The Role of Probiotics in Chronic Rhinosinusitis Treatment: An Update of the Current Literature
Abstract
:1. Introduction
2. Microbiota
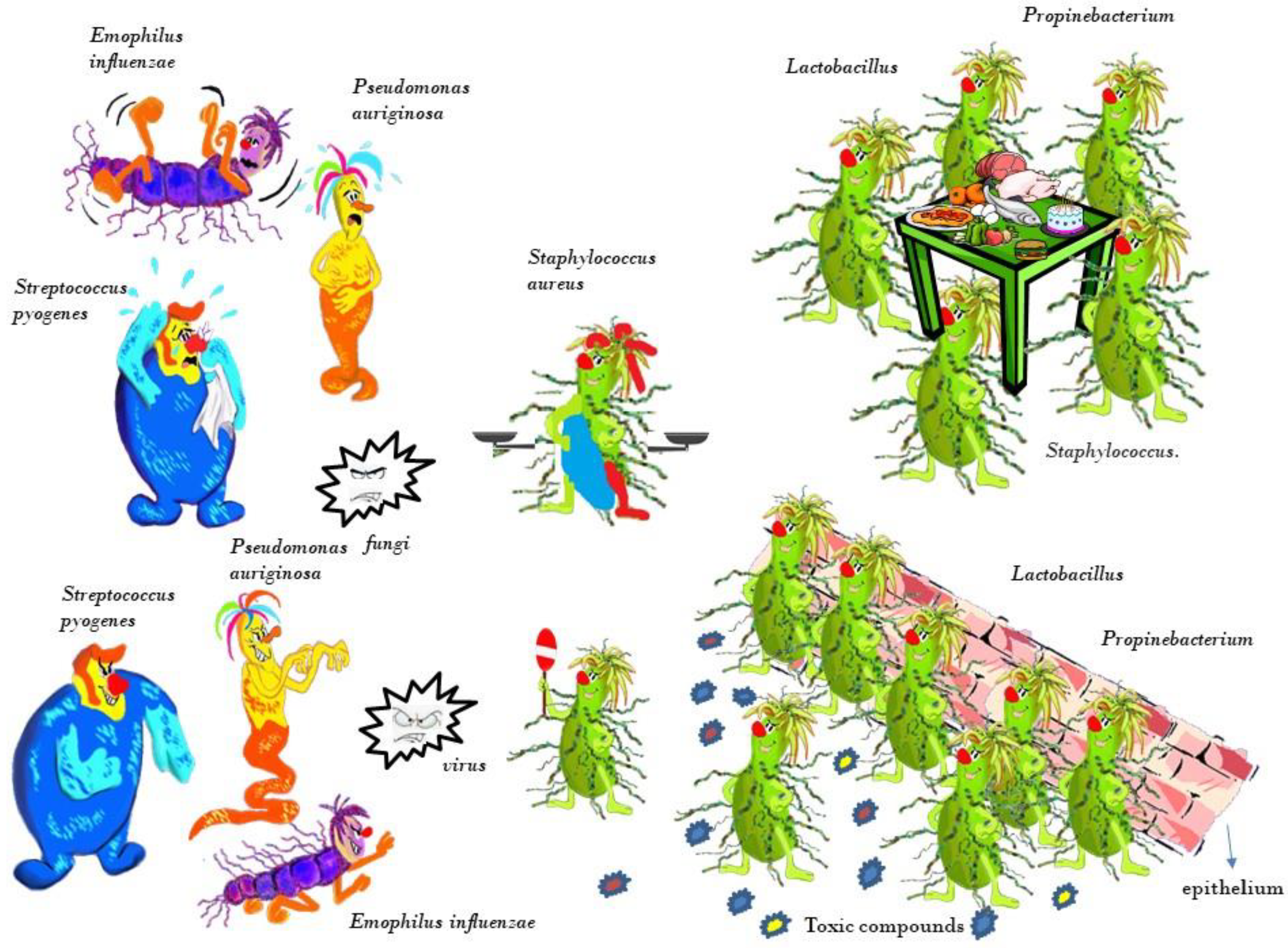
3. Nasal Microbiota
4. Microbiota and Rhinosinusitis
5. Probiotics
6. Clinical Studies
6.1. Clinical Studies That Used Oral Administration of Probiotics
6.2. Clinical Studies That Used Local Administration of Probiotics
7. In Vivo and In Vitro Experimental Studies
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Fokkens, W.J.; Lund, V.J.; Hopkins, C.; Hellings, P.W.; Kern, R.; Reitsma, S.; Toppila-Salmi, S.; Bernal-Sprekelsen, M.; Mullol, J.; Alobid, I.; et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2020. Rhinology 2020, 58 (Suppl. S29), 1–464. [Google Scholar] [CrossRef]
- Benninger, M.S.; Ferguson, B.J.; Hadley, J.A.; Hamilos, D.L.; Jacobs, M.; Kennedy, D.W.; Lanza, D.C.; Marple, B.F.; Osguthorpe, J.D.; Stankiewicz, J.A.; et al. Adult chronic rhinosinusitis: Definitions, diagnosis, epidemiology, and pathophysiology. Otolaryngol. Head Neck Surg. 2003, 129, S1–S32. [Google Scholar] [CrossRef] [PubMed]
- Hastan, D.; Fokkens, W.J.; Bachert, C.; Newson, R.B.; Bislimovska, J.; Bockelbrink, A.; Bousquet, P.J.; Brozek, G.; Bruno, A.; Dahlén, S.E.; et al. Chronic rhinosinusitis in Europe—An underestimated disease. A GA²LEN study. Allergy 2011, 66, 1216–1223. [Google Scholar] [CrossRef] [PubMed]
- Lam, K.; Schleimer, R.; Kern, R.C. The etiology and pathogenesis of chronic rhinosinusitis: A review of current hypotheses. Curr. Allergy Asthma Rep. 2015, 15, 41. [Google Scholar] [CrossRef] [Green Version]
- Bianco, M.R.; Sabatini, U.; Alessio, C.; Chimento, I.; Russo, E.; Allegra, E. Role of anatomical variations in chronic non polipoid rhinosinusitis. Acta Med. Mediterr. 2021, 37, 1203–1208. [Google Scholar]
- Casula, E.; Manca, M.L.; Manconi, M. An integrative review on the uses of plant-derived bioactives formulated in conventional and innovative dosage forms for the local treatment of damaged nasal cavity. Int. J. Pharm. 2021, 610, 121229. [Google Scholar] [CrossRef]
- Ciprandi, G.; La Mantia, I.; Damiani, V.; Passali, D. Local Bacteriotherapy—A promising preventive tool in recurrent respiratory infections. Expert Rev. Clin. Immunol. 2020, 16, 1047–1052. [Google Scholar] [CrossRef]
- Sanders, M.E. Probiotics: Definition, sources, selection, and uses. Clin. Infect. Dis. 2008, 46 (Suppl. 2), S58–S61, discussion S144–S151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ren, J.; Zhao, Y.; Huang, S.; Lv, D.; Yang, F.; Lou, L.; Zheng, Y.; Zhang, J.; Liu, S.; Zhang, N.; et al. Immunomodulatory effect of Bifidobacterium breve on experimental allergic rhinitis in BALB/c mice. Exp. Med. 2018, 16, 3996–4004. [Google Scholar] [CrossRef] [Green Version]
- Choi, S.P.; Oh, H.N.; Choi, C.Y.; Ahn, H.; Yun, H.S.; Chung, Y.M.; Chun, T. Oral administration of Lactobacillus plantarum CJLP133 and CJLP243 alleviates birch pollen-induced allergic rhinitis in mice. J. Appl. Microbiol. 2018, 124, 821–828. [Google Scholar] [CrossRef]
- Kim, W.G.; Kang, G.D.; Kim, H.I.; Han, M.J.; Kim, D.H. Bifidobacterium longum IM55 and Lactobacillus plantarum IM76 alleviate allergic rhinitis in mice by restoringTh2/Treg imbalance and gut microbiota disturbance. Benef Microbes 2019, 10, 55–67. [Google Scholar] [CrossRef]
- La Mantia, I.; Varricchio, A.; Ciprandi, G. Bacteriotherapy with Streptococcus salivarius 24SMB and Streptococcus oralis 89a nasal spray for preventing recurrent acute otitis media in children: A real-life clinical experience. Int. J. Gen. Med. 2017, 10, 171–175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andaloro, C.; Santagati, M.; Stefani, S.; La Mantia, I. Bacteriotherapy with Streptococcus salivarius 24SMB and Streptococcus oralis 89a oral spray for children with recurrent streptococcal pharyngotonsillitis: A randomized placebo-controlled clinical study. Eur. Arch. Otorhinolaryngol. 2019, 276, 879–887. [Google Scholar] [CrossRef] [PubMed]
- Dekaboruah, E.; Suryavanshi, M.V.; Chettri, D.; Verma, A.K. Human microbiome: An academic update on human body site specific surveillance and its possible role. Arch. Microbiol. 2020, 202, 2147–2167. [Google Scholar] [CrossRef]
- Chu, D.M.; Ma, J.; Prince, A.L.; Antony, K.M.; Seferovic, M.D.; Aagaard, K.M. Maturation of the infant microbiome community structure and function across multiple body sites and in relation to mode of delivery. Nat. Med. 2017, 23, 314–326. [Google Scholar] [CrossRef] [Green Version]
- Dominguez-Bello, M.G.; Godoy-Vitorino, F.; Knight, R.; Blaser, M.J. Role of the microbiome in human development. Gut 2019, 68, 1108–1114. [Google Scholar] [CrossRef]
- Bhatt, A.P.; Redinbo, M.R.; Bultman, S.J. The role of the microbiome in cancer development and therapy. CA Cancer J. Clin. 2017, 67, 326–344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DeGruttola, A.K.; Low, D.; Mizoguchi, A.; Mizoguchi, E. Current understanding of dysbiosis in disease in human and animal models. Inflamm. Bowel Dis. 2016, 22, 1137–1150. [Google Scholar] [CrossRef] [Green Version]
- Esposito, S.; Principi, N. Impact of nasopharyngeal microbiota on the development of respiratory tract diseases. Eur. J. Clin. Microbiol. Infect. Dis. 2018, 37, 1–7. [Google Scholar] [CrossRef]
- Huang, Y.J. Nasopharyngeal microbiota: Gatekeepers or fortune tellers of susceptibility to respiratory tract infections? Am. J. Respir Crit. Care Med. 2017, 196, 1504–1505. [Google Scholar] [CrossRef]
- Yan, M.; Pamp, S.J.; Fukuyama, J.; Hwang, P.H.; Cho, D.Y.; Holmes, S.; Relman, D.A. Nasal microenvironments and interspecific interactions influence nasal microbiota complexity and S. aureus carriage. Cell Host Microbe 2013, 14, 631–640. [Google Scholar] [CrossRef] [Green Version]
- Hardy, B.L.; Merrell, D.S. Friend or Foe: Interbacterial Competition in the Nasal Cavity. J. Bacteriol. 2021, 203, e00480-20. [Google Scholar] [CrossRef]
- Kluytmans, J.A.; Wertheim, H.F. Nasal carriage of Staphylococcus aureus and prevention of nosocomial infections. Infection 2005, 33, 3–8. [Google Scholar] [CrossRef]
- Tong, S.Y.; Davis, J.S.; Eichenberger, E.; Holland, T.L.; Fowler, V.G., Jr. Staphylococcus aureus infections: Epidemiology, pathophysiology, clinical manifestations, and management. Clin. Microbiol. Rev. 2015, 28, 603–661. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, E.B.; Hong, S.W.; Kim, D.K.; Jeon, S.G.; Kim, K.R.; Cho, S.H.; Kim, Y.K. Decreased diversity of nasal microbiota and their secreted extracellular vesicles in patients with chronic rhinosinusitis based on a metagenomic analysis. Allergy 2014, 69, 517–526. [Google Scholar] [CrossRef] [PubMed]
- Lal, D.; Keim, P.; Delisle, J.; Barker, B.; Rank, M.A.; Chia, N.; Cope, E.K. Mapping and comparing bacterial microbiota in the sinonasal cavity of healthy, allergic rhinitis, and chronic rhinosinusitis subjects. Int. Forum Allergy Rhinol. 2017, 7, 561–569. [Google Scholar] [CrossRef] [PubMed]
- Dimitri-Pinheiro, S.; Soares, R.; Barata, P. The Microbiome of the Nose—Friend or Foe? Allergy Rhinol. 2020, 11, 2152656720911605. [Google Scholar] [CrossRef] [Green Version]
- De Boeck, I.; Wittouck, S.; Martens, K.; Claes, J.; Jorissen, M.; Steelant, B.; Van den Broek, M.F.L.; Seys, S.F.; Hellings, P.W.; Vanderveken, O.M.; et al. Anterior nares diversity and pathobionts represent sinus microbiome in chronic rhinosinusitis. MSphere 2019, 4, e00532-19. [Google Scholar] [CrossRef] [Green Version]
- Sivasubramaniam, R.; Douglas, R. The microbiome and chronic rhinosinusitis. World J. Otorhinolaryngol. Head Neck Surg. 2018, 4, 216–221. [Google Scholar] [CrossRef]
- Wagner Mackenzie, B.; Waite, D.W.; Hoggard, M.; Douglas, R.G.; Taylor, M.W.; Biswas, K. Bacterial community collapse: A meta-analysis of the sinonasal microbiota in chronic rhinosinusitis. Environ. Microbiol. 2017, 19, 381–392. [Google Scholar] [CrossRef] [PubMed]
- Yamanishi, S.; Pawankar, R. Current advances on the microbiome and role of probiotics in upper airways disease. Curr. Opin. Allergy Clin. Immunol. 2020, 20, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Wood, A.J.; Antoszewska, H.; Fraser, J.; Douglas, R.G. Is chronic rhinosinusitis caused by persistent respiratory virus infection? Int. Forum Allergy Rhinol. 2011, 1, 95–100. [Google Scholar] [CrossRef]
- Zhao, Y.C.; Bassiouni, A.; Tanjararak, K.; Vreugde, S.; Wormald, P.J.; Psaltis, A.J. Role of fungi in chronic rhinosinusitis through ITS sequencing. Laryngoscope 2018, 128, 16–22. [Google Scholar] [CrossRef]
- Zhang, I.; Pletcher, S.D.; Goldberg, A.N.; Barker, B.M.; Cope, E.K. Fungal microbiota in chronic airway inflammatory disease and emerging relationships with the host immune response. Front Microbiol. 2017, 8, 2477. [Google Scholar] [CrossRef] [Green Version]
- Gevers, D.; Knight, R.; Petrosino, J.F.; Huang, K.; McGuire, A.L.; Birren, B.W.; Nelson, K.E.; White, O.; Methé, B.A.; Huttenhower, C. The Human Microbiome Project: A communityresource for the healthy human microbiome. PLoS Biol. 2012, 10, e1001377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fastenberg, J.H.; Hsueh, W.D.; Mustafa, A.; Akbar, N.A.; Abuzeid, W.M. Biofilms in chronic rhinosinusitis: Pathophysiology and therapeutic strategies. World J. Otorhinolaryngol. Head Neck Surg. 2016, 2, 219–229. [Google Scholar] [CrossRef] [Green Version]
- Suh, J.D.; Cohen, N.A.; Palmer, J.N. Biofilms in chronic rhinosinusitis. Curr. Opin. Otolaryngol. Head Neck. Surg. 2010, 18, 27–31. [Google Scholar] [CrossRef]
- Galli, J.; Calò, L.; Ardito, F.; Imperiali, M.; Bassotti, E.; Passali, G.C.; La Torre, G.; Paludetti, G.; Fadda, G. Damage to ciliated epithelium in chronic rhinosinusitis: What is the role of bacterial biofilms. Ann. Otol. Rhinol. Laryngol. 2008, 117, 902–908. [Google Scholar] [CrossRef]
- Ramakrishnan, V.R.; Feazel, L.M.; Gitomer, S.A.; Ir, D.; Robertson, C.E.; Frank, D.N. The microbiome of the middle meatus in healthy adults. PLoS ONE 2013, 8, e85507. [Google Scholar]
- Copeland, E.; Leonard, K.; Carney, R.; Kong, J.; Forer, M.; Naidoo, Y.; Oliver, B.G.G.; Seymour, J.R.; Woodcock, S.; Burke, C.M.; et al. Chronic rhinosinusitis: Potential role of microbial dysbiosis and recommendations for sampling sites. Front. Cell Infect. Microbiol. 2018, 8, 57. [Google Scholar] [CrossRef] [PubMed]
- Gómez-López, A. Microbioma, salud y enfermedad: Probióticos, prebióticos y simbióticos. Biomedica 2019, 39, 617–621. [Google Scholar]
- Williams, N.T. Probiotici. Am. J. Health Syst. Pharm. 2010, 67, 449–458. [Google Scholar] [CrossRef]
- Martens, K.; Pugin, B.; De Boeck, I.; Spacova, I.; Steelant, B.; Seys, S.F.; Lebeer, S.; Hellings, P.W. Probiotics for the airways: Potential to improve epithelial and immune homeostasis. Allergy 2018, 73, 1954–1963. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Boeck, I.; Spacova, I.; Vanderveken, O.M.; Lebeer, S. Lactic acid bacteria as probiotics for the nose? Microb. Biotechnol. 2021, 14, 859–869. [Google Scholar] [CrossRef] [PubMed]
- Habermann, W.; Zimmermann, K.; Skarabis, H.; Kunze, R.; Rusch, V. Reduction of acute recurrence in patients with chronic recurrent hypertrophic sinusitis by treatment with a bacterial immunostimulant (Enterococcus faecalis Bacteriae of human origin). Arzneim. Forsch. 2002, 52, 622–627. [Google Scholar]
- Mukerji, S.S.; Pynnonen, M.A.; Kim, H.M.; Singer, A.; Tabor, M.; Terrell, J.E. Probiotics as adjunctive treatment for chronic rhinosinusitis: A randomized controlled trial. Otolaryngol. Head Neck Surg. 2009, 140, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Mårtensson, A.; Abolhalaj, M.; Lindstedt, M.; Mårtensson, A.; Olofsson, T.C.; Vásquez, A.; Greiff, L.; Cervin, A. Clinical efficacy of a topical lactic acid bacterial microbiome in chronic rhinosinusitis: A randomized controlled trial. Laryngoscope Investig. Otolaryngol. 2017, 2, 410–416. [Google Scholar] [CrossRef]
- Endam, L.M.; Alromaih, S.; Gonzalez, E.; Madrenas, J.; Cousineau, B.; Renteria, A.E.; Desrosiers, M. Intranasal Application of Lactococcus lactis W136 is safe in chronic rhinosinusitis patients with previous sinus surgery. Front. Cell Infect. Microbiol. 2020, 10, 440. [Google Scholar] [CrossRef]
- Schwartz, J.S.; Peres, A.G.; Mfuna Endam, L.; Cousineau, B.; Madrenas, J.; Desrosiers, M. Topical probiotics as a therapeutic alternative for chronic rhinosinusitis: A preclinical proof of concept. Am. J. Rhinol. Allergy. 2016, 30, 202–205. [Google Scholar] [CrossRef]
- Cho, D.Y.; Skinner, D.; Lim, D.J.; Mclemore, J.G.; Koch, C.G.; Zhang, S.; Swords, W.E.; Hunter, R.; Crossman, D.K.; Crowley, M.R.; et al. The impact of Lactococcus lactis (probiotic nasal rinse) co-culture on growth of patient-derived strains of Pseudomonas aeruginosa. Int. Forum. Allergy Rhinol. 2020, 10, 444–449. [Google Scholar] [CrossRef]
- Abreu, N.A.; Nagalingam, N.A.; Song, Y.; Roediger, F.C.; Pletcher, S.D.; Goldberg, A.N.; Lynch, S.V. Sinus microbiome diversity depletion and Corynebacterium tuberculostearicum enrichment mediates rhinosinusitis. Sci. Transl. Med. 2012, 4, 151ra124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cleland, E.J.; Drilling, A.; Bassiouni, A.; James, C.; Vreugde, S.; Wormald, P.J. Probiotic manipulation of the chronic rhinosinusitis microbiome. Int. Forum. Allergy Rhinol. 2014, 4, 309–314. [Google Scholar] [CrossRef] [PubMed]
| Sites of the Nose | Commensal Bacteria |
|---|---|
| Vestibules | Corynebacterium, Propionibavterium, Staphylococcus |
| Nasal cavities | Staphylococcus, Corynebacterium, Dolosigranulum |
| Nasopharynx | Moraxella, Streptococcus, Fusobacterium, Haemophilus |
| Author | Type of Study | Probiotic | N. Patients | Results |
|---|---|---|---|---|
| Habermann et al., 2002 | Multicenter, randomized, double blind, placebo controlled trial | Enterococcus faecalis | 157 | Reduction of CRS flare-ups |
| Mukerji et al., 2009 | prospective, randomized, double-blind, placebo-controlled trial | Lactobacillus rhamnosus | 77 | Transient improvement in the quality of life |
| Author | Type of Study | Probiotic | N. Patients | Results |
|---|---|---|---|---|
| Martensson et al., 2017 | randomized, double-blinded, crossover, and sham-controlled trial | Honeybee lactic acid bacteria | 20 | Not effective |
| Endam et al., 2020 | Prospective open-label pilot trial of safety and feasibility | Lactococcus lactis | 24 | Transient improvement in CRS symptoms |
| Author | Type of Study | Probiotic | Conclusions |
|---|---|---|---|
| Schwartz et al., 2016 | In vitro study | Lactococcus lactis | Absence of cellular toxicity, induction of IL-10 and TNF |
| Cho et al., 2020 | In vitro study | Lactococcus lactis | Lactis nasal washes may not be helpful for all CRS patients |
| Abreu et al., 2012 | In vivo study (mouse) | Lactobacillus sakei | Treatment with L.sakei could counteract the action of C. tuberculostearicum |
| Cleland et al., 2014 | In vivo study (mouse) | Staphylococcus epidermidis | S. epidermidis inhibits the colonization of S. aureus |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bianco, M.R.; Ralli, M.; Modica, D.M.; Amata, M.; Poma, S.; Mattina, G.; Allegra, E. The Role of Probiotics in Chronic Rhinosinusitis Treatment: An Update of the Current Literature. Healthcare 2021, 9, 1715. https://doi.org/10.3390/healthcare9121715
Bianco MR, Ralli M, Modica DM, Amata M, Poma S, Mattina G, Allegra E. The Role of Probiotics in Chronic Rhinosinusitis Treatment: An Update of the Current Literature. Healthcare. 2021; 9(12):1715. https://doi.org/10.3390/healthcare9121715
Chicago/Turabian StyleBianco, Maria Rita, Massimo Ralli, Domenico Michele Modica, Marta Amata, Salvatore Poma, Gianfranco Mattina, and Eugenia Allegra. 2021. "The Role of Probiotics in Chronic Rhinosinusitis Treatment: An Update of the Current Literature" Healthcare 9, no. 12: 1715. https://doi.org/10.3390/healthcare9121715
APA StyleBianco, M. R., Ralli, M., Modica, D. M., Amata, M., Poma, S., Mattina, G., & Allegra, E. (2021). The Role of Probiotics in Chronic Rhinosinusitis Treatment: An Update of the Current Literature. Healthcare, 9(12), 1715. https://doi.org/10.3390/healthcare9121715







