Psychosocial Factors Related to Stroke Patients’ Rehabilitation Motivation: A Scoping Review and Meta-Analysis Focused on South Korea
Abstract
:1. Introduction
2. Methods and Analysis
2.1. Stage 1. Identifying the Research Question
2.2. Stage 2. Identifying Relevant Studies (Information Sources)
Search
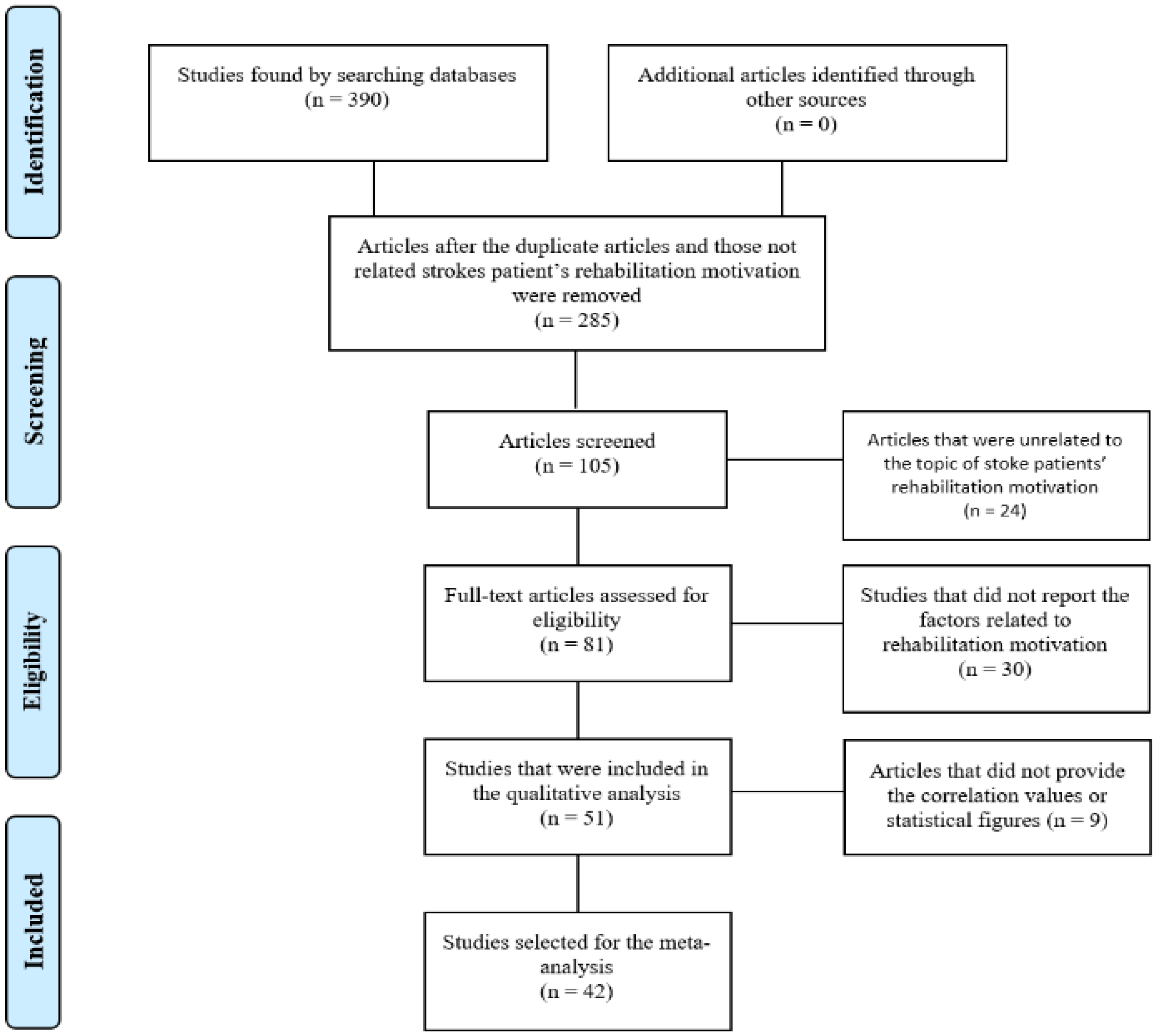
2.3. Stage 3. Study Selection
2.4. Stage 4. Data Charting Process
2.5. Synthesis of Scoping Review Results
2.6. Meta-Analysis
2.6.1. Data Coding and Categorization Criteria
2.6.2. Data Analysis and Effect Size Estimation
2.7. Ethics and Dissementation
3. Results
3.1. Synthesizing the Scoping Review’s Results
3.1.1. Year
3.1.2. Academic Paper and Thesis
3.1.3. Field
3.1.4. Study Design and Program
3.1.5. Factors Related to Rehabilitation Motivation
3.2. Meta-Analysis Result
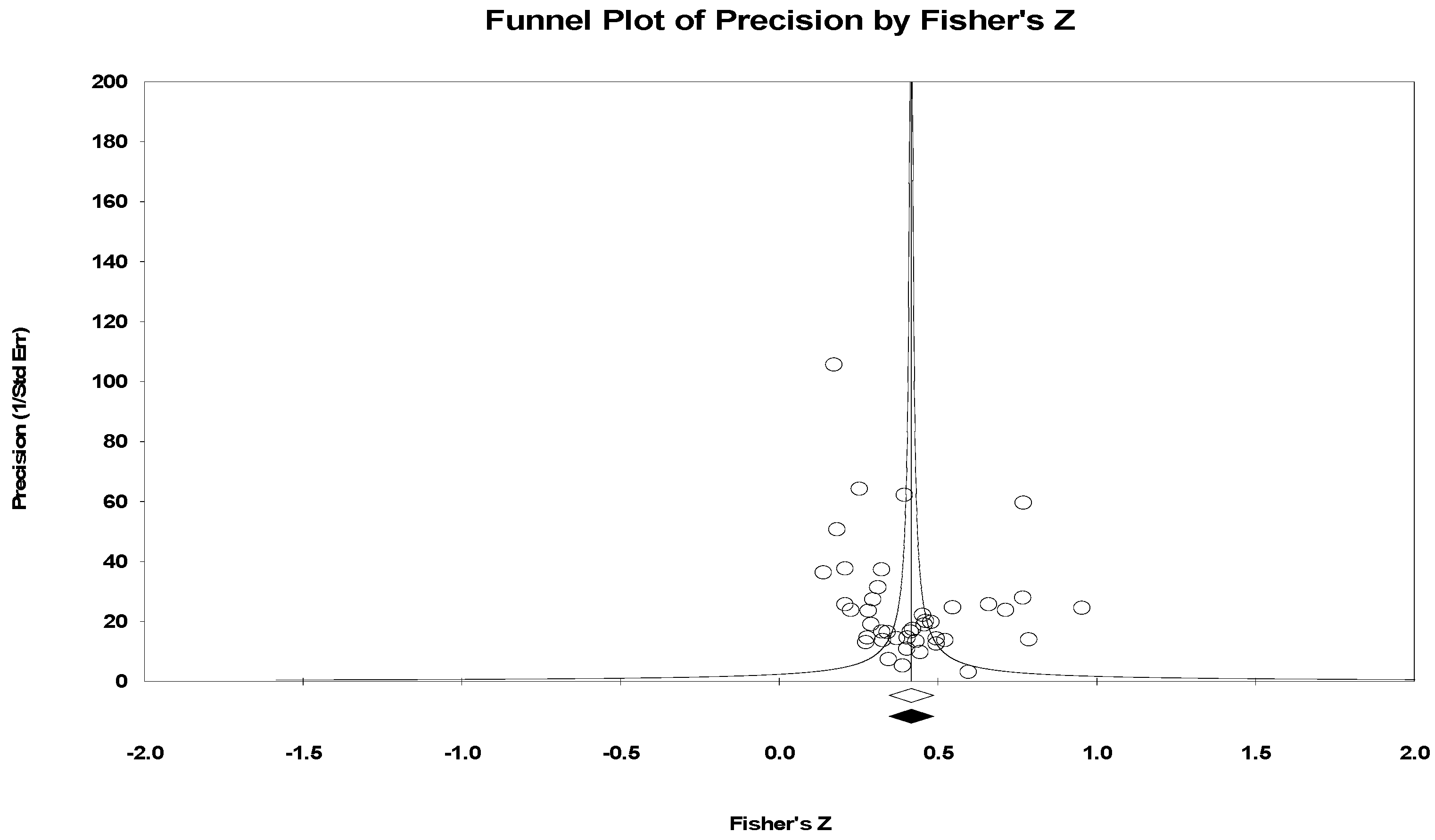
3.2.1. Publication Bias
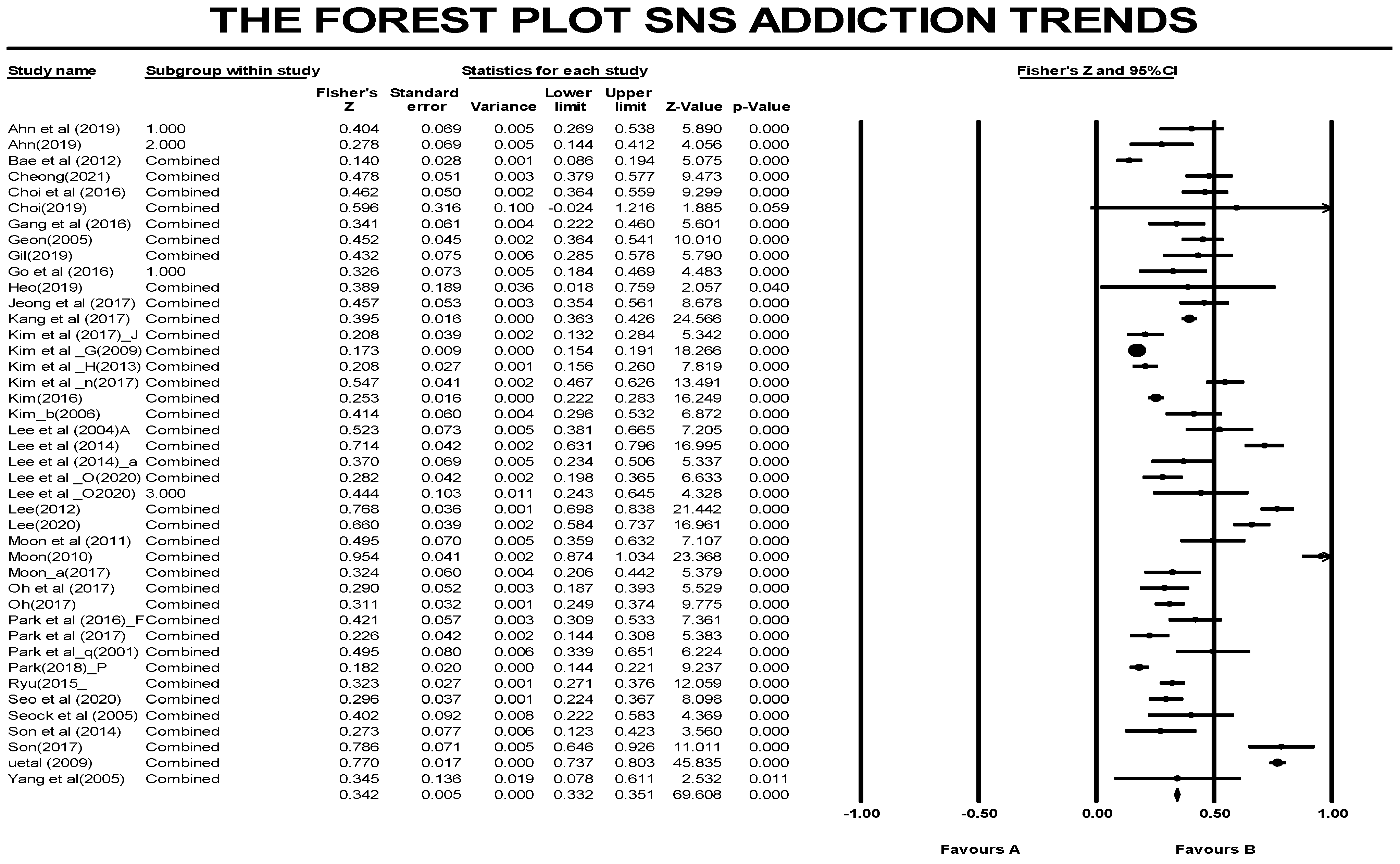
3.2.2. Overall Effect Size of the Variables Related to Rehabilitation Motivation
3.2.3. Effect Size of Each Factor Related to Rehabilitation Motivation (Internal, Psychological, Physical, Environmental, Risk or Protective Factor)
3.2.4. Analysis of the Internal and External Factors’ Sub-Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Waqas, M.; Rai, A.T.; Vakharia, K.; Chin, F.; Siddiqui, A.H. Effect of definition and methods on estimates of prevalence of large vessel occlusion in acute ischemic stroke: A systematic review and meta-analysis. J. NeuroIntervent. Surg. 2020, 12, 260–265. [Google Scholar] [CrossRef]
- Moon, S.R.; Keum, D.H. Effects of the western-oriental medicine joint rehabilitation on the daily activities and cognitive functions in stroke patients. J. Korean Med. 2020, 30, 2. [Google Scholar]
- Donkel, S.J.; Pater, K.; Leebeek, F.W.G.; Dippel, D.W.J.; Cate, H.T.; de Maat, M.P.M. Thrombin generation is associated with ischemic stroke at a young age. Thromb. Res. 2021, 202, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.J. Policy directions and tasks for the 4th public health plan: A focus on health habits and chronic disease management. Public Health Care Forum. 2017, 1, 6–21. [Google Scholar]
- Ha, J.-Y.; Park, H.-S.; Lee, S.-J.; Jeon, J.-H.; Jo, H.-Y.; Jee, Y.-J. A study on the recovery experience of young and middle-aged stroke patients. J. Adult Nurs. 2010, 22, 342–351. [Google Scholar]
- Lee, G.S.; Bae, H.J.; Kim, H.S. Resource and cost expenditure regarding stroke patients: From the patients’ perspectives. J. Korean Neurol. Assoc. 2004, 22, 583–589. [Google Scholar]
- Oh, S.Y.; Hwang, S.Y. Relationship Between depression and rehabilitation motivation in middle-aged stroke patients: A focus on the mediating effects of resilience. J. Korea Acad. Ind. Coop. Soc. 2017, 18, 58–66. [Google Scholar]
- Bae, J.H.; Lee, T.Y.; Kang, D.H. Effects of pain catastrophizing and rehabilitation motivation on the activities of daily living in stroke patients. J. Korean Soc. Occup. Ther. 2012, 20, 57–68. [Google Scholar]
- Kim, J.H.; Kim, H.; Park, J.W. Correlation analysis of the psychosocial factors and therapeutic immersion in stroke patients. J. Digit. Converg. 2017, 15, 253–262. [Google Scholar]
- Jeong, H.G.; Moon, S.M. Effects of social support on the rehabilitation motivation in stroke patients: A focus on the mediating effects of uncertainty. J. Adult Nurs. 2017, 29, 323–331. [Google Scholar] [CrossRef]
- Moo-Sik, L.; Kyeong-Soo, L.; Jung-Jeung, L.; Tae-Yoon, H.; Jin-Yong, L.; Weon-Seob, Y.; Keon-Yeop, K.; Sang-Kyu, K.; Jong-Yeon, K.; Ki-Soo, P.; et al. Directions and current issues on the policy of prevention and management for hypertension and diabetes, and development of chronic disease prevention and management model in Korea. J. Agric. Med. Community Health 2020, 45, 13–40. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Armstrong, R.; Hall, B.J.; Doyle, J.; Waters, E. ‘Scoping the scope’ of a Cochrane Review. J. Public Health 2011, 33, 147–150. [Google Scholar] [CrossRef]
- Borenstein, M.; Cooper, H.; Hedges, L.; Valentine, J. Effect sizes for continuous data. Handb. Res. Synth. Meta-Anal. 2009, 2, 221–235. [Google Scholar]
- Kim, D.H.; Oh, M.H.; Park, G.A.; Baek, H.H. Effects of the activities of daily living and self-esteem in stroke patients on the care burden of the carer. J. Rehabil. Res. 2014, 18, 247–266. [Google Scholar]
- Lee, J.M.; Ryu, S.H.; Choi, H. A study on the rehabilitation motivation and stress in stroke patients based on behavior types. J. Korean Soc. Cogn. Rehabil. 2014, 3, 25–40. [Google Scholar] [CrossRef]
- Seo, M.Y.; Yang, J.H. The rehabilitation motivation and related factors in veteran stroke patients. J. Fundam. Nurs. 2020, 27, 215–225. [Google Scholar] [CrossRef]
- Sohn, Y.S.; Lee, S.; Kim, J.Y.; Lee, A.G. Analysis of the depression, rehabilitation motivation, quality of life, and interpersonal caring in stroke patients in relation to horticultural preference. J. People Plants Environ. 2014, 123, 16. [Google Scholar]
- Ahn, E.S.; Seo, S.R.; Kim, E.H. Effects of self-esteem and rehabilitation motivation on the quality of life in stroke patients during rehabilitation. J. Korea Acad. Ind. Coop. Soc. 2019, 20, 176–187. [Google Scholar]
- Moon, J.Y.; Cho, B.H. Relationship among perceived stress, social support, and rehabilitation motivation in stroke patients. Korean J. Rehabil. Nurs. 2011, 14, 24–31. [Google Scholar]
- Lee, J.Y.; Kim, H.S. Effects of social support, self-esteem, and rehabilitation motivation on the activities of daily living in stroke patients. J. East. West. Nurs. Res. 2014, 20, 145–153. [Google Scholar] [CrossRef]
- Choi, E.S.; Lee, E.N.; Cho, J.R. Mediating effects of resilience in the relationship between depression and rehabilitation motivation in stroke patients. J. Korean Soc. Muscle Jt. Health 2016, 23, 19–27. [Google Scholar] [CrossRef]
- Park, A.S.; Ko, E.; Kang, H.S. Comparison of Motivation for Rehabilitation, Family Support and Adherence to Rehabilitation between Depressive and Non-Depressive Stroke Patients’. Korean J. Rehabil. Nurs. 2016, 19, 138–147. [Google Scholar] [CrossRef] [Green Version]
- Kang, H.J.; Kwon, S.H.; Youn, S.C. The Convergent Influence of Perceived Stress and the Empowerment on Rehabilitation Motive of Stroke Patients. J. Digit. Converg. 2016, 14, 291–303. [Google Scholar] [CrossRef] [Green Version]
- Choi, M.G. Effects of a tool-based daily activity program on the self-efficacy, rehabilitation motivation, and social support in stroke patients during recovery. J. Korean Soc. Integr. Med. 2019, 7, 11–19. [Google Scholar]
- Park, A.S.; Eun, K. Influences of Rehabilitation Motivation, Self-Efficacy and Family Support on Rehabilitation Adherence in Stroke Patients. JKBNS 2017, 19, 113–122. [Google Scholar]
- Kang, G.Y. Effects of an observed action gait training on the visuospatial parameters and rehabilitation motivation in stroke patients. J. Korean Soc. Phys. Med. 2013, 8, 351–360. [Google Scholar] [CrossRef]
- Lee, M.H.; Oh, S.Y. Mediating effects of self-efficacy in the relationship between depression and rehabilitation motivation in stroke patients. J. Humanit. Soc. Sci. 2020, 21, 927–939. [Google Scholar]
- Kang, M.S.; Hong, G.H.; Jeong, H.R. relationship among the sleep quality, stress, and rehabilitation motivation in stroke patients. J. Korean Soc. Occup. Ther. 2017, 25, 59–70. [Google Scholar] [CrossRef]
- Ko, E.; Kim, H.Y. The depression, self-efficacy, and rehabilitation motivation in stroke patients at a rehabilitation ward. Conf. Korean Soc. Adult Nurs. 2016, 6, 176. [Google Scholar]
- Jeong, E.J.; Lee, B.H. A study of the rehabilitation motivation, gait ability, and quality of life in stroke patients. J. Korean Soc. Exerc. Rehabil. 2012, 8, 19–26. [Google Scholar]
- Park, J.W.; Kim, S.; Lee, B. The Moderator Effect of Rehabilitation Motivation on Physical Function, Balance, and Cognition of Stroke Patients. JKPTS 2020, 27, 13–24. [Google Scholar] [CrossRef]
- Song, Y.J. Effects of Photographic Presentation on the Rehabilitation Motivation and Motor Functions in Stroke Patients with Hemiplegia. Ph.D. Thesis, Chosun University Graduate School of Public Health Care, Gwangju, Korea, 2011. [Google Scholar]
- Moon, J.H.; Park, J.H.; Kim, Y.S.; Park, I.H. Effects of a goal-oriented activity based on art therapy on the hand functions, daily activities, depression, and rehabilitation motivation in acute stroke patients: A pilot study. J. Korean Soc. Neurocogn. Rehabil. 2018, 10, 15–24. [Google Scholar]
- Park, S.J.; Song, S.I. Effects of the time-use intervention on the depression and rehabilitation motivation in stroke patients. J. Korean Soc. Occup. Ther. 2015, 23, 25–37. [Google Scholar]
- Song, S.I.; Lee, J.M.; Jeong, J.H. Effects of a task-oriented activity on the self-efficacy and rehabilitation motivation in stroke patients. J. Spec. Educ. Rehabil. Sci. 2015, 54, 303–321. [Google Scholar] [CrossRef]
- Kwon, H.K.; Lee, S.J. The Effect of a Movie-Based Nursing Intervention Program on Rehabilitation Motivation and Depression in Stroke Patients. J. Korean Acad. Nurs. 2017, 47, 345–356. [Google Scholar] [CrossRef] [Green Version]
- Cha, S.; Kim, H.; Lee, J.; Lim, N.; Cho, H.; Hwang, H. The Effect of Self-Administered Check Program on Rehabilitative Motivation and Functional Recovery of Stroke Patients. Korean Aging Frendly Ind. Assoc. 2020, 12, 75–83. [Google Scholar] [CrossRef]
- Jung, Y.R. Effects of a discussion of lyrics on the depression and rehabilitation motivation in stroke patients. J. Music Hum. Behav. 2015, 12, 43–64. [Google Scholar]
- Song, S.; Lee, J.M. Effects of a game program on the depression, self-efficacy, and rehabilitation motivation in stroke patients. J. Spec. Educ. Rehabil. Sci. 2014, 53, 133–153. [Google Scholar] [CrossRef]
- Park, S.I. The Effect of the Social Re-Adjustment Program for Stroke Survivors. AJMAHS 2017, 7, 399–408. [Google Scholar] [CrossRef] [Green Version]
- Park, S.I.; Seo, E.H.; Cho, B.H. Effects of the tai-chi exercise program on the upper limb function, functional independence, and rehabilitation motivation in stroke patients in a care facility. J. Korean Soc. Exerc. Rehabil. 2012, 8, 115–124. [Google Scholar]
- Hahm, Y.J. Effects of a cognition rehabilitation training using a smart rehabilitation system on the cognition, depression, and rehabilitation motivation in stroke patients with mild cognitive impairment. Korea J. Geriatr. Occup. Ther. 2020, 2, 7–16. [Google Scholar]
- Jheon, S.H. Effects of a Rehabilitation Motivation Enhancing Nursing Intervention on the Social Readjustment of Elderly Stroke Patients with Hemiplegia. Master’s Thesis, Korea University Graduate School of Education, Seoul, Korea, 2013. [Google Scholar]
- Park, C.S. Effects of a VR-Based Robot-Assisted Gait Training on the Balance, Fall Efficacy, and Rehabilitation Motivation in Stroke Patients. Master’s Thesis, Nambu University Graduate School, Gwangju, Korea, 2018. [Google Scholar]
- Choi, H.S. Effects of a VR-Based Rehabilitation Training on the Self-Efficacy and Rehabilitation Motivation in Stroke Patients. Master’s Thesis, Inje University Graduate School of Public Health Care, Gimhae-si, Korea, 2016. [Google Scholar]
- Jeong, B.C. Effects of a Pelvic Exercise Using Visual Feedback on the Balance, Gait, Activities of Daily Living, Rehabilitation Motivation, and Quality of Life in Stroke Patients. Ph.D. Thesis, Namseoul University, Cheonan-si, Korea, 2019. [Google Scholar]
- Hyun, D.S. Effects of Group Art Therapy on the Psychological Rehabilitation of Elderly Stroke Patients. Master’s Thesis, Jeju National University Graduate School of Education, Jeju-do, Korea, 2012. [Google Scholar]
- Cho, S.T. Effects of an Early Robot-Assisted Gait Training on the Functional Recovery, Self-Efficacy, and Rehabilitation Motivation in Acute Stroke Patients. Master’s Thesis, Sahmyook University Graduate School, Seoul, Korea, 2016. [Google Scholar]
- Gil, S.R. Effects of Rehabilitation Motivation on the Functional Performance in Stroke Patients. Master’s Thesis, Cheongju University, Cheongju-si, Korea, 2020. [Google Scholar]
- Lee, Y.J. Mediating Effects of Social Support and Self-Efficacy in the Relationship between Depression and Rehabilitation Motivation in Stroke Patients. Master’s Thesis, Kunsan National University Graduate School, Kunsan-si, Korea, 2020. [Google Scholar]
- Moon, G.J. Effects of Marital Intimacy and Depression on the Rehabilitation Motivation in Stroke Patients. Ph.D. Thesis, Hanyang University Graduate School, Seoul, Korea, 2017. [Google Scholar]
- Kim, Y. Effects of Depression, Disability Acceptance, and Social Support on the Rehabilitation Motivation in Stroke Patients with Hemiplegia. Master’s Thesis, Gyeongsang National University Graduate School, Jinju-si, Korea, 2016. [Google Scholar]
- Sohn, S.H. Correlations among the Quality of Life, Resilience, and Rehabilitation Motivation in Elderly Stroke Patients. Master’s Thesis, Catholic University of Pusan Graduate School, Busan, Korea, 2017. [Google Scholar]
- Oh, S.Y. A Predictive Model of Rehabilitation Motivation in Middle-Aged Stroke Patients during Rehabilitation. Ph.D. Thesis, Hanyang University Graduate School, Seoul, Korea, 2017. [Google Scholar]
- Ryu, S.H. Effects of a Virtual Reality Program on the Depression, Rehabilitation Motivation, and Work Participation of Stroke Patients. Master’s Thesis, Daegu University, Gyeongsan-si, Korea, 2015. [Google Scholar]
- Lee, J.A. Effects of Disability Acceptance and Social Support on the Rehabilitation Motivation in Stroke Patients. Master’s Thesis, Nambu University Graduate School, Gwangju, Korea, 2012. [Google Scholar]
- Jeong, H.N. Effects of Rehabilitation Motivation and Healthcare Providers Support on Self-Nursing of Stroke Patients during Rehabilitation. Master’s Thesis, Pukyong National University, Busan, Korea, 2021. [Google Scholar]
- Park, S.H. Factors Influencing the Rehabilitation Motivation in Stroke Patients. Master’s Thesis, Jeonbuk National University Graduate School, Jeonju-si, Korea, 2018. [Google Scholar]
- Heo, S.G. Effects of the Body Scan Training Based on Mindfulness on the Depression, Disability Acceptance, Rehabilitation Motivation in Stroke Patients. Master’s Thesis, Jeonbuk National University College of Administration, Jeonju-si, Korea, 2019. [Google Scholar]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hedges, L.V. Estimation of Effect Size from a Series of Independent Experiments. Psychol. Bull. 1982, 92, 490. [Google Scholar] [CrossRef]
- Rodriguez, B.L.; D’Agostino, R.; Abbott, R.D.; Kagan, A.; Burchfiel, C.M.; Yano, K.; Ross, G.W.; Silbershatz, H.; Higgins, M.W.; Popper, J.; et al. Risk of hospitalized stroke in men enrolled in the honolulu heart program and the framingham study: A comparison of incidence and risk factor effects. Stroke 2002, 33, 230–236. [Google Scholar] [CrossRef] [Green Version]
- Phipps, W.J.; Monahan, F.D. Phipps’ Medical-Surgical Nursing: Health and Illness Perspectives, 8th ed.; Mosby: Maryland Heights, MO, USA, 2007. [Google Scholar]
| Author (Year) | Article (Thesis) | Field | Study Design (Intervention Methods) | Factors Related to Rehabilitation Motivation |
|---|---|---|---|---|
| 1. Bae et al. (2012) [8] | Article | Occupational Therapy | Survey | Pain catastrophizing, activities of daily living |
| 2. Kim et al. (2013) [15] | Article | Occupational Therapy | Survey | Activities of daily living: ADL self-esteem |
| 3. Lee et al. (2014) [16] | Article | Occupational Therapy | Survey | (Heart type A)/stress |
| 4. Kim et al. (2017) [9] | Article | Occupational Therapy | Survey | Psychosocial factors (depression, stress, self-efficacy), therapeutic flow |
| 5. Seo et al. (2020) [17] | Article | Nursing | Survey | self-efficacy, social support (family support, friends support, healthcare providers support), depression |
| 6. Son et al. (2014) [18] | Article | Nursing/Rehabilitation | Survey | Interpersonal caring behavior, motivation of rehabilitation, QOL, horticultural therapy |
| 7. An et al. (2019) [19] | Article | Nursing | Survey | Self-Esteem, Stroke Specific Quality of Life |
| 8. Moon et al. (2011) [20] | Article | Nursing | Survey | Multidimensional Scale Perceived Social Support |
| 9. Lee et al. (2014) [21] | Article | Nursing | Survey | Self-esteem, rehabilitation motivation/self-efficacy, activities of daily living (ADL) |
| 10. Choi et al. (2016) [22] | Article | Nursing | Survey | Depression, rehabilitation motivation, resilience |
| 11. Park et al. (2016) [23] | Article | Nursing | Survey | Depression, rehabilitation motivation, family support, rehabilitation adherence |
| 12. Kang et al. (2016) [24] | Article | Nursing | Survey | Empowerment, rehabilitation motivation/self-efficacy, perceived stress |
| 13. Choi (2019) [25] | Article | Occupational Therapy | Observational Study (Program effectiveness) | General self-efficacy/rehabilitation motivation |
| 14. Park and Ko (2017) [26] | Article | Nursing | Survey | Rehabilitation adherence, rehabilitation motivation/self-efficacy |
| 15. Kang (2013) [27] | Article | Physical Therapy | Observational Study (Program effectiveness | Rehabilitation motivation/self-efficacy |
| 16. Lee et al. (2020) [28] | Article | Nursing | Survey | Depression, rehabilitation motivation/self-efficacy |
| 17. Kang et al. (2017) [29] | Article | Occupational Therapy | Survey | Sleep quality, stress, rehabilitation motivation |
| 18.Oh et al. (2017) [7] | Article | Nursing | Survey | Depression, rehabilitation motivation/self-efficacy, resilience |
| 19. Go et al. (2016) [30] | Article | Nursing | Survey | Rehabilitation motivation, depression, self-efficacy |
| 20. Jeong et al. (2017) [11] | Article | Nursing | Survey | Social support, uncertainty, rehabilitation motivation/self-efficacy |
| 21. Chung et al. (2012) [31] | Article | Physical Therapy | Survey | Rehabilitation motivation/self-efficacy, gait ability test, stroke specific quality of life |
| 22. Park et al. (2020) [32] | Article | Physical Therapy | Survey | Physical function, balance, cognition, rehabilitation motivation/self-efficacy |
| 23. Song et al. (2012) [33] | Article | Occupational Therapy | Observational Study (Program experiment) | Self-esteem, self-efficacy, family support, rehabilitation motivation, motor function |
| 24. Moon et al. (2018) [34] | Article | Occupational Therapy | Observational Study (Conventional program) | Hand function, modified Barthel index, depression scale, motivation questionnaire |
| 25. Park and Song (2015) [35] | Article | Occupational Therapy | Observational Study (Time-use intervention) | Depression, rehabilitation motivation/self-efficacy |
| 26. Song et al. (2015) [36] | Article | Occupational Therapy | Observational Study (Conventional program, Task-oriented activity) | Rehabilitation motivation, self-efficacy |
| 27. Kwon and Lee (2017) [37] | Article | Nursing | Observational Study (Movie-based nursing intervention) | Rehabilitation motivation/self-efficacy, depression |
| 28. Ca et al. (2020) [38] | Article | Occupational Therapy | Observational Study (Self-check program) | Rehabilitation motivation/self-efficacy, functional recovery |
| 29. Jung (2015) [39] | Article | Occupational Therapy | Observational Study (Discussion of lyrics) | Depression, rehabilitation motivation/self-efficacy |
| 30. Song et al. (2014) [40] | Article | Occupational Therapy | Observational Study (Game program) | Depression, self-efficacy, rehabilitation motivation |
| 31. Park (2017) [41] | Article | Occupational Therapy | Observational Study (Stepwise social readjustment program) | Upper limb function, shoulder pain, functional independence, rehabilitation motivation/self-efficacy, social readjustment, |
| 32. Park et al. (2012) [42] | Article | Occupational Therapy | Observational Study (Tai-chi exercise program) | Upper limb function, functional independence, rehabilitation motivation/self-efficacy |
| 33. Ham (2020) [43] | Article | Occupational Therapy | Observational Study (Cognitive rehabilitation program) | Depression |
| 34. Jeon (2013) [44] | Thesis (Master’s) | Nursing | Observational Study (Rehabilitation motivation enhancing nursing intervention) | Shoulder pain, depression, rehabilitation motivation/self-efficacy, social readjustment |
| 35. Park (2018) [45] | Thesis (Master’s) | Physical Therapy | Observational Study (Robot-assisted virtual reality program) | Rehabilitation motivation/self-efficacy, balance ability |
| 36. Choi (2016) [46] | Thesis (Master’s) | Public health | Observational Study (Traditional occupational therapy vs. virtual reality-based rehabilitation training) | Self-efficacy, rehabilitation motivation |
| 37. Park (2013) [44] | Thesis (Doctoral) | Rehabilitation | Observational Study (Image training based on mindfulness) | Cognition Scale for Older Adults |
| 38. Jung (2019) [47] | Thesis (Master’s) | Physical Therapy | Observational Study (Pelvic exercise using visual feedback) | Balance, gait, activities of daily living, rehabilitation motivation/self-efficacy, quality of life |
| 39. Hyun (2012) [48] | Thesis (Master’s) | Psychological and Counseling | Observational Study (Group art therapy) | Psychological rehabilitation (depression, self-esteem, rehabilitation motivation/self-efficacy) |
| 40. Cho (2016) [49] | Thesis (Master’s) | Physical Therapy | Observational Study (Robot-assisted gait training) | Balance test, gait ability test, self-efficacy and rehabilitation motivation tests |
| 41. GIL (2019) [50] | Thesis (Master’s) | Physical therapy | Survey | Rehabilitation motivation, self-efficacy, functional performance |
| 42. Lee (2020) [51] | Thesis (Master’s) | Nursing | Survey | Depression, social support, self-efficacy, rehabilitation motivation/self-efficacy |
| 43. Moon (2017) [52] | Thesis (Master’s) | Nursing | Survey | Marital intimacy, depression, rehabilitation motivation /self-efficacy |
| 44. Kim (2016) [53] | Thesis (Master’s) | Nursing | Survey | Rehabilitation motivation/self-efficacy, depression, disability acceptance, social support |
| 45. Son (2017) [54] | Thesis (Master’s) | Nursing | Survey | Quality of life, resilience, rehabilitation motivation |
| 46. Oh (2017) [55] | Thesis (Doctoral) | Nursing | Survey | Rehabilitation motivation, activities of daily living, social support (family support, healthcare providers support), depression, self-efficacy |
| 47. Ryu (2015) [56] | Thesis (Master’s) | Occupational Therapy | Observational Study (Program virtual reality) | Depression, rehabilitation motivation/self-efficacy, work participation |
| 48. Lee (2012) [57] | Thesis (Master’s) | Social welfare | Survey | Disability acceptance, social support, rehabilitation motivation/self-efficacy |
| 49. Jeong (2021) [58] | Thesis (Master’s) | Nursing | Survey | Rehabilitation motivation/self-efficacy, healthcare providers support, self-nursing |
| 50. Park (2018) [59] | Thesis (Master’s) | Nursing | Survey | Rehabilitation motivation, risk factor (stroke-related family history, medical history |
| 51.Heo(2018) [60] | Thesis (Master’s) | Psychology | Observational Study (Program effectiveness) | Depression, disability acceptance, rehabilitation motivation/self-efficacy |
| Studies Trimmed | ESZr | 95% CI | Q | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Observed | 0 | 0.42 | 0.35 | 0.49 | 1805.72 |
| Adjusted | 0 | 0.42 | 0.35 | 0.49 | 1805.72 |
| Random Effect Model | Heterogeneity | |||||||
|---|---|---|---|---|---|---|---|---|
| Division | K | n | ESZr | 95% CI | Q (df) | p | I2 | |
| Lower | Upper | |||||||
| Overall | 42 | 362 | 0.33 | 0.30 | 0.36 | 2716.47 (361) | 0.00 | 86.71 |
| Structural Factors | N | ESZr | 95% CI | SE | p | Q(d) | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Internal factor | 94 | 0.36 | 0.30 | 0.41 | 0.02 | 0.00 | |
| External factor | 264 | 0.32 | 0.28 | 0.35 | 0.01 | 0.00 | 1.73(1) |
| Physical factor | 100 | 0.31 | 0.27 | 0.35 | 0.02 | 0.00 | p = 0.189 |
| Psychological factor | 94 | 0.36 | 0.31 | 0.41 | 0.02 | 0.00 | 1.96(2) |
| Environmental factor | 164 | 0.32 | 0.28 | 0.36 | 0.02 | 0.00 | p = 0.375 |
| Risk factor | 251 | 0.34 | 0.30 | 0.37 | 0.02 | 0.00 | 6.41(1) * |
| Protective factor | 79 | 0.27 | 0.21 | 0.31 | 0.02 | 0.00 | p = 0.01 |
| Sub-Factor | N | ESZr | 95% CI | SE | p | Qb | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Social support (family support, healthcare providers support, peer support) | 32 | 0.52 | 0.42 | 0.61 | 0.05 | 0.00 | 54.79 (5) ** |
| Self-efficacy | 16 | 0.41 | 0.30 | 0.52 | 0.06 | 0.00 | |
| Volition | 42 | 0.34 | 0.28 | 0.40 | 0.03 | 0.00 | |
| Depression | 49 | 0.32 | 0.26 | 0.38 | 0.03 | 0.00 | |
| Quality of life | 96 | 0.27 | 0.22 | 0.32 | 0.03 | 0.00 | |
| Activities of daily living | 21 | 0.12 | 0.05 | 0.20 | 0.04 | 0.00 | |
| Overall | 286 | 0.32 | 0.30 | 0.35 | 0.01 | 0.00 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheong, M.J.; Kang, Y.; Kang, H.W. Psychosocial Factors Related to Stroke Patients’ Rehabilitation Motivation: A Scoping Review and Meta-Analysis Focused on South Korea. Healthcare 2021, 9, 1211. https://doi.org/10.3390/healthcare9091211
Cheong MJ, Kang Y, Kang HW. Psychosocial Factors Related to Stroke Patients’ Rehabilitation Motivation: A Scoping Review and Meta-Analysis Focused on South Korea. Healthcare. 2021; 9(9):1211. https://doi.org/10.3390/healthcare9091211
Chicago/Turabian StyleCheong, Moon Joo, Yeonseok Kang, and Hyung Won Kang. 2021. "Psychosocial Factors Related to Stroke Patients’ Rehabilitation Motivation: A Scoping Review and Meta-Analysis Focused on South Korea" Healthcare 9, no. 9: 1211. https://doi.org/10.3390/healthcare9091211
APA StyleCheong, M. J., Kang, Y., & Kang, H. W. (2021). Psychosocial Factors Related to Stroke Patients’ Rehabilitation Motivation: A Scoping Review and Meta-Analysis Focused on South Korea. Healthcare, 9(9), 1211. https://doi.org/10.3390/healthcare9091211





