Patterns and Facilitators for the Promotion of Glaucoma Medication Adherence—A Qualitative Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Setting
2.2. Sample Characteristics
3. Results
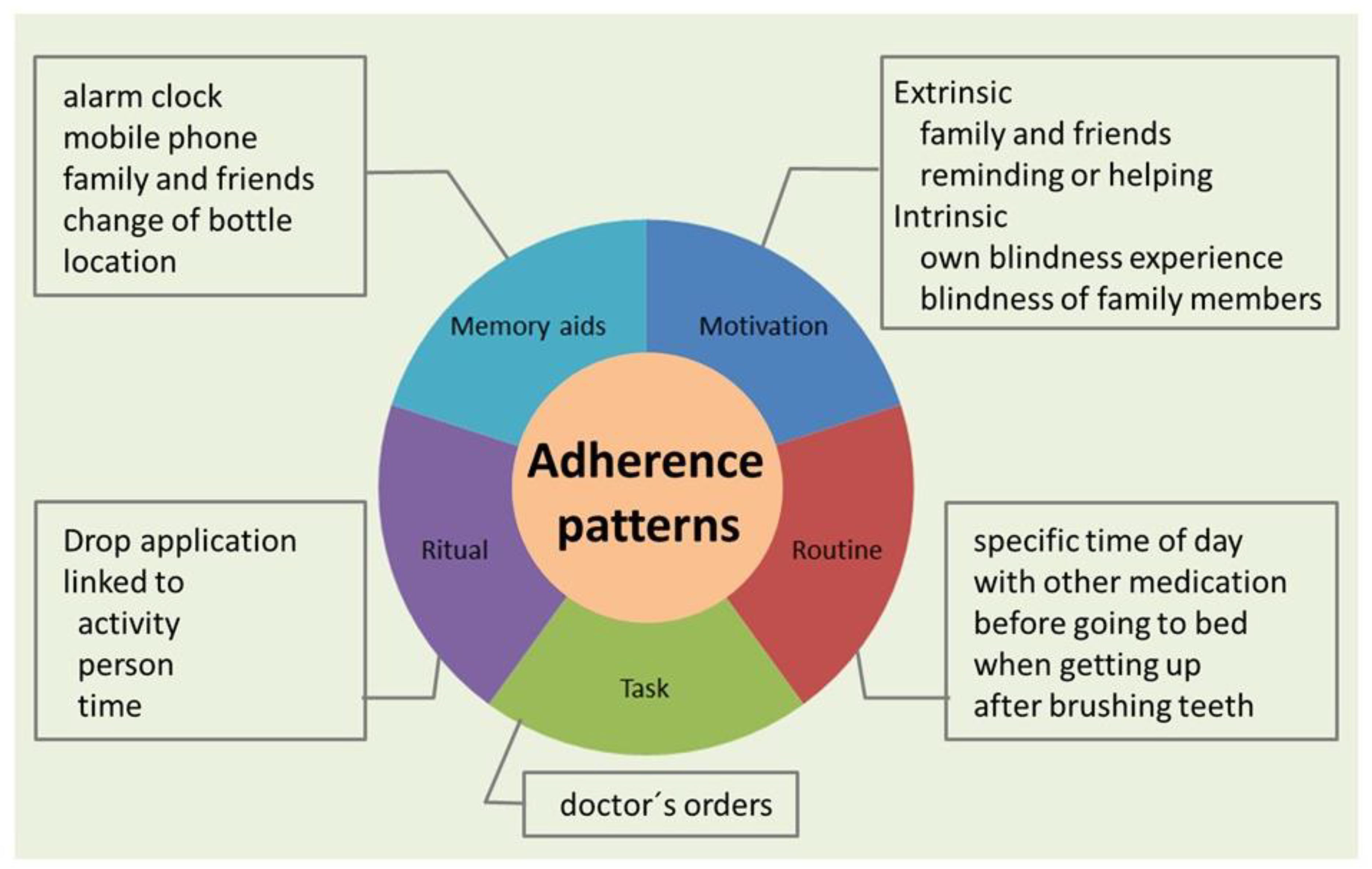
3.1. Motivation
3.1.1. Extrinsic Motivation
“And we do it very conscientiously and every evening at half past nine it’s my time to take my drops and my wife is doing this well. So this puts me in a stable situation”(PDA09)
“And when I’m out with a group of friends, I get a phone call, then someone from the group gives me my drops. Yes, my husband calls me to say: eye drops!”(PDA18)
3.1.2. Intrinsic Motivation
“But if you know you have to, and if it’s about keeping your eyesight, then you can do anything”(PDA17)
“You know, if you only have one eye left, then you´re gonna get, how should I put it, you get scared, you know?”(PDA15)
3.2. Ritual
“When I take my drops, say in the evening, let´s start in the evening. Well, then I’ve already taken the drops and so then I put the bottle on my facial care jar for the next morning. And then, before I can apply my facial care cream, I need to take the bottle of drops off of it”(PDA06)
“We take the drops at 8 pm, when it’s time for the weather forecast then it’s time for the drops, so we don’t forget them. Yes, so just before the weather forecast comes on, my husband gets up and gets the drops. That’s just part of it now”(PDA18)
3.3. Routine
“It has become second nature to me, just like brushing my teeth and getting undressed”(PDA02)
“Man is a creature of habit, right?”(PD03)
“I swallow my pills, I apply the eye drops”(PDA13)
3.4. Task
“Well I do as I´m told. I think that’s the right way to do it. Well, that’s how we live”(PD03)
“I try to take it regularly, as it’s been prescribed, and then that’s the way it is for me”(PDA12)
3.5. Memory Aids
“Yes, yes, when I sit and read in the evening, then I have it set for about 8. It rings, and the last one at 10, and then it’s automatically set to 8 a.m. and then, well, that´s part of my life, I hardly notice it anymore […] I’m just always armed with an alarm clock”(PDA17)
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Coleman, A.L.; Miglior, S. Risk factors for glaucoma onset and progression. Surv. Ophthalmol. 2008, 53 (Suppl. 1), S3–S10. [Google Scholar] [CrossRef] [PubMed]
- Rees, G.; Leong, O.; Crowston, J.G.; Lamoureux, E.L. Intentional and unintentional nonadherence to ocular hypotensive treatment in patients with glaucoma. Ophthalmology 2010, 117, 903–908. [Google Scholar] [CrossRef] [PubMed]
- Kholdebarin, R.; Campbell, R.J.; Jin, Y.-P.; Buys, Y.M. Multicenter study of compliance and drop administration in glaucoma. Can. J. Ophthalmol. 2008, 43, 454–461. [Google Scholar] [CrossRef] [PubMed]
- Frech, S.; Kreft, D.; Guthoff, R.F.; Doblhammer, G. Pharmacoepidemiological assessment of adherence and influencing co-factors among primary open-angle glaucoma patients-An observational cohort study. PLoS ONE 2018, 13, e0191185. [Google Scholar] [CrossRef]
- Mohindroo, C.; Ichhpujani, P.; Kumar, S. How ‘Drug Aware’ are our Glaucoma Patients? J. Curr. Glaucoma Pract. 2015, 9, 33–37. [Google Scholar] [CrossRef]
- Lanzl, I.; Kaercher, T. Konservierte Augentropfen und Adhärenz in der augenärztlichen Praxis. Ophthalmologe 2012, 109, 1087–1092. [Google Scholar] [CrossRef]
- Dietlein, T.S.; Rosentreter, A.; Lappas, A. Umsetzung und Schwierigkeiten bei Tropftherapien—Der ältere Glaukompatient im Fokus. Klin. Monbl. Augenheilkd. 2016, 233, 138–142. [Google Scholar] [CrossRef]
- Tsai, J.C.; McClure, C.A.; Ramos, S.E.; Schlundt, D.G.; Pichert, J.W. Compliance barriers in glaucoma: A systematic classification. J. Glaucoma 2003, 12, 393–398. [Google Scholar] [CrossRef]
- Green, J.; Britten, N. Qualitative research and evidence based medicine. BMJ 1998, 316, 1230–1232. [Google Scholar] [CrossRef]
- Taylor, S.A.; Galbraith, S.M.; Mills, R.P. Causes of non-compliance with drug regimens in glaucoma patients: A qualitative study. J. Ocul. Pharm. Ther. 2002, 18, 401–409. [Google Scholar] [CrossRef]
- Lacey, J.; Cate, H.; Broadway, D.C. Barriers to adherence with glaucoma medications: A qualitative research study. Eye 2009, 23, 924–932. [Google Scholar] [CrossRef]
- Stryker, J.E.; Beck, A.D.; Primo, S.A.; Echt, K.V.; Bundy, L.; Pretorius, G.C.; Glanz, K. An exploratory study of factors influencing glaucoma treatment adherence. J. Glaucoma 2010, 19, 66–72. [Google Scholar] [CrossRef]
- Cramer, J.A.; Roy, A.; Burrell, A.; Fairchild, C.J.; Fuldeore, M.J.; Ollendorf, D.A.; Wong, P.K. Medication compliance and persistence: Terminology and definitions. Value Health 2008, 11, 44–47. [Google Scholar] [CrossRef]
- Brown, M.T.; Bussell, J.K. Medication adherence: WHO cares? Mayo Clin. Proc. 2011, 86, 304–314. [Google Scholar] [CrossRef]
- Nohl, A.-M. Interview und Dokumentarische Methode: Anleitungen für Die Forschungspraxis, 5., Aktualisierte und Erweiterte Auflage; Springer: Wiesbaden, Germany, 2017; ISBN 978-3-658-16079-1. [Google Scholar]
- Przyborski, A.; Wohlrab-Sahr, M. Qualitative Sozialforschung: Ein Arbeitsbuch, 2., korr. Auflage; Oldenbourg: München, Germany, 2009; ISBN 9783486591033. [Google Scholar]
- Fiese, B.H. Routines and Rituals: Opportunities for Participation in Family Health. OTJR Occup. Particip. Health 2007, 27, 41S–49S. [Google Scholar] [CrossRef]
- Marshall, D. Food as ritual, routine or convention. Consum. Mark. Cult. 2005, 8, 69–85. [Google Scholar] [CrossRef]
- Lavie, I.; Steiner, A.; Sfard, A. Routines we live by: From ritual to exploration. Educ. Stud. Math. 2019, 101, 153–176. [Google Scholar] [CrossRef]
- Black, K.; Lobo, M. A conceptual review of family resilience factors. J. Fam. Nurs. 2008, 14, 33–55. [Google Scholar] [CrossRef]
- McDonald, S.; Ferguson, E.; Hagger, M.S.; Foss, A.J.E.; King, A.J. A theory-driven qualitative study exploring issues relating to adherence to topical glaucoma medications. Patient Prefer. Adherence 2019, 13, 819–828. [Google Scholar] [CrossRef]
- Pound, P.; Britten, N.; Morgan, M.; Yardley, L.; Pope, C.; Daker-White, G.; Campbell, R. Resisting medicines: A synthesis of qualitative studies of medicine taking. Soc. Sci. Med. 2005, 61, 133–155. [Google Scholar] [CrossRef]
- Fiese, B.H.; Tomcho, T.J.; Douglas, M.; Josephs, K.; Poltrock, S.; Baker, T. A review of 50 years of research on naturally occurring family routines and rituals: Cause for celebration? J. Fam. Psychol. 2002, 16, 381–390. [Google Scholar] [CrossRef]
- Lunnela, J.; Kääriäinen, M.; Kyngäs, H. The views of compliant glaucoma patients on counselling and social support. Scand. J. Caring Sci. 2010, 24, 490–498. [Google Scholar] [CrossRef]
- Waterman, H.; Brunton, L.; Fenerty, C.; Mottershead, J.; Richardson, C.; Spencer, F. Adherence to ocular hypotensive therapy: Patient health education needs and views on group education. Patient Prefer. Adherence 2013, 7, 55–63. [Google Scholar] [CrossRef][Green Version]
- Why You Need to Take Your Medications as Prescribed or Instructed. FDA. 2018. Available online: https://www.fda.gov/drugs/special-features/why-you-need-take-your-medications-prescribed-or-instructed (accessed on 12 February 2021).
- Vin, A.; Schneider, S.; Muir, K.W.; Rosdahl, J.A. Health coaching for glaucoma care: A pilot study using mixed methods. Clin. Ophthalmol. 2015, 9, 1931–1943. [Google Scholar] [CrossRef]
- Somner, J.E.A.; Sii, F.; Bourne, R.; Cross, V.; Shah, P. What do patients with glaucoma think about personal health records? Ophthalmic Physiol. Opt. 2013, 33, 627–633. [Google Scholar] [CrossRef]
- Killeen, O.J.; MacKenzie, C.; Heisler, M.; Resnicow, K.; Lee, P.P.; Newman-Casey, P.A. User-centered Design of the eyeGuide: A Tailored Glaucoma Behavior Change Program. J. Glaucoma 2016, 25, 815–821. [Google Scholar] [CrossRef]
- Hawkshead, J.; Krousel-Wood, M.A. Techniques for Measuring Medication Adherence in Hypertensive Patients in Outpatient Settings. Dis. Manag. Health Outcomes 2007, 15, 109–118. [Google Scholar] [CrossRef]
- Feldman, R.; Bacher, M.; Campbell, N.; Drover, A.; Chockalingam, A. Adherence to Pharmacologic Management of Hypertension. Can. J. Public Health 1998, 89, I16–I18. [Google Scholar] [CrossRef] [PubMed]
- Arlinghaus, K.R.; Johnston, C.A. The Importance of Creating Habits and Routine. Am. J. Lifestyle Med. 2019, 13, 142–144. [Google Scholar] [CrossRef] [PubMed]
- Schuster, A.K.; Wolfram, C.; Pfeiffer, N.; Finger, R.P. Augenheilkunde 2019—Wo stehen wir: Eine Betrachtung der Versorgungssituation in Deutschland. Ophthalmologe 2019, 116, 829–837. [Google Scholar] [CrossRef]
- Fisher, J.D.; Fisher, W.A.; Misovich, S.J.; Kimble, D.L.; Malloy, T.E. Changing AIDS risk behavior: Effects of an intervention emphasizing AIDS risk reduction information, motivation, and behavioral skills in a college student population. Health Psychol. 1996, 15, 114–123. [Google Scholar] [CrossRef]
- Amico, K.R.; Mugavero, M.; Krousel-Wood, M.A.; Bosworth, H.B.; Merlin, J.S. Advantages to Using Social-Behavioral Models of Medication Adherence in Research and Practice. J. Gen. Intern. Med. 2018, 33, 207–215. [Google Scholar] [CrossRef]
- Alany, R.G. Adherence, persistence and cost-consequence comparison of bimatoprost topical ocular formulations. Curr. Med. Res. Opin. 2013, 29, 1187–1189. [Google Scholar] [CrossRef]
| 1. Narrative stimulus “When was your glaucoma diagnosed and how do you experience it in your daily life? Please tell me everything that comes to mind.” |
| 2. Eye drop management “How about the eye drops that you take, please tell me about that.” |
| 3. Situations leading to non-adherence “Please recall a situation that led you to not using drops. Can you tell me about it?” |
| 4. Doctors visit“Remember the last time you went to the eye doctor and got your prescription for eye drops. Please tell me about it.” |
| 5. Recommendations for other patients “With your experience with glaucoma, what would you recommend to other patients?” |
| 6. Summary question “Do you associate anything else with “drops and glaucoma” that you haven’t spoken of?” |
| Sex | Number |
| female | 12 |
| male | 9 |
| Age [years] | Number |
| 55–70 | 8 |
| 71–80 | 9 |
| 81–90 | 4 |
| mean age ± SD | 73.1 ± 8.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frech, S.; Guthoff, R.F.; Gamael, A.; Helbig, C.; Diener, A.; Ritzke, M.; Wollny, A.; Altiner, A. Patterns and Facilitators for the Promotion of Glaucoma Medication Adherence—A Qualitative Study. Healthcare 2021, 9, 426. https://doi.org/10.3390/healthcare9040426
Frech S, Guthoff RF, Gamael A, Helbig C, Diener A, Ritzke M, Wollny A, Altiner A. Patterns and Facilitators for the Promotion of Glaucoma Medication Adherence—A Qualitative Study. Healthcare. 2021; 9(4):426. https://doi.org/10.3390/healthcare9040426
Chicago/Turabian StyleFrech, Stefanie, Rudolf F. Guthoff, Amin Gamael, Christian Helbig, Annette Diener, Manuela Ritzke, Anja Wollny, and Attila Altiner. 2021. "Patterns and Facilitators for the Promotion of Glaucoma Medication Adherence—A Qualitative Study" Healthcare 9, no. 4: 426. https://doi.org/10.3390/healthcare9040426
APA StyleFrech, S., Guthoff, R. F., Gamael, A., Helbig, C., Diener, A., Ritzke, M., Wollny, A., & Altiner, A. (2021). Patterns and Facilitators for the Promotion of Glaucoma Medication Adherence—A Qualitative Study. Healthcare, 9(4), 426. https://doi.org/10.3390/healthcare9040426






