obesity. Acta Paediatr. 2022, 111, 1420–1426. [Google Scholar] [CrossRef]
- Ballestero, M.F.M.; Frigieri, G.; Cabella, B.C.T.; De Oliveira, S.M.; De Oliveira, R.S. Prediction of intracranial hypertension through noninvasive intracranial pressure waveform analysis in pediatric hydrocephalus. Childs Nerv. Syst. 2017, 33, 1517–1524. [Google Scholar] [CrossRef]
- Padayachy, L.C.; Padayachy, V.; Galal, U.; Gray, R.; Fieggen, A.G. The relationship between transorbital ultrasound measurement of the optic nerve sheath diameter (ONSD) and invasively measured ICP in children: Part I: Repeatability, observer variability and general analysis. Childs Nerv. Syst. 2016, 32, 1769–1778. [Google Scholar] [CrossRef]
- Steinberg, D.M.; Fine, J.; Chappell, R. Sample size for positive and negative predictive value in diagnostic research using case-control designs. Biostatistics 2009, 10, 94–105. [Google Scholar] [CrossRef] [PubMed]
- Cui, Y.; Yang, X.; Shi, Z.; Yang, Z.; Du, X.; Zhao, Z.; Cheng, X. Radiomics analysis of multiparametric MRI for prediction of pathological complete response to neoadjuvant chemoradiotherapy in locally advanced rectal cancer. Eur. Radiol. 2019, 29, 1211–1220. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Dong, D.; Li, H.; Tian, J.; Ouyang, F.; Mo, X.; Zhang, B.; Luo, X.; Lian, Z.; Pei, S.; et al. Development and validation of a magnetic resonance imaging-based model for the prediction of distant metastasis before initial treatment of nasopharyngeal carcinoma: A retrospective cohort study. EBioMedicine 2019, 40, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Devi, C.N.; Chandrasekharan, A.; Sundararaman, V.K.; Alex, Z.C. Neonatal brain MRI segmentation: A review. Comput. Biol. Med. 2015, 64, 163–178. [Google Scholar] [CrossRef] [PubMed]
- Gui, L.; Lisowski, R.; Faundez, T.; Huppi, P.S.; Lazeyras, F.; Kocher, M. Morphology-driven automatic segmentation of MR images of the neonatal brain. Med. Image Anal. 2012, 16, 1565–1579. [Google Scholar] [CrossRef]
- Makropoulos, A.; Counsell, S.J.; Rueckert, D. A review on automatic fetal and neonatal brain MRI segmentation. Neuroimage 2018, 170, 231–248. [Google Scholar] [CrossRef]




| Characteristic | ICH Group (n = 80) | Non-ICH Group (n = 37) | p Values |
|---|---|---|---|
| Sex | NA | NA | NA |
| Male, NO. (%) | 56 (70) | 23 (62) | 0.40 |
| Female, NO. (%) | 24 (30) | 14 (38) | |
| Gestational age, mean (SD), w | 39.38 ± 0.95 | 39.13 ± 1.07 | 0.20 |
| Postmenstrual age, mean (SD), w | 40.88 ± 1.24 | 40.90 ± 1.85 | 0.95 |
| Head Circumference, mean (SD), cm | 34.60 ± 1.19 | 34.43 ± 3.68 | 0.72 |
| Weight, mean (SD), kg | 3.38 ± 0.44 | 3.10 ± 0.52 | 0.00 |
| Apgar score, mean (SD) | 9.14 ± 1.85 | 8.70 ± 1.64 | 0.22 |
| Mode of Delivery | NA | NA | NA |
| Cesarean Section, NO. (%) | 28 (35) | 20 (54) | 0.51 |
| Vaginal Delivery, NO. (%) | 52 (65) | 17 (46) | |
| TICV, mL | 468.85 ± 48.21 | 444.94 ± 54.23 | 0.02 |
| GM, mL | 190.55 ± 42.55 | 163.51 ± 38.90 | 0.00 |
| WM, mL | 167.27 ± 36.59 | 172.74 ± 43.89 | 0.48 |
| CSF, mL | 71.17 ± 21.76 | 70.72 ± 19.48 | 0.92 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qin, Y.; Liu, Y.; Cao, C.; Ouyang, L.; Ding, Y.; Wang, D.; Zheng, M.; Liao, Z.; Yue, S.; Liao, W. A Novel Nomogram Based on Quantitative MRI and Clinical Features for the Prediction of Neonatal Intracranial Hypertension. Children 2023, 10, 1582. https://doi.org/10.3390/children10101582
Qin Y, Liu Y, Cao C, Ouyang L, Ding Y, Wang D, Zheng M, Liao Z, Yue S, Liao W. A Novel Nomogram Based on Quantitative MRI and Clinical Features for the Prediction of Neonatal Intracranial Hypertension. Children. 2023; 10(10):1582. https://doi.org/10.3390/children10101582
Chicago/Turabian StyleQin, Yan, Yang Liu, Chuanding Cao, Lirong Ouyang, Ying Ding, Dongcui Wang, Mengqiu Zheng, Zhengchang Liao, Shaojie Yue, and Weihua Liao. 2023. "A Novel Nomogram Based on Quantitative MRI and Clinical Features for the Prediction of Neonatal Intracranial Hypertension" Children 10, no. 10: 1582. https://doi.org/10.3390/children10101582
APA StyleQin, Y., Liu, Y., Cao, C., Ouyang, L., Ding, Y., Wang, D., Zheng, M., Liao, Z., Yue, S., & Liao, W. (2023). A Novel Nomogram Based on Quantitative MRI and Clinical Features for the Prediction of Neonatal Intracranial Hypertension. Children, 10(10), 1582. https://doi.org/10.3390/children10101582






