Virtual Reality Rehabilitation’s Impact on Negative Symptoms and Psychosocial Rehabilitation in Schizophrenia Spectrum Disorder: A Systematic Review
Abstract
:1. Introduction
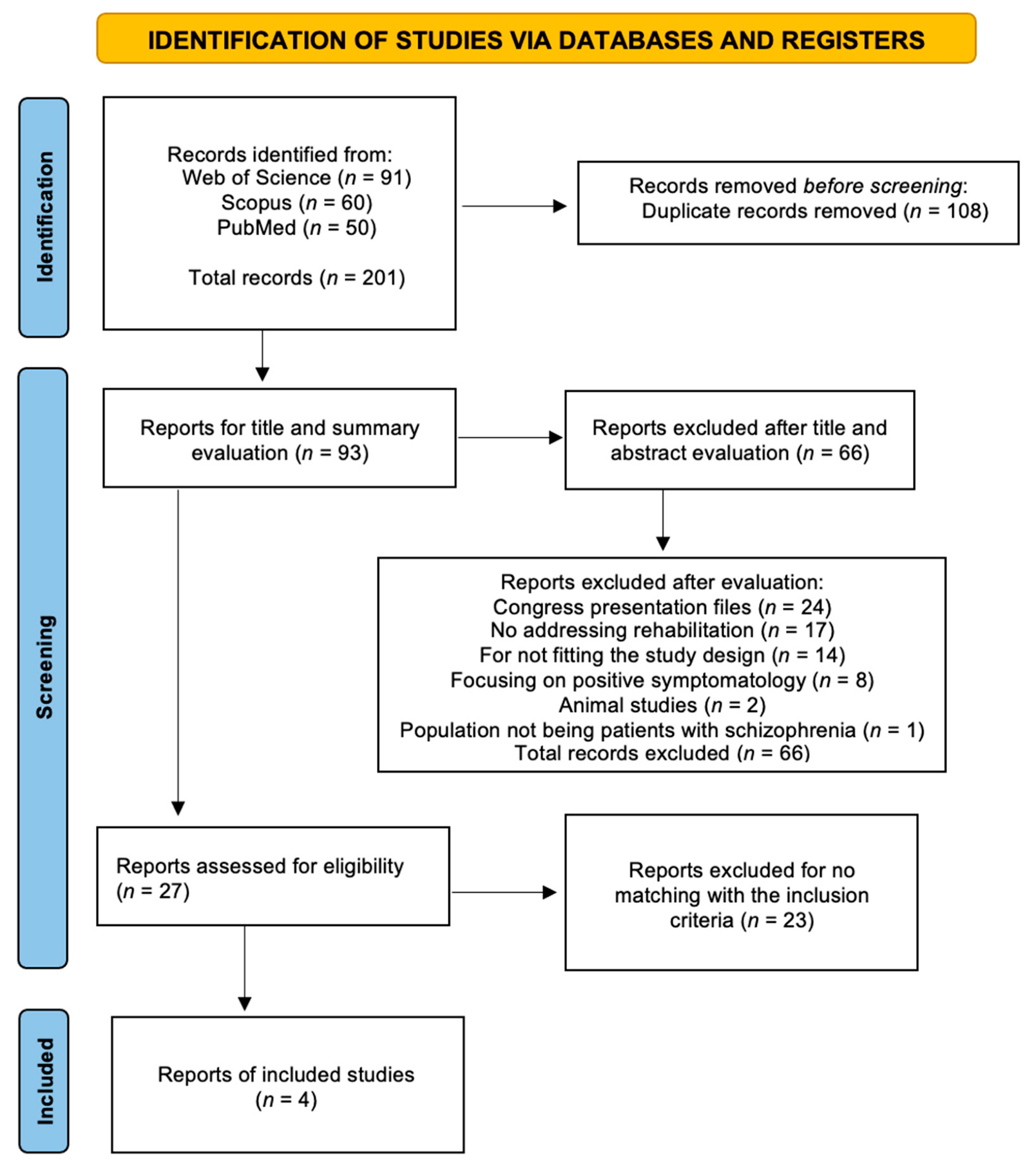
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
- Participants: Patients diagnosed with schizophrenia
- Intervention: Virtual reality exposure therapy
- Comparison: No intervention with virtual reality
- Outcomes to be considered: Negative symptoms and psychosocial functioning
- Study design: Randomized controlled trial
2.3. Data Extraction and Synthesis
- (1)
- Identification: Records were identified through database search and reference screening. All references were exported to the data management software (Rayyan) [18], and all duplicates were removed. After this step, the data were exported to the Mendeley reference manager.
- (2)
- Screening: Two reviewers independently examined the titles and abstracts of studies applying the eligibility criteria, and all irrelevant studies were excluded.
- (3)
- Eligibility and selection: Full reading of the most relevant records was conducted, and all papers not meeting the inclusion criteria were excluded from the systematic review. If there were disagreements, these were resolved by a third reviewer.
- (4)
- Data extraction: Reviewers J.F. and A.N. sought to extract the following data: title, year, authors, study design, sample size, intervention type, DSM, frequency and duration of interventions, purpose of study and assessment methods (Table 1), technology used, intervention outcomes, other results, and conclusion. Pre- and postintervention outcomes were analyzed and measured using specific scales used in each study.
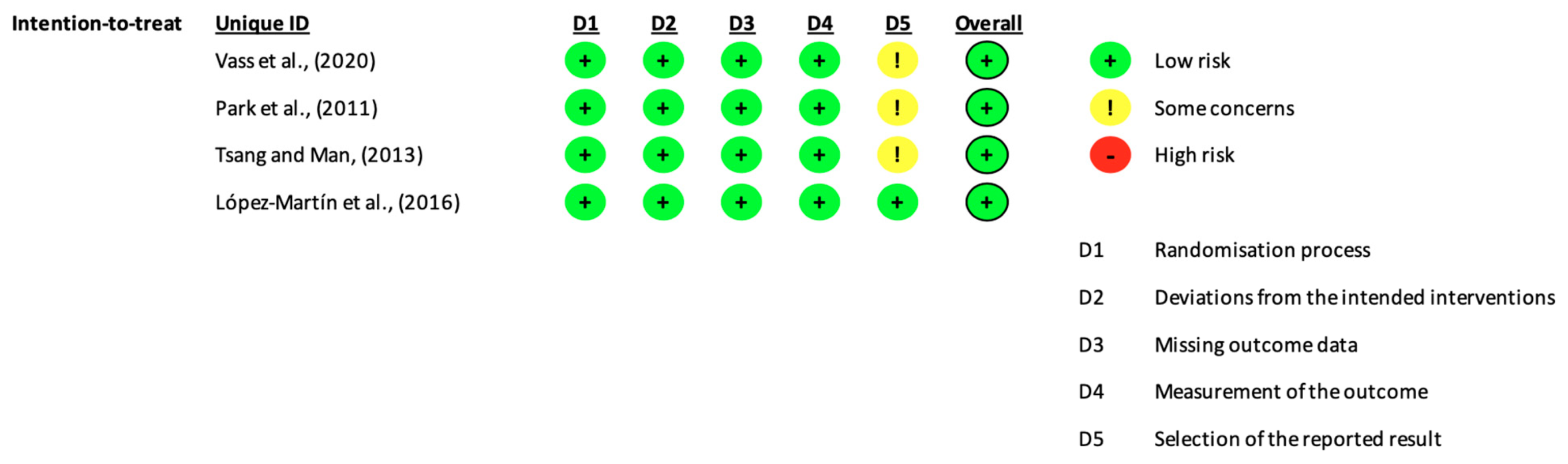
2.4. Risk of Bias Assessment
3. Results
3.1. Characteristics of the Included Studies
3.2. Purpose of Study, Procedures, and Assessment Methods
3.2.1. Purpose and Procedures
3.2.2. Assessment
3.3. Diagnosis
3.4. Technology Used
3.5. Sessions and Samples
3.6. Statistical Results of the Interventions
3.6.1. Negative Symptoms
3.6.2. Cognitive and Functional Outcomes
3.7. Patient Feedback
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barbato, A. Schizophrenia and Public Health; WHO: Geneva, Switzerland, 1997. [Google Scholar]
- Gainsford, K.; Fitzgibbon, B.; Fitzgerald, P.B.; Hoy, K.E. Transforming treatments for schizophrenia: Virtual reality, brain stimulation and social cognition. Psychiatry Res. 2020, 288, 112974. [Google Scholar] [CrossRef]
- Adery, L.H.; Ichinose, M.; Torregrossa, L.J.; Wade, J.; Nichols, H.; Bekele, E.; Bian, D.; Gizdic, A.; Granholm, E.; Sarkar, N.; et al. The acceptability and feasibility of a novel virtual reality based social skills training game for schizophrenia: Preliminary findings. Psychiatry Res. 2018, 270, 496–502. [Google Scholar] [CrossRef] [PubMed]
- Bekele, E.; Bian, D.; Zheng, Z.; Peterman, J.; Park, S.; Sarkar, N. Responses during facial emotional expression recognition tasks using virtual reality and static IAPS pictures for adults with schizophrenia. Int. Conf. Virtual Augment. Mix. Real. 2014, 8526, 225–235. [Google Scholar] [CrossRef]
- Möller, H.J.; Czobor, P. Pharmacological treatment of negative symptoms in schizophrenia. Eur. Arch. Psychiatry Clin. Neurosci. 2015, 265, 567–578. [Google Scholar] [CrossRef] [PubMed]
- Möller, H.-J. The Relevance of Negative Symptoms in Schizophrenia and How to Treat Them with Psychopharmaceuticals? Psychiatr. Danub. 2016, 28, 435–440. [Google Scholar]
- Pourmand, A.; Davis, S.; Lee, D.; Barber, S.; Sikka, N. Emerging Utility of Virtual Reality as a Multidisciplinary Tool in Clinical Medicine. Games Health J. 2017, 6, 263–270. [Google Scholar] [CrossRef]
- Dores, A.R.; Barbosa, F.; Marques, A.; Carvalho, I.P.; De Sousa, L.; Castro-Caldas, A. Realidade virtual na reabilitação: Por que sim e por que não? uma revisão sistemática. Acta Med. Port. 2012, 25, 414–421. [Google Scholar]
- Park, M.J.; Kim, D.J.; Lee, U.; Na, E.J.; Jeon, H.J. A Literature Overview of Virtual Reality (VR) in Treatment of Psychiatric Disorders: Recent Advances and Limitations. Front. Psychiatry 2019, 10, 505. [Google Scholar] [CrossRef] [PubMed]
- Lopes, R.P.; Barroso, B.; Deusdado, L.; Novo, A.; Guimarães, M.; Teixeira, J.P. Digital Technologies for Innovative Mental Health Rehabilitation. Electronics 2021, 10, 2260. [Google Scholar] [CrossRef]
- Bisso, E.; Signorelli, M.S.; Milazzo, M.; Maglia, M.; Polosa, R.; Aguglia, E.; Caponnetto, P. Immersive Virtual Reality Applications in Schizophrenia Spectrum Therapy: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 6111. [Google Scholar] [CrossRef]
- Gregg, L.; Tarrier, N. Virtual reality in mental health. A review of the literature. Soc. Psychiatry Psychiatr. Epidemiol. 2007, 42, 343–354. [Google Scholar] [CrossRef]
- Han, D.H.; Sim, M.E.; Kim, J.I.; Arenella, L.S.; Lyoo, I.K.; Renshaw, P.F. The effect of internet video game play on clinical and extrapyramidal symptoms in patients with schizophrenia. Schizophr. Res. 2008, 103, 338–340. [Google Scholar] [CrossRef]
- Lasaponara, S.; Marson, F.; Doricchi, F.; Cavallo, M. A scoping review of cognitive training in neurodegenerative diseases via computerized and virtual reality tools: What we know so far. Brain Sci. 2021, 11, 528. [Google Scholar] [CrossRef]
- Shimizu, N.; Umemura, T.; Matsunaga, M.; Hirai, T. An interactive sports video game as an intervention for rehabilitation of community-living patients with schizophrenia: A controlled, single-blind, crossover study. PLoS ONE 2017, 12, 1–21. [Google Scholar] [CrossRef]
- Amado, I.; Brenugat-Herne, L.; Orriols, E.; Desombre, C.; Dos Santos, M.; Prost, Z.; Krebs, M.-O.; Piolino, P. A Serious Game to Improve Cognitive Functions in Schizophrenia: A Pilot Study. Front. Psychiatr. 2016, 7, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eldridge, S.; Campbell, M.K.; Campbell, M.J.; Drahota, A.K.; Giraudeau, B.; Reeves, B.; Siegfried, N. Revised Cochrane Risk of Bias Tool for Randomized Trials (RoB 2) Additional Considerations for Cluster-Randomized Trials. Available online: https://sites.google.com/site/riskofbiastool/welcome/rob-2-0-tool (accessed on 1 September 2021).
- Vass, E.; Simon, V.; Fekete, Z.; Lencse, L.; Ecseri, M.; Kis, B.; Simon, L. A novel virtual reality-based theory of mind intervention for outpatients with schizophrenia: A proof-of-concept pilot study. Clin. Psychol. Psychother. 2020, 28, 727–738. [Google Scholar] [CrossRef] [PubMed]
- Park, K.-M.; Ku, J.; Choi, S.-H.; Jang, H.-J.; Park, J.-Y.; Kim, S.I.; Kim, J.J. A virtual reality application in role-plays of social skills training for schizophrenia: A randomized, controlled trial. Psychiatry Res. 2011, 189, 166–172. [Google Scholar] [CrossRef]
- Tsang, M.M.Y.; Man, D.W.K. A virtual reality-based vocational training system (VRVTS) for people with schizophrenia in vocational rehabilitation. Schizophr. Res. 2013, 144, 51–62. [Google Scholar] [CrossRef]
- López-Martín, O.; Segura Fragoso, A.; Rodríguez Hernández, M.; Dimbwadyo Terrer, I.; Polonio-López, B. Efectividad de un programa de juego basado en realidad virtual para la mejora cognitiva en la esquizofrenia. Gac. Sanit. 2016, 30, 133–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barch, D.M. The relationships among cognition, motivation, and emotion in schizophrenia: How much and how little we know. Schizophr. Bull. 2005, 31, 875–881. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Scale | Brief Description |
|---|---|
| Scale | Brief description |
| PANSS | Positive and Negative Syndrome Scale |
| WCST-64 | Wisconsin Card Sorting Test |
| BCMET | Baron-Cohen Mind in the Eyes Test |
| RBANS | Repeated Battery for the Assessment of Neuropsychological Status |
| SBS | Social Behavior Scales |
| RAS | Rathus Assertiveness Schedule |
| RCS | Relationship Change Scale |
| SPSI-R | Social Problem-Solving Inventory—Revised |
| BNCE | Brief Neuropsychological Cognitive Examination |
| DVT | Digit Vigilance Test |
| RBMT | Rivermead Behavioral Memory Test |
| WCST-CV4 | Wisconsin Card Sorting Test—Computer Version 4 |
| VCRS | Vocational Cognitive Rating Scale |
| MCCB-MATRICS | MATRICS Consensus Cognitive Battery (MCCB) |
| Intervention Type | Description |
|---|---|
| VR-ToMIS | Virtual reality (VR)-based targeted theory of mind (ToM). Immersive VR-based targeted ToM intervention that is especially designed for patients with schizophrenia (VR- ToMIS = VR-based ToM Intervention in Schizophrenia) [20] |
| SST-VR and SST-TR | VR role-playing (SST-VR) and SST using traditional role-playing (SST-TR). The virtual environments are used as simulators of the scenes and avatars as actors in VR role-plays, whereas verbal, writing, picture, and video supplies are used as simulators of the scenes. SST therapists are used as actors in TR role-plays [21]. |
| VRVTS | VR-based vocational training system (VRVTS). Inpatients with schizophrenia are randomly assigned to a VR-based vocational training group (VRG), a therapist-administered group (TAG), and a conventional group (CG) [22]. |
| Big Brain Academy game | A virtual reality system and software using the Nintendo® Wii video console [23]. |
| Title 1 | Study Purpose | Study Design | Sample Size | Intervention Type and Duration | DSM | Scales |
|---|---|---|---|---|---|---|
| López-Martín et al. (2016) [21] | To evaluate the effectiveness of a VR-based gaming program for the improvement of cognitive domains in patients with schizophrenia. | RCT | 40 patients Control group (n = 20) Experimental group (n = 20) | Big Brain Academy Game, 5 weeks, 50 min per session | DSM-IV-TR | MCCB-MATRICS |
| Park et al. (2011) [19] | To compare SST using VR role-playing (SST-VR) to SST using traditional role-playing (SST-TR) | RCT | 64 participants SST-VR group (n = 32) SST-TR group (n = 31) | SST-VR and SST-TR, 5 weeks, 90 min per session | DSM-IV Axis I | SBS RAS RCS SPSI-R PANSS |
| Tsang et al. (2013) [20] | To investigate the efficacy and effectiveness of VR as a cognitive intervention for enhancing vocational outcomes. | RCT | 75 participants VR-based training group (VRG, n = 25) Therapist-administered group (TAG, n = 25) Conventional group (CG, n = 25) | VRVTS, 5 weeks, 90 min per session | DSM-IV | BNCE DVT RBMT WCST-CV4 VCRS |
| Vass et al. (2020) [18] | To evaluate the feasibility and tolerability of VR-ToMIS | RCT | 17 patients VR-ToMIS (n = 9) Passive VR (n = 8) | VR-ToMIS and Passive VR, 9 weeks, 50 min per session | DSM-IV-TR | PANSS WCST-64 BCMET RBANS |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Novo, A.; Fonsêca, J.; Barroso, B.; Guimarães, M.; Louro, A.; Fernandes, H.; Lopes, R.P.; Leitão, P. Virtual Reality Rehabilitation’s Impact on Negative Symptoms and Psychosocial Rehabilitation in Schizophrenia Spectrum Disorder: A Systematic Review. Healthcare 2021, 9, 1429. https://doi.org/10.3390/healthcare9111429
Novo A, Fonsêca J, Barroso B, Guimarães M, Louro A, Fernandes H, Lopes RP, Leitão P. Virtual Reality Rehabilitation’s Impact on Negative Symptoms and Psychosocial Rehabilitation in Schizophrenia Spectrum Disorder: A Systematic Review. Healthcare. 2021; 9(11):1429. https://doi.org/10.3390/healthcare9111429
Chicago/Turabian StyleNovo, André, Jéssica Fonsêca, Bárbara Barroso, Manuel Guimarães, Afonso Louro, Hélder Fernandes, Rui Pedro Lopes, and Paulo Leitão. 2021. "Virtual Reality Rehabilitation’s Impact on Negative Symptoms and Psychosocial Rehabilitation in Schizophrenia Spectrum Disorder: A Systematic Review" Healthcare 9, no. 11: 1429. https://doi.org/10.3390/healthcare9111429
APA StyleNovo, A., Fonsêca, J., Barroso, B., Guimarães, M., Louro, A., Fernandes, H., Lopes, R. P., & Leitão, P. (2021). Virtual Reality Rehabilitation’s Impact on Negative Symptoms and Psychosocial Rehabilitation in Schizophrenia Spectrum Disorder: A Systematic Review. Healthcare, 9(11), 1429. https://doi.org/10.3390/healthcare9111429









