Factors Associated with Burden in Caregivers of Patients with End-Stage Kidney Disease (A Systematic Review)
Abstract
1. Introduction
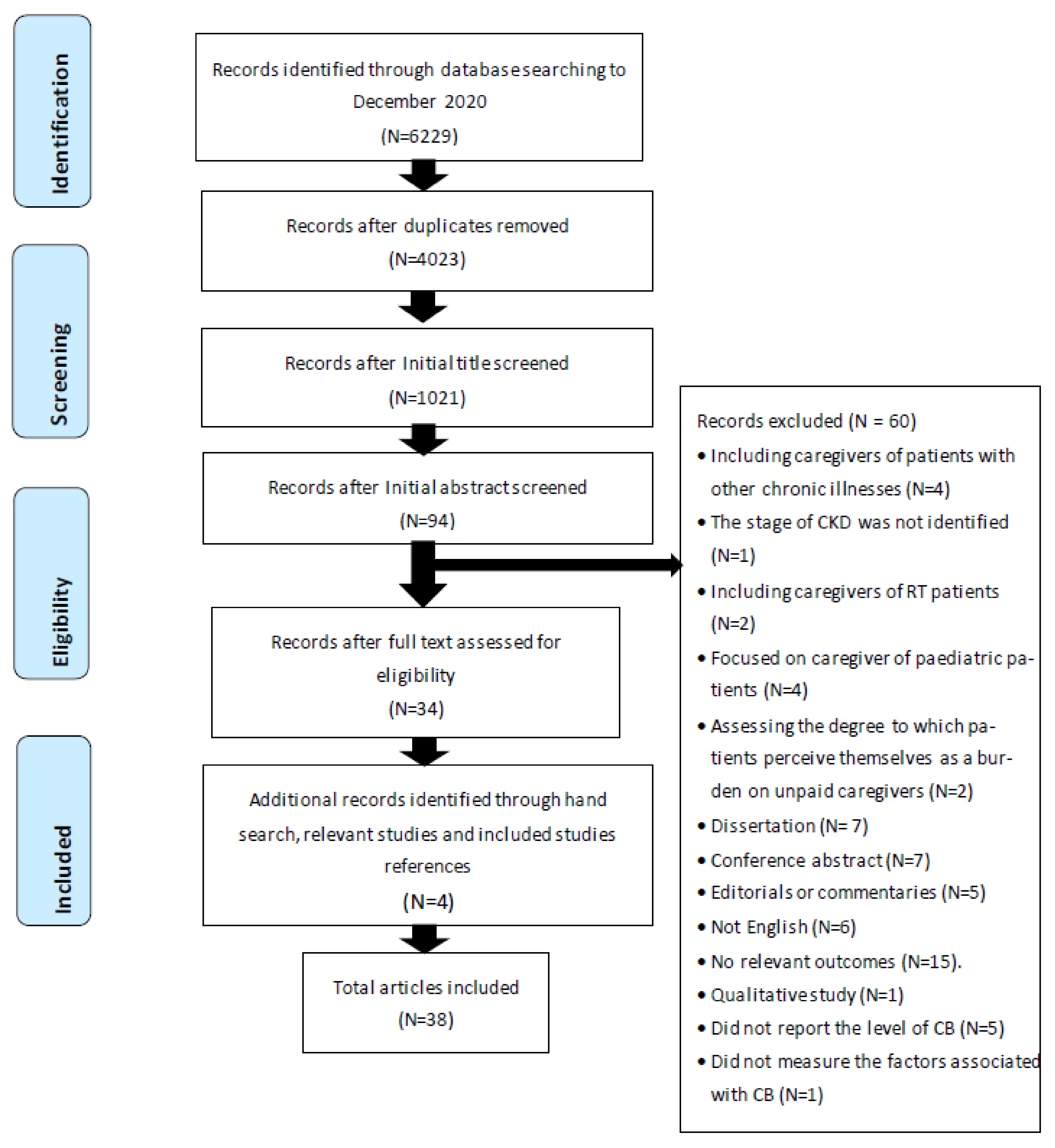
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
- Studies including informal caregivers of adult patients with ESKD, either undergoing dialysis or receiving supportive/palliative care.
- Studies measuring CB and the factors associated positively or negatively with CB. In all studies included in this review, caregiver burden was defined as the extent to which caregivers perceive their emotional or physical health, social life, and financial status as becoming worse because of caring for their relative [4] measured by burden-specific instruments such as the Zarit Burden Interview (ZBI).
- Studies examining informal caregiving of patients with renal transplant (RT) were excluded.
- Studies exploring informal caregiving of patients with early stages of CKD were excluded.
- Studies measuring CB in informal caregivers of patients with a range of chronic illnesses, which did not differentiate the burden experienced by informal caregivers of individuals with renal disease, were excluded.
- Studies published in English were included.
- No time limit was employed to exclude studies, to help maximise the number of studies included.
- Studies assessing the effectiveness of interventions in CB were excluded.
- Primary research studies were included.
- Reviews, conference abstracts, dissertations, editorials, or researcher opinions were excluded.
2.3. Selection of Studies
2.4. Data Extraction
2.5. Quality Assessment Tool
2.6. Data Analysis, Synthesis, and Presentation
3. Results
3.1. Characteristics of Included Studies
3.2. Level of CB
3.3. Factors Associated with CB
- Caregiver’s and patient’s socio-demographical factors including age, gender, ethnicity, marital status, education, employment, income, ethnicity and race, and religion/spirituality.
- Disease-related factors including treatment modality, frequency of weekly dialysis sessions, duration and frequency of dialysis, duration of illness, comorbidity, level of patient’s dependency, and quality of Life (QoL).
- Situational and relational factors including cohabiting status, relationship to the patient, the duration of caregiving, contact time per week, duration of relationship with patients, number of children, smoking and alcohol consumption, and caregiver performing exercise.
- Environmental factors including social support.
- Psychological factors including depression and anxiety.
3.3.1. Caregiver and Patient Socio-Demographical Factors
Age of Caregivers and Patients, and Perceived CB
Gender and CB
Marital Status and CB
Education, Income and Employment
Ethnicity, Race and Religion
3.3.2. Disease-Related Factors
Comorbidity, Duration of Illness, Patient’s Dependency, Health Status and QoL
Duration and Frequency of Dialysis, and Treatment Modality
3.3.3. Situational and Relational Factors
Caregiver relationship to patients, cohabiting arrangements, place of residency, duration of caregiving and duration of relationship between patients and caregivers
3.3.4. Environmental Factors
3.3.5. Psychological Factors
4. Discussion
4.1. Consistency between Studies
4.2. Inconsistent Findings
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Included Studies | Were the Criteria for Inclusion in the Sample Clearly Defined? | Were the Study Subjects and the Setting Described in Detail? | Was Exposure Measured in a Valid and Reliable Way? | Were Objective, Standard Criteria Used for Measurement of the Condition? | Were Confounding Factors Identified? | Were Strategies to Deal with Confounding Factors Stated? | Were the Outcomes Measured in a Valid and Reliable Way? | Was Appropriate Statistical Analysis Used? | Quality Assessment Scores |
|---|---|---|---|---|---|---|---|---|---|
| Abed et al. (2020) | Yes | Unclear | Unclear | Yes | Unclear | Unclear | Yes | Yes | Moderate |
| Adejumo et al. (2019) | Unclear | Unclear | Yes | Yes | Unclear | Unclear | Yes | Yes | Moderate |
| Affinito et al. (2018) | Yes | Unclear | Unclear | Yes | Unclear | Unclear | Yes | Yes | Moderate |
| Alnazly (2016) | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | High |
| Alvarez-Ude et al. (2004) | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | High |
| Al Wakeel & Bayoumi (2016) | Yes | Unclear | Yes | Yes | Unclear | Unclear | Yes | Yes | Moderate |
| Avsar et al. (2013) | Yes | Unclear | Yes | Unclear | Yes | Yes | Yes | Yes | High |
| Avsar et al. (2015) | Yes | Unclear | Unclear | Unclear | Yes | Yes | Yes | Yes | Moderate |
| Bardak et al. (2018) | Yes | Unclear | Yes | Yes | Unclear | Unclear | Yes | Yes | Moderate |
| Bayoumi (2014) | Yes | Unclear | Unclear | Yes | Yes | Yes | Yes | Yes | High |
| Belasco and Sesso (2002) | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | High |
| Belasco et al. (2006) | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | High |
| Cagan et al. (2018) | Unclear | Unclear | Yes | Unclear | Unclear | Yes | Yes | Yes | Moderate |
| Cantekin et al. (2016) | Unclear | Unclear | Unclear | Unclear | Yes | Yes | Yes | Yes | Moderate |
| Faridah et al. (2020) | Unclear | Unclear | yes | unclear | Unclear | Unclear | Yes | yes | Moderate |
| Harris et al. (2000) | Yes | Unclear | Unclear | Unclear | Yes | Yes | Yes | Yes | Moderate |
| Hoang et al. (2019) | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | High |
| Jafari et al. (2018) | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | High |
| Joy et al. (2019) | unclear | Unclear | Yes | yes | Unclear | unclear | yes | Yes | Moderate |
| Kang et al. (2019) | Unclear | Unclear | Yes | Unclear | Unclear | unclear | Yes | Yes | Moderate |
| Kilic and Kaptanogullari (2017) | Yes | Unclear | Yes | Yes | Unclear | Unclear | Yes | Yes | Moderate |
| Mashayekhi et al. (2015) | Yes | Unclear | Yes | Yes | Unclear | Unclear | Yes | Yes | Moderate |
| Molloaoglu et al. (2013) | Yes | Unclear | Yes | Yes | Yes | Unclear | Yes | Yes | High |
| Nagarathnam et al. (2019) | Unclear | Unclear | Unclear | Yes | Unclear | Unclear | Yes | Yes | Moderate |
| Oyegbile and Brysiewicz (2017) | Yes | Unclear | Yes | Unclear | Yes | Yes | Yes | Yes | High |
| Paschou et al. (2018) | Unclear | Unclear | Yes | Unclear | Unclear | Unclear | Yes | Yes | Moderate |
| Rafati et al. (2019) | Yes | Unclear | Yes | Yes | Yes | Unclear | Yes | Yes | High |
| Rioux et al. (2012) | Yes | Unclear | Yes | Unclear | Unclear | Unclear | Yes | Yes | Moderate |
| Rodrigue et al. (2010) | Yes | Unclear | Yes | Unclear | yes | Unclear | Yes | Yes | Moderate |
| Senmar et al. (2019) | Yes | Yes | Yes | Yes | Unclear | Unclear | Yes | Yes | High |
| Shah et al. (2017) | Unclear | Unclear | Yes | Unclear | Unclear | Unclear | Yes | Yes | Moderate |
| Shakya et al. (2017) | Yes | Unclear | Yes | Unclear | Unclear | Unclear | Yes | Yes | Moderate |
| Shimoyama et al. (2003) | Unclear | Unclear | Yes | Yes | Unclear | Unclear | Yes | Yes | Moderate |
| Tao et al. (2020) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | High |
| Washio et al. (2012) | Unclear | Unclear | Yes | Unclear | Yes | Unclear | Yes | Yes | Moderate |
| Wicks et al. (1997) | Yes | Unclear | Yes | Unclear | Yes | Yes | yes | yes | High |
| Zhang et al. (2016) | Unclear | Unclear | Yes | Unclear | Unclear | Unclear | Yes | Yes | Moderate |
| Zhang et al. (2020) | Yes | Yes | Yes | Yes | Unclear | Unclear | Yes | Yes | High |
References
- Hill, N.R.; Fatoba, S.T.; Oke, J.L.; Hirst, J.A.; O’Callaghan, C.A.; Lasserson, D.S.; Hobbs, F.R. Global prevalence of chronic kidney disease—A systematic review and meta-analysis. PLoS ONE 2016, 11, e0158765. [Google Scholar] [CrossRef]
- Hoang, V.L.; Green, T.; Bonner, A. Informal caregivers’ experiences of caring for people receiving dialysis: A mixed-methods systematic review. J. Ren. Care 2018, 44, 82–95. [Google Scholar] [CrossRef]
- Etters, L.; Goodall, D.; Harrison, B.E. Caregiver burden among dementia patient caregivers: A review of the literature. J. Am. Acad. Nurse Pract. 2008, 20, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Zarit, S.H.; Todd, P.A.; Zarit, J.M. Subjective burden of husbands and wives as caregivers: A longitudinal study. Gerontologist 1986, 26, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Rodrigue, J.R.; Dimitri, N.; Reed, A.; Antonellis, T.; Pavlakis, M.; Johnson, S.R.; Mandelbrot, D.A. Spouse caregivers of kidney transplant patients: Quality of life and psychosocial outcomes. Prog. Transplant. 2010, 20, 335–342. [Google Scholar] [CrossRef]
- Oyegbile, Y.O.; Brysiewicz, P. Exploring caregiver burden experienced by family caregivers of patients with End-Stage Renal Disease in Nigeria. Int. J. Afr. Nurs. Sci. 2017, 7, 136–143. [Google Scholar] [CrossRef]
- Chiao, C.-Y.; Wu, H.-S.; Hsiao, C.-Y. Caregiver burden for informal caregivers of patients with dementia: A systematic review. Int. Nurs. Rev. 2015, 62, 340–350. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Bayoumi, M.M. Subjective burden on family carers of hemodialysis patients. Open J. Nephrol. 2014, 4, 79. [Google Scholar] [CrossRef]
- Shakya, D. Burden and Depression among Caregivers of Hemodialysis Patients. PMCOA Palliat. Med. Care Open Access 2017, 4, 1–6. [Google Scholar] [CrossRef]
- Cagan, O.; Unsal, A.; Celik, N.; Yilmaz, A.T.; Culha, I.; Eren, H.K. Care Burden of Caregivers of Hemodialysis Patients and Related Factors. Int. J. Caring Sci. 2018, 11, 279. [Google Scholar]
- Zhang, R.; Cui, X.; Zhuang, H.; Xie, W.; Iv, L.; Liu, Y. The burden for caring patients on maintenance hemodialysis is influenced by social and demographic factors. Gen. Med. 2016, 4, 281. [Google Scholar] [CrossRef]
- Aromataris, E.; Munn, Z. Joanna Briggs Institute Reviewer’s Manual; The Joanna Briggs Institute: Adelaide, Australia, 2017. [Google Scholar]
- Popay, J.; Roberts, H.; Sowden, A.; Petticrew, M.; Arai, L.; Rodgers, M.; Britten, N.; Roen, K.; Duffy, S. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews: A Product from the ESRC Methods Programme Version 1; Lancaster University: Lancaster UK, 2006. [Google Scholar]
- Ioannidis, J.P.; Patsopoulos, N.A.; Rothstein, H.R. Reasons or excuses for avoiding meta-analysis in forest plots. BMJ 2008, 336, 1413–1415. [Google Scholar] [CrossRef]
- Abed, M.A.; Khalifeh, A.H.; Khalil, A.A.; Darawad, M.W.; Moser, D.K. Functional health literacy and caregiving burden among family caregivers of patients with end-stage renal disease. Res. Nurs. Health 2020, 43, 529–537. [Google Scholar] [CrossRef]
- Adejumo, O.A.; Iyawe, I.O.; Akinbodewa, A.A.; Abolarin, O.S.; Alli, E.O. Burden, psychological well-being and quality of life of caregivers of end stage renal disease patients. Ghana Med. J. 2019, 53, 190–196. [Google Scholar] [CrossRef]
- Affinito, J.; Louie, K. Positive Coping and Self-Assessed Levels of Health and Burden in Unpaid Caregivers of Patients with End Stage Renal Disease Receiving Hemodialysis Therapy. Nephrol. Nurs. J. 2018, 45, 373–380. [Google Scholar]
- Alnazly, E.K. Burden and coping strategies among J ordanian caregivers of patients undergoing hemodialysis. Hemodial. Int. 2016, 20, 84–93. [Google Scholar] [CrossRef]
- Alvarez-Ude, F.; Valdés, C.; Estébanez, C.; Rebollo, P. Health-related quality of life of family caregivers of dialysis patients. J. Nephrol. 2004, 17, 841–850. [Google Scholar] [PubMed]
- Al Wakeel, J.S.; Bayoumi, M.M. Caregiver burden among peritoneal dialysis and hemodialysis family in Saudi Arabia. Kuwait Med. J. 2016, 48, 197–201. [Google Scholar]
- Avsar, U.; Avsar, U.; Cansever, Z.; Set, T.; Cankaya, E.; Kaya, A.; Gozubuyuk, H.; Saatci, F.; Keles, M. Psychological and emotional status, and caregiver burden in caregivers of patients with peritoneal dialysis compared with caregivers of patients with renal transplantation. Transplant. Proc. 2013, 45, 883–886. [Google Scholar] [CrossRef] [PubMed]
- Avşar, U.; Avşar, U.Z.; Cansever, Z.; Yucel, A.; Cankaya, E.; Certez, H.; Keles, M.; Aydınlı, B.; Yucelf, N. Caregiver burden, anxiety, depression, and sleep quality differences in caregivers of hemodialysis patients compared with renal transplant patients. Transplant. Proc. 2015, 47, 1388–1391. [Google Scholar] [CrossRef]
- Bardak, S.; Demir, S.; Aslan, E.; Turgutalp, K.; Celikcan, H.D.; Dolarslan, M.E.; Kılıcarslan, C.; Karasu, F.; Gunes, A.J.; Kurt, C. The other side of the coin in renal replacement therapies: The burden on caregivers. Int. Urol. Nephrol. 2019, 51, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Belasco, A.; Barbosa, D.; Bettencourt, A.R.; Diccini, S.; Sesso, R. Quality of life of family caregivers of elderly patients on hemodialysis and peritoneal dialysis. Am. J. Kidney Dis. 2006, 48, 955–963. [Google Scholar] [CrossRef]
- Belasco, A.G.; Sesso, R. Burden and quality of life of caregivers for hemodialysis patients. Am. J. Kidney Dis. 2002, 39, 805–812. [Google Scholar] [CrossRef]
- Cantekin, I.; Kavurmacı, M.; Tan, M. An analysis of caregiver burden of patients with hemodialysis and peritoneal dialysis. Hemodial. Int. 2016, 20, 94–97. [Google Scholar] [CrossRef] [PubMed]
- Faridah, V.N.; Nursalam, N.; Agustini, N.L.P.I.B.; Lestari, T.P.; Suratmi, S.; Juanita, F.; Aris, A. Determinants of the Caregiver Burden of CKD Patients Undergoing Hemodialysis. Int. J. Psychosoc. Rehabil. 2020, 24. [Google Scholar] [CrossRef]
- Harris, T.T.; Thomas, C.M.; Wicks, M.N.; Faulkner, M.S. Subjective burden in young and older African-American caregivers of patients with end stage renal disease awaiting transplant/Commentary and response. Nephrol. Nurs. J. 2000, 27, 383. [Google Scholar]
- Hoang, V.L.; Green, T.; Bonner, A. Informal caregivers of people undergoing haemodialysis: Associations between activities and burden. J. Ren. Care 2019, 45, 151–158. [Google Scholar] [CrossRef]
- Jafari, H.; Ebrahimi, A.; Aghaei, A.; Khatony, A. The relationship between care burden and quality of life in caregivers of hemodialysis patients. BMC Nephrol. 2018, 19, 321. [Google Scholar] [CrossRef]
- Joy, J.; TJ, H.K.; Abraham, P.M.; Gopalakrishnan, S. Burden and resilience in caregivers of patients on maintenance haemodialysis. Int. J. Res. Med. Sci. 2019, 7, 4033. [Google Scholar] [CrossRef]
- Kilic, H.F.; Kaptanogullari, H. A Bicommunal Study: Burden of Caregivers of Hemodialysis Patients. Int. J. Caring Sci. 2017, 10, 1382–1390. [Google Scholar]
- Mashayekhi, F.; Pilevarzadeh, M.; Rafati, F. The assessment of caregiver burden in caregivers of hemodialysis patients. Mater. Soc. Med. 2015, 27, 333. [Google Scholar] [CrossRef]
- Nagarathnam, M.; Sivakumar, V.; Latheef, S. Burden, coping mechanisms, and quality of life among caregivers of hemodialysis and peritoneal dialysis undergoing and renal transplant patients. Indian J. Psychiatry 2019, 61, 380. [Google Scholar] [PubMed]
- Paschou, A.; Damigos, D.; Skapinakis, P.; Siamopoulos, K. The Relationship between Burden and Depression in Spouses of Chronic Kidney Disease Patients. Depress. Res. Treat. 2018, 2018. [Google Scholar] [CrossRef] [PubMed]
- Rafati, F.; Mashayekhi, F.; Dastyar, N. Caregiver Burden and Spiritual Well-being in Caregivers of Hemodialysis Patients. J. Relig. Health 2019, 59, 3084–3096. [Google Scholar] [CrossRef]
- Rioux, J.P.; Narayanan, R.; Chan, C.T. Caregiver burden among nocturnal home hemodialysis patients. Hemodial. Int. 2012, 16, 214–219. [Google Scholar] [CrossRef]
- Senmar, M.; Rafiei, H.; Yousefi, F.; Razaghpoor, A.; Bokharaei, M. Caregiver burden among family caregivers of older patients receiving hemodialysis and its relevant factors. J. Nephropharmacol. 2019, 8, e12. [Google Scholar] [CrossRef]
- Shah, H.B.U.; Atif, I.; Rashid, F.; Babar, M.W.; Arshad, F.; Qamar, W.; Khan, O.A.; Qadir, M.L. Assessment of caregiver burden of patients receiving dialysis treatment in Rawalpindi. J. Pak. Med. Assoc. 2017, 67, 1498–1501. [Google Scholar]
- Shimoyama, S.; Hirakawa, O.; Yahiro, K.; Mizumachi, T.; Schreiner, A.; Kakuma, T. Health-related quality of life and caregiver burden among peritoneal dialysis patients and their family caregivers in Japan. Perit. Dial. Int. 2003, 23, S200–S205. [Google Scholar] [CrossRef]
- Tao, X.; Chow, S.K.Y.; Zhang, H.; Huang, J.; Gu, A.; Jin, Y.; He, Y.; Li, N. Family caregiver’s burden and the social support for older patients undergoing peritoneal dialysis. J. Ren. Care 2020, 46, 222–232. [Google Scholar] [CrossRef]
- Washio, M.; Yoshida, H.; Ura, N.; Ohnishi, H.; Togashi, N.; Sakauchi, F.; Arai, Y.; Mori, M.; Shimamoto, K. Burden among family caregivers of patients on chronic hemodialysis in northern Japan. Int. Med. J. 2012, 19, 221–223. [Google Scholar]
- Wicks, M.N.; Milstead, E.J.; Hathaway, D.K.; Cetingok, M.; Hickey, J.V.; Currier, H. Subjective burden and quality of life in family caregivers of patients with end stage renal disease. ANNA J. 1997, 24, 527–539. [Google Scholar]
- Zhang, R.; Pu, C.; Cui, X.; Zhang, N.; Li, X.; Zheng, F. Burden in primary family caregivers caring for uremic patients on maintenance peritoneal dialysis. Perit. Dial. Int. 2020, 40, 556–562. [Google Scholar] [CrossRef]
- Mollaoğlu, M.; Kayataş, M.; Yürügen, B. Effects on caregiver burden of education related to home care in patients undergoing hemodialysis. Hemodial. Int. 2013, 17, 413–420. [Google Scholar] [CrossRef]
- Kang, A.; Yu, Z.; Foo, M.; Chan, C.M.; Griva, K. Evaluating burden and quality of life among caregivers of patients receiving peritoneal dialysis. Perit. Dial. Int. 2019, 39, 176–180. [Google Scholar] [CrossRef] [PubMed]
- Zarit, S.H.; Reever, K.E.; Bach-Peterson, J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist 1980, 20, 649–655. [Google Scholar] [CrossRef]
- Elmståhl, S.; Malmberg, B.; Annerstedt, L. Caregiver’s burden of patients 3 years after stroke assessed by a novel caregiver burden scale. Arch. Phys. Med. Rehabil. 1996, 77, 177–182. [Google Scholar] [CrossRef]
- Novak, M.; Guest, C. Application of a Multidimensional Caregiver Burden Inventory1. Gerontologist 1989, 29, 798–803. [Google Scholar] [CrossRef] [PubMed]
- Bakas, T.; Austin, J.K.; Jessup, S.L.; Williams, L.S.; Oberst, M.T. Time and difficulty of tasks provided by family caregivers of stroke survivors. J. Neurosci. Nurs. 2004, 36, 95. [Google Scholar] [CrossRef] [PubMed]
- Abe, K. Reconsidering the Caregiving Stress Appraisal scale: Validation and examination of its association with items used for assessing long-term care insurance in Japan. Arch. Gerontol. Geriatr. 2007, 44, 287–297. [Google Scholar] [CrossRef] [PubMed]
- Robinson, B.C. Validation of a Caregiver Strain Index. J. Gerontol. 1983, 38, 344–348. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, A.; Rahmani, H.; Shariati, A.; Asayesh, H.; Ashraf Rezaee, N.; Mollaei, E.; Shoori Bidgoli, A.; Bathaei, S. The relationship between caring burden and coping strategies in hemodialysis patients caregivers. J. Urmia Nurs. Midwifery Fac. 2012, 10, 533–539. [Google Scholar]
- Arechabala, M.; Catoni, M.I.; Palma, E.; Barrios, S. Depression and self-perceived burden of care by hemodialysis patients and their caregivers. Rev. Panam. Salud Publica Pan Am. J. Public Health 2011, 30, 74–79. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gülpak, M.; Kocaöz, S. The care burden and the affecting factors of individuals receiving hemodialysis treatment. TAF Prev. Med. Bull. 2014, 13, 99–108. [Google Scholar] [CrossRef]
- Talebi, M.; Mokhtari Lakeh, N.; Rezasoltani, P. Caregiver Burden in Caregivers of RenalF Patients under Hemodialysis. J. Holist. Nurs. Midwifery 2016, 26, 59–68. [Google Scholar]
- Teixidó-Planas, J.; Velasco, L.T.; Suárez, N.A.; Mas, A.C. Carer’s burden of peritoneal dialysis patients. Questionnaire and scale validation. Nefrol. Engl. Ed. 2018, 38, 535–544. [Google Scholar] [CrossRef]
- Dastyar, N.; Mashayekhi, F.; Rafati, F. Caregiving burden in hemodialysis patients’ caregivers in Kerman Province: A descriptive-analytical study. J. Jiroft Univ. Med Sci. 2020, 7, 323–331. [Google Scholar]
- Al-Rawashdeh, S.Y.; Lennie, T.A.; Chung, M.L. Psychometrics of the Zarit Burden Interview in caregivers of patients with heart failure. J. Cardiovasc. Nurs. 2016, 31, E21. [Google Scholar] [CrossRef]
- Chou, K.R. Caregiver burden: A concept analysis. J. Pediatr. Nurs. 2000, 15, 398–407. [Google Scholar] [CrossRef]
- Xiong, C.; Biscardi, M.; Astell, A.; Nalder, E.; Cameron, J.I.; Mihailidis, A.; Colantonio, A. Sex and gender differences in caregiving burden experienced by family caregivers of persons with dementia: A systematic review. PLoS ONE 2020, 15, e0231848. [Google Scholar] [CrossRef] [PubMed]
- Chappell, N.L.; Dujela, C.; Smith, A. Caregiver Well-Being:Intersections of Relationship and Gender. Res. Aging 2015, 37, 623–645. [Google Scholar] [CrossRef]
- Akpınar, B.; Küçükgüçlü, Ö.; Yener, G. Effects of Gender on Burden Among Caregivers of Alzheimer’s Patients. J. Nurs. Scholarsh. 2011, 43, 248–254. [Google Scholar] [CrossRef]
- Chaplin, T.M. Gender and Emotion Expression: A Developmental Contextual Perspective. Emot. Rev. 2015, 7, 14–21. [Google Scholar] [CrossRef]
- Kring, A.M.; Gordon, A.H. Sex Differences in Emotion: Expression, Experience, and Physiology. J. Pers. Soc. Psychol. 1998, 74, 686–703. [Google Scholar] [CrossRef]
- Almutary, H.; Bonner, A.; Douglas, C. Which patients with chronic kidney disease have the greatest symptom burden? A comparative study of advanced ckd stage and dialysis modality. J. Ren. Care 2016, 42, 73–82. [Google Scholar] [CrossRef]
- Andrén, S.; Elmståhl, S. Relationships between income, subjective health and caregiver burden in caregivers of people with dementia in group living care: A cross-sectional community-based study. Int. J. Nurs. Stud. 2007, 44, 435–446. [Google Scholar] [CrossRef] [PubMed]
- Serrano-Aguilar, P.; Lopez-Bastida, J.; Yanes-Lopez, V. Impact on health-related quality of life and perceived burden of informal caregivers of individuals with Alzheimer’s disease. Neuroepidemiology 2006, 27, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Conde-Sala, J.L.; Garre-Olmo, J.; Turró-Garriga, O.; Vilalta-Franch, J.; López-Pousa, S. Differential features of burden between spouse and adult-child caregivers of patients with Alzheimer’s disease: An exploratory comparative design. Int. J. Nurs. Stud. 2010, 47, 1262–1273. [Google Scholar] [CrossRef] [PubMed]
- Ganapathy, V.; Graham, G.D.; DiBonaventura, M.D.; Gillard, P.J.; Goren, A.; Zorowitz, R.D. Caregiver burden, productivity loss, and indirect costs associated with caring for patients with poststroke spasticity. Clin. Interv. Aging 2015, 10, 1793. [Google Scholar]
- Miller, B.; Montgomery, A. Family caregivers and limitations in social activities. Res. Aging 1990, 12, 72–93. [Google Scholar] [CrossRef]
- Raccichini, A.; Spazzafumo, L.; Castellani, S.; Civerchia, P.; Pelliccioni, G.; Scarpino, O. Living with mild to moderate Alzheimer patients increases the caregiver’s burden at 6 months. Am. J. Alzheimers Dis. Dement. 2015, 30, 463–467. [Google Scholar] [CrossRef]
- Viñas-Diez, V.; Turró-Garriga, O.; Portellano-Ortiz, C.; Gascón-Bayarri, J.; Reñé-Ramírez, R.; Garre-Olmo, J.; Conde-Sala, J.L. Kinship and cohabitation in relation to caregiver burden in the context of Alzheimer’s disease: A 24-month longitudinal study. Int. J. Geriatr. Psychiatry 2017, 32, e72–e82. [Google Scholar] [CrossRef]
- Jung, H.-Y.; Jeon, Y.; Park, Y.; Kim, Y.S.; Kang, S.-W.; Yang, C.W.; Kim, N.-H.; Choi, J.-Y.; Cho, J.-H.; Park, S.-H. Better quality of life of peritoneal dialysis compared to hemodialysis over a two-year period after dialysis initiation. Sci. Rep. 2019, 9, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Fang, B.; Chan, J.; Chen, G. The relationship between comorbidities in dementia patients and burden on adult–child primary caregivers: Does having a secondary caregiver matter? Int. J. Ment. Health Nurs. 2019, 28, 1306–1317. [Google Scholar] [CrossRef] [PubMed]
- Garcia, R.S.; Pinheiro, B.V.; Lucinda, L.M.; Pimentel, A.L.; Júnior, J.M.; Paula, R.B.; Reboredo, M.M. Association between exercise training in haemodialysis patients and burden of their family caregivers: A cross-sectional study. Nephrology 2020, 25, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Kim, D. Relationships between Caregiving Stress, Depression, and Self-Esteem in Family Caregivers of Adults with a Disability. Occup. Ther. Int. 2017, 2017, 9. [Google Scholar] [CrossRef]
- Kim, H.; Chang, M.; Rose, K.; Kim, S. Predictors of caregiver burden in caregivers of individuals with dementia. J. Adv. Nurs. 2012, 68, 846–855. [Google Scholar] [CrossRef] [PubMed]
- Anngela-Cole, L.; Hilton, J.M. The Role of Attitudes and Culture in Family Caregiving for Older Adults. Home Health Care Serv. Q. 2009, 28, 59–83. [Google Scholar] [CrossRef] [PubMed]
- Yeh, Y.J. Knowledge management enablers: A case study. Ind. Manag. Data Syst. 2006, 106, 793–810. [Google Scholar] [CrossRef]
- Creedle, C.; Leak, A.; Deal, A.M.; Walton, A.M.; Talbert, G.; Riff, B.; Hornback, A. The impact of education on caregiver burden on two inpatient oncology units. J. Cancer Educ. 2012, 27, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Burnley, C.S. Caregiving: The impact on emotional support for single women. J. Aging Stud. 1987, 1, 253–264. [Google Scholar] [CrossRef]
- Vaingankar, J.A.; Chong, S.A.; Abdin, E.; Picco, L.; Jeyagurunathan, A.; Zhang, Y.; Sambasivam, R.; Chua, B.Y.; Ng, L.L.; Prince, M.; et al. Care participation and burden among informal caregivers of older adults with care needs and associations with dementia. Int. Psychogeriatr. 2016, 28, 221–231. [Google Scholar] [CrossRef]
- Randall, A.K.; Bodenmann, G. The role of stress on close relationships and marital satisfaction. Clin. Psychol. Rev. 2009, 29, 105–115. [Google Scholar] [CrossRef]
- Lin, I.F.; Fee, H.R.; Wu, H.S. Negative and Positive Caregiving Experiences: A Closer Look at the Intersection of Gender and Relatioships. Fam. Relat. 2012, 61, 343–358. [Google Scholar] [CrossRef] [PubMed]
- Friedemann, M.-L.; Buckwalter, K.C. Family Caregiver Role and Burden Related to Gender and Family Relationships. J. Fam. Nurs. 2014, 20, 313–336. [Google Scholar] [CrossRef] [PubMed]
- Zeng, L.; Zhu, X.; Meng, X.; Mao, Y.; Wu, Q.; Shi, Y.; Zhou, L. Responsibility and burden from the perspective of seniors’ family caregivers: A qualitative study in Shanghai, China. Int. J. Clin. Exp. Med. 2014, 7, 1818. [Google Scholar]
- Arun, R.; Inbakamal, S.; Tharyan, A.; Premkumar, P.S. Spousal caregiver burden and its relation with disability in schizophrenia. Indian J. Psychol. Med. 2018, 40, 22–28. [Google Scholar] [CrossRef]
| Author/Year/Country | Aim | Design/Sample | Caregiver Burden Level/Measurement Tool | Factors Associated with CB |
|---|---|---|---|---|
| Abed et al. (2020) Jordan | To investigate the functional health literacy and CB among family caregivers for patients receiving HD | Cross sectional study of 88 caregivers of patients on HD | Severe CB level using ZBI | Positive relationship of caregivers’ age to CB but no with patient age, history of comorbidity of caregivers. Caregivers with adequate health literacy had less CB than caregivers with limited health literacy. |
| Adejumo et al. (2019) Nigeria | To measure burden, psychological well-being, and QOL of caregivers of patients with ESKD | Cross sectional study of 57 caregivers of patients on HD | Mild to moderate CB level using ZBI | CB of female caregivers and experience higher scores of anxiety and depression were significantly higher than male caregivers. |
| Affinito and Louie (2018) USA | To explore the association between CB and the levels of health of caregivers of HD patients | Cross sectional study of 89 caregivers of patients on HD | Mean of 29.38 out of a total score of 48 indicating moderate to severe CB using CSA | Caregivers with good level of health, and who viewed their caregiver role positively, experienced a lesser degree of CB. |
| Alnazly (2016) Jordan | To explore the burden and coping strategies of caregivers of patients receiving HD | Cross sectional study of 139 caregivers of patients on HD | Moderate degree of burden using OCBS | Living with the patient was the only variable positively correlated to CB. Caregivers’ and patients’ age, gender, education, employment status, relation to patient, years of caregiving, and caregiving hours per week were not significantly related to CB. |
| Alvarez-Ude et al. (2004) Spain | To evaluate the HRQoL and burden of family caregivers of chronic dialysis patients and analyse the factors associated with it | Cross sectional study of 221 patients/caregivers of patients on HD and PD | Moderate to severe burden using ZBI | CB was higher in caregivers with less social support, and poor physical and mental health. Age of patients, number of caregiving hours, number of comorbid conditions of patients and caregivers, number of medications of patients, correlated positively with CB. No differences in CB were found between caregivers of patients with HD and PD. |
| Al wakeel and Bayoumi (2016) Saudi Arabia | To compare the burden on family caregiver between HD and PD in Saudi Arabian population | Cross sectional study of 105 caregivers, 50 caregivers of patients receiving HD and 55 caregivers of patients receiving PD | Mean CB in patient receiving HD was 43.3 (21.7) and 49 (24.5) in caregivers of the PD group. Both reported moderate to severe burden using ZBI | No significant differences between CB in caregivers of patients receiving PD and HD. Caregiver’s age and education level correlated negatively to CB in the HD group. Age and level of education and dialysis duration were not correlated to CB in PD group. |
| Avsar et al. (2013) Turkey | To examine the relationship between caregivers of PD and RT patients with regard to sleep quality, anxiety, depression, and overall burden | Cross sectional study of 113 caregivers, 53 RT recipients and 60 caregivers of PD patients | 51 (96.2%) of caregivers of RT recipients reported low CB and 30 (50%) of caregivers of patients on PD reported moderate CB using ZBI | CB scores were significantly higher in caregivers of PD patients compared with RT patients. The demographic data of caregivers did not significantly affect CB in either group including age, gender, income, and educational level. Duration of caregiving in year was not associated to CB. |
| Avsar et al. (2015) Turkey | To compare the caregivers of HD patients and caregivers of patients with RT in terms of anxiety, depression, sleep quality, and CB | Cross sectional study of 133 caregivers, 65 caregivers in the RT group and 68 in the HD group | 62 (95.4%) of caregivers of RT patients reported low CB. 31 (45.6%) of caregivers of HD patients reported low CB and 27 (39.7%) of them reported moderate CB using ZBI | CB scores were significantly higher for caregivers in the HD group compared with caregivers in the RT group. |
| Bardak et al. (2018) Turkey | To compare CB, psychological symptoms in caregivers of PD, HD, and RT, and find out associated factors | Cross sectional study of 127 caregivers caring for 43 PD, 42 HD, 42 RT patients | Participants reported mild to moderate CB in all caregiver groups (PD, HD, RT) using ZBI. | CB score was found to be higher in caregivers who reported higher level of psychological symptoms (anxiety and depression). CB score was found to be highest in caregivers of patients receiving HD, and it was significantly higher than PD and RT groups. The gender, age, occupation, marital status, and education level of caregivers and patients were not associated with ZBI score. ZBI score was also not associated to caregiver relationships to the patient, living in the same house, or whether caregivers take all responsibility alone or not. Longer duration of HD affected the ZBI scores positively. |
| Bayoumi (2014) Saudi Arabia | To evaluate the CB of individuals who provide care for patients on maintenance HD | Cross sectional study of 50 caregivers for patients on HD | Moderate to severe burden using ZBI | The total caregiver burden significantly correlated positively with patient age and negatively correlated with caregiver age. Negative correlations were identified between caregivers’ and patients’ levels of education in relation to CB. |
| Belasco and Sesso (2002) Brazil | To describe the characteristics of caregivers of chronic HD patients, assess their perceived burden and HRQoL and the factors influencing this burden | Cross sectional study of 100 caregivers of HD patients | Moderate CB using CBS | Caregivers of male patients with a low education level (illiterate or primary), with a multiple number of patient comorbid conditions had a higher mean score burden. Caregivers who were female spouses of patients, and caring for long lengths of time, perceived a significantly greater burden than those with other types of relationships. |
| Belasco et al. (2006) Brazil | To describe caregivers’ characteristics and evaluate their burden and QoL | Cross sectional study of 201 caregivers, 161 caregivers of HD patients and 40 caregivers of PD patients | Moderate burden for both caregivers of elderly HD and PD patients using CBS | There is a significant difference noted in the environment dimension of CBS, which was better for caregivers of the elderly receiving HD than in younger patients. Caregiver’s mental status score was lower for caregivers of elderly receiving PD than caregivers of patient receiving HD. No significant influence of caregiver sex detected. |
| Cagan et al. (2018) Turkey | To examine the burden of caregivers of HD patients and some related variables | Cross sectional study of 163 caregivers of HD patients | Moderate CB using ZBI | Higher CB reported in female caregivers and in those who were being employed, having 3 or more children, having difficulty in meeting their health expenses (poor income), reporting that their role in the family and work is negatively affected, and giving care for longer than 5 years. There was no correlation between CB and caregivers’ age, marital status, educational status, place of residence (county, town, village, province), type of personality, smoking and alcohol consumption and number of weekly dialysis sessions. |
| Cantekin et al. (2016) Turkey | To determine the burden on primary caregivers of patients undergoing dialysis | Cross sectional survey of 114 patients, 54 were relatives of HD patients and 60 were relatives of PD patients | Caregivers of HD patients reported moderate to high burden while caregivers of PD reported low to medium levels of CB using ZBI | Caregivers of PD patients had lower levels of burden than caregivers of HD patients, and this was highly significant. |
| Faridah et al. (2020) Indonesia | To determine the factors associated with the CB of caring families of HD patients | Cross sectional survey of 95 caregivers of HD patients | No burden to low burden using ZBI | High CB is associated with the low salary and older age of caregivers. Duration of care (time), gender, and education level of caregivers were not significant in relation to CB. |
| Harris et al. (2000) USA | To identify the level of CB reported by African American caregivers of patients with ESKD waiting for RT and to identify whether subjective burdens varied by caregiver age | Cross sectional survey of 78 African American family caregivers of patients with ESKD | Little to no burden using ZBI | There was no significant difference in the level of subjective burden reported by young and older African-American caregivers. |
| Hoang et al. (2019) Vietnam | To analyse the burden and support activities of informal caregivers caring for adults receiving haemodialysis | Cross-sectional study recruited 178 adult informal caregivers of patients receiving HD | Moderate to severe burden using ZBI | Being old, married to the care recipients, having comorbidity condition, longer time spent on caregiving tasks, duration of being caregiver, and having difficulty of doing caregiving tasks were significantly associated with increasing the CB. Employment types of caregivers, income, and being a relative to the patients have no effect on CB |
| Jafari et al. (2018) Iran | To determine the level of CB and its relationship with the QoL of caregivers of HD patients | Cross sectional study of 246 caregivers of HD patients | 42.7% experiencing moderate CB and 37.4% were experiencing high to severe levels of CB, using the Novak and Guest Care Burden Questionnaire | A significant positive correlation between the age of caregivers and CB. Increased education level decreased CB. With the increasing capability of patients in self-care, the CB of the caregiver decreased. High CB associated with the presence of comorbidity conditions. Significant and negative correlations between the total scores of CB and QoL. Patient age, caregiver and patient gender, occupation, education, and income were not associated with CB levels. |
| Joy et al. (2019) India | To assess the level of caregiver burden and resilience in caregivers of haemodialysis patients | Cross sectional study in 120 caregivers of patients on maintenance HD | Moderate to severe burden using ZBI | Duration of caregiving and time spent per day looking after the patients were associated positively with CB. Female caregivers reported higher burden than male caregivers. Age of caregivers was not associated with CB. Caregivers with low ability of adaptation to caregiving role had high burden. |
| Kang et al. (2019) Singapore | To examine changes in burden and QOL in caregivers of prevalent PD patients over 12 months | Longitudinal study in 44 caregivers of PD patients | Mild to moderate burden using ZBI | CB significantly increased over time. Over a 1 year period, the level of CB increased from mild to moderate burden to moderate to severe burden. |
| Kilic and Kaptanogullari (2017) Turkey | To evaluate the burden of caregivers who provided care to HD patients in two different communities | Cross sectional study of 210 caregivers of patients receiving HD | In Turkey (central district), mild CB & in Northern Cyprus (rural area) moderate CB, using ZBI | Caregiver to patient relationships: spouses had lower CB scores compared to other caregivers such as children, grandmothers/grandfathers, or siblings. Caregivers who live in the central district reported lower CB than those who live in rural areas. Caregiver age, sex, marital status, and educational status have no relation. |
| Mashayekhi et al. (2015) Iran | To assess the level of CB in caregivers of HD patients | Cross sectional study of 51 caregivers of HD patients | Moderate to severe levels of CB using CBS | Caregivers with inadequate income, caring for male patients had a higher CB score. Single caregivers gained higher scores of CB. No significant relationship between CB and patient’s occupation, education, marital status, comorbidities, duration of dialysis, level of patient dependency and frequency of HD per week. Education, occupation, gender, age of caregiver and kind of relationship with patient were associated to CB. |
| Mollaoglu et al. (2013) Turkey | To determine the burden, educational needs, influential factors, and the effects of home care education over CB among primary caregivers of patients undergoing HD | Pre and post-test design including 122 caregivers of HD patients | Moderate to severe, using ZBI | CB score was significantly higher in caregivers who are female, single than in married, young, caregivers with higher education and caregivers with comorbidity conditions compared to those who have no health problems. The spouses had a lower mean value of CB compared to those of daughters, daughters-in-law, and sisters/brothers Caregivers who live in a peripheral district or small town were found to have high CB, whereas those living in a central district of a province had low CB scores. Caregiver occupation and income were observed to have no impact on CB. |
| Nagarathnam et al. (2019) India | To evaluate the burden, coping mechanisms, and QOL among caregivers of HD and PD undergoing and RT patients | Cross sectional study of 90 patients (30 HD, 30 PD, and 30 RT patients) | Moderate to severe burden observed in caregivers of patients receiving HD, mild to moderate burden in patients receiving PD, and no burden were observed in RT patients, using ZBI | Significantly higher burden score in caregivers of HD undergoing than RT patients. |
| Oyegbile and Brysiewicz (2017) Nigeria | To explore the CB of family caregivers of ESKD patients in South-West Nigeria | Mixed method study including a cross sectional survey of 96 family caregivers of patients with ESKD | Moderate to severe CB using ZBI | Female caregivers experienced more burden of caregiving than their male counterparts. Caregivers living with patients experienced more burden of caregiving than those who live in separate residences. However, these did not reach statistically significant results. No significant differences in CB according to caregiver marital status, educational levels, religion, ethnicity, working status, relationship with patients, and duration of contact with patient. |
| Paschou et al. (2018) Greece | To explore the CB and depression in spouses of patients with CKD | Cross sectional study of 50 spouses of patients; 29 of whom were dialysis dependent and 21 were not dialysis dependent. | Moderate burden using ZBI | Caregiver age, gender, marital satisfaction, education, employment status and whether the patients were dialysis dependent or not have no relation to level CB. Higher levels of depression correlated to the increased perceived CB. |
| Rafati et al. (2019) Iran | To examine the relationship between caregiver burden and spiritual well-being in caregivers of patients receiving HD | Cross sectional-correlational study was conducted on 382 caregivers of patients receiving HD | Moderate to severe CB using the Novak and Guest Care Burden Questionnaire | A significant high CB was reported in caregivers who have a lower level of education, unemployed, lower spiritual well-being, older age. A significant high CB was reported in caregivers whose patients with low income, performing higher number of dialysis sessions per week, having lower level of dependency, and not having a kidney transplant history. |
| Rioux et al. (2012) Canada | To assess CB, QOL, and depressive symptoms and to compare these with their patients’ | Cross sectional study of 61 caregivers of HD patients | Low level burden perceived using CBS | Depression was correlated positively to CB. |
| Rodrigue et al. (2010) USA | To characterise the psychosocial functioning of spouse/partner caregivers | Cross sectional study spouse/partner caregivers of HD and PD patients before (n = 33) and after (n = 46) kidney transplantation | High CB before and after transplantation using CSI | CB was not associated with age, sex, or relationship duration even though older females reported high CB but did not reach statistical significance. High levels of patient physical health associated with lower CB. CB was higher when the patient was on HD than not yet on dialysis. Higher CB was associated with worse patient health and lower mental QOL. No differences between CB of patients before and after RT. |
| Senmar et al. (2019) Iran | To measure CB among caregivers of older patients receiving HD and its relevant factors | Cross sectional study in 52 caregivers of elderly patients receiving HD | Moderate to severe level of CB using Novak and Guest Caregiver Burden questionnaire. | High age of caregivers, high age of patients and the caregiver-patient relationship were factors that significantly associated with increasing the level of CB. Gender of patients and caregivers, marital status of patients and caregivers, education level of caregivers, the income of patients and duration of dialysis were not associated with CB. Spouses had higher level of CB than other relationship. |
| Shah et al. (2017) Pakistan | To determine CB of patients receiving dialysis | Cross sectional study 164 caregivers of patients receiving dialysis | Mild to moderate CB using ZBI | A positive correlation was found between the duration of patient on dialysis/year, daily hours of caregiving and the total CB score. Low social class, high level of patient functional dependency associated with high CB. |
| Shakya et al. (2017) Nepal | To assess the burden on caregivers and find out their liability for developing depression | Cross sectional, descriptive study design. 164 caregivers of patients taking maintenance HD | The mean CB score was 46.99(14.6) indicating moderate to severe burden using ZBI | CB increased with increasing caregiver age, decreasing education, low socio-economic status and decreasing social support. Widow caregiver reported high CB then in married and the lowest CB was on single. Relationship to patient were also found to affect burden (spouses and parents having higher CB than in children, siblings, children in law, and grandchildren). CB was significantly positively associated with caregiver depression. However, duration of dialysis, frequency of dialysis, comorbid illness of (patients) were not found to have any significant association with CB. |
| Shimoyama et al. (2003) Japan | To examine the relationship in Japan between PD patients and caregivers with regard to HRQOL and CB | Cross sectional survey 34 caregivers of PD patients | Mean CB was 14.1 indicating little to No burden using ZBI | Caregivers of patient receiving PD reported low CB levels. CB associated with increasing age of patients and decreasing health-related QoL of caregivers. |
| Tao et al. (2020) China | To examine the level of CB on family caregivers of elderly adults receiving PD and to identify any contributing factors | Cross sectional survey 60 caregivers of PD patients | Mild to moderate CB using ZBI | Being female caregiver with insufficient financial status, low level of social support for the caregiver, depressive symptoms in the patients and caring for a patient with disability were statistically significant predictors of CB. Patient gender and educational level were not associated with CB. Caregiver educational level, living with the patients at the same resident, relationship with patients, and hours of caregiving per week was not associated with CB. |
| Washio et al. (2012) Japan | To investigate factors related to burden among caregivers of regular HD patients | Cross sectional survey 108 caregivers of HD | Mean CB score of 29 indicating mild burden to moderate using ZBI | Being spouse, having chronic diseases, and long time spent on caregiving is reported to be a related factor to the heavy burden among caregivers. |
| Wicks et al. (1997) USA | To explore QoL and CB reported by caregivers of persons with ESKD and to examine the relationship between these variables | Cross sectional design 96 caregivers of 96 RT candidates diagnosed with ESKD | Little to no burden using ZBI | Neither caregiver race, gender, relationship to the patient, caregiver health level, nor patient gender significantly contributed to CB. CB did not differ by dialysis type (PD, incenter HD, etc.) or employment category (full-time, part-time, etc.). Caregivers Qol related negatively with CB. |
| Zhang et al. (2016) China | To assess the burden for caring patients on maintenance HD by primary family caregivers | Cross sectional survey 151 caregiver of HD patients | 151 caregivers, 51% of them reported mild to moderate burden and 25.2% caregivers reported moderate to severe burden using ZBI | Caregiver age increasing, low educational levels, without job, long caring hours were associated with high CB. CB was at lesser degree with high level of caregiver health. CB was significantly increased in patients with more than two comorbidities and patient’s low income. CB did not associate with duration of HD. Relationship with patients, spouses, parents, and adult children felt more stressful than siblings, daughters- and sons-in-law. |
| Zhang et al. (2020) China | To assess the burden in primary family members caring for uremic patients on PD | Cross sectional design on 170 PD patients | 60% of caregivers reported mild to moderate burden and 18.2% reported moderate to severe burden using ZBI | Duration of PD and presence of comorbidity in patients, being female caregivers, spending longer hours providing care to patients were associated with higher CB. Caregivers who lived with patient had higher CB than those who lived separately. Caregivers who exercised for more than 1 h a week had a lower CB. CB is negatively associated with Qol. Age of caregivers, educational level, relationship to patients, and annual income were not associated with CB. Level of patients. Frailty was associated positively with CB. |
| Abed et al. | Adejumo et al. | Affinito et al. | Alnazly | Alvarez et al. | Al Wakeel & Bayoumi | Avsar et al. | Avsar et al. | Bardak et al. | Bayoumi | Belasco & Sesso | Belasco et al. | Cagan et al. | Cantekin et al. | Faridah et al. | Harris et al. | Hoang et al. | Jafari et al. | Joy et al. | Kang et al. | Kilic & Kaptanogullari | Mashayekhi et al. | Mollaoğlu et al. | Nagarathnam et al. | Oyegbile | Paschou et al. | Rafati et al. | Rioux et al. | Rodrigue et al. | Senmar et al. | Shah et al. | Shakya et al. | Shimoyama et al. | Tao et al. | Washio et al. | Wicks et al. | Zhang et al. | Zhang et al. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Caregiver Age | s | n | s | n | n | s | n | n | n | s | n | s | s | n | n | n | s | n | s | n | s | s | s | n | ||||||||||||||
| Patients Age | n | n | s | n | s | n | s | n | n | n | s | s | n | |||||||||||||||||||||||||
| Caregiver gender | n | s | n | n | n | s | n | s | n | n | n | s | n | n | s | n | n | n | n | s | n | s | ||||||||||||||||
| Patient gender | n | n | n | s | n | n | s | n | n | n | n | n | ||||||||||||||||||||||||||
| Caregiver education | n | n | s | n | n | s | n | n | n | n | s | n | n | s | n | n | s | n | s | n | s | n | ||||||||||||||||
| Patient education | n | n | n | s | s | n | s | n | ||||||||||||||||||||||||||||||
| Caregiver occupation | n | n | n | s | n | n | n | n | n | n | s | n | s | |||||||||||||||||||||||||
| Patient occupation | n | n | n | n | s | |||||||||||||||||||||||||||||||||
| Marital status of caregiver | n | n | n | s | n | n | s | s | n | n | n | n | s | |||||||||||||||||||||||||
| Marital status of patient | n | n | n | n | n | |||||||||||||||||||||||||||||||||
| caregiver income | n | n | n | s | n | s | n | n | s | n | n | s | n | |||||||||||||||||||||||||
| Patient income | n | n | s | n | s | |||||||||||||||||||||||||||||||||
| Socio-economic class caregiver | s | s | s | |||||||||||||||||||||||||||||||||||
| Caregiver ethnicity and race | n | n | ||||||||||||||||||||||||||||||||||||
| Caregiver Religion/ spirituality | n | s | ||||||||||||||||||||||||||||||||||||
| Caregiving hours/day, week | n | s | n | n | s | s | n | s | n | s | s | |||||||||||||||||||||||||||
| Length of caregiving (months, years) | n | n | n | s | s | n | s | s | s | s | ||||||||||||||||||||||||||||
| Duration of patient illness | n | n | ||||||||||||||||||||||||||||||||||||
| Duration of dialysis | n | s | n | s | n | n | n | n | s | n | s | |||||||||||||||||||||||||||
| Caregiver relationship to patient | n | n | n | s | n | n | s | n | s | n | n | s | s | n | s | n | s | n | ||||||||||||||||||||
| Duration of relationship | ||||||||||||||||||||||||||||||||||||||
| Cohabiting status | s | n | n | n | n | n | s | |||||||||||||||||||||||||||||||
| Place of residence (town, village) (rural–urban) | n | s | s | |||||||||||||||||||||||||||||||||||
| Patient functional dependency level | s | s | n | s | s | s | s | s | ||||||||||||||||||||||||||||||
| Caregiver poor physical and mental health | s | s | ||||||||||||||||||||||||||||||||||||
| Patient comorbidity history | n | s | s | s | n | n | s | s | ||||||||||||||||||||||||||||||
| Caregiver comorbidity history | s | s | n | n | s | s | s | |||||||||||||||||||||||||||||||
| Smoking and alcohol consumptions | n | |||||||||||||||||||||||||||||||||||||
| Number of medication of patients | s | |||||||||||||||||||||||||||||||||||||
| Number of caregiver children | s | |||||||||||||||||||||||||||||||||||||
| Number (frequency) of dialysis session | n | n | s | n | ||||||||||||||||||||||||||||||||||
| Social support | s | s | s | s | ||||||||||||||||||||||||||||||||||
| Coping ability to caregiving role | s | s | ||||||||||||||||||||||||||||||||||||
| Positive role caregiver | s | |||||||||||||||||||||||||||||||||||||
| HRQol of caregiver/QoL | n | s | s | s | s | s | ||||||||||||||||||||||||||||||||
| Carer Depression and anxiety | s | s | s | s | s | s | ||||||||||||||||||||||||||||||||
| Patient Depression and anxiety | s | |||||||||||||||||||||||||||||||||||||
| Dialysis modalities (HD, PD) | n | n | s | n | s | n | ||||||||||||||||||||||||||||||||
| Dialysis dependent or not | n | s | ||||||||||||||||||||||||||||||||||||
| Before and after RT | s | s | s | s | s | n | ||||||||||||||||||||||||||||||||
| Caregiver health literacy | s | s | ||||||||||||||||||||||||||||||||||||
| Caregiver performing exercise | s |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alshammari, B.; Noble, H.; McAneney, H.; Alshammari, F.; O’Halloran, P. Factors Associated with Burden in Caregivers of Patients with End-Stage Kidney Disease (A Systematic Review). Healthcare 2021, 9, 1212. https://doi.org/10.3390/healthcare9091212
Alshammari B, Noble H, McAneney H, Alshammari F, O’Halloran P. Factors Associated with Burden in Caregivers of Patients with End-Stage Kidney Disease (A Systematic Review). Healthcare. 2021; 9(9):1212. https://doi.org/10.3390/healthcare9091212
Chicago/Turabian StyleAlshammari, Bushra, Helen Noble, Helen McAneney, Farhan Alshammari, and Peter O’Halloran. 2021. "Factors Associated with Burden in Caregivers of Patients with End-Stage Kidney Disease (A Systematic Review)" Healthcare 9, no. 9: 1212. https://doi.org/10.3390/healthcare9091212
APA StyleAlshammari, B., Noble, H., McAneney, H., Alshammari, F., & O’Halloran, P. (2021). Factors Associated with Burden in Caregivers of Patients with End-Stage Kidney Disease (A Systematic Review). Healthcare, 9(9), 1212. https://doi.org/10.3390/healthcare9091212








