Different Trajectories for Diabetes Mellitus Onset and Recovery According to the Centralized Aerobic–Anaerobic Energy Balance Compensation Theory
Abstract
1. Introduction
2. Materials and Methods
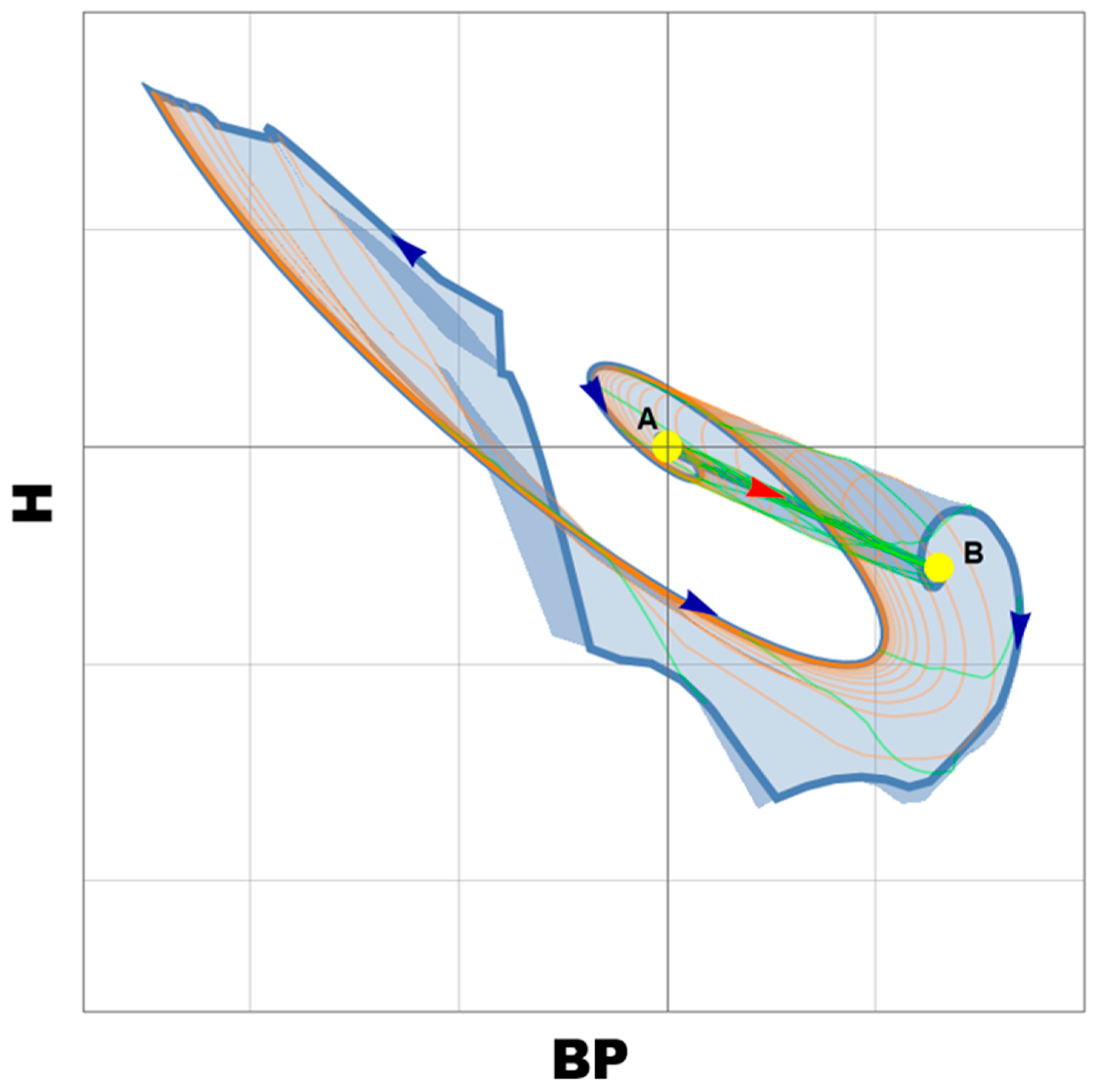
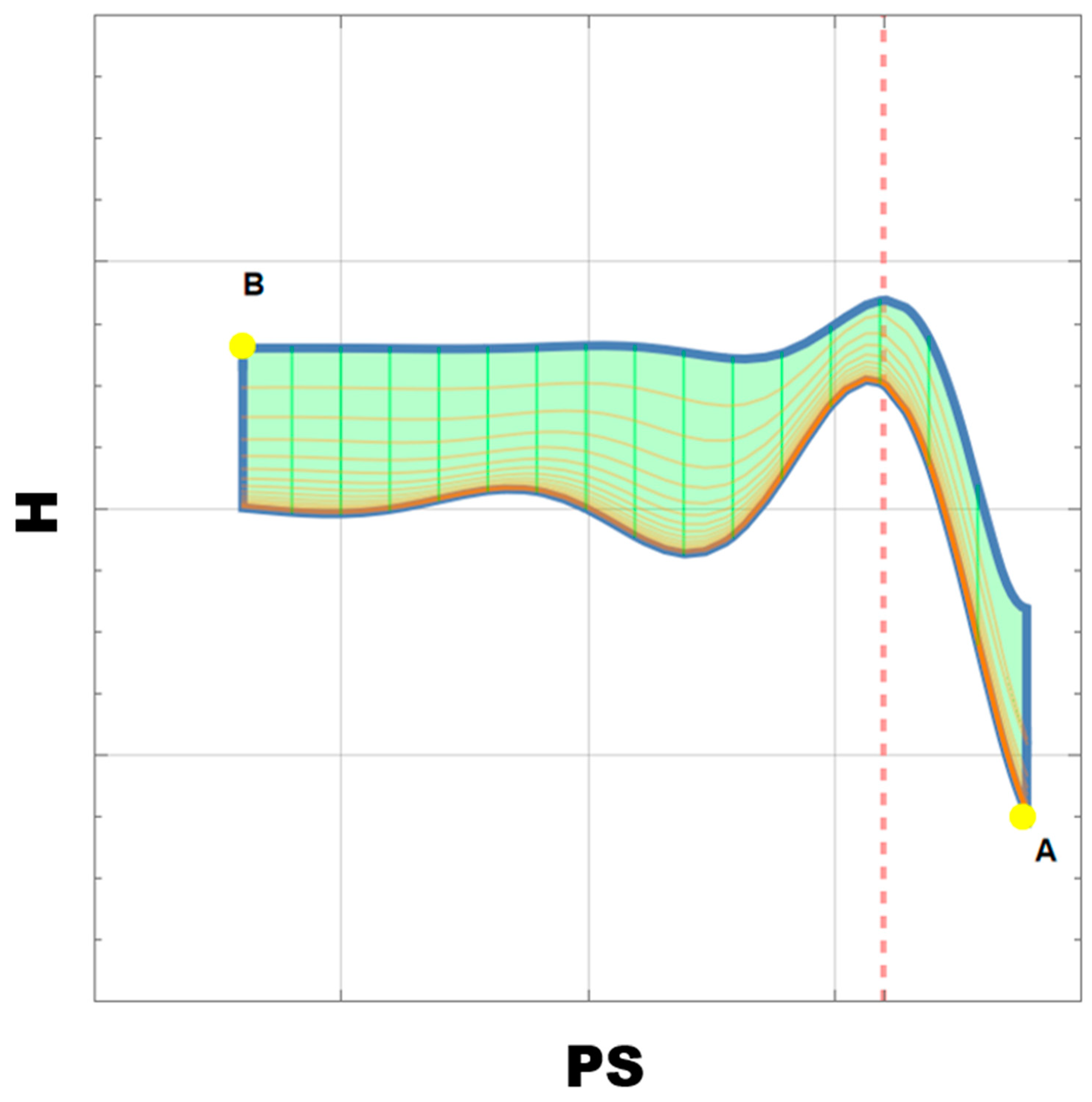
3. Modeling
Model Explanation
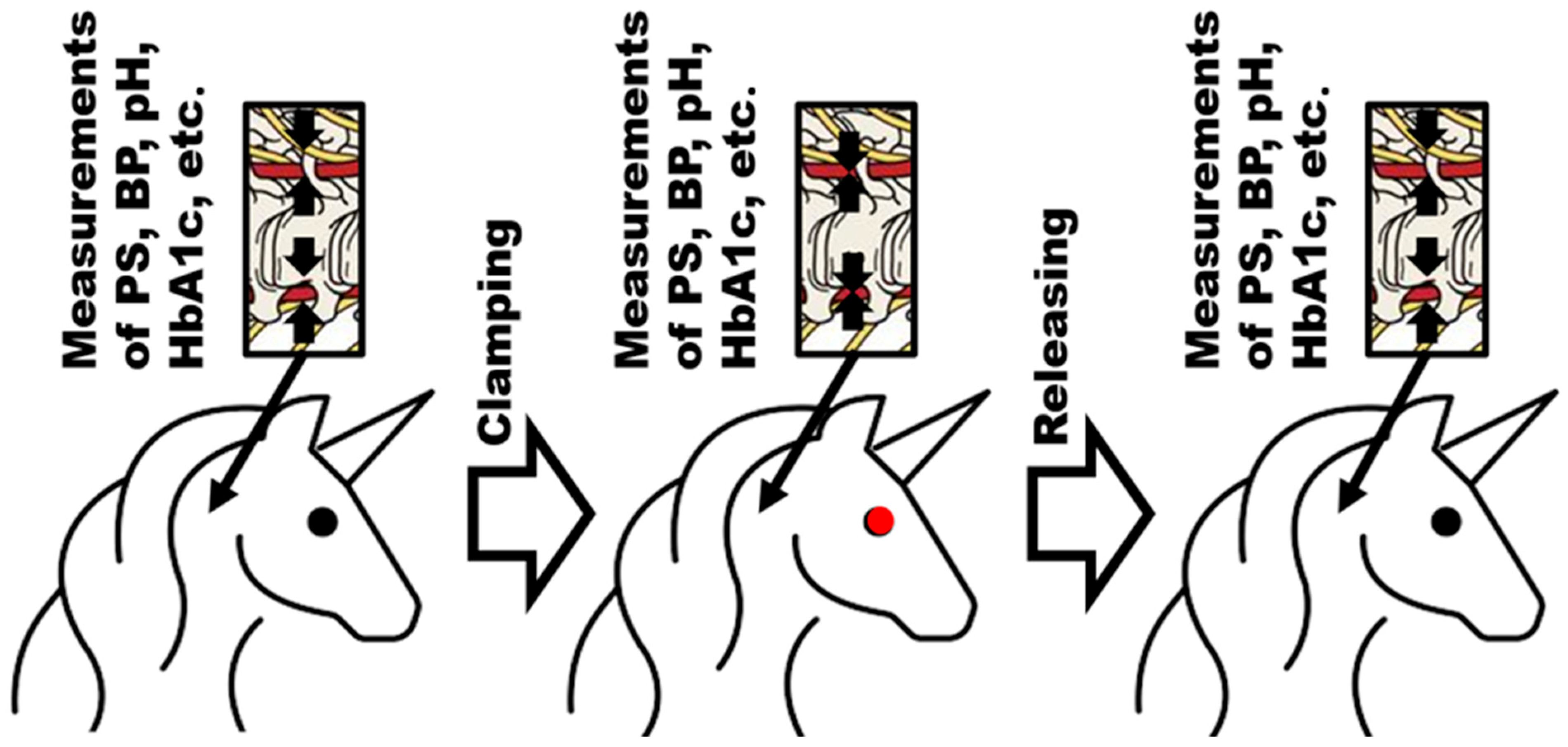
4. Appropriate Animal Model(s)
| Model Animal | Results Are Transferrable to Human Clinical Situation(s) | Lack of Reserve Arterial Way to Rhomboid Fossa | General Convenience to Measure BP | Blood Boost for Biochemical Analysis | Simplicity of Brachycephalic Arterial Blood Flow Measurement | Availability of Reported Positive Experience with the Reverse Brachycephalic Arteries Blocking |
|---|---|---|---|---|---|---|
| Mice | + | − | + | + | + | − |
| Rats | + | − | + | + | + | + |
| Rabbits | + | − | + | + | + | − |
| Minipigs | + | + | + | + | + | − |
| Goats | − | − | + | + | + | − |
| Sheep | − | − | + | + | - | − |
| Guinea pigs | − | − | + | + | + | − |
| Cats | + | + | + | + | + | − |
| Dogs | + | + | + | + | + | − |
5. Gaps in Evidence and Future Directions Instead of Conclusions
- The onset and recovery itineraries from pre-DM are different;
- The slope of the HbA1c dependence on PS demonstrates two different areas. Each of them should have different health condition situations, which should be verified on animal models. These preliminary conclusions should be preceded by the optimization of the list of parameters to obtain a further description of OABFRH’s influence on DM. The collected data could be used in the evaluation of the set of proper parameters for the aging index(es). This became critically important in 2022, when WHO (in ICD-11) eventually started to consider aging as a health condition and not as a normal stage of development [75]; therefore, AHT and DM, which were considered aging satellites, could experience a change in mankind’s attitude toward them.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bower, J.K.; Appel, L.J.; Matsushita, K.; Young, J.H.; Alonso, A.; Brancati, F.L.; Selvin, E. Glycated Hemoglobin and Risk of Hypertension in the Atherosclerosis Risk in Communities Study. Diabetes Care 2012, 35, 1031–1037. [Google Scholar] [CrossRef] [PubMed]
- Selvin, E.; Steffes, M.W.; Zhu, H.; Matsushita, K.; Wagenknecht, L.; Pankow, J.; Coresh, J.; Brancati, F.L. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N. Engl. J. Med. 2010, 362, 800–811. [Google Scholar] [CrossRef] [PubMed]
- Adams, R.J.; Appleton, S.L.; Hill, C.L.; Wilson, D.H.; Taylor, A.W.; Chittleborough, C.R.; Gill, T.K.; Ruffin, R.E. Independent association of HbA(1c) and incident cardiovascular disease in people without diabetes. Obes. (Silver Spring) 2009, 17, 559–563. [Google Scholar]
- Song, J.; Wei, N.; Zhao, Y.; Jiang, Y.; Wu, X.; Gao, H. Elevated glycosylated hemoglobin levels and their interactive effects on hypertension risk in nondiabetic Chinese population: A cross-sectional survey. BMC Cardiovasc. Disord. 2020, 20, 218. [Google Scholar] [CrossRef]
- Cosentino, F.; Grant, P.J.; Aboyans, V.; Bailey, C.J.; Ceriello, A.; Delgado, V.; Federici, M.; Filippatos, G.; Grobbee, D.E.; Hansen, T.B.; et al. ESC Scientific Document Group. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020, 41, 255–323. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Perrone, V.; Veronesi, C.; Gambera, M.; Nati, G.; Perone, F.; Tagliabue, P.F.; Degli Esposti, L.; Volpe, M. Treatment with Free Triple Combination Therapy of Atorvastatin, Perindopril, Amlodipine in Hypertensive Patients: A Real-World Population Study in Italy. High Blood Press. Cardiovasc. Prev. 2019, 26, 399–404. [Google Scholar] [CrossRef]
- Mancia, G.; Kreutz, R.; Brunström, M.; Burnier, M.; Grassi, G.; Januszewicz, A.; Muiesan, M.L.; Tsioufis, K.; Agabiti-Rosei, E.; Algharably, E.A.E.; et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension Endorsed by the European Renal Association (ERA) and the International Society of Hypertension (ISH). J Hypertens. 2023. Online ahead of print. [Google Scholar] [CrossRef]
- Mancia, G. The association of hypertension and diabetes: Prevalence, cardiovascular risk and protection by blood pressure reduction. Acta Diabetol. 2005, 42, 17–25. [Google Scholar] [CrossRef]
- Petrie, J.; Guzik, T.J.; Touyz, R.M. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Can. J. Cardiol. 2017, 34, 575–584. [Google Scholar] [CrossRef]
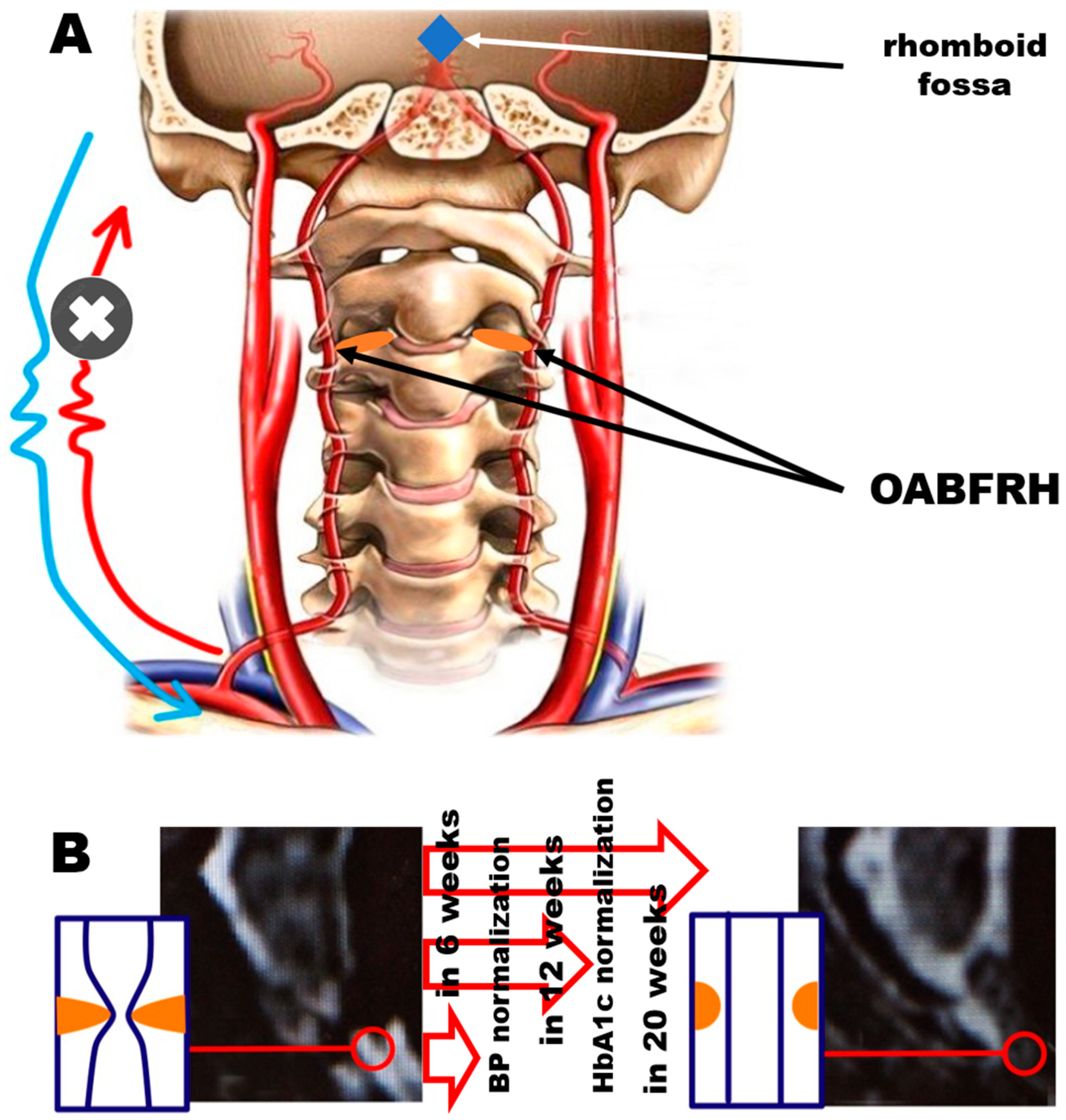
- Vetcher, A.A.; Zhukov, K.V.; Gasparyan, B.A.; Shishonin, A.Y. Hypothetical reason for the restoration of HbA1c level for pre-diabetic patients through the restoration of arterial blood flow access to rhomboid fossa. Diabetology 2022, 3, 470–476. [Google Scholar] [CrossRef]
- Zhukov, K.V.; Gasparuan, B.A.; Vetcher, A.A.; Shishonin, A.Y. Centralized aerobic-anaerobic energy balance compensation theory perspective in biomedicine. Arch. Biotechnol. Biomed. 2022, 6, 7–9. [Google Scholar] [CrossRef]
- King, H. The Holistic Hippocrates: Treating the Patient, Not Just the Disease. In Hippocrates Now: The ‘Father of Medicine’ in the Internet Age; Bloomsbury Academic: London, UK, 2020; pp. 133–154. [Google Scholar] [CrossRef]
- Correll, J. Descartes’ Dualism and Its Influence on Our Medical System. SUURJ Seattle Univ. Undergrad. Res. J. 2022, 6, 47–55. [Google Scholar]
- Alex, S. Rene Descartes: Colossus of binaries—Real or perceived? Arch. Med. Health Sci. 2017, 5, 126–128. [Google Scholar] [CrossRef]
- Billman, G.E. Homeostasis: The Underappreciated and Far Too Often Ignored Central Organizing Principle of Physiology. Front. Physiol. 2020, 11, 200–2011. [Google Scholar] [CrossRef]
- Vetcher, A.A.; Zhukov, K.V.; Gasparuan, B.A.; Shishonin, A.Y. Time to take the Thermodynamics of Irreversible processes into consideration to describe in vivo biodegradation. Res. Dev. Polym. Sci. 2022, 1, 1004–1006. [Google Scholar] [CrossRef]
- Vetcher, A.A.; Zhukov, K.V.; Gasparuan, B.A.; Shishonin, A.Y. The cerebellum role in arterial hypertension. Med. Hypotheses 2022, 162, 10835. [Google Scholar] [CrossRef]
- Vetcher, A.A.; Zhukov, K.V.; Gasparuan, B.A.; Shishonin, A.Y. The Role of Cervical Vertebral Arteries Blood Flow in Centralized Aerobic- Anaerobic Energy Balance Compensation: When Hypothesis Becomes a Theory. Antioxid. Cardiovasc. Dis. 2021, 5, 1027–1032. [Google Scholar]
- Braukmann, S. The Organism and the Open System: Ervin Bauer and Ludwig von Bertalanffy. Ann. New York Acad. Sci. 2006, 901, 291–300. [Google Scholar]
- Elek, G.; Muller, M. The living matter according to Ervin Bauer (1890–1938), (on the 75th anniversary of his tragic death). Acta Physiol. Hung. 2013, 100, 124–132. [Google Scholar] [CrossRef]
- Gumenyuk, V.I.; Dobroborsky, B.S.; Fedosovsky, M.E. Determination of the effectiveness of training of personnel of energy facilities by quantitatively accounting for the human factor. Glob. Energy 2012, 154, 308–312. (In Russian) [Google Scholar]
- Curtelin, D.; Morales-Alamo, D.; de Torres-Peralta, R.S.; Rasmussen, P.; Martin-Rincon, M.; Perez-Valera, M.; Siebenmann, C.; Perez-Suarez, I.; Cherouveim, E.; Sheel, A.W.; et al. Cerebral blood flow, frontal lobe oxygenation and intra-arterial blood pressure during sprint exercise in normoxia and severe acute hypoxia in humans. J. Cereb. Blood Flow Metab. 2018, 38, 136–150. [Google Scholar] [CrossRef] [PubMed]
- He, Z.B.; Lv, Y.-K.; Li, H.; Yao, Q.; Wang, K.; Song, X.; Wu, Z.; Qin, X. Atlantoaxial Misalignment Causes High Blood Pressure in Rats: A Novel AHT Model. BioMed Res. Int. 2017, 2017, 5986957. [Google Scholar] [PubMed]
- Zhukov, K.V.; Gasparyan, B.A.; Vetcher, A.A.; Shishonin, A.Y. Left ventricular hypertrophy linked with arterial hypertension through centralized aerobic-anaerobic energy balance compensation theory. Ann. Clin. Hypertens. 2022, 6, 012–014. [Google Scholar] [CrossRef]
- Vetcher, A.A.; Zhukov, K.V.; Gasparyan, B.A.; Shishonin, A.Y. How the theory of centralized aerobic-anaerobic energy balance compensation explains sudden cardiac death in young athletes. Eur. J. Intern. Med. 2022, 107, 118–119. [Google Scholar] [CrossRef]
- Zhukov, K.V.; Vetcher, A.A.; Gasparuan, B.A.; Shishonin, A.Y. Alteration of Relative Rates of Biodegradation and Regeneration of Cervical Spine Cartilage through the Restoration of Arterial Blood Flow Access to Rhomboid Fossa: A Hypothesis. Polymers 2021, 13, 4248. [Google Scholar] [CrossRef]
- Zhukov, K.V.; Gasparyan, B.A.; Vetcher, A.A.; Shishonin, A.Y. The theory of centralized aerobic-anaerobic energy balance compensation and the right posture. Open J. Orthop. Rheumatol. 2022, 7, 011–012. [Google Scholar] [CrossRef]
- Bulatov, E.; Khaiboullina, S.; dos Reis, H.J.; Palotás, A.; Venkataraman, K.; Vijayalakshmi, M.; Rizvanov, A. Ubiquitin-Proteasome System: Promising Therapeutic Targets in Autoimmune and Neurodegenerative Diseases. Bionanoscience 2016, 6, 341–344. [Google Scholar] [CrossRef]
- Banwarth-Kuhn, M.; Sindi, S. How and why to build a mathematical model: A case study using prion aggregation. J. Biol. Chem. 2020, 295, 5022–5035. [Google Scholar] [CrossRef]
- Porgo, T.V.; Norris, S.L.; Salanti, G.; Johnson, L.F.; Simpson, J.A.; Low, N.; Egger, M.; Althaus, C.L. The use of mathematical modeling studies for evidence synthesis and guideline development: A glossary. Res. Synth. Methods 2019, 10, 125–133. [Google Scholar] [CrossRef]
- Menshikov, Y. Criteria for Adequacy Estimation of Mathematical Descriptions of Physical Processes. In Computational Models in Engineering; Volkov, K., Ed.; IntechOpen: London, UK, 2019; pp. 1–19. [Google Scholar] [CrossRef]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2010, 33 (Suppl. 1), S62–S69. [Google Scholar] [CrossRef] [PubMed]
- WHO. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia; Report of a WHO/IDF Consultation; WHO Document Production Services: Geneva, Switzerland, 2006; p. 50. [Google Scholar]
- American Diabetes Association. Standards of medical care in diabetes-2015 abridged for primary care providers. Clin. Diabetes 2015, 33, 97–111. [Google Scholar] [CrossRef] [PubMed]
- Genc, S.; Gurdol, F.; Kanmaz-Ozer, M.; Ince, N.; Ozcelik, F.; Omer, B. The Analytical Performances of Four Different Glycated Hemoglobin Methods. Med. Chem. 2014, 4, 501–505. [Google Scholar] [CrossRef]
- Kobalava, Z.D.; Konradi, A.O.; Nedogoda, S.V.; Shlyakhto, E.V. Arterial hypertension in adults. Clinical guidelines 2020. Russ. J. Cardiol. 2020, 25, 149–218. [Google Scholar]
- Schoning, M.; Walter, J.; Scheel, P. Estimation of cerebral blood flow through color duplex sonography of the carotid and vertebral arteries in healthy adults. Stroke 1994, 25, 17–22. [Google Scholar] [CrossRef]
- Kholin, A.M.; Muminova, K.T.; Balashov, I.S.; Khodzhaeva, Z.S.; Borovikov, P.I.; Ivanets, T.Y.; Gus, A.I. First-trimester prediction of preeclampsia: Validation of screening algorithms in a Russian population. Akusherstvo I Ginekol. Obstet. Gynecol. 2017, 8, 74–84. (In Russian) [Google Scholar] [CrossRef]
- Vetcher, A.A.; Zhukov, K.V.; Gasparuan, B.A.; Shishonin, A.Y. The cervical blood flow parameters with the best correlation from arterial blood pressure in hypertension cases. Int. J. Recent Sci. Res. 2021, 9, 42957–42958. [Google Scholar] [CrossRef]
- Baselli, G.; Fasani, F.; Pelizzari, L.; Cazzoli, M.; Baglio, F.; Laganà, M.M. Real-Time Phase-Contrast MRI to Monitor Cervical Blood and Cerebrospinal Fluid Flow Beat-by-Beat Variability. Biosensors 2022, 12, 417. [Google Scholar] [CrossRef]
- Du, Y.; Ding, H.; He, L.; Yiu, B.Y.S.; Deng, L.; Yu, A.C.H.; Zhu, L. Quantitative Blood Flow Measurements in the Common Carotid Artery: A Comparative Study of High-Frame-Rate Ultrasound Vector Flow Imaging, Pulsed Wave Doppler, and Phase Contrast Magnetic Resonance Imaging. Diagnostics 2022, 12, 690. [Google Scholar] [CrossRef]
- Gewirtz, H.; Dilsizian, V. Integration of quantitative positron emission tomography absolute myocardial blood flow measurements in the clinical management of coronary artery disease. Circulation 2016, 133, 2180–2196. [Google Scholar]
- Li, D.; Liu, Y.; Zeng, X.; Xiong, Z.; Yao, Y.; Liang, D.; Qu, H.; Xiang, H.; Yang, Z.; Nie, L.; et al. Quantitative study of the changes in cerebral blood flow and iron deposition during progression of Alzheimer’s disease. J. Alzheimer’s Dis. 2020, 78, 439–452. [Google Scholar] [CrossRef] [PubMed]
- Munk, J.K.; Lind, B.S.; Jørgensen, H.L. Change in HbA1c concentration as decision parameter for frequency of HbA1c measurement. Scand. J. Clin. Lab. Investig. 2019, 79, 320–324. [Google Scholar] [CrossRef] [PubMed]
- Higgins, T.N.; Tran, D.; Cembrowski, G.S.; Shalapay, C.; Steele, P.; Wiley, C. Is HbA1c a good screening test for diabetes mellitus? Clin. Biochem. 2011, 44, 1469–1472. [Google Scholar] [CrossRef] [PubMed]
- Karnchanasorn, R.; Huang, J.; Ou, H.-Y.; Feng, W.; Chuang, L.-M.; Ken, C.; Chiu, K.C.; Samoa, R. Comparison of the Current Diagnostic Criterion of HbA1c with Fasting and 2-Hour Plasma Glucose Concentration. J. Diabetes Res. 2016, 2016, 6195494. [Google Scholar] [CrossRef]
- Resende, E.A.M.R.; Silva, V.J.D.; Correia, D. Comparison of pulse wave analysis parameters by oscillometry in hypertensive diabetic and nondiabetic patients in a Brazilian outpatient care. Medicine 2019, 98, e18100. [Google Scholar] [CrossRef]
- Tąpolska, M.; Spałek, M.; Szybowicz, U.; Domin, R.; Owsik, K.; Sochacka, K.; Skrypnik, D.; Bogdański, P.; Owecki, M. Arterial Stiffness Parameters Correlate with Estimated Cardiovascular Risk in Humans: A Clinical Study. Int. J. Environ. Res. Public Health 2019, 16, 2547. [Google Scholar] [CrossRef]
- Murkamilov, I.T.; Aitbaev, K.A.; Fomin, V.V.; Murkamilova, Z.A.; Redzhapova, N.A.; Yusupov, F.A. Clinical and functional characteristics of arterial stiffness in elderly. Syst. Hypertens. 2021, 18, 31–36. [Google Scholar] [CrossRef]
- Iltis, H. Gregor Mendel and His Work. Sci. Mon. 1943, 56, 414–423. [Google Scholar]
- Nogler, G.A. The lesser-known Mendel: His experiments on Hieracium. Genetics 2006, 172, 1–6. [Google Scholar] [CrossRef]
- Phillips, K.A.; Bales, K.L.; Capitanio, J.P.; Conley, A.; Czoty, P.W.; ‘t Hart, B.A.; Hopkins, W.D.; Hu, S.-L.; Miller, L.A.; Nader, M.A.; et al. Why primate models matter. Am. J. Primatol. 2014, 76, 801–827. [Google Scholar] [CrossRef]
- Aguilera, B.; Perez Gomez, J.; DeGrazia, D. Should biomedical research with great apes be restricted? A systematic review of reasons. BMC Med. Ethics 2021, 22, 15. [Google Scholar] [CrossRef]
- Casals, J.B.; Pieri, N.C.G.; Feitosa, M.L.T.; Ercolin, A.C.M.; Roballo, K.C.S.; Barreto, R.S.N.; Bressan, F.F.; Martins, D.S.; Miglino, M.A.; Ambrósio, C.E. The use of animal models for stroke research: A review. Comp. Med. 2011, 61, 305–313. [Google Scholar]
- Jia, T.; Wang, C.; Han, Z.; Wang, X.; Ding, M.; Wang, Q. Experimental Rodent Models of Cardiovascular Diseases. Front. Cardiovasc. Med. 2020, 7, 588075. [Google Scholar] [CrossRef] [PubMed]
- Zaragoza, C.; Gomez-Guerrero, C.; Martin-Ventura, J.L.; Blanco-Colio, L.; Lavin, B.; Mallavia, B.; Tarin, C.; Mas, S.; Ortiz, A.; Egido, J. Animal Models of Cardiovascular Diseases. J. Biomed. Biotechnol. 2011, 2011, 497841. [Google Scholar] [CrossRef] [PubMed]
- Leong, X.F.; Ng, C.Y.; Jaarin, K. Animal Models in Cardiovascular Research: Hypertension and Atherosclerosis. BioMed Res. Int. 2015, 2015, 528757. [Google Scholar] [CrossRef]
- Mazensky, D.; Flesarova, S.; Sulla, I. Arterial Blood Supply to the SpinalCord in Animal Models of Spinal CordInjury: A Review. Anat. Rec. 2017, 300, 2091–2106. [Google Scholar] [CrossRef]
- Li, Y.; Zhang, J. Animal models of stroke. Anim. Model. Exp. Med. 2021, 4, 204–219. [Google Scholar] [CrossRef] [PubMed]
- Simon, F.; Oberhuber, A. Ischemia and reperfusion injury ofthe spinal cord: Experimental strategies to examine postischemicparaplegia. Neural Regen. Res. 2016, 11, 414–415. [Google Scholar] [CrossRef]
- Melissano, G.; Civilini, E.; Bertoglio, L.; Calliari, F.; Campos, M.; Amato, A.; Chiesa, R. Angio-CT imaging of the spinal cordvascularisation: A pictorial essay. Eur. J. Vasc. Endovasc. Surg. 2010, 39, 436–440. [Google Scholar] [CrossRef]
- Ramer, L.M.; Ramer, M.S.; Bradbury, E.J. Restoring function afterspinal cord injury: Towards clinical translation of experimental strategies. Lancet Neurol. 2014, 13, 1241–1256. [Google Scholar] [CrossRef]
- Courtine, G.; Bunge, M.B.; Fawcett, J.W.; Grossman, R.G.; Kaas, J.H.; Lemon, R.; Maier, I.; Martin, J.; Nudo, R.J.; Ramon-Cueto, A.; et al. Can experiments in nonhuman primates expedite the translation of treatments for spinal cord injury in humans? Nat. Med. 2007, 13, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Geissler, S.A.; Schmidt, C.E.; Schallert, T. Rodent models and behavioral outcomes of cervical spinal cord injury. J. Spine 2013, S4, 001. [Google Scholar] [CrossRef] [PubMed]
- Simon, F.; Erhart, P.; Vcelar, B.; Scheuerle, A.; Schelzig, H.; Oberhuber, A. Erythropoietin preconditioning improves clinical and histo-logic outcome in an acute spinal cord ischemia and reperfusionrabbit model. J. Vasc. Surg. 2015, 64, 1797–1804. [Google Scholar] [CrossRef]
- Uezu, T.; Koja, K.; Kuniyoshi, Y.; Miyagi, K.; Shimoji, M.; Arakaki, K.; Yamashiro, S.; Mabuni, K.; Senaha, S. Blood distribution tothe anterior spinal artery from each segment of intercostal andlumbar arteries. J. Cardiovasc. Surg. 2003, 44, 637–645. [Google Scholar]
- Singh, V.K.; Thrall, K.D.; Hauer-Jensen, M. Minipigs as models in drug discovery. Expert Opin. Drug Discov. 2016, 11, 1131–1134. [Google Scholar] [CrossRef]
- Maršala, M. Spinal cord blood flow and metabolism in transient spinal ischemia. In Spinal Cord Monitoring; Stålberg, E., Sharma, H.S., Olsson, Y., Eds.; Springer: New York, NY, USA, 1998; pp. 5–25. [Google Scholar]
- Pais, D.; Casal, D.; Arantes, M.; Casimiro, M.; O’Neill, J.G. 2007. Spinal cord arteries in Canis familiaris and their variations: Implications in experimental procedures. Braz. J. Morphol. Sci. 2007, 24, 224–228. [Google Scholar]
- De Girolami, U.; Zivin, J.A. Neuropathology of experimental spinal cord ischemia in the rabbit. J. Neuropathol. Exp. Neurol. 1982, 41, 129–149. [Google Scholar] [CrossRef]
- National Research Council (US) Committee on Scientific and Humane Issues in the Use of Random Source Dogs and Cats in Research. Scientific and Humane Issues in the Use of Random Source Dogs and Cats in Research; Use of Dogs and Cats in Research: Public Perception and Evolution of Laws and Guidelines; National Academies Press (US): Washington, DC, USA, 2009; pp. 1–9. [Google Scholar]
- Scremin, O.U. The spinal cord blood vessels. In The Spinal Cord: A Christopher and Dana Reeve Foundation Text and Atlas; Watson, C., Paxinos, C., Kayalioglu, G., Eds.; Elsevier: San Diego, CA, USA, 2009; pp. 57–63. [Google Scholar]
- Amato, A.C.M.; Stolf, N.A.G. Anatomy of spinal blood supply. J. Vasc. Bras. 2015, 14, 248–252. [Google Scholar] [CrossRef]
- Available online: https://icd.who.int (accessed on 27 July 2023).
| Parameter | M | F | M + F | Normal |
|---|---|---|---|---|
| Sample size | 19 | 29 | 48 | |
| Age, years | 63.1 ± 11.7 | 65.5 ± 12.2 | 64.3 ± 12.0 | |
| BP before treatment, torr | 159.5 ± 18.3 | 163.5 ± 17.9 | 161.9 ± 18.1 | |
| BP after treatment, torr | 132.3 ± 19.2 | 131.7 ± 16.6 | 132.9 ± 17.3 | <140 [37] |
| PS before treatment, cm/s | 22.5 ± 8.1 | 21.9 ± 9.3 | 22.2 ± 7.5 | |
| PS after treatment, cm/s | 41.7 ± 6.7 | 43.2 ± 7.4 | 42.5 ± 7.8 | 48 ± 10 [38] |
| H before treatment, % | 6.03 ± 0.34 | 6.11 ± 0.45 | 6.08 ± 0.41 | |
| H after treatment, % | 5.7 ± 0.63 | 5.73 ± 0.51 | 5.72 ± 0.58 | 5.7–6.4 [35] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vetcher, A.A.; Zhukov, K.V.; Gasparyan, B.A.; Borovikov, P.I.; Karamian, A.S.; Rejepov, D.T.; Kuznetsova, M.N.; Shishonin, A.Y. Different Trajectories for Diabetes Mellitus Onset and Recovery According to the Centralized Aerobic–Anaerobic Energy Balance Compensation Theory. Biomedicines 2023, 11, 2147. https://doi.org/10.3390/biomedicines11082147
Vetcher AA, Zhukov KV, Gasparyan BA, Borovikov PI, Karamian AS, Rejepov DT, Kuznetsova MN, Shishonin AY. Different Trajectories for Diabetes Mellitus Onset and Recovery According to the Centralized Aerobic–Anaerobic Energy Balance Compensation Theory. Biomedicines. 2023; 11(8):2147. https://doi.org/10.3390/biomedicines11082147
Chicago/Turabian StyleVetcher, Alexandre A., Kirill V. Zhukov, Bagrat A. Gasparyan, Pavel I. Borovikov, Arfenia S. Karamian, Dovlet T. Rejepov, Maria N. Kuznetsova, and Alexander Y. Shishonin. 2023. "Different Trajectories for Diabetes Mellitus Onset and Recovery According to the Centralized Aerobic–Anaerobic Energy Balance Compensation Theory" Biomedicines 11, no. 8: 2147. https://doi.org/10.3390/biomedicines11082147
APA StyleVetcher, A. A., Zhukov, K. V., Gasparyan, B. A., Borovikov, P. I., Karamian, A. S., Rejepov, D. T., Kuznetsova, M. N., & Shishonin, A. Y. (2023). Different Trajectories for Diabetes Mellitus Onset and Recovery According to the Centralized Aerobic–Anaerobic Energy Balance Compensation Theory. Biomedicines, 11(8), 2147. https://doi.org/10.3390/biomedicines11082147









