Biomarkers in Anal Cancer: Current Status in Diagnosis, Disease Progression and Therapeutic Strategies
Abstract
:1. Introduction
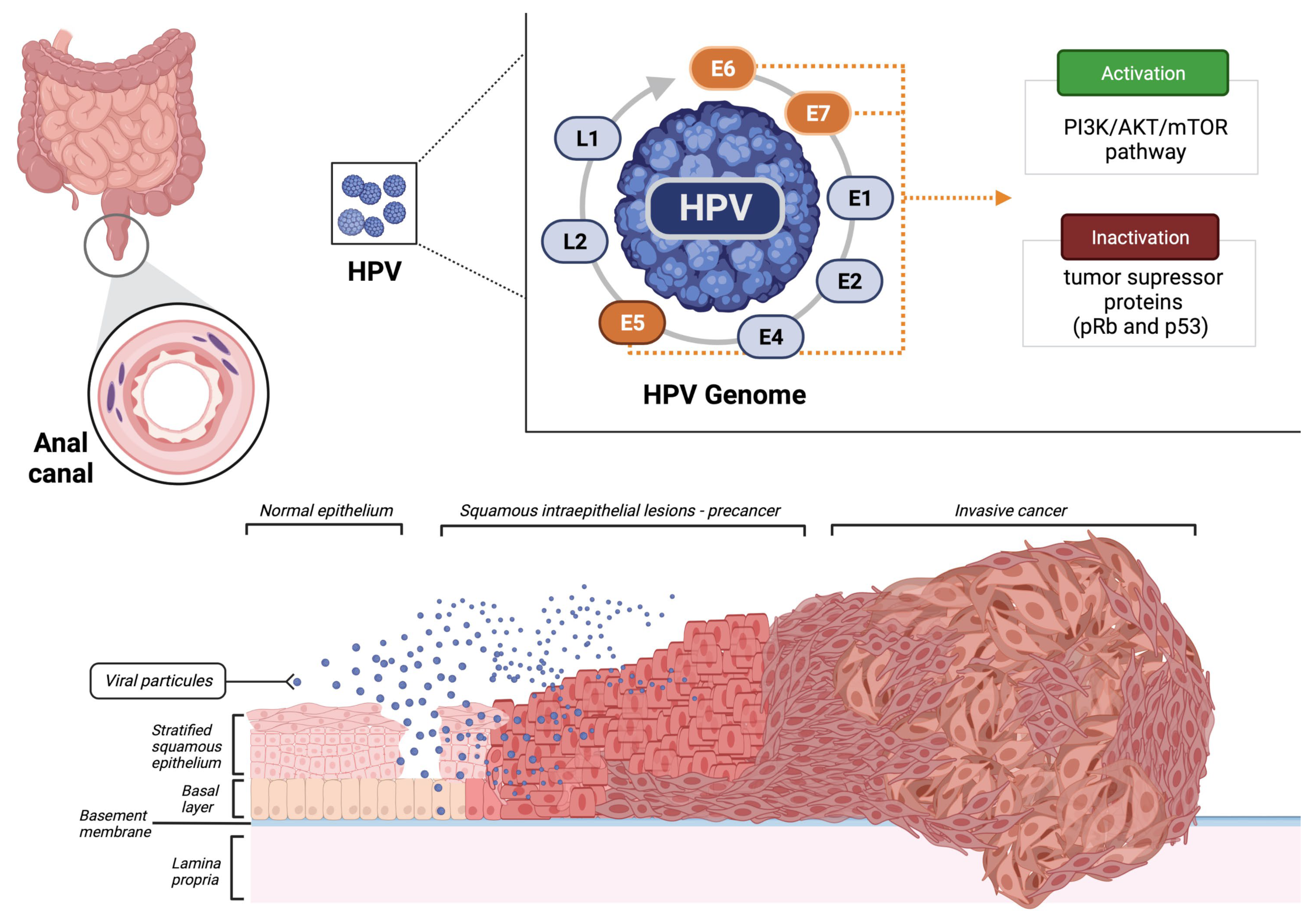
2. Standard of Care of SCCA
3. Molecular Characterization of SCCA
4. Biomarkers
4.1. HPV
4.2. Circulating Tumor DNA (ctDNA)
4.3. HIV
4.4. Ki-67
4.5. PD-L1
4.6. Tumor-Infiltrating Lymphocytes (TILs)
4.7. RAS/BRAF
4.8. Tumor Mutational Burden (TMB)
4.9. Microsatellite Instability
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Eng, C.; Ciombor, K.K.; Cho, M.; Dorth, J.A.; Rajdev, L.N.; Horowitz, D.P.; Gollub, M.J.; Jácome, A.A.; Lockney, N.A.; Muldoon, R.L.; et al. Anal Cancer: Emerging Standards in a Rare Rare Disease. J. Clin. Oncol. 2022, 2102566. [Google Scholar] [CrossRef] [PubMed]
- Hoff, P.M.; Coudry, R.; Moniz, C.M.V. Pathology of Anal Cancer. Surg. Oncol. Clin. N. Am. 2017, 26, 57–71. [Google Scholar] [CrossRef] [PubMed]
- Han, K.; Cummings, B.J.; Lindsay, P.; Skliarenko, J.; Craig, T.; Le, L.W.; Brierley, J.; Wong, R.; Dinniwell, R.; Bayley, A.J.; et al. Prospective evaluation of acute toxicity and quality of life after IMRT and concurrent chemotherapy for anal canal and perianal cancer. Int. J. Radiat. Oncol. Biol. Phys. 2014, 90, 587–594. [Google Scholar] [CrossRef] [PubMed]
- National Comprehensive Cancer Network. Physician Guidelines: Anal Cancer. 2022. Available online: https://www.nccn.org/professionals/physician_gls/pdf/anal.pdf (accessed on 7 July 2022).
- Deshmukh, A.A.; Suk, R.; Shiels, M.S.; Sonawane, K.; Nyitray, A.G.; Liu, Y.; Gaisa, M.M.; Palefsky, J.M.; Sigel, K. Recent Trends in Squamous Cell Carcinoma of the Anus Incidence and Mortality in the United States, 2001–2015. J. Natl. Cancer Inst. 2020, 112, 829–838. [Google Scholar] [CrossRef]
- Shiels, M.S.; Kreimer, A.R.; Coghill, A.E.; Darragh, T.M.; Devesa, S.S. Anal Cancer Incidence in the United States, 1977–2011: Distinct Patterns by Histology and Behavior. Cancer Epidemiol. Biomark. Prev. 2015, 24, 1548–1556. [Google Scholar] [CrossRef] [Green Version]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics, 2021. CA A Cancer J. Clin. 2021, 71, 7–33. [Google Scholar] [CrossRef]
- American Joint Committee on Cancer. AJCC Cancer Staging Manual, 8th ed.; Springer Cham: New York, NY, USA, 2017; pp. 715–725. Available online: https://link.springer.com/book/9783319406176 (accessed on 27 June 2022).
- Daling, J.R.; Weiss, N.S.; Hislop, T.G.; Maden, C.; Coates, R.J.; Sherman, K.J.; Ashley, R.L.; Beagrie, M.; Ryan, J.A.; Corey, L. Sexual practices, sexually transmitted diseases, and the incidence of anal cancer. N. Engl. J. Med. 1987, 317, 973–977. [Google Scholar] [CrossRef]
- Zhang, L.; Wu, J.; Ling, M.T.; Zhao, L.; Zhao, K.N. The role of the PI3K/Akt/mTOR signalling pathway in human cancers induced by infection with human papillomaviruses. Mol. Cancer 2015, 14, 87. [Google Scholar] [CrossRef] [Green Version]
- Bernard-Tessier, A.; Jeannot, E.; Guenat, D.; Debernardi, A.; Michel, M.; Proudhon, C.; Vincent-Salomon, A.; Bièche, I.; Pierga, J.-Y.; Buecher, B.; et al. Clinical Validity of HPV Circulating Tumor DNA in Advanced Anal Carcinoma: An Ancillary Study to the Epitopes-HPV02 Trial. Clin. Cancer Res. 2019, 25, 2109–2115. [Google Scholar] [CrossRef]
- Crum-Cianflone, N.F.; Hullsiek, K.H.; Marconi, V.; Ganesan, A.; Weintrob, A.; Barthel, R.V.; Agan, B. Anal cancers among HIV-infected persons: HAART is not slowing rising incidence. AIDS 2010, 24, 535–543. [Google Scholar] [CrossRef] [Green Version]
- Gunderson, L.L.; Winter, K.A.; Ajani, J.A.; Pedersen, J.E.; Moughan, J.; Benson, A.B.; Thomas, C.R., Jr.; Mayer, R.J.; Haddock, M.G.; Rich, T.A.; et al. Long-term update of US GI intergroup RTOG 98-11 phase III trial for anal carcinoma: Survival, relapse, and colostomy failure with concurrent chemoradiation involving fluorouracil/mitomycin versus fluorouracil/cisplatin. J. Clin. Oncol. 2012, 30, 4344–4351. [Google Scholar] [CrossRef] [PubMed]
- Nigro, N.D.; Vaitkevicius, V.K.; Considine, B. Combined therapy for cancer of the anal canal: A preliminary report. Dis. Colon. Rectum 1974, 17, 354–356. [Google Scholar] [CrossRef] [PubMed]
- Glynne-Jones, R.; Sebag-Montefiore, D.; Meadows, H.M.; Cunningham, D.; Begum, R.; Adab, F.; Benstead, K.; Harte, R.J.; Stewart, J.; Beare, S.; et al. Best time to assess complete clinical response after chemoradiotherapy in squamous cell carcinoma of the anus (ACT II): A post-hoc analysis of randomised controlled phase 3 trial. Lancet Oncol. 2017, 18, 347–356. [Google Scholar] [CrossRef] [Green Version]
- James, R.D.; Glynne-Jones, R.; Meadows, H.M.; Cunningham, D.; Myint, A.S.; Saunders, M.P.; Maughan, T.; McDonald, A.; Essapen, S.; Leslie, M.; et al. Mitomycin or cisplatin chemoradiation with or without maintenance chemotherapy for treatment of squamous-cell carcinoma of the anus (ACT II): A randomised, phase 3, open-label, 2 × 2 factorial trial. Lancet Oncol. 2013, 14, 516–524. [Google Scholar] [CrossRef]
- Ajani, J.A.; Winter, K.A.; Gunderson, L.L.; Pedersen, J.; Benson, A.B.; Thomas, C.R.; Mayer, R.J.; Haddock, M.G.; Rich, T.A.; Willett, C. Fluorouracil, Mitomycin, and Radiotherapy vs Fluorouracil, Cisplatin, and Radiotherapy for Carcinoma of the Anal Canal: A Randomized Controlled Trial. JAMA 2008, 299, 1914–1921. [Google Scholar] [CrossRef]
- Peiffert, D.; Tournier-Rangeard, L.; Gérard, J.-P.; Lemanski, C.; François, E.; Giovannini, M.; Cvitkovic, F.; Mirabel, X.; Bouché, O.; Luporsi, E.; et al. Induction chemotherapy and dose intensification of the radiation boost in locally advanced anal canal carcinoma: Final analysis of the randomized UNICANCER ACCORD 03 trial. J. Clin. Oncol. 2012, 30, 1941–1948. [Google Scholar] [CrossRef]
- Rao, S.; Sclafani, F.; Eng, C.; Adams, R.A.; Guren, M.G.; Sebag-Montefiore, D.; Benson, A.; Bryant, A.; Peckitt, C.; Segelov, E.; et al. International Rare Cancers Initiative Multicenter Randomized Phase II Trial of Cisplatin and Fluorouracil Versus Carboplatin and Paclitaxel in Advanced Anal Cancer: InterAAct. J. Clin. Oncol. 2020, 38, 2510–2518. [Google Scholar] [CrossRef]
- Kim, S.; François, E.; André, T.; Samalin, E.; Jary, M.; El Hajbi, F.; Baba-Hamed, N.; Pernot, S.; Kaminsky, M.-C.; Bouché, O.; et al. Docetaxel, cisplatin, and fluorouracil chemotherapy for metastatic or unresectable locally recurrent anal squamous cell carcinoma (Epitopes-HPV02): A multicentre, single-arm, phase 2 study. Lancet Oncol. 2018, 19, 1094–1106. [Google Scholar] [CrossRef]
- Rajdev, L.; Lensing, S.; Ramos, J.; Baiocchi, R.; Wang, C.-C.; Ratner, L.; Rubinstein, P.; Ambinder, R.; Henry, D.; Streicher, H.; et al. 1023MO AMC 095: A report of nivolumab (nivo) in advanced HIV associated solid tumours (ST). Ann. Oncol. 2020, 31, S706. [Google Scholar] [CrossRef]
- Morris, V.; Liu, S.; Johnson, B.; Prasad, S.; Mahvash, A.; Bhosale, P.; Rubin, M.; Rothschild, N.; Futreal, A.; Wistuba, I.; et al. 403MO Atezolizumab in combination with bevacizumab for patients with unresectable/metastatic anal cancer. Ann. Oncol. 2020, 31, S412. [Google Scholar] [CrossRef]
- Ott, P.A.; Piha-Paul, S.A.; Munster, P.; Pishvaian, M.J.; van Brummelen, E.M.J.; Cohen, R.B.; Gomez-Roca, C.; Ejadi, S.; Stein, M.; Chan, E.; et al. Safety and antitumor activity of the anti-PD-1 antibody pembrolizumab in patients with recurrent carcinoma of the anal canal. Ann. Oncol. 2017, 28, 1036–1041. [Google Scholar] [CrossRef] [PubMed]
- Marabelle, A.; Cassier, P.A.; Fakih, M.; Guren, T.K.; Italiano, A.; Kao, S.C.-H.; Nielsen, D.; Ascierto, P.A.; Bariani, G.M.; Santoro, A.; et al. Pembrolizumab for advanced anal squamous cell carcinoma (ASCC): Results from the multicohort, phase II KEYNOTE-158 study. J. Clin. Oncol. 2020, 38 (Suppl. S4), 1. [Google Scholar] [CrossRef] [PubMed]
- Rao JCapdevila DGilbert, S.K.i.m. LBA42—POD1UM-202: Phase II study of retifanlimab in patients (pts) with squamous carcinoma of the anal canal (SCAC) who progressed following platinum-based chemotherapy. Ann. Oncol. 2020, 31 (Suppl. S4), S1142–S1215. [Google Scholar]
- Lonardi, S.; Prete, A.A.; Morano, F.; Messina, M.; Formica, V.; Corsi, D.C.; Orciuolo, C.; Frassineti, G.L.; Zampino, M.G.; Casagrande, M.; et al. Randomized phase II trial of avelumab alone or in combination with cetuximab for patients with previously treated, locally advanced, or metastatic squamous cell anal carcinoma: The CARACAS study. J. Immunother. Cancer 2021, 9, e002996. [Google Scholar] [CrossRef]
- Kim, S.; Ghiringhelli, F.; De La Fouchardiere, C.; Francois, E.; Smith, D.M.; Samalin, E.; Ataz, D.L.-T.; Parzy, A.; Desrame, J.; Baba-Hamed, N.; et al. Atezolizumab plus modified DCF (docetaxel, cisplatin, and 5-fluorouracil) as first-line treatment for metastatic or locally advanced squamous cell anal carcinoma: A SCARCE-PRODIGE 60 randomized phase II study. J. Clin. Oncol. 2022, 40 (Suppl. S16), 3508. [Google Scholar] [CrossRef]
- Smaglo, B.G.; Tesfaye, A.; Halfdanarson, T.R.; Meyer, J.E.; Wang, J.; Gatalica, Z.; Reddy, S.; Arguello, D.; Boland, P.M. Comprehensive multiplatform biomarker analysis of 199 anal squamous cell carcinomas. Oncotarget 2015, 6, 43594–43604. [Google Scholar] [CrossRef] [Green Version]
- Chung, J.H.; Sanford, E.; Johnson, A.; Klempner, S.J.; Schrock, A.B.; Palma, N.A.; Erlich, R.L.; Frampton, G.M.; Chalmers, Z.R.; Vergilio, J.; et al. Comprehensive genomic profiling of anal squamous cell carcinoma reveals distinct genomically defined classes. Ann Oncol. 2016, 27, 1336–1341. [Google Scholar] [CrossRef]
- Morris, V.; Rao, X.; Pickering, C.; Foo, W.C.; Rashid, A.; Eterovic, K.; Kim, T.; Chen, K.; Wang, J.; Shaw, K.; et al. Comprehensive Genomic Profiling of Metastatic Squamous Cell Carcinoma of the Anal Canal. Mol. Cancer Res. 2017, 15, 1542–1550. [Google Scholar] [CrossRef] [Green Version]
- Tamaki, A.; Ierano, C.; Szakacs, G.; Robey, R.W.; Bates, S.E. The controversial role of ABC transporters in clinical oncology. Essays Biochem. 2011, 50, 209–232. [Google Scholar]
- Lukan, N.; Ströbel, P.; Willer, A.; Kripp, M.; Dinter, D.; Mai, S.; Hochhaus, A.; Hofheinz, R.-D. Cetuximab-based treatment of metastatic anal cancer: Correlation of response with KRAS mutational status. Oncology 2009, 77, 293–299. [Google Scholar] [CrossRef]
- Bernardi, M.-P.; Ngan, S.Y.; Michael, M.; Lynch, A.C.; Heriot, A.G.; Ramsay, R.; Phillips, W. Molecular biology of anal squamous cell carcinoma: Implications for future research and clinical intervention. Lancet Oncol. 2015, 16, e611–e621. [Google Scholar] [CrossRef]
- Clarke, M.A.; Wentzensen, N. Strategies for screening and early detection of anal cancers: A narrative and systematic review and meta-analysis of cytology, HPV testing, and other biomarkers: Review of Anal Cancer Screening Tests. Cancer Cytopathol. 2018, 126, 447–460. [Google Scholar] [CrossRef] [PubMed]
- Škamperle, M.; Kocjan, B.J.; Maver, P.J.; Seme, K.; Poljak, M. Human papillomavirus (HPV) prevalence and HPV type distribution in cervical, vulvar, and anal cancers in central and eastern Europe. Acta Derm. Alp. Pannonica Adriat. 2013, 22, 1–5. [Google Scholar]
- De Vuyst, H.; Clifford, G.M.; Nascimento, M.C.; Madeleine, M.M.; Franceschi, S. Prevalence and type distribution of human papillomavirus in carcinoma and intraepithelial neoplasia of the vulva, vagina and anus: A meta-analysis. Int. J. Cancer 2009, 124, 1626–1636. [Google Scholar] [CrossRef] [PubMed]
- Valmary-Degano, S.; Jacquin, E.; Prétet, J.-L.; Monnien, F.; Girardo, B.; Arbez-Gindre, F.; Joly, M.; Bosset, J.-F.; Kantelip, B.; Mougin, C. Signature patterns of human papillomavirus type 16 in invasive anal carcinoma. Hum. Pathol. 2013, 44, 992–1002. [Google Scholar] [CrossRef]
- Wong, A.K.; Chan, R.C.; Aggarwal, N.; Singh, M.K.; Nichols, W.S.; Bose, S. Human papillomavirus genotypes in anal intraepithelial neoplasia and anal carcinoma as detected in tissue biopsies. Mod. Pathol. 2010, 23, 144–150. [Google Scholar] [CrossRef]
- Rödel, F.; Wieland, U.; Fraunholz, I.; Kitz, J.; Rave-Fränk, M.; Wolff, H.A.; Weiss, C.; Wirtz, R.; Balermpas, P.; Fokas, E.; et al. Human papillomavirus DNA load and p16 INK4a expression predict for local control in patients with anal squamous cell carcinoma treated with chemoradiotherapy: HPV16 DNA and p16 INK4a Expression. Int. J. Cancer 2015, 136, 278–288. [Google Scholar] [CrossRef]
- Mai, S.; Welzel, G.; Ottstadt, M.; Lohr, F.; Severa, S.; Prigge, E.-S.; Wentzensen, N.; Trunk, M.J.; Wenz, F.; von Knebel-Doeberitz, M.; et al. Prognostic Relevance of HPV Infection and p16 Overexpression in Squamous Cell Anal Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2015, 93, 819–827. [Google Scholar] [CrossRef]
- Parwaiz, I.; MacCabe, T.A.; Thomas, M.G.; Messenger, D.E. A Systematic Review and Meta-Analysis of Prognostic Biomarkers in Anal Squamous Cell Carcinoma Treated with Primary Chemoradiotherapy. Clin. Oncol. (R Coll. Radiol.) 2019, 31, e1–e13. [Google Scholar] [CrossRef]
- Moniz, C.M.V.; Riechelmann, R.P.; Oliveira, S.C.R.; Bariani, G.M.; Rivelli, T.G.; Ortega, C.; Pereira, A.A.L.; Meireles, S.I.; Franco, R.; Chen, A.; et al. A Prospective Cohort Study of Biomarkers in Squamous Cell Carcinoma of the Anal Canal (SCCAC) and their Influence on Treatment Outcomes. J. Cancer 2021, 12, 7018–7025. [Google Scholar] [CrossRef]
- Chatfield-Reed, K.; Roche, V.P.; Pan, Q. cfDNA detection for HPV+ squamous cell carcinomas. Oral Oncol. 2021, 115, 104958. [Google Scholar] [CrossRef] [PubMed]
- Moati, E.; Taly, V.; Garinet, S.; Didelot, A.; Taieb, J.; Laurent-Puig, P.; Zaanan, A. Role of Circulating Tumor DNA in Gastrointestinal Cancers: Current Knowledge and Perspectives. Cancers 2021, 13, 4743. [Google Scholar] [CrossRef] [PubMed]
- Cabel, L.; Jeannot, E.; Bieche, I.; Vacher, S.; Callens, C.; Bazire, L.; Morel, A.; Bernard-Tessier, A.; Chemlali, W.; Schnitzler, A.; et al. Prognostic Impact of Residual HPV ctDNA Detection after Chemoradiotherapy for Anal Squamous Cell Carcinoma. Clin. Cancer Res. 2018, 24, 5767–5771. [Google Scholar] [CrossRef] [Green Version]
- Colón-López, V.; Shiels, M.S.; Machin, M.; Ortiz, A.P.; Strickler, H.; Castle, P.E.; Pfeiffer, R.M.; Engels, E.A. Anal Cancer Risk Among People with HIV Infection in the United States. J. Clin. Oncol 2018, 36, 68–75. [Google Scholar] [CrossRef]
- Guiguet, M.; Boué, F.; Cadranel, J.; Lang, J.-M.; Rosenthal, E.; Costagliola, D. Effect of immunodeficiency, HIV viral load, and antiretroviral therapy on the risk of individual malignancies (FHDH-ANRS CO4): A prospective cohort study. Lancet Oncol. 2009, 10, 1152–1159. [Google Scholar] [CrossRef]
- Bertisch, B.; Franceschi, S.; Lise, M.; Vernazza, P.; Keiser, O.; Schöni-Affolter, F.; Bouchardy, C.; Dehler, S.; Levi, F.; Jundt, G.; et al. Risk factors for anal cancer in persons infected with HIV: A nested case-control study in the Swiss HIV Cohort Study. Am. J. Epidemiol. 2013, 178, 877–884. [Google Scholar] [CrossRef]
- Wieland, U.; Kreuter, A.; Pfister, H. Human papillomavirus and immunosuppression. Curr. Probl. Dermatol. 2014, 45, 154–165. [Google Scholar] [PubMed]
- Geskus, R.B.; González, C.; Torres, M.; Del Romero, J.; Viciana, P.; Masiá, M.; Blanco, J.R.; Iribarren, M.; De Sanjosé, S.; Hernández-Novoa, B.; et al. Incidence and clearance of anal high-risk human papillomavirus in HIV-positive men who have sex with men: Estimates and risk factors. AIDS 2016, 30, 37–44. [Google Scholar] [CrossRef] [Green Version]
- The INSIGHT START Study Group; Lundgren, J.D.; Babiker, A.G.; Gordin, F.; Emery, S.; Grund, B.; Sharma, S.; Avihingsanon, A.; Cooper, D.A.; Fätkenheuer, G.; et al. Initiation of Antiretroviral Therapy in Early Asymptomatic HIV Infection. N. Engl. J. Med. 2015, 373, 795–807. [Google Scholar]
- The TEMPRANO ANRS 12136 Study Group; Danel, C.; Moh, R.; Gabillard, D.; Badje, A.; Le Carrou, J.; Ouassa, T.; Ouattara, E.; Anzian, A.; Ntakpé, J.B.; et al. A Trial of Early Antiretrovirals and Isoniazid Preventive Therapy in Africa. N. Engl. J. Med. 2015, 373, 808–822. [Google Scholar]
- Grinsztejn, B.; Hosseinipour, M.C.; Ribaudo, H.J.; Swindells, S.; Eron, J.; Chen, Y.Q.; Wang, L.; Ou, S.-S.; Anderson, M.; McCauley, M.; et al. Effects of early versus delayed initiation of antiretroviral treatment on clinical outcomes of HIV-1 infection: Results from the phase 3 HPTN 052 randomised controlled trial. Lancet Infect. Dis. 2014, 14, 281–290. [Google Scholar] [CrossRef] [Green Version]
- Borges, Á.H.; Neuhaus, J.; Babiker, A.G.; Henry, K.; Jain, M.K.; Palfreeman, A.; Mugyenyi, P.; Domingo, P.; Hoffmann, C.; Read, T.R.H.; et al. Immediate Antiretroviral Therapy Reduces Risk of Infection-Related Cancer During Early HIV Infection. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2016, 63, 1668. [Google Scholar] [CrossRef] [PubMed]
- WHO. Guideline on When to Start Antiretroviral Therapy and on Pre-Exposure Prophylaxis for HIV. 2015. Available online: https://apps.who.int/iris/bitstream/handle/10665/186275/9789241509565_eng.pdf (accessed on 27 June 2022).
- Cobucci, R.N.O.; Lima, P.H.; de Souza, P.C.; Costa, V.V.; Cornetta, M.; Fernandes, J.V.; Gonçalves, A.K. Assessing the impact of HAART on the incidence of defining and non-defining AIDS cancers among patients with HIV/AIDS: A systematic review. J. Infect. Public Health 2015, 8, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Kelly, H.; Chikandiwa, A.; Alemany Vilches, L.; Palefsky, J.M.; de Sanjose, S.; Mayaud, P. Association of antiretroviral therapy with anal high-risk human papillomavirus, anal intraepithelial neoplasia, and anal cancer in people living with HIV: A systematic review and meta-analysis. Lancet HIV 2020, 7, e262–e278. [Google Scholar] [CrossRef]
- Peddada, A.V.; Smith, D.E.; Rao, A.R.; Frost, D.B.; Kagan, A.R. Chemotherapy and low-dose radiotherapy in the treatment of HIV-infected patients with carcinoma of the anal canal. Int. J. Radiat. Oncol. Biol. Phys. 1997, 37, 1101–1105. [Google Scholar] [CrossRef]
- Kim, J.H.; Sarani, B.; Orkin, B.A.; Young, H.A.; White, J.; Tannebaum, I.; Stein, S.; Bennett, B. HIV-positive patients with anal carcinoma have poorer treatment tolerance and outcome than HIV-negative patients. Dis. Colon. Rectum 2001, 44, 1496–1502. [Google Scholar] [CrossRef]
- Alfa-Wali, M.; Allen-Mersh, T.; Antoniou, A.; Tait, D.; Newsom-Davis, T.; Gazzard, B.; Nelson, M.; Bower, M. Chemoradiotherapy for anal cancer in HIV patients causes prolonged CD4 cell count suppression. Ann. Oncol. 2012, 23, 141–147. [Google Scholar] [CrossRef]
- Chiao, E.Y.; Giordano, T.P.; Richardson, P.; El-Serag, H.B. Human immunodeficiency virus-associated squamous cell cancer of the anus: Epidemiology and outcomes in the highly active antiretroviral therapy era. J. Clin. Oncol. 2008, 26, 474–479. [Google Scholar] [CrossRef]
- Fraunholz, I.; Rabeneck, D.; Gerstein, J.; Jäck, K.; Haberl, A.; Weiss, C.; Rödel, C. Concurrent chemoradiotherapy with 5-fluorouracil and mitomycin C for anal carcinoma: Are there differences between HIV-positive and HIV-negative patients in the era of highly active antiretroviral therapy? Radiother. Oncol. 2011, 98, 99–104. [Google Scholar] [CrossRef]
- Seo, Y.; Kinsella, M.T.; Reynolds, H.L.; Chipman, G.; Remick, S.C.; Kinsella, T.J. Outcomes of chemoradiotherapy with 5-Fluorouracil and mitomycin C for anal cancer in immunocompetent versus immunodeficient patients. Int. J. Radiat. Oncol. Biol. Phys. 2009, 75, 143–149. [Google Scholar] [CrossRef]
- Wexler, A.; Berson, A.M.; Goldstone, S.E.; Waltzman, R.; Penzer, J.; Maisonet, O.G.; McDermott, B.; Rescigno, J. Invasive anal squamous-cell carcinoma in the HIV-positive patient: Outcome in the era of highly active antiretroviral therapy. Dis. Colon. Rectum. 2008, 51, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Martin, D.; Balermpas, P.; Fokas, E.; Rödel, C.; Yildirim, M. Are there HIV-specific Differences for Anal Cancer Patients Treated with Standard Chemoradiotherapy in the Era of Combined Antiretroviral Therapy? Clin. Oncol. 2017, 29, 248–255. [Google Scholar] [CrossRef]
- Hogg, M.E.; Popowich, D.A.; Wang, E.C.; Kiel, K.D.; Stryker, S.J.; Halverson, A.L. HIV and anal cancer outcomes: A single institution’s experience. Dis. Colon. Rectum 2009, 52, 891–897. [Google Scholar] [CrossRef]
- Munoz-Bongrand, N.; Poghosyan, T.; Zohar, S.; Gerard, L.; Chirica, M.; Quéro, L.; Gornet, J.-M.; Cattan, P. Anal carcinoma in HIV-infected patients in the era of antiretroviral therapy: A comparative study. Dis. Colon. Rectum 2011, 54, 729–735. [Google Scholar] [CrossRef] [PubMed]
- Oehler-Jänne, C.; Huguet, F.; Provencher, S.; Seifert, B.; Negretti, L.; Riener, M.-O.; Bonet, M.; Allal, A.S.; Ciernik, I.F. HIV-specific differences in outcome of squamous cell carcinoma of the anal canal: A multicentric cohort study of HIV-positive patients receiving highly active antiretroviral therapy. J. Clin. Oncol. 2008, 26, 2550–2557. [Google Scholar] [CrossRef] [PubMed]
- Grew, D.; Bitterman, D.; Leichman, C.G.; Leichman, L.; Sanfilippo, N.; Moore, H.G.; Du, K. HIV Infection Is Associated with Poor Outcomes for Patients with Anal Cancer in the Highly Active Antiretroviral Therapy Era. Dis. Colon. Rectum 2015, 58, 1130–1136. [Google Scholar] [CrossRef] [PubMed]
- Morris, V.K.; Salem, M.E.; Nimeiri, H.; Iqbal, S.; Singh, P.; Ciombor, K.; Polite, B.; Deming, D.; Chan, E.; Wade, J.L.; et al. Nivolumab for previously treated unresectable metastatic anal cancer (NCI9673): A multicentre, single-arm, phase 2 study. Lancet Oncol. 2017, 18, 446–453. [Google Scholar] [CrossRef] [Green Version]
- Yanik, E.L.; Kaunitz, G.J.; Cottrell, T.R.; Succaria, F.; McMiller, T.L.; Ascierto, M.L.; Esandrio, K.; Xu, H.; Ogurtsova, A.; Cornish, T.; et al. Association of HIV Status with Local Immune Response to Anal Squamous Cell Carcinoma: Implications for Immunotherapy. JAMA Oncol. 2017, 3, 974–978. [Google Scholar] [CrossRef]
- Dyck, L.; Mills, K.H.G. Immune checkpoints and their inhibition in cancer and infectious diseases. Eur. J. Immunol. 2017, 47, 765–779. [Google Scholar] [CrossRef]
- Lampejo, T.; Kavanagh, D.; Clark, J.; Goldin, R.; Osborn, M.; Ziprin, P.; Cleator, S. Prognostic biomarkers in squamous cell carcinoma of the anus: A systematic review. Br. J. Cancer 2010, 103, 1858–1869. [Google Scholar] [CrossRef] [Green Version]
- Ajani, J.A.; Wang, X.; Izzo, J.G.; Crane, C.H.; Eng, C.; Skibber, J.M.; Das, P.; Rashid, A. Molecular biomarkers correlate with disease-free survival in patients with anal canal carcinoma treated with chemoradiation. Dig. Dis. Sci. 2010, 55, 1098–1105. [Google Scholar] [CrossRef]
- Doll, C.M.; Moughan, J.; Klimowicz, A.; Ho, C.K.; Kornaga, E.N.; Lees-Miller, S.P.; Ajani, J.A.; Crane, C.H.; Kachnic, L.A.; Okawara, G.S.; et al. Significance of Co-expression of Epidermal Growth Factor Receptor and Ki67 on Clinical Outcome in Patients with Anal Cancer Treated with Chemoradiotherapy: An Analysis of NRG Oncology RTOG 9811. Int. J. Radiat. Oncol. Biol. Phys. 2017, 97, 554–562. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Govindarajan, R.; Gujja, S.; Siegel, E.R.; Batra, A.; Saeed, A.; Lai, K.; James, J.D.; Fogel, B.J.; Williamson, S. Programmed Cell Death-Ligand 1 (PD-L1) Expression in Anal Cancer. Am. J. Clin. Oncol. 2018, 41, 638–642. [Google Scholar] [CrossRef] [PubMed]
- Wessely, A.; Heppt, M.V.; Kammerbauer, C.; Steeb, T.; Kirchner, T.; Flaig, M.J.; French, L.E.; Berking, C.; Schmoeckel, E.; Reinholz, M. Evaluation of PD-L1 Expression and HPV Genotyping in Anal Squamous Cell Carcinoma. Cancers 2020, 12, 2516. [Google Scholar] [CrossRef] [PubMed]
- Iseas, S.; Golubicki, M.; Robbio, J.; Ruiz, G.; Guerra, F.; Mariani, J.; Salanova, R.; Cabanne, A.; Eleta, M.; Gonzalez, J.V.; et al. A clinical and molecular portrait of non-metastatic anal squamous cell carcinoma. Transl. Oncol. 2021, 14, 101084. [Google Scholar] [CrossRef]
- Balermpas, P.; Martin, D.; Wieland, U.; Rave-Fränk, M.; Strebhardt, K.; Rödel, C.; Fokas, E.; Rödel, F. Human papilloma virus load and PD-1/PD-L1, CD8+ and FOXP3 in anal cancer patients treated with chemoradiotherapy: Rationale for immunotherapy. Oncoimmunology 2017, 6, e1288331. [Google Scholar] [CrossRef] [Green Version]
- Armstrong, S.A.; Malley, R.; Wang, H.; Lenz, H.-J.; Arguello, D.; El-Deiry, W.S.; Xiu, J.; Gatalica, Z.; Philip, P.A.; Shields, A.F.; et al. Molecular characterization of squamous cell carcinoma of the anal canal. J. Gastrointest. Oncol. 2021, 12, 2423–2437. [Google Scholar] [CrossRef]
- Rao, S.; Guren, M.; Khan, K.; Brown, G.; Renehan, A.; Steigen, S.; Deutsch, E.; Martinelli, E.; Arnold, D. Anal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2021, 32, 1087–1100. [Google Scholar] [CrossRef]
- Xiao, W.; Yuan, Y.; Wang, S.; Liao, Z.; Cai, P.; Chen, B.; Zhang, R.; Wang, F.; Zeng, Z.; Gao, Y. Neoadjuvant PD-1 Blockade Combined with Chemotherapy Followed by Concurrent Immunoradiotherapy in Locally Advanced Anal Canal Squamous Cell Carcinoma Patients: Antitumor Efficacy, Safety and Biomarker Analysis. Front. Immunol. 2021, 12, 798451. [Google Scholar] [CrossRef]
- Wakeham, K.; Murray, L.; Muirhead, R.; Hawkins, M.; Sebag-Montefiore, D.; Brown, S.; Murphy, L.; Thomas, G.; Bell, S.; Whibley, M.; et al. Multicentre Investigation of Prognostic Factors Incorporating p16 and Tumour Infiltrating Lymphocytes for Anal Cancer After Chemoradiotherapy. Clin. Oncol. 2021, 33, 638–649. [Google Scholar] [CrossRef]
- Zou, Q.; Wang, X.; Ren, D.; Hu, B.; Tang, G.; Zhang, Y.; Huang, M.; Pai, R.K.; Buchanan, D.D.; Win, A.K.; et al. DNA methylation-based signature of CD8+ tumor-infiltrating lymphocytes enables evaluation of immune response and prognosis in colorectal cancer. J. Immunother. Cancer 2021, 9, e002671. [Google Scholar] [CrossRef] [PubMed]
- Ward, M.J.; Thirdborough, S.M.; Mellows, T.; Riley, C.; Harris, S.; Suchak, K.; Webb, A.; Hampton, C.; Patel, N.N.; Randall, C.J.; et al. Tumour-infiltrating lymphocytes predict for outcome in HPV-positive oropharyngeal cancer. Br. J. Cancer 2014, 110, 489–500. [Google Scholar] [CrossRef] [Green Version]
- Gilbert, D.C.; Serup-Hansen, E.; Linnemann, D.; Høgdall, E.; Bailey, C.; Summers, J.; Havsteen, H.; Thomas, G.J. Tumour-infiltrating lymphocyte scores effectively stratify outcomes over and above p16 post chemo-radiotherapy in anal cancer. Br. J. Cancer 2016, 114, 134–137. [Google Scholar] [CrossRef] [PubMed]
- Misale, S.; Di Nicolantonio, F.; Sartore-Bianchi, A.; Siena, S.; Bardelli, A. Resistance to anti-EGFR therapy in colorectal cancer: From heterogeneity to convergent evolution. Cancer Discov. 2014, 4, 1269–1280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hecht, J.R.; Douillard, J.-Y.; Schwartzberg, L.; Grothey, A.; Kopetz, S.; Rong, A.; Oliner, K.S.; Sidhu, R. Extended RAS analysis for anti-epidermal growth factor therapy in patients with metastatic colorectal cancer. Cancer Treat. Rev. 2015, 41, 653–659. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kopetz, S.; Grothey, A.; Yaeger, R.; Van Cutsem, E.; Desai, J.; Yoshino, T.; Wasan, H.; Ciardiello, F.; Loupakis, F.; Hong, Y.S.; et al. Encorafenib, Binimetinib, and Cetuximab in BRAF V600E–Mutated Colorectal Cancer. N. Engl. J. Med. 2019, 381, 1632–1643. [Google Scholar] [CrossRef] [Green Version]
- Morris, V.; Eng, C. Metastatic Anal Cancer and Novel Agents. Surg. Oncol. Clin. 2017, 26, 133–142. [Google Scholar] [CrossRef]
- Rogers, J.E.; Ohinata, A.; Silva, N.N.; Mehdizadeh, A.; Eng, C. Epidermal growth factor receptor inhibition in metastatic anal cancer. Anticancer Drugs 2016, 27, 804–808. [Google Scholar] [CrossRef]
- Rogers, J.E.; Jácome, A.A.A.; Ohinata, A.; Wolff, R.; Morris, V.K.; Johnson, B.; Mehdizadeh, A.; Rothschild, N.D.; Ahmed, S.U.; Guerra, J.L.; et al. Outcomes with anti-EGFR monoclonal antibodies in metastatic and recurrent anal squamous cell carcinoma. Expert Rev. Anticancer Ther. 2020, 20, 901–908. [Google Scholar] [CrossRef]
- Tchelebi, L.T.; Eng, C.; Messick, C.A.; Hong, T.S.; Ludmir, E.B.; Kachnic, L.A.; Zaorsky, N.G. Current treatment and future directions in the management of anal cancer. CA Cancer J. Clin. 2022, 72, 183–195. [Google Scholar] [CrossRef]
- Salem, M.E.; Puccini, A.; Grothey, A.; Raghavan, D.; Goldberg, R.M.; Xiu, J.; Korn, W.M.; Weinberg, B.A.; Hwang, J.J.; Shields, A.F.; et al. Landscape of Tumor Mutation Load, Mismatch Repair Deficiency, and PD-L1 Expression in a Large Patient Cohort of Gastrointestinal Cancers. Mol. Cancer Res. 2018, 16, 805–812. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shao, C.; Li, G.; Huang, L.; Pruitt, S.; Castellanos, E.; Frampton, G.; Carson, K.R.; Snow, T.; Singal, G.; Fabrizio, D.; et al. Prevalence of High Tumor Mutational Burden and Association with Survival in Patients with Less Common Solid Tumors. JAMA Netw. Open 2020, 3, e2025109. [Google Scholar] [CrossRef] [PubMed]
- Marabelle, A.; Fakih, M.; Lopez, J.; Shah, M.; Shapira-Frommer, R.; Nakagawa, K.; Chung, H.C.; Kindler, H.L.; Lopez-Martin, J.A.; Miller, W.H., Jr.; et al. Association of tumour mutational burden with outcomes in patients with advanced solid tumours treated with pembrolizumab: Prospective biomarker analysis of the multicohort, open-label, phase 2 KEYNOTE-158 study. Lancet Oncol. 2020, 21, 1353–1365. [Google Scholar] [CrossRef]
|
|
|
|
|
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mathias-Machado, M.C.; Peixoto, R.D.; Moniz, C.M.V.; Jácome, A.A. Biomarkers in Anal Cancer: Current Status in Diagnosis, Disease Progression and Therapeutic Strategies. Biomedicines 2022, 10, 2029. https://doi.org/10.3390/biomedicines10082029
Mathias-Machado MC, Peixoto RD, Moniz CMV, Jácome AA. Biomarkers in Anal Cancer: Current Status in Diagnosis, Disease Progression and Therapeutic Strategies. Biomedicines. 2022; 10(8):2029. https://doi.org/10.3390/biomedicines10082029
Chicago/Turabian StyleMathias-Machado, Maria Cecília, Renata D’Alpino Peixoto, Camila Motta Venchiarutti Moniz, and Alexandre A. Jácome. 2022. "Biomarkers in Anal Cancer: Current Status in Diagnosis, Disease Progression and Therapeutic Strategies" Biomedicines 10, no. 8: 2029. https://doi.org/10.3390/biomedicines10082029
APA StyleMathias-Machado, M. C., Peixoto, R. D., Moniz, C. M. V., & Jácome, A. A. (2022). Biomarkers in Anal Cancer: Current Status in Diagnosis, Disease Progression and Therapeutic Strategies. Biomedicines, 10(8), 2029. https://doi.org/10.3390/biomedicines10082029






