Mechanical Properties of Polymethyl Methacrylate as Denture Base Material: Heat-Polymerized vs. 3D-Printed—Systematic Review and Meta-Analysis of In Vitro Studies
Abstract
1. Introduction
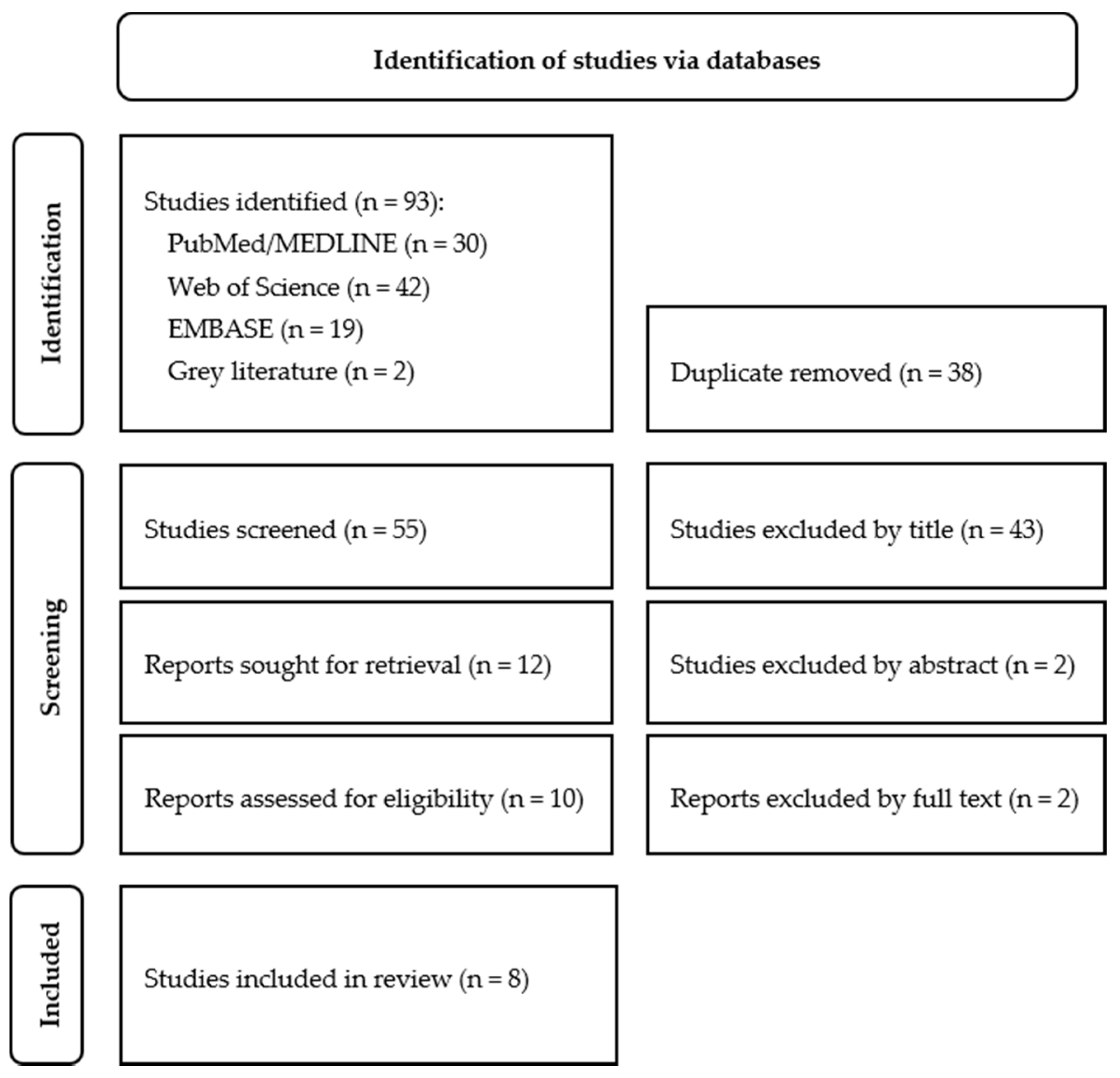
2. Materials and Methods
2.1. Information Sources and Search Strategy
2.2. Selection of Studies
2.3. Data Extraction and Quality Assessment
2.4. Statistical Analysis
3. Results
3.1. Study Characteristics
3.2. Quality Assessment
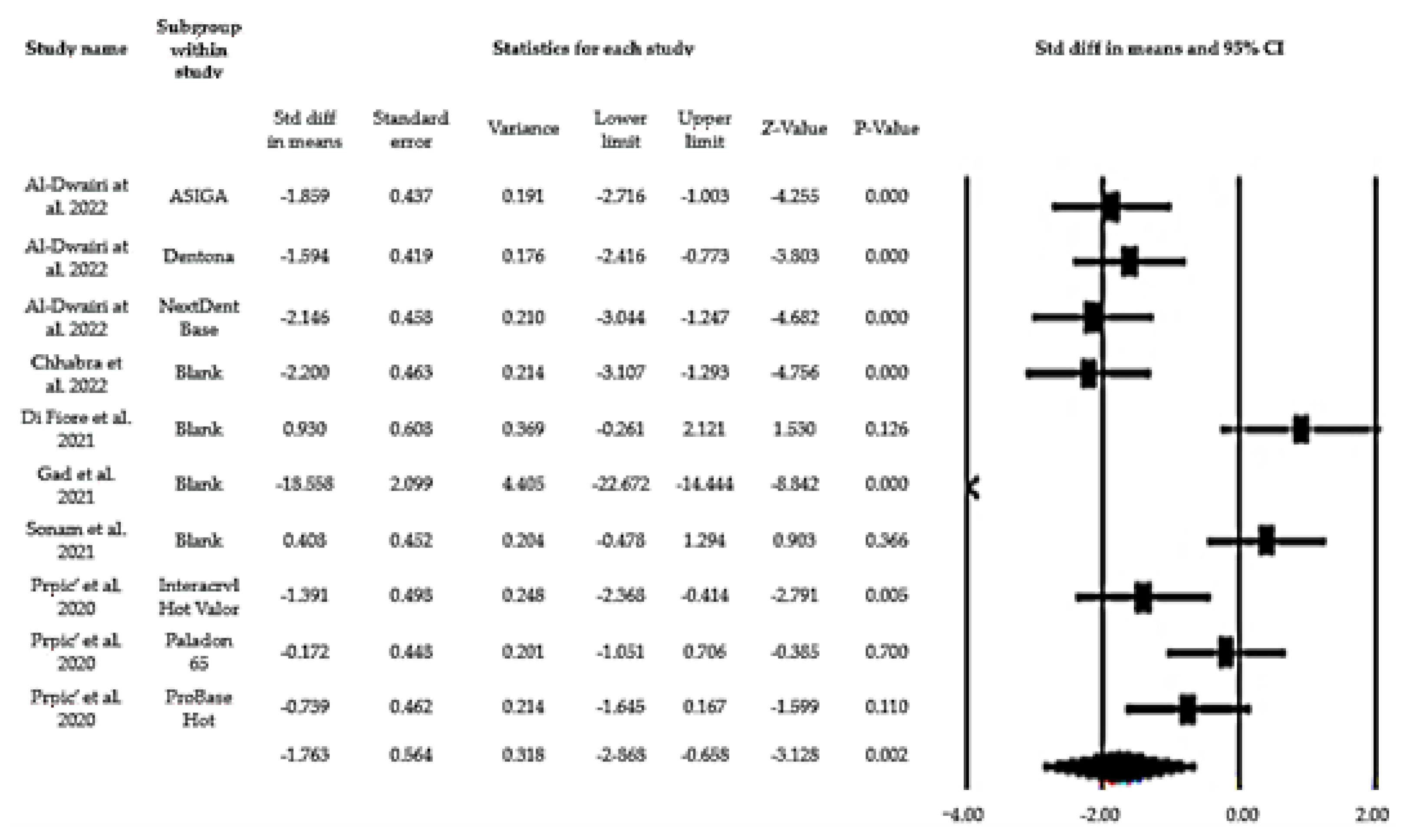
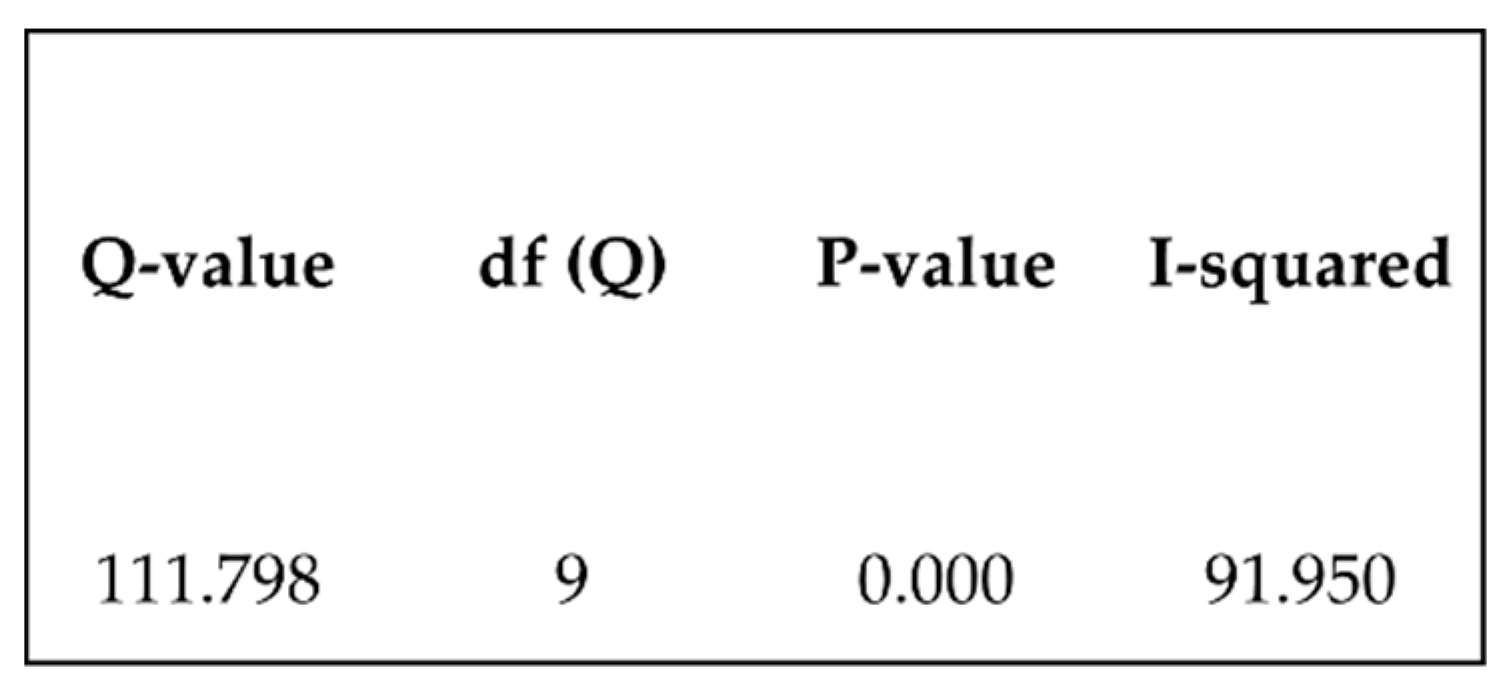
3.3. Flexural Strength
3.4. Impact Strength
3.5. Hardness
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zafar, M.S. Prosthodontic applications of polymethyl methacrylate (PMMA): An update. Polymers 2020, 12, 2299. [Google Scholar] [CrossRef] [PubMed]
- de Souza Leão, R.; de Moraes, S.L.D.; de Luna Gomes, J.M.; Lemos, C.A.A.; da Silva Casado, B.G.; do Egito Vasconcelos, B.C.; Pellizzer, E.P. Influence of addition of zirconia on PMMA: A systematic review. Mat. Sci. Eng. C Mater. Biol. Appl. 2020, 106, 110292. [Google Scholar] [CrossRef] [PubMed]
- Aldegheishem, A.; AlDeeb, M.; Al-Ahdal, K.; Helmi, M.; Alsagob, E.I. Influence of reinforcing agents on the mechanical properties of denture base resin: A systematic review. Polymers 2021, 13, 3083. [Google Scholar] [CrossRef] [PubMed]
- Gad, M.M.; Al-Thobity, A.M. The impact of nanoparticles-modified repair resin on denture repairs: A systematic review. Jpn. Dent. Sci. Rev. 2021, 57, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.; Asghar, M.; Din, S.U.; Zafar, M.S. Chapter 8—Thermoset Polymethacrylate-Based Materials for Dental Applications. Thermoset and Thermoplastic Polymers, 1st ed.; Grumezescu, V., Grumezescu, A.M., Eds.; ScienceDirect Elsevier: Amsterdam, The Netherlands, 2019; pp. 273–308. [Google Scholar] [CrossRef]
- Kul, E.; Aladağ, L.İ.; Yesildal, R. Evaluation of thermal conductivity and flexural strength properties of poly(methyl methacrylate) denture base material reinforced with different fillers. J. Prosthet. Dent. 2016, 116, 803–810. [Google Scholar] [CrossRef] [PubMed]
- Pillai, S.; Upadhyay, A.; Khayambashi, P.; Farooq, I.; Sabri, H.; Tarar, M.; Lee, K.T.; Harb, I.; Zhou, S.; Wang, Y.; et al. Dental 3D-printing: Transferring art from the laboratories to the clinics. Polymers 2021, 13, 157. [Google Scholar] [CrossRef] [PubMed]
- Schweiger, J.; Edelhoff, D.; Güth, J.F. 3D printing in digital prosthetic dentistry: An overview of recent developments in additive manufacturing. J. Clin. Med. 2021, 10, 2010. [Google Scholar] [CrossRef]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.S.; Jiang, H.B. A Review of 3D Printing in Dentistry: Technologies, Affecting Factors, and Applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Qin, Q.; Wang, J. A review of stereolithography: Processes and systems. Processes 2020, 8, 1138. [Google Scholar] [CrossRef]
- Lasserson, T.J.; Thomas, J.; Higgins, J.P.T. Chapter 1: Starting a review. In Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (Updated February 2021); Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, UK, 2021; pp. 1–11. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Tufanaru, C.; Munn, Z.; Aromataris, E.; Campbell, J.; Hopp, L. Chapter 3: Systematic reviews of effectiveness. Joanna Briggs Institute Reviewer’s Manual; Aromataris, E., Munn, Z., Eds.; The Joanna Briggs Institute: Adelaide, Australia, 2017. Available online: https://reviewersmanual.joannabriggs.org/ (accessed on 13 May 2022).
- Comprehensive Meta-Analysis Software (CMA). Available online: https://www.meta-analysis.com/?gclid=EAIaIQobChMIypPKrbGoAIVY7R3Ch1QfgDPEAAYASAAEgJlL_D_BwE (accessed on 27 May 2022).
- Sonam, D.; Dayalan, M.; Fatima, S.R.; Sasirekha, K. Comparative evaluation of impact and flexural strength of 3D printed, CAD/CAM milled and heat activated polymethyl methacrylate resins—An in vitro study. Int. J. Sci. Res. 2021, 10, 194–202. [Google Scholar]
- Fiore, A.D.; Meneghello, R.; Brun, P.; Rosso, S.; Gattazzo, A.; Stellini, E.; Yilmaz, B. Comparison of the flexural and surface properties of milled, 3D-printed, and heat polymerized PMMA resins for denture bases: An in vitro study. J. Prosthodont. Res. 2022, 66, 502–508. [Google Scholar] [CrossRef] [PubMed]
- ISO 1567:1999; Dentistry–Denture Base Polymers . ISO. Available online: https://www.iso.org/standard/20266.html (accessed on 3 July 2022).
- Abualsaud, R.; Gad, M.M. Flexural strength of CAD/CAM denture base materials: Systematic review and meta-analysis of in-vitro studies. J. Int. Soc. Prevent. Communit. Dent. 2022, 12, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Al-Dwairi, Z.N.; Al Haj Ebrahim, A.A.; Baba, N.Z. A comparison of the surface and mechanical properties of 3D printable denture-base resin material and conventional polymethylmethacrylate (PMMA). J. Prosthodont. 2022, in press. [Google Scholar] [CrossRef]
- Prpić, V.; Schauperl, Z.; Ćatić, A.; Dulčić, N.; Čimić, S. Comparison of mechanical properties of 3D-printed, CAD/CAM, and conventional denture base materials. J. Prosthodont. 2022, 29, 524–528. [Google Scholar] [CrossRef] [PubMed]
- Perea-Lowery, L.; Gibreel, M.; Vallittu, P.K.; Lassila, L.V. 3D-printed vs heat-polymerizing and autopolymerizing denture base acrylic resins. Materials 2021, 14, 5781. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M.; Abualsaud, R.; Alshahrani, F.A.; Al-Thobity, A.M.; Khan, S.Q.; Akhtar, S.; Ateeq, I.S.; Helal, M.A.; Al-Harbi, F.A. Strength and surface properties of a 3D-printed denture base polymer. J. Prosthodont. 2021, 31, 412–418. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Belles, D.; Gonzalez, M.; Kiat-Amnuay, S.; Dugarte, A.; Ontiveros, J. Impact strength of 3D printed and conventional heat-cured and cold-cured denture base acrylics. Int. J. Prosthodont. 2022, 35, 240–244. [Google Scholar] [CrossRef]
- Chhabra, M.; Kumar, M.N.; RaghavendraSwamy, K.N.; Thippeswamy, H.M. Flexural strength and impact strength of heat-cured acrylic and 3D printed denture base resins—A comparative in vitro study. J. Oral Biol. Craniofac. Res. 2022, 12, 1–3. [Google Scholar] [CrossRef]
- Naik, A.V. Complete denture fractures: A clinical study. J. Indian Prosthodont. Soc. 2009, 9, 148–150. [Google Scholar] [CrossRef]
| No. | First Author, Year of Publication | Title | Journal | Country |
|---|---|---|---|---|
| 1 | Lee J, 2022 | Impact strength of 3D printed and conventional heat-cured and cold-cured denture base acrylics | Int. J. Prosthodontics | USA |
| 2 | Al-Dwairi ZN, 2022 | A Comparison of the Surface and Mechanical Properties of 3D Printable Denture-Base Resin Material and Conventional Polymethylmethacrylate (PMMA) | J. Prosthodont. | Jordan |
| 3 | Chhabra M, 2022 | Flexural strength and impact strength of heat-cured acrylic and 3D printed denture base resins- A comparative in vitro study | J. Oral Biol. Craniofac. Res. | India |
| 4 | Fiore AD, 2022 | Comparison of the flexural and surface properties of milled, 3D-printed, and heat polymerized PMMA resins for denture bases: an in vitro study | J. Prosthodont. Res. | Italy |
| 5 | Perea-Lowery L, 2021 | 3D-Printed vs. Heat-Polymerizing and Autopolymerizing | Materials | Finland |
| 6 | Gad MM, 2021 | Strength and Surface Properties of a 3D-Printed Denture Base Polymer | J. Prosthodont. | Saudi Arabia |
| 7 | Sonam D, 2021 | Comparative Evaluation of Impact and Flexural Strength of 3D Printed, CAD/CAM Milled and Heat Activated Poylmethyl Methacrylate Resins: An In-Vitro Study | Int. J Sci. Res. | India |
| 8 | Prpic’ V, 2020 | Comparison of Mechanical Properties of 3D-Printed, CAD/CAM, and Conventional Denture Base Materials | J. Prosthodont. | Croatia |
| No. | Heat-Cured PMMA | 3D Printing PMMA | Samples (Number/Size) | Properties | Tests/Machine |
|---|---|---|---|---|---|
| 1 | Lucitone 199 Dentsply Sirona | Denture Base LP Formlabs, USA | 50 (25 per group) 64 × 12.7 × 3.2 mm | Impact strength | Izod impact strength test (Monitor Impact Tester, Testing Machines Inc) |
| 2 | Meliodent | NextDent, Denture 3D + 3D Systems, USA Dentona 3D, Dentona, Germany DentaBASE, ASIGA, Australia | 120 (15 per group) 65 × 10 × 3 mm 60 (15 per group) 25 × 25 × 3 mm | Flexural strength Impact strength Hardness | Three-point bending test, Charpy pendulum test, Vickers hardness test |
| 3 | DPI heat cure Dental Products Mumbai, India | Next Dent Denture 3D + 3D Systems, USA | 30 (15 per group) 64 × 10 × 3.3 mm 50 × 6 × 4 mm | Flexural strength Impact strength | Three-point bending test Izod impact strength test (International Equipments, India) |
| 4 | Aesthetic Blue Clear Candulor | NextDent Denture 3D + 3D Systems, USA | 12 (6 per group) 65 × 10 × 3.3 ± 0.2 mm | Flexural strength | Three-point bending test (Universal Testing Machine) (Acumen 3; MTS Systems Corp) |
| 5 | Paladon® 65 Kulzer GmbH Mitsui Chemicals Hanau, Germany | IMPRIMO® LC Denture Scheu-Dental GmbH Iserlohn, Germany | 48 (16 per group) 10 × 65 × 3.3 ± 0.2 mm | Flexural strength Mod. elasticity Fracture toughness | Three-point bending test (Model LRX; Lloyds Instruments Ltd., Fareham, UK) |
| 6 | Major Base.20 | NextDent Denture 3D + 3D Systems, USA | 60 (12 per group) 64 × 10 × 3.3 ± 0.2 mm 50 × 6 × 4 mm | Flexural strength Impact strength Hardness | Three-point bending test (Universal Testing Machine); Charpy pendulum test, Vickers hardness test and profilometer |
| 7 | Not identified | Not identified | 40 (10 per group) 64 × 10 × 3.3 mm 50 × 6 × 4 mm | Flexural strength Impact strength | Three-point bending test (Universal Testing Machine) Izod impact strength test (Digital Izod type impact testing machine) |
| 8 | ProBase Hot Paladon 65 Interacryl Hot | NextDent Denture 3D + 3D Systems, USA | 20 (10 per group) 64 × 10 × 3.3 ± 0.2 mm | Flexural strength Hardness | Three-point bending test; Brinell method |
| No. | Aim | Conclusions |
|---|---|---|
| 1 | Compare the impact strength of a 3D printing resin with a heat-cured resin. | The 3D printing resin ˃ impact strength than the heat-cured resin. |
| 2 | Compare the mechanical properties of three 3D printing resins with a heat-cured resin. | Regarding flexural strength and hardness, the heat-cured resin presented better results. Impact resistance: there were no statistically significant differences between the heat-cured resin and 3D printing resins. |
| 3 | Compare the flexural strength and impact strength of a heat-cured resin with a 3D printing resin. | The heat-cured resin presented better results in terms of flexural strength and impact strength compared with the resin for 3D printing. |
| 4 | Compare the flexural strength of a heat-cured resin with one for 3D printing. | The heat-cured resin and 3D printing resin showed similar results in terms of flexural strength. |
| 5 | Investigate the effects of two post-processing methods on the mechanical properties of a 3D printing resin and compare it with a heat-cured resin. | Post-processing methods impact the flexural strength of 3D printing resins. The resin for 3D printing had inferior mechanical properties when compared with the heat-cured resin. |
| 6 | Evaluate the flexural strength, impact strength and hardness of a resin for 3D printing and a heat-cured resin. | The resin for 3D printing had inferior results in flexural strength, impact strength and hardness compared with the thermosetting resin. |
| 7 | Evaluate the impact strength and flexural strength of a 3D printing resin and heat-cured resin. | The polymerization process has an influence on impact strength and flexural strength. The 3D printing resin presented higher impact and flexural strength in relation to the heat-cured resin. The impact strength and flexural strength values were higher than the recommended minimum. |
| 8 | Evaluate and compare the flexural strength and hardness of different materials and technologies for the manufacture of denture bases. | The resin for 3D printing had lower values of flexural strength and hardness compared with the other group under study. |
| Nº | Control Group | 3D Printing PMMA |
|---|---|---|
| 2 | 92.44 ± 7.91 | 74.89 ± 8.44 (NextDent); 81.33 ± 5.88 (Dentona); 79.33 ± 6.07 (ASIGA) |
| 3 | 92.01 ± 12.14 | 69.78 ± 7.54 |
| 4 | 80.79 ± 7.64 | 87.34 ± 6.39 |
| 6 | 86.63 ± 1.0 | 69.15 ± 0.88 |
| 7 | 93.90 ± 4.6 | 95.46 ± 2.84 |
| 8 | 97.35 ± 18.74 (Interacryl Hot) 86.25 ± 20.44 (ProBase Hot) 75.35 ± 18.60 (Paladon 65) | 72.25 ± 17.32 |
| Nº | Control Group | 3D Printing PMMA |
|---|---|---|
| 1 | 8.9 ± 0.3 | 11.2 ± 0.7 |
| 2 | 16.64 ± 1.69 | 15.20 ± 0.69 (NextDent); 17.98 ± 1.76 (Dentona); 16.76 ± 1.75 (ASIGA) |
| 3 | 1.67 ± 0.79 | 1.15 ± 0.40 |
| 6 | 6.32 ± 0.50 | 2.44 ± 0.31 |
| 7 | 2.08 ± 0.19 | 3.27 ± 0.12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lourinho, C.; Salgado, H.; Correia, A.; Fonseca, P. Mechanical Properties of Polymethyl Methacrylate as Denture Base Material: Heat-Polymerized vs. 3D-Printed—Systematic Review and Meta-Analysis of In Vitro Studies. Biomedicines 2022, 10, 2565. https://doi.org/10.3390/biomedicines10102565
Lourinho C, Salgado H, Correia A, Fonseca P. Mechanical Properties of Polymethyl Methacrylate as Denture Base Material: Heat-Polymerized vs. 3D-Printed—Systematic Review and Meta-Analysis of In Vitro Studies. Biomedicines. 2022; 10(10):2565. https://doi.org/10.3390/biomedicines10102565
Chicago/Turabian StyleLourinho, Cláudia, Helena Salgado, André Correia, and Patrícia Fonseca. 2022. "Mechanical Properties of Polymethyl Methacrylate as Denture Base Material: Heat-Polymerized vs. 3D-Printed—Systematic Review and Meta-Analysis of In Vitro Studies" Biomedicines 10, no. 10: 2565. https://doi.org/10.3390/biomedicines10102565
APA StyleLourinho, C., Salgado, H., Correia, A., & Fonseca, P. (2022). Mechanical Properties of Polymethyl Methacrylate as Denture Base Material: Heat-Polymerized vs. 3D-Printed—Systematic Review and Meta-Analysis of In Vitro Studies. Biomedicines, 10(10), 2565. https://doi.org/10.3390/biomedicines10102565






