Influence of Pre-Treatment and Artificial Aging on the Retention of 3D-Printed Permanent Composite Crowns
Abstract
1. Introduction
2. Material and Method
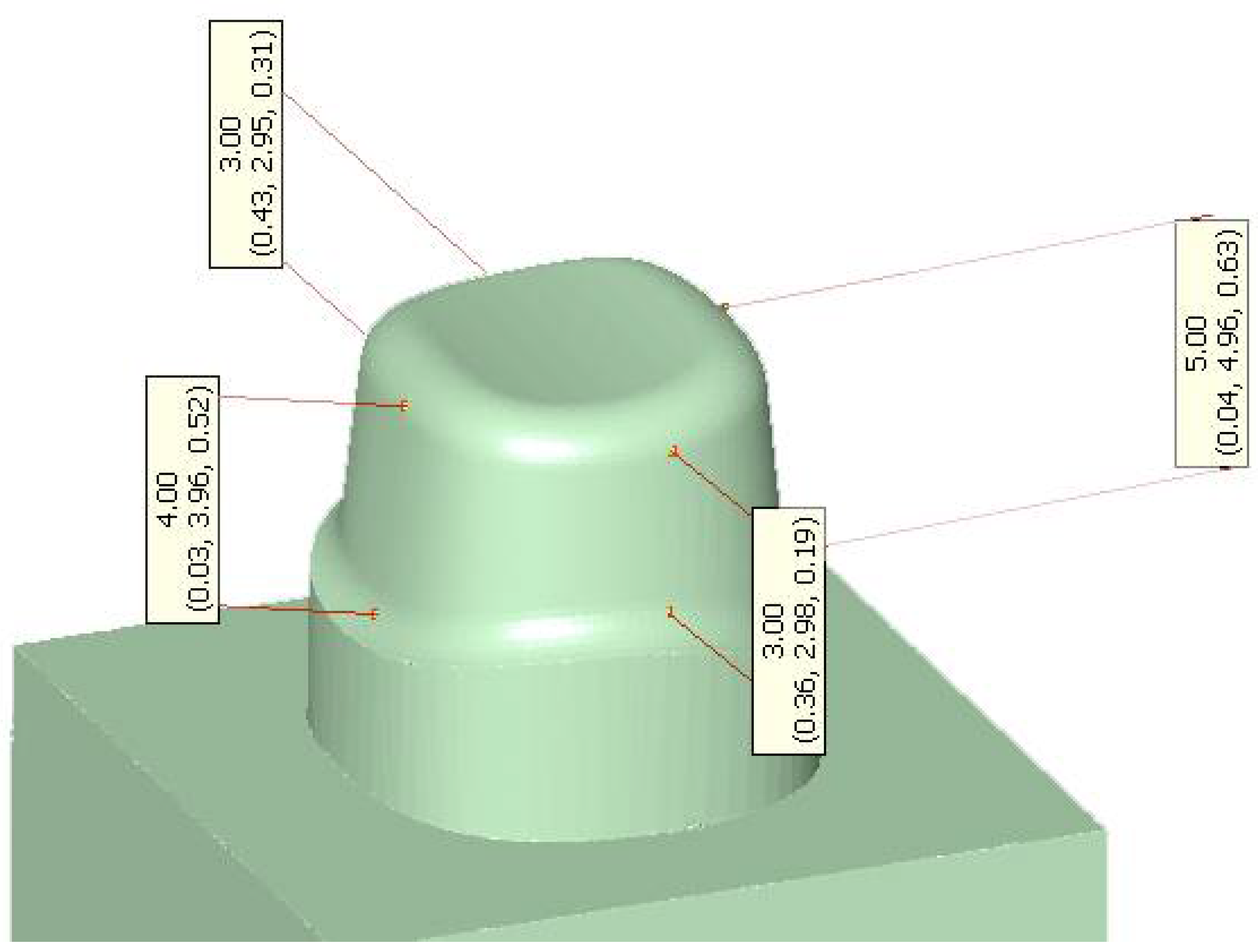
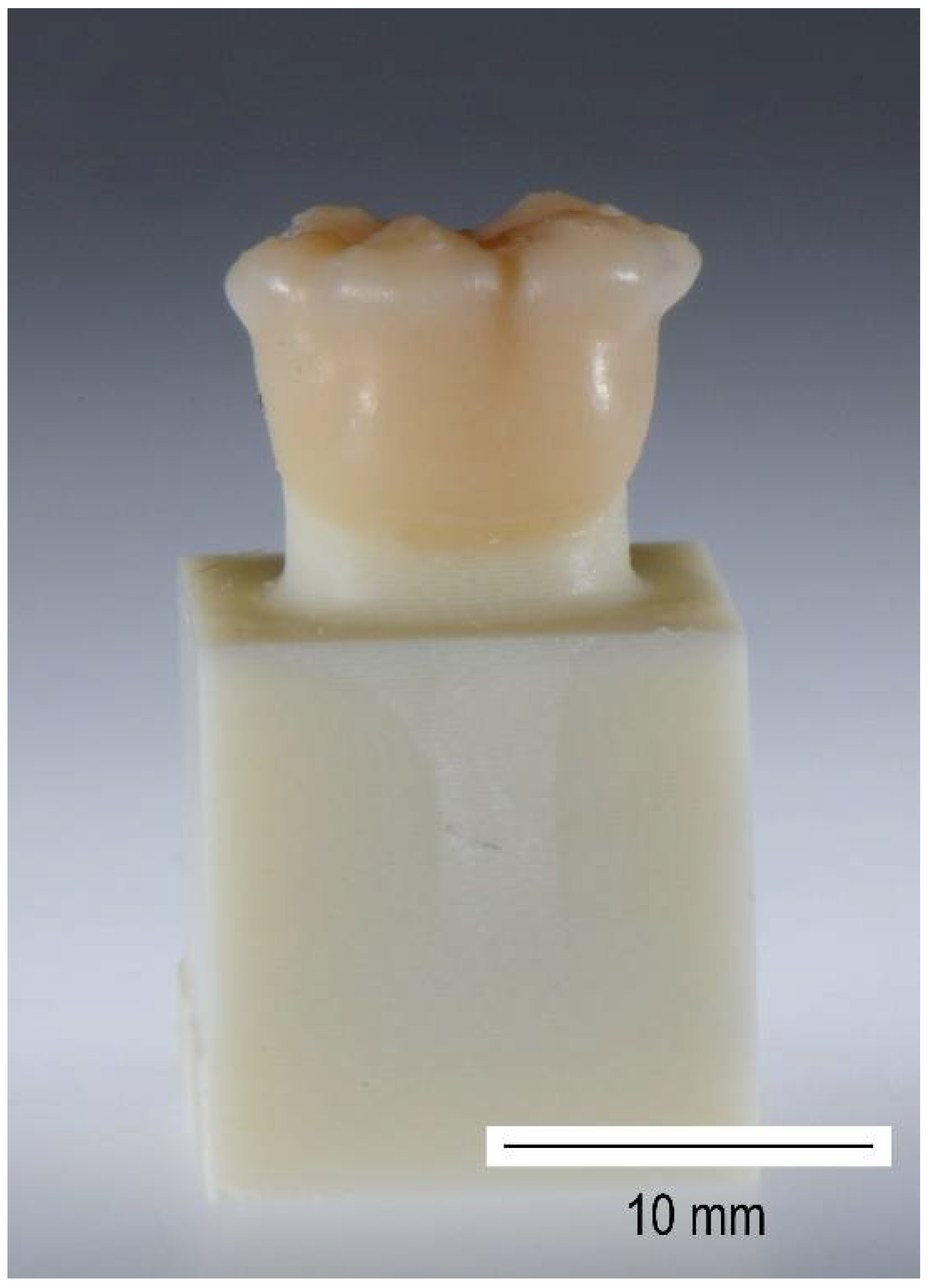
2.1. Fabrication of Test Specimens
2.2. Adhesive Luting Protocols
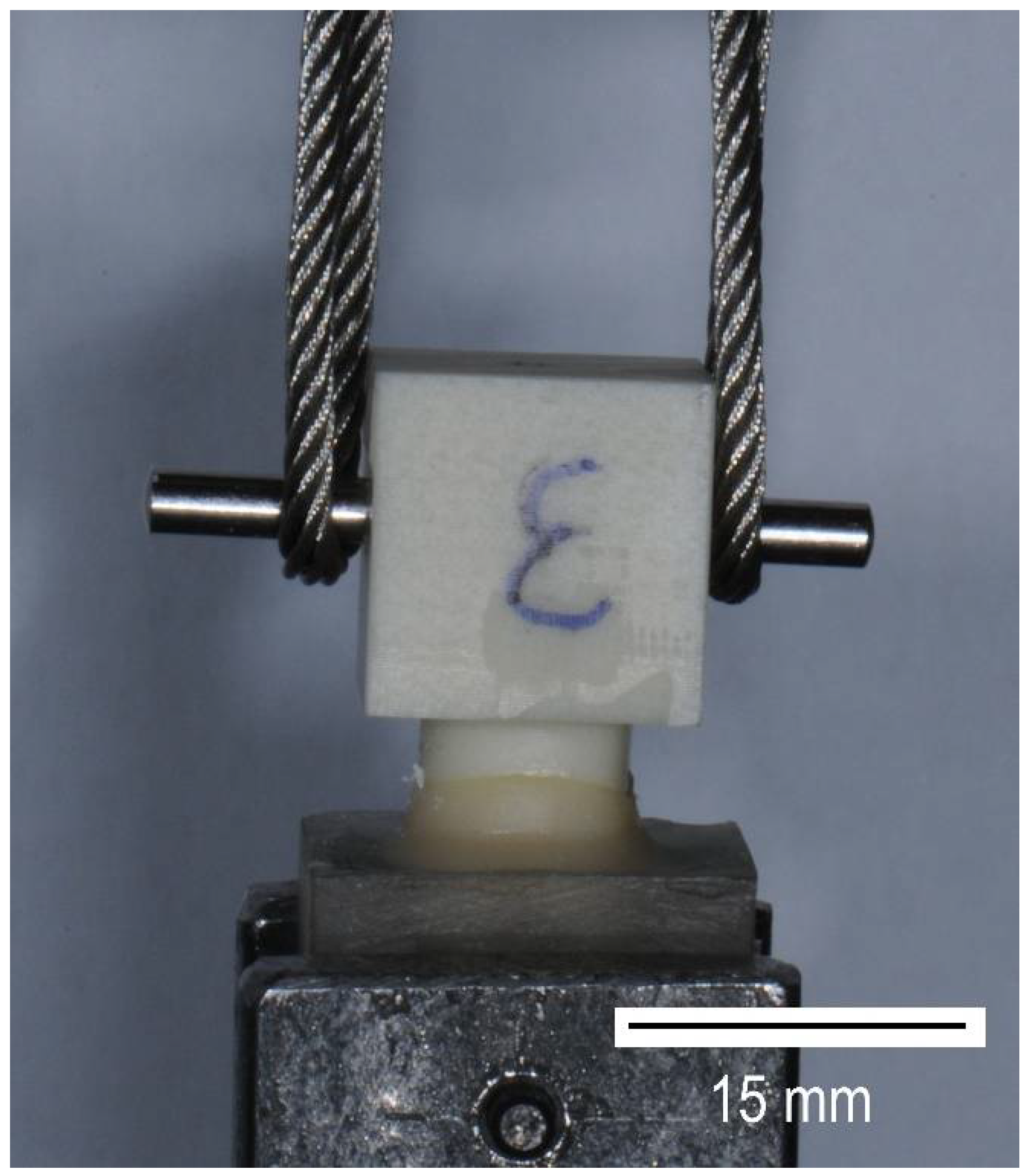
2.3. Artificial Aging and Pull-Off Test
- #1: “Complete debonding” (more than 50% of the lateral stump surface detached from the crown),
- #2: “Partial debonding” (less than 50% of the lateral stump surface detached from the crown),
- #3: “Debonding of the occlusal crown surface” (lateral crown surface adheres to the stump—excluded the occlusal surface), and
- #4: “Stump fractured”.
2.4. Statistics
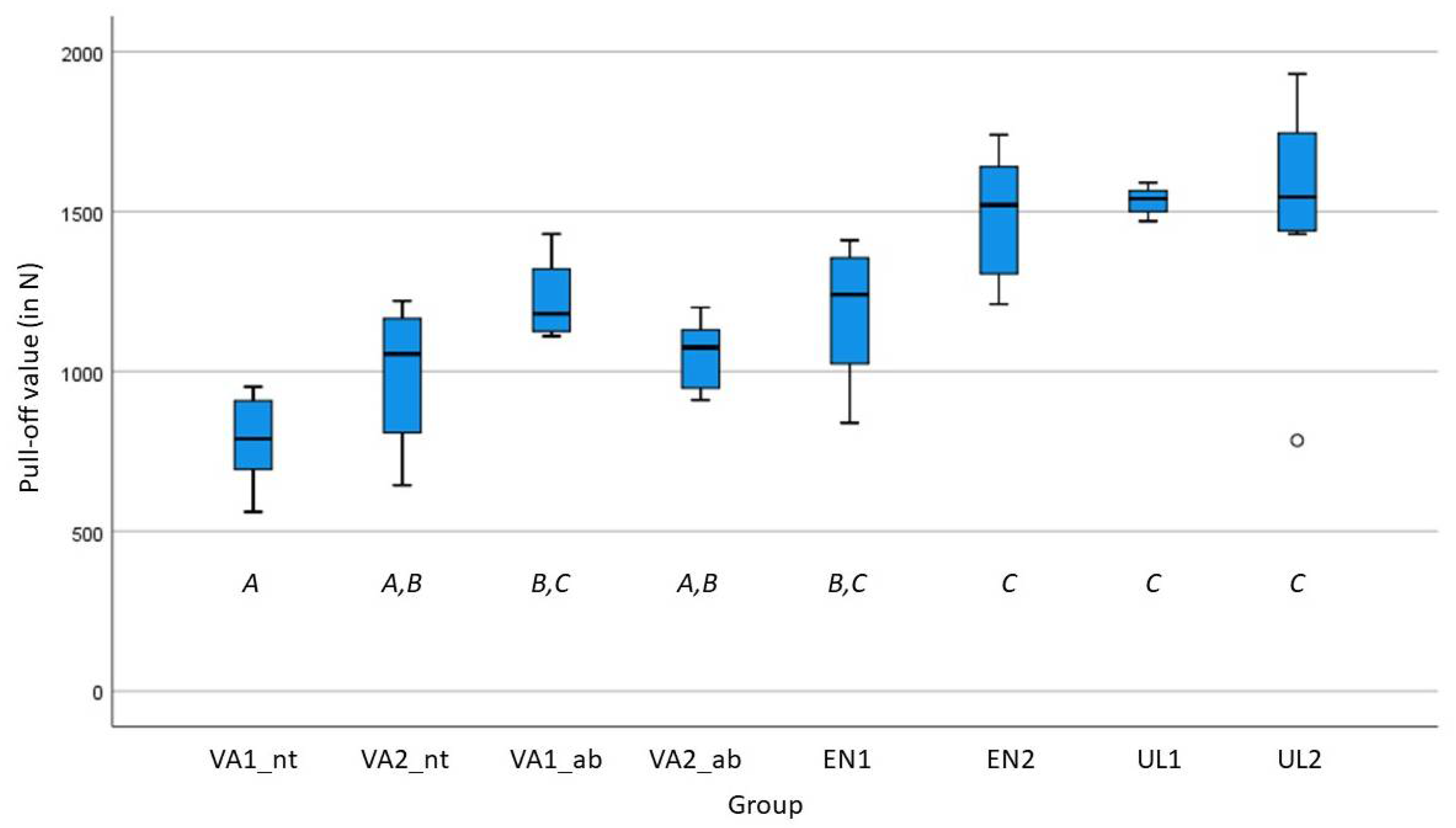
3. Results
4. Discussion
5. Conclusions
- Artificial aging does not seem to influence the pull-off forces for adhesively luted crowns of VA, EN, and UL.
- Uniform failure modes could not be detected in any of the test groups. Nevertheless, pull-off force values determined for all crown materials were within a high range and on comparable, probably clinically acceptable levels.
- Airborne-particle abrasion of the intaglio surfaces of the crowns made from VA did not result in significantly higher adhesion values. However, it is recommended to ensure the best possible conditions for bonding.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pillai, S.; Upadhyay, A.; Khayambashi, P.; Farooq, I.; Sabri, H.; Tarar, M.; Lee, K.T.; Harb, I.; Zhou, S.; Wang, Y.; et al. Dental 3D-Printing: Transferring Art from the Laboratories to the Clinics. Polymers 2021, 13, 157. [Google Scholar] [CrossRef] [PubMed]
- Schweiger, J.; Edelhoff, D.; Güth, J.F. 3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. J. Clin. Med. 2021, 10, 2010. [Google Scholar] [CrossRef] [PubMed]
- Schweiger, J.; Güth, J.F.; Edelhoff, D.; Seidel, K.; Graf, T. Application of 3D-printed colored 3D-models for the fabrication of full ceramic restorations: A technical report. J. Esthet. Restor. Dent. 2022, 34, 235–243. [Google Scholar] [CrossRef] [PubMed]
- VarseoSmile Crown Plus—The Ceramic Filled Hybrid Material for 3D Printing of Permanent Restorations. Available online: https://www.bego.com/3d-printing/materials/varseosmile-crown-plus/ (accessed on 15 May 2022).
- Spitznagel, F.A.; Boldt, J.; Gierthmuehlen, P.C. CAD/CAM Ceramic Restorative Materials for Natural Teeth. J. Dent. Res. 2018, 97, 1082–1091. [Google Scholar] [CrossRef]
- Spitznagel, F.A.; Scholz, K.J.; Strub, J.R.; Vach, K.; Gierthmuehlen, P.C. Polymer-infiltrated ceramic CAD/CAM inlays and partial coverage restorations: 3-year results of a prospective clinical study over 5 years. Clin. Oral Investig. 2018, 22, 1973–1983. [Google Scholar] [CrossRef]
- Spitznagel, F.A.; Scholz, K.J.; Vach, K.; Gierthmuehlen, P.C. Monolithic Polymer-Infiltrated Ceramic Network CAD/CAM Single Crowns: Three-Year Mid-Term Results of a Prospective Clinical Study. Int. J. Prosthodont. 2020, 33, 160–168. [Google Scholar] [CrossRef]
- Fathy, H.; Hamama, H.H.; El-Wassefy, N.; Mahmoud, S.H. Clinical performance of resin-matrix ceramic partial coverage restorations: A systematic review. Clin. Oral Investig. 2022, 26, 3807–3822. [Google Scholar] [CrossRef]
- Kabetani, T.; Ban, S.; Mine, A.; Ishihara, T.; Nakatani, H.; Yumitate, M.; Yamanaka, A.; Ishida, M.; Matsumoto, M.; Van Meerbeek, B.; et al. Four-year clinical evaluation of CAD/CAM indirect resin composite premolar crowns using 3D digital data: Discovering the causes of debonding. J. Prosthodont. Res. 2022, 66, 402–408. [Google Scholar] [CrossRef]
- Sulaiman, T.A. Materials in digital dentistry-A review. J. Esthet. Restor. Dent. 2020, 32, 171–181. [Google Scholar] [CrossRef]
- Edelhoff, D.; Ozcan, M. To what extent does the longevity of fixed dental prostheses depend on the function of the cement? Working Group 4 materials: Cementation. Clin. Oral Implant. Res. 2007, 18, 193–204. [Google Scholar] [CrossRef]
- Frankenberger, R.; Hartmann, V.E.; Krech, M.; Krämer, N.; Reich, S.; Braun, A.; Roggendorf, M. Adhesive luting of new CAD/CAM materials. Int. J. Comput. Dent. 2015, 18, 9–20. [Google Scholar]
- Reymus, M.; Roos, M.; Eichberger, M.; Edelhoff, D.; Hickel, R.; Stawarczyk, B. Bonding to new CAD/CAM resin composites: Influence of air abrasion and conditioning agents as pretreatment strategy. Clin. Oral Investig. 2019, 23, 529–538. [Google Scholar] [CrossRef] [PubMed]
- Peumans, M.; Valjakova, E.B.; De Munck, J.; Mishevska, C.B.; Van Meerbeek, B. Bonding Effectiveness of Luting Composites to Different CAD/CAM Materials. J. Adhes. Dent. 2016, 18, 289–302. [Google Scholar] [CrossRef] [PubMed]
- Shembish, F.A.; Tong, H.; Kaizer, M.; Janal, M.N.; Thompson, V.P.; Opdam, N.J.; Zhang, Y. Fatigue resistance of CAD/CAM resin composite molar crowns. Dent. Mater. 2016, 32, 499–509. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, T.; Schmid, I.; Locher, M.; Addison, O. Extraction force and its determinants for minimally invasive vertical tooth extraction. J. Mech. Behav. Biomed. Mater. 2020, 105, 103711. [Google Scholar] [CrossRef] [PubMed]
- Tsujimoto, A.; Shimatani, Y.; Nojiri, K.; Barkmeier, W.W.; Markham, M.D.; Takamizawa, T.; Latta, M.A.; Miyazaki, M. Influence of surface wetness on bonding effectiveness of universal adhesives in etch-and-rinse mode. Eur. J. Oral Sci. 2019, 127, 162–169. [Google Scholar] [CrossRef]
- Graf, T.; Schweiger, J.; Güth, J.-F.; Sciuk, T.; Schubert, O.; Erdelt, K.-J. Arithmetic Relationship between Fracture Load and Material Thickness of Resin-Based CAD-CAM Restorative Materials. Polymers 2021, 14, 58. [Google Scholar] [CrossRef]
- Adebayo, O.A.; Burrow, M.F.; Tyas, M.J. Bond strength test: Role of operator skill. Aust. Dent. J. 2008, 53, 145–150. [Google Scholar] [CrossRef]
- Grzebieluch, W.; Będziński, R.; Czapliński, T.; Kaczmarek, U. The mechanical properties of human dentin for 3-D finite element modeling: Numerical and analytical evaluation. Adv. Clin. Exp. Med. Off. Organ Wroc. Med Univ. 2017, 26, 645–653. [Google Scholar] [CrossRef]
- Lin, J.; Shinya, A.; Gomi, H.; Shinya, A. Bonding of self-adhesive resin cements to enamel using different surface treatments: Bond strength and etching pattern evaluations. Dent. Mater. J. 2010, 29, 425–432. [Google Scholar] [CrossRef][Green Version]
- Buonocore, M.G. A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J. Dent. Res. 1955, 34, 849–853. [Google Scholar] [CrossRef]
- Capa, N.; Say, E.C.; Celebi, C.; Casur, A. Microtensile bond strengths of adhesively bonded polymer-based CAD/CAM materials to dentin. Dent. Mater. J. 2019, 38, 75–85. [Google Scholar] [CrossRef]
- Mine, A.; Kabetani, T.; Kawaguchi-Uemura, A.; Higashi, M.; Tajiri, Y.; Hagino, R.; Imai, D.; Yumitate, M.; Ban, S.; Matsumoto, M.; et al. Effectiveness of current adhesive systems when bonding to CAD/CAM indirect resin materials: A review of 32 publications. Jpn. Dent. Sci. Rev. 2019, 55, 41–50. [Google Scholar] [CrossRef]
- Soares, C.J.; Soares, P.V.; Pereira, J.C.; Fonseca, R.B. Surface treatment protocols in the cementation process of ceramic and laboratory-processed composite restorations: A literature review. J. Esthet. Restor. Dent. 2005, 17, 224–235. [Google Scholar] [CrossRef]
- Miranda, J.S.; Monteiro, J.B.; Silva, P.N.F.; Valera, M.C.; Bresciani, E.; Melo, R.M. Can different etching protocols change the properties of a hybrid ceramic? Gen. Dent. 2020, 68, 20–25. [Google Scholar]
- May, M.M.; Fraga, S.; May, L.G. Effect of milling, fitting adjustments, and hydrofluoric acid etching on the strength and roughness of CAD-CAM glass-ceramics: A systematic review and meta-analysis. J. Prosthet. Dent. 2021. online ahead of print. [Google Scholar] [CrossRef]
- Yadav, R.; Kumar, M. Dental restorative composite materials: A review. J. Oral Biosci. 2019, 61, 78–83. [Google Scholar] [CrossRef]
- Rosentritt, M.; Ilie, N.; Lohbauer, U. Werkstoffkunde in der Zahnmedizin, 1st ed.; Thieme: Stuttgart, Germany, 2018; Volume 1, p. 480. [Google Scholar]
- Wedekind, L.; Güth, J.F.; Schweiger, J.; Kollmuss, M.; Reichl, F.X.; Edelhoff, D.; Högg, C. Elution behavior of a 3D-printed, milled and conventional resin-based occlusal splint material. Dent. Mater. 2021, 37, 701–710. [Google Scholar] [CrossRef]
- Heintze, S.D. Crown pull-off test (crown retention test) to evaluate the bonding effectiveness of luting agents. Dent. Mater. 2010, 26, 193–206. [Google Scholar] [CrossRef]
- Muhlemann, S.; Truninger, T.C.; Stawarczyk, B.; Hammerle, C.H.; Sailer, I. Bending moments of zirconia and titanium implant abutments supporting all-ceramic crowns after aging. Clin. Oral Implant. Res. 2014, 25, 74–81. [Google Scholar] [CrossRef]
- Truninger, T.C.; Stawarczyk, B.; Leutert, C.R.; Sailer, T.R.; Hammerle, C.H.; Sailer, I. Bending moments of zirconia and titanium abutments with internal and external implant-abutment connections after aging and chewing simulation. Clin. Oral Implant. Res. 2012, 23, 12–18. [Google Scholar] [CrossRef]
- DeLong, R.; Sakaguchi, R.L.; Douglas, W.H.; Pintado, M.R. The wear of dental amalgam in an artificial mouth: A clinical correlation. Dent. Mater. 1985, 1, 238–242. [Google Scholar] [CrossRef]




| Code | Crown Material | Material Type (Monolithic) | Process | Manufacture | Treatment of Restorative Material | Artificial Aging | Flexural Strength [MPa] |
|---|---|---|---|---|---|---|---|
| VA1_ab | VarseoSmile Crown plus | 3D-printed hybrid composite | Additive (3D-printed) | BEGO, Bremen, Germany | 50 μm, Al2O3, 1.5 bar, Monobond Plus | No | 116 a |
| VA2_ab | VarseoSmile Crown plus | 3D-printed hybrid composite | Additive (3D-printed) | BEGO, Bremen, Germany | 50 μm, Al2O3, 1.5 bar, Monobond Plus | Yes | 116 a |
| VA1_nt | VarseoSmile Crown plus | 3D-printed hybrid composite | Additive (3D-printed) | BEGO, Bremen, Germany | Monobond Plus | No | 116 a |
| VA2_nt | VarseoSmile Crown plus | 3D-printed hybrid composite | Additive (3D-printed) | BEGO, Bremen, Germany | Monobond Plus | Yes | 116 a |
| EN1 | Enamic | Hybrid ceramic: polymer-infiltrated ceramic networks (PICN) | Subtractive (milled) | VITA Zahnfabrik, Bad Säckingen, Germany, Germany | 60 s HF, Espe Sil | No | 150–160 a |
| EN2 | Enamic | Hybrid ceramic: polymer-infiltrated ceramic networks (PICN) | Subtractive (milled) | VITA Zahnfabrik, Bad Säckingen, Germany, Germany | 60 s HF, Espe Sil | Yes | 150–160 a |
| UL1 | Lava Ultimate | Resin nano ceramic or resin-based composite | Subtractive (milled) | 3M Deutschland GmbH, Neuss, Germany | 50 μm, Al2O3, 1.5 bar, Scotchbond Universal Adhesive | No | 191 [15] |
| UL2 | Lava Ultimate | Resin nano ceramic or resin-based composite | Subtractive (milled) | 3M Deutschland GmbH, Neuss, Germany | 50 μm, Al2O3, 1.5 bar, Scotchbond Universal Adhesive | Yes | 191 [15] |
| Code | VA1_ab | VA2_ab | VA1_nt | VA2_nt | EN1 | EN2 | UL1 | UL2 |
|---|---|---|---|---|---|---|---|---|
| Pull-off forces | ||||||||
| Arithmetic average [N] | 1223.8 | 1051.9 | 786.6 | 988.6 | 1185.9 | 1485.0 | 1533.8 | 1521.8 |
| Standard deviation [N] | 119.2 | 107.2 | 137.6 | 212.1 | 211.8 | 198.2 | 42.4 | 343.4 |
| Maximum [N] | 1430.0 | 1200.0 | 952.0 | 1220.0 | 1410.0 | 1740.0 | 1590.0 | 1930.0 |
| Minimum [N] | 1110.0 | 910.0 | 561.0 | 644.0 | 839.0 | 1210.0 | 1470.0 | 784.0 |
| ANOVA Scheffè method (post hoc test) | ||||||||
| Subgroup for alpha = 0.05 | B, C | A, B | A | A, B | B, C | C | C | C |
| Failure mode | ||||||||
| #1 | 0 | 0 | 4 | 0 | 1 | 0 | 0 | 0 |
| #2 | 4 | 5 | 4 | 5 | 4 | 2 | 0 | 1 |
| #3 | 1 | 3 | 0 | 3 | 0 | 0 | 4 | 1 |
| #4 | 3 | 0 | 0 | 0 | 3 | 6 | 4 | 6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Graf, T.; Erdelt, K.-J.; Güth, J.-F.; Edelhoff, D.; Schubert, O.; Schweiger, J. Influence of Pre-Treatment and Artificial Aging on the Retention of 3D-Printed Permanent Composite Crowns. Biomedicines 2022, 10, 2186. https://doi.org/10.3390/biomedicines10092186
Graf T, Erdelt K-J, Güth J-F, Edelhoff D, Schubert O, Schweiger J. Influence of Pre-Treatment and Artificial Aging on the Retention of 3D-Printed Permanent Composite Crowns. Biomedicines. 2022; 10(9):2186. https://doi.org/10.3390/biomedicines10092186
Chicago/Turabian StyleGraf, Tobias, Kurt-Jürgen Erdelt, Jan-Frederik Güth, Daniel Edelhoff, Oliver Schubert, and Josef Schweiger. 2022. "Influence of Pre-Treatment and Artificial Aging on the Retention of 3D-Printed Permanent Composite Crowns" Biomedicines 10, no. 9: 2186. https://doi.org/10.3390/biomedicines10092186
APA StyleGraf, T., Erdelt, K.-J., Güth, J.-F., Edelhoff, D., Schubert, O., & Schweiger, J. (2022). Influence of Pre-Treatment and Artificial Aging on the Retention of 3D-Printed Permanent Composite Crowns. Biomedicines, 10(9), 2186. https://doi.org/10.3390/biomedicines10092186






