The Effect of Social Media Use on Depressive Symptoms in Older Adults with Self-Reported Hearing Impairment: An Empirical Study
Abstract
:1. Introduction
2. Literature Review and Hypothesis Development
2.1. Social Relationship
2.2. Subjective Aging
2.3. Hypothesis Development
2.3.1. Influence of Social Media Use
2.3.2. Subjective Aging
2.3.3. Depressive Symptoms
3. Research Methodology
3.1. Measurement
3.2. Ethical Consideration
3.3. Eligibility Criteria
3.3.1. Inclusion Criteria
- Have experience in using social media and are using social media;
- Are over 60 years old;
- Have self-reported hearing impairment.
3.3.2. Exclusion Criteria
- Have dual sensory loss (hearing and vision).
3.4. Data Collection and Sample
4. Results
4.1. Measurement Model Testing
4.1.1. Common Method Bias and Multicollinearity
4.1.2. Reliability and Validity
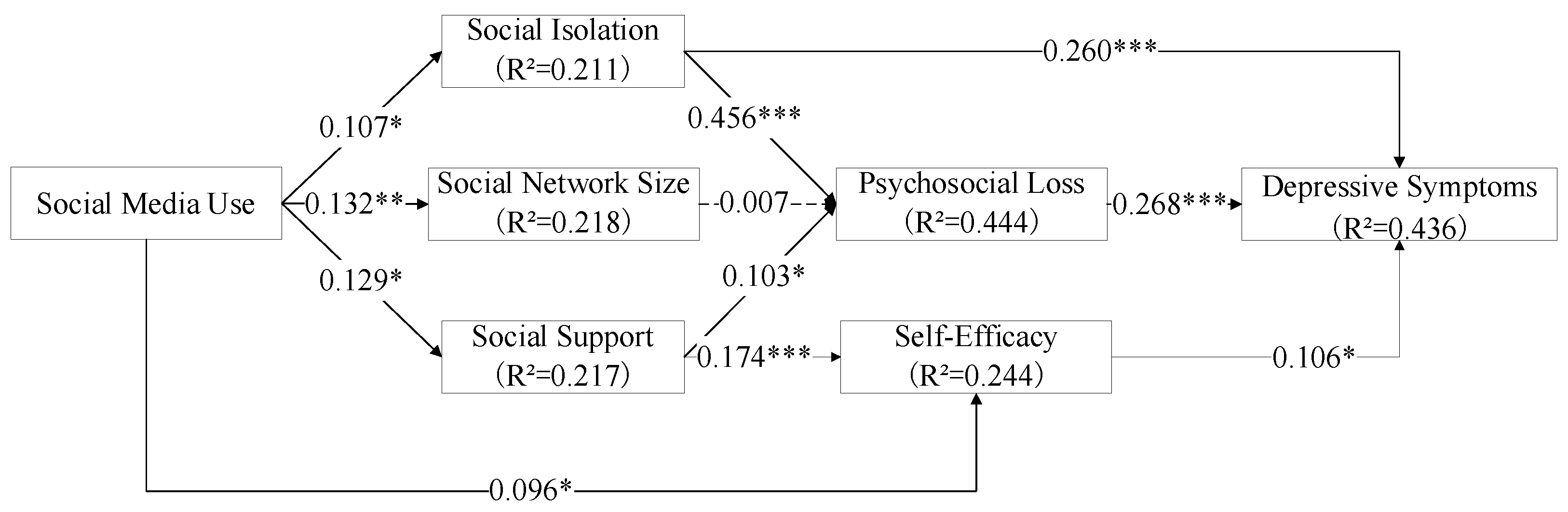
4.2. Structural Model
5. Discussion
5.1. Findings
5.2. Implications for Practice
6. Conclusions and Limitations
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Decade of Healthy Ageing: Baseline Report; 9240017909; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- World Health Organization. World Report on Hearing; 9240020489; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Yang, S.; Huang, L.; Zhang, Y.; Zhang, P.; Zhao, Y.C. Unraveling the links between active and passive social media usage and seniors’ loneliness: A field study in aging care communities. Internet Res. 2021. [Google Scholar] [CrossRef]
- Fu, L.; Teng, T.; Wang, Y.; He, L. Data Analysis Model Design of Health Service Monitoring System for China’s Elderly Pop-ulation: The Proposal of the FW Model Based on the Collaborative Governance Theory of Healthy Aging. Healthcare 2021, 9, 9. [Google Scholar] [CrossRef] [PubMed]
- Khoo, S.S.; Yang, H. Social media use improves executive functions in middle-aged and older adults: A structural equation modeling analysis. Comput. Hum. Behav. 2020, 111. [Google Scholar] [CrossRef]
- Nakagomi, A.; Shiba, K.; Kondo, K.; Kawachi, I. Can online communication prevent depression among older people? A lon-gitudinal analysis. J. Appl. Gerontol. 2020, 733464820982147. [Google Scholar]
- Manchaiah, V.; Bellon-Harn, M.L.; Kelly-Campbell, R.J.; Beukes, E.W.; Bailey, A.; Pyykkő, I. Media Use by Older Adults With Hearing Loss: An Exploratory Survey. Am. J. Audiol. 2020, 29, 218–225. [Google Scholar] [CrossRef] [PubMed]
- Henshaw, H.; Clark, D.P.; Kang, S.; Ferguson, M.A. Computer Skills and Internet Use in Adults Aged 50-74 Years: Influence of Hearing Difficulties. J. Med. Internet Res. 2012, 14, e113. [Google Scholar] [CrossRef]
- Uchida, Y.; Mise, K.; Suzuki, D.; Fukunaga, Y.; Hakuba, N.; Oishi, N.; Ogawa, T.; Takahashi, M.; Takumi, Y.; Fujimoto, S.; et al. A Multi-Institutional Study of Older Hearing Aids Beginners—A Prospective Single-Arm Observation on Executive Function and Social Interaction. J. Am. Med. Dir. Assoc. 2021, 22, 1168–1174. [Google Scholar] [CrossRef] [PubMed]
- Davidson, J.G.S.; Guthrie, D.M. Older Adults With a Combination of Vision and Hearing Impairment Experience Higher Rates of Cognitive Impairment, Functional Dependence, and Worse Outcomes Across a Set of Quality Indicators. J. Aging Health 2017, 31, 85–108. [Google Scholar] [CrossRef]
- Huang, A.R.; Deal, J.A.; Rebok, G.W.; Pinto, J.M.; Waite, L.; Lin, F.R. Hearing Impairment and Loneliness in Older Adults in the United States. J. Appl. Gerontol. 2020, 40, 1366–1371. [Google Scholar] [CrossRef]
- Zhang, K.; Kim, K.; Silverstein, N.M.; Song, Q.; Burr, J.A. Social Media Communication and Loneliness Among Older Adults: The Mediating Roles of Social Support and Social Contact. Gerontology 2020, 61, 888–896. [Google Scholar] [CrossRef]
- Melchiorre, M.G.; Chiatti, C.; Lamura, G.; Torres-Gonzales, F.; Stankunas, M.; Lindert, J.; Ioannidi-Kapolou, E.; Barros, H.; Macassa, G.; Soares, J.F.J. Social Support, Socio-Economic Status, Health and Abuse among Older People in Seven European Countries. PLoS ONE 2013, 8, e54856. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Chang, E.-S. Social Networks among the Older Chinese Population in the USA: Findings from the PINE Study. Gerontology 2017, 63, 238–252. [Google Scholar] [CrossRef]
- Chachamovich, E.; Fleck, M.; Laidlaw, K.; Power, M. Impact of Major Depression and Subsyndromal Symptoms on Quality of Life and Attitudes Toward Aging in an International Sample of Older Adults. Gerontology 2008, 48, 593–602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kotwal, A.A.; Kim, J.; Waite, L.; Dale, W. Social Function and Cognitive Status: Results from a US Nationally Representative Survey of Older Adults. J. Gen. Intern. Med. 2016, 31, 854–862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karlin, N.J.; Weil, J.; Felmban, W.J.G.; Medicine, G. Aging in Saudi Arabia: An exploratory study of contemporary older per-sons’ views about daily life, health, and the experience of aging. Gerontol. Geriatr. Med. 2016, 2, 2333721415623911. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schreurs, K.; Quan-Haase, A.; Martin, K. Problematizing the Digital Literacy Paradox in the Context of Older Adults’ ICT Use: Aging, Media Discourse, and Self-Determination. Can. J. Commun. 2017, 42, 359–377. [Google Scholar] [CrossRef] [Green Version]
- Han, M.; Tan, X.Y.; Lee, R.; Lee, J.K.; Mahendran, R. Impact of Social Media on Health-Related Outcomes Among Older Adults in Singapore: Qualitative Study. JMIR Aging 2021, 4, e23826. [Google Scholar] [CrossRef]
- Mehrabian, A.; Russell, J.A. An Approach to Environmental Psychology; MIT Press: Cambridge, MA, USA, 1974. [Google Scholar]
- Pandita, S.; Mishra, H.G.; Chib, S. Psychological impact of covid-19 crises on students through the lens of Stimu-lus-Organism-Response (SOR) model. Child. Youth Serv. Rev. 2021, 120, 105783. [Google Scholar] [CrossRef]
- Yang, X.; Gu, D.; Wu, J.; Liang, C.; Ma, Y.; Li, J. Factors influencing health anxiety: The stimulus–organism–response model perspective. Internet Res. 2021. [Google Scholar] [CrossRef]
- Cao, X.; Khan, A.N.; Zaigham, G.H.; Khan, N.A. The stimulators of social media fatigue among students: Role of moral dis-engagement. J. Educ. Comput. Res. 2019, 57, 1083–1107. [Google Scholar] [CrossRef]
- Cao, X.; Sun, J. Exploring the effect of overload on the discontinuous intention of social media users: An S-O-R perspective. Comput. Hum. Behav. 2018, 81, 10–18. [Google Scholar] [CrossRef]
- Liu, H.; Liu, W.; Yoganathan, V.; Osburg, V.-S. COVID-19 information overload and generation Z’s social media discontinu-ance intention during the pandemic lockdown. Technol. Forecast. Soc. Chang. 2021, 166, 120600. [Google Scholar] [CrossRef]
- Whelan, E.; Islam, A.N.; Brooks, S. Is boredom proneness related to social media overload and fatigue? A stress–strain–outcome approach. Internet Res. 2020, 30, 869–887. [Google Scholar] [CrossRef]
- Carr, D.; Moorman, S.M. Social relations and aging. In Handbook of Sociology of Aging; Springer: Berlin/Heidelberg, Germany, 2011; pp. 145–160. [Google Scholar]
- Due, P.; Holstein, B.; Lund, R.; Modvig, J.; Avlund, K. Social relations: Network, support and relational strain. Soc. Sci. Med. 1999, 48, 661–673. [Google Scholar] [CrossRef]
- Chen, Y.; Hicks, A.; While, A.E. Loneliness and social support of older people in C hina: A systematic literature review. Health Soc. Care Community 2014, 22, 113–123. [Google Scholar] [CrossRef] [PubMed]
- Ashida, S.; Sewell, D.K.; Schafer, E.J.; Schroer, A.; Friberg, J. Social network members who engage in activities with older adults: Do they bring more social benefits than other members? Ageing Soc. 2019, 39, 1050–1069. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ogawa, T.; Uchida, Y.; Nishita, Y.; Tange, C.; Sugiura, S.; Ueda, H.; Nakada, T.; Suzuki, H.; Otsuka, R.; Ando, F. Hear-ing-impaired elderly people have smaller social networks: A population-based aging study. Arch. Gerontol. Geriatr. 2019, 83, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Shukla, A.; Harper, M.; Pedersen, E.; Goman, A.; Suen, J.J.; Price, C.; Applebaum, J.; Hoyer, M.; Lin, F.R.; Reed, N.S. Hearing Loss, Loneliness, and Social Isolation: A Systematic Review. Otolaryngol. Neck Surg. 2020, 162, 622–633. [Google Scholar] [CrossRef] [PubMed]
- Staudinger, U.M. Images of Aging: Outside and Inside Perspectives. Annu. Rev. Gerontol. Geriatr. 2015, 35, 187–209. [Google Scholar] [CrossRef]
- López-Otín, C.; Blasco, M.A.; Partridge, L.; Serrano, M.; Kroemer, G. The hallmarks of aging. Cell 2013, 153, 1194–1217. [Google Scholar] [CrossRef] [Green Version]
- Schaie, K.W.; Willis, S.L. Handbook of the Psychology of Aging, 7th ed.; Academic Press: New York, NY, USA, 2010. [Google Scholar]
- Brothers, A.; Miche, M.; Wahl, H.-W.; Diehl, M. Examination of Associations among Three Distinct Subjective Aging Constructs and Their Relevance for Predicting Developmental Correlates. J. Gerontol. Ser. B 2015, 72, 547–560. [Google Scholar] [CrossRef]
- Tovel, H.; Carmel, S.; Raveis, V. Relationships among Self-perception of Aging, Physical Functioning, and Self-efficacy in Late Life. J. Gerontol. Ser. B 2017, 74, 212–221. [Google Scholar] [CrossRef] [Green Version]
- Sneed, J.R.; Whitbourne, S.K. Models of the aging self. J. Soc. Issues 2005, 61, 375–388. [Google Scholar] [CrossRef]
- Eum, M.; Kim, H. Relationship between Active Aging and Quality of Life in Middle-Aged and Older Koreans: Analysis of the 2013–2018 KNHANES. Healthcare 2021, 9, 240. [Google Scholar] [CrossRef]
- Boccardi, M.; Boccardi, V. Psychological Wellbeing and Healthy Aging: Focus on Telomeres. Geriatrics 2019, 4, 25. [Google Scholar] [CrossRef] [Green Version]
- Ghisletta, P.; Aichele, S. Quantitative Methods in Psychological Aging Research: A Mini-Review. Gerontology 2017, 63, 529–537. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McAuley, E.; Konopack, J.F.; Motl, R.W.; Morris, K.S.; Doerksen, S.E.; Rosengren, K.R. Physical activity and quality of life in older adults: Influence of health status and self-efficacy. Ann. Behav. Med. 2006, 31, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Hill, R.A.; Dunbar, R.I.M. Social network size in humans. Hum. Nat. 2003, 14, 53–72. [Google Scholar] [CrossRef]
- Khalaila, R.; Vitman-Schorr, A. Internet use, social networks, loneliness, and quality of life among adults aged 50 and older: Mediating and moderating effects. Qual. Life Res. 2017, 27, 479–489. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-H.; Xiao, M.; Wells, R.H. The Effects of Avatars’ Age on Older Adults’ Self-Disclosure and Trust. Cyberpsychology Behav. Soc. Netw. 2018, 21, 173–178. [Google Scholar] [CrossRef]
- Cohen, S.E.; Syme, S. Social Support and Health; Academic Press: Cambridge, MA, USA, 1985. [Google Scholar]
- Hay-McCutcheon, M.J.; Hyams, A.; Yang, X.; Parton, J. Hearing loss and social support in urban and rural communities*. Int. J. Audiol. 2018, 57, 610–617. [Google Scholar] [CrossRef]
- Quan-Haase, A.; Mo, G.Y.; Wellman, B. Connected seniors: How older adults in East York exchange social support online and offline. Inf. Commun. Soc. 2016, 20, 967–983. [Google Scholar] [CrossRef] [Green Version]
- Wu, H.-Y.; Chiou, A.-F. Social media usage, social support, intergenerational relationships, and depressive symptoms among older adults. Geriatr. Nurs. 2020, 41, 615–621. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Lloyd-Evans, B.; Giacco, D.; Forsyth, R.; Nebo, C.; Mann, F.; Johnson, S. Social isolation in mental health: A conceptual and methodological review. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 1451–1461. [Google Scholar] [CrossRef] [Green Version]
- Lawrence, B.J.; Jayakody, D.M.P.; Bennett, R.J.; Eikelboom, R.; Gasson, N.; Friedland, P.L. Hearing Loss and Depression in Older Adults: A Systematic Review and Meta-analysis. Gerontology 2019, 60, e137–e154. [Google Scholar] [CrossRef]
- Ruusuvuori, J.E.; Aaltonen, T.; Koskela, I.; Ranta, J.; Lonka, E.; Salmenlinna, I.; Laakso, M. Studies on stigma regarding hearing impairment and hearing aid use among adults of working age: A scoping review. Disabil. Rehabil. 2019, 43, 436–446. [Google Scholar] [CrossRef] [PubMed]
- Hogeboom, D.L.; McDermott, R.J.; Perrin, K.M.; Osman, H.; Bell-Ellison, B.A. Internet Use and Social Networking among Middle Aged and Older Adults. Educ. Gerontol. 2010, 36, 93–111. [Google Scholar] [CrossRef]
- Litchman, M.L.; Rothwell, E.; Edelman, L.S. The diabetes online community: Older adults supporting self-care through peer health. Patient Educ. Couns. 2018, 101, 518–523. [Google Scholar] [CrossRef]
- Steverink, N.; Westerhof, G.J.; Bode, C.; Dittmann-Kohli, F. The personal experience of aging, individual resources, and sub-jective well-being. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2001, 56, P364–P373. [Google Scholar]
- Kaunonen, M.; Tarkka, M.-T.; Paunonen, M.; Laippala, P. Grief and social support after the death of a spouse. J. Adv. Nurs. 1999, 30, 1304–1311. [Google Scholar] [CrossRef]
- Heffernan, E.; Coulson, N.S.; Henshaw, H.; Barry, J.G.; Ferguson, M.A. Understanding the psychosocial experiences of adults with mild-moderate hearing loss: An application of Leventhal’s self-regulatory model. Int. J. Audiol. 2016, 55 (Suppl. 3), S3–S12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gow, A.J.; Pattie, A.; Whiteman, M.C.; Whalley, L.J.; Deary, I.J. Social support and successful aging: Investigating the rela-tionships between lifetime cognitive change and life satisfaction. J. Individ. Differ. 2007, 28, 103–115. [Google Scholar] [CrossRef]
- Kalfoss, M.H.; Low, G.; Molzahn, A.E. Reliability and validity of the attitudes to ageing questionnaire for Canadian and Norwegian older adults. Scand. J. Caring Sci. 2010, 24, 75–85. [Google Scholar] [CrossRef]
- Maharani, A.; Pendleton, N.; Leroi, I. Hearing Impairment, Loneliness, Social Isolation, and Cognitive Function: Longitudinal Analysis Using English Longitudinal Study on Ageing. Am. J. Geriatr. Psychiatry 2019, 27, 1348–1356. [Google Scholar] [CrossRef]
- Bandura, A. Guide for constructing self-efficacy scales. Self-Effic. Beliefs Adolesc. 2006, 5, 307–337. [Google Scholar]
- Bandura, A. Self-efficacy mechanism in human agency. Am. Psychol. 1982, 37, 122–147. [Google Scholar] [CrossRef]
- Gatti, F.M.; Brivio, E.; Galimberti, C. “The future is ours too”: A training process to enable the learning perception and increase self-efficacy in the use of tablets in the elderly. Educ. Gerontol. 2017, 43, 209–224. [Google Scholar] [CrossRef]
- Ma, Y.; Liang, C.; Gu, D.; Zhao, S.; Yang, X.; Wang, X. How Social Media Use at Work Affects Improvement of Older People’s Willingness to Delay Retirement during Transfer from Demographic Bonus to Health Bonus: Causal Relationship Empirical Study. J. Med. Internet Res. 2021, 23, e18264. [Google Scholar] [CrossRef]
- Jeste, D.V.; Savla, G.N.; Thompson, W.K.; Vahia, I.V.; Glorioso, D.K.; Martin, A.S.; Palmer, B.; Rock, D.; Golshan, S.; Kraemer, H.C.; et al. Association Between Older Age and More Successful Aging: Critical Role of Resilience and Depression. Am. J. Psychiatry 2013, 170, 188–196. [Google Scholar] [CrossRef] [Green Version]
- Mitina, M.; Young, S.; Zhavoronkov, A. Psychological aging, depression, and well-being. Aging 2020, 12, 18765. [Google Scholar] [CrossRef]
- Abbasi, M.; Mirderikvand, F.; Adavi, H.; Hojati, M. The Relationship Between Personality Traits (Neuroticism and Extraversion) and Self-Efficacy with Aging Depression. Salmand 2018, 12, 458–466. [Google Scholar] [CrossRef] [Green Version]
- Heine, C.; Browning, C. Communication and psychosocial consequences of sensory loss in older adults: Overview and reha-bilitation directions. Disabil. Rehabil. 2002, 24, 763–773. [Google Scholar] [CrossRef] [PubMed]
- Cacioppo, J.T.; Hawkley, L.C.; Thisted, R.A. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol. Aging 2010, 25, 453–463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robb, C.E.; De Jager, C.A.; Ahmadi-Abhari, S.; Giannakopoulou, P.; Udeh-Momoh, C.; McKeand, J.; Price, G.; Car, J.; Majeed, A.; Ward, H.; et al. Associations of Social Isolation with Anxiety and Depression During the Early COVID-19 Pandemic: A Survey of Older Adults in London, UK. Front. Psychiatry 2020, 11, 591120. [Google Scholar] [CrossRef]
- Boer, M.; Stevens, G.W.M.; Finkenauer, C.; de Looze, M.E.; Eijnden, R.J.M.V.D. Social media use intensity, social media use problems, and mental health among adolescents: Investigating directionality and mediating processes. Comput. Hum. Behav. 2020, 116, 106645. [Google Scholar] [CrossRef]
- Kuiper, J.S.; Smidt, N.; Zuidema, S.U.; Comijs, H.C.; Voshaar, R.C.O.; Zuidersma, M. A longitudinal study of the impact of social network size and loneliness on cognitive performance in depressed older adults. Aging Ment. Health 2019, 24, 889–897. [Google Scholar] [CrossRef] [Green Version]
- Zhang, R. The stress-buffering effect of self-disclosure on Facebook: An examination of stressful life events, social support, and mental health among college students. Comput. Hum. Behav. 2017, 75, 527–537. [Google Scholar] [CrossRef]
- Nicholson, N.R., Jr.; Feinn, R.; Casey, E.; Dixon, J. Psychometric evaluation of the social isolation scale in older adults. Gerontologist 2020, 60, e491–e501. [Google Scholar] [CrossRef]
- Laidlaw, K.; Power, M.J.; Schmidt, S.; The WHOQOL-OLD Group. The attitudes to ageing questionnaire (AAQ): Development and psychometric properties. Int. J. Geriatr. Psychiatry 2006, 22, 367–379. [Google Scholar] [CrossRef]
- Cheung, S.-K.; Sun, S.Y.K. Assessment of Optimistic Self-Beliefs: Further Validation of the Chinese Version of the General Self-Efficacy Scale. Psychol. Rep. 1999, 85, 1221–1224. [Google Scholar] [CrossRef]
- Rinaldi, P.; Mecocci, P.; Benedetti, C.; Ercolani, S.; Bregnocchi, M.; Menculini, G.; Catani, M.; Senin, U.; Cherubini, A. Validation of the Five-Item Geriatric Depression Scale in Elderly Subjects in Three Different Settings. J. Am. Geriatr. Soc. 2003, 51, 694–698. [Google Scholar] [CrossRef]
- Hair, J.F.; Sarstedt, M.; Ringle, C.M.; Mena, J.A. An assessment of the use of partial least squares structural equation modeling in marketing research. J. Acad. Mark. Sci. 2011, 40, 414–433. [Google Scholar] [CrossRef]
- Podsakoff, P.M.; Organ, D.W. Self-Reports in Organizational Research: Problems and Prospects. J. Manag. 1986, 12, 531–544. [Google Scholar] [CrossRef]
- Mattila, A.S.; Enz, C.A. The Role of Emotions in Service Encounters. J. Serv. Res. 2002, 4, 268–277. [Google Scholar] [CrossRef] [Green Version]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Mark. Sci. 2014, 43, 115–135. [Google Scholar] [CrossRef] [Green Version]
- Fornell, C.; Bookstein, F.L. Two Structural Equation Models: LISREL and PLS Applied to Consumer Exit-Voice Theory. J. Mark. Res. 1982, 19, 440–452. [Google Scholar] [CrossRef] [Green Version]
- Cantor, M.H. Neighbors and friends: An overlooked resource in the informal support system. Res. Aging 1979, 1, 434–463. [Google Scholar] [CrossRef]
- Hope, A.; Schwaba, T.; Piper, A.M. Understanding digital and material social communications for older adults. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Toronto, ON, Canada, 26 April–1 May 2014; pp. 3903–3912. [Google Scholar]
- Bell, C.; Fausset, C.; Farmer, S.; Nguyen, J.; Harley, L.; Fain, W.B. Examining social media use among older adults. In Proceedings of the 24th ACM Conference on Hypertext and Social Media, Paris, France, 2–4 May 2013; pp. 158–163. [Google Scholar]
- Bandura, A.; Adams, N.E. Analysis of self-efficacy theory of behavioral change. Cogn. Ther. Res. 1977, 1, 287–310. [Google Scholar] [CrossRef]
- Cosh, S.; Helmer, C.; Delcourt, C.; Robins, T.G.; Tully, P.J. Depression in elderly patients with hearing loss: Current perspectives. Clin. Interv. Aging 2019, 14, 1471–1480. [Google Scholar] [CrossRef] [Green Version]
- Wänström, G.; Öberg, M.; Rydberg, E.; Lunner, T.; Laplante-Lévesque, A.; Andersson, G. The psychological process from avoidance to acceptance in adults with acquired hearing impairment. Hear. Balance Commun. 2014, 12, 27–35. [Google Scholar] [CrossRef]
- West, J.S. Hearing impairment, social support, and depressive symptoms among US adults: A test of the stress process paradigm. Soc. Sci. Med. 2017, 192, 94–101. [Google Scholar] [CrossRef] [PubMed]

| Latent Variable | Measurement Item | Reference |
|---|---|---|
| Social Media Use | SMU1: How long have you been using social media (years)? | [71] |
| SMU2: How much time per week do you spend on social media? | ||
| SMU3: How many times per day do you respond to messages, photos, or videos of others on social media? | ||
| SMU4: How many times per day do you send a message, photo, or video via your social media? | ||
| Social Network Size | SNS1: I have many family members to keep in touch with. | [72] |
| SNS2: I have many friends to keep in touch with. | ||
| SNS3: I have many good acquaintances to keep in touch with. | ||
| SNS4: I maintain a good relationship with my neighbors. | ||
| Social Isolation | SI1: Overall, I feel that my relationships are fulfilling. | [74] |
| SI2: I feel like I just do not belong. | ||
| SI3: I feel that I spend enough time involved in social activities. | ||
| Social Support | SS1: Someone to give you good advice about a crisis. | [73] |
| SS2: Someone to help with daily chores if you were sick. | ||
| SS3: Someone to confide in or talk to about yourself or your problems. | ||
| SS4: Someone to show you love and affection. | ||
| SS5: Someone to have a good time with. | ||
| Psychosocial Loss | PL1: I do not feel involved in society now that I am older. | [75] |
| PL2: As I get older, I find it more difficult to make new friends. | ||
| PL3: I feel excluded from things because of my age. | ||
| PL4: I find it more difficult to talk about my feelings as I get older. | ||
| PL5: Old age is a depressing time of life. | ||
| PL6: Old age is a time of loneliness. | ||
| Self-Efficacy | SE1: I can always manage to solve difficult problems if I try hard enough. | [76] |
| SE2: If someone opposes me, I can find the means and ways to get what I want. | ||
| SE3: It is easy for me to stick to my aims and accomplish my goals. | ||
| SE4: I am confident that I could deal efficiently with unexpected events. | ||
| SE5: Thanks to my resourcefulness, I know how to handle unforeseen situations. | ||
| SE6: I can solve most problems if I invest the necessary effort. | ||
| SE7: I can remain calm when facing difficulties because I can rely on my coping skills. | ||
| SE8: When I am confronted with a problem, I can usually find several solutions. | ||
| SE9: If I am in trouble, I can usually think of a solution. | ||
| SE10: I can usually handle whatever comes my way. | ||
| Depressive Symptoms | DS1: Are you basically satisfied with your life? | [77] |
| DS2: Do you often get bored? | ||
| DS3: Do you often feel helpless? | ||
| DS4: Do you prefer to stay at home rather than going out and doing new things? | ||
| DS5: Do you feel worthless the way you are now? |
| Measure | Item | Count | Measure | Item | Count |
|---|---|---|---|---|---|
| Gender | Male | 316 (49.14%) | Hearing Loss | One ear | 36 (5.60%) |
| Female | 327 (50.86%) | Both ears | 607 (94.40%) | ||
| Age | 60–64 | 294 (45.72%) | Self-Reported Hearing Disability | Very easy | 266 (41.37%) |
| 65–69 | 187 (29.08%) | Fairly easy | 171 (26.50%) | ||
| 70–74 | 102 (15.86%) | Fairly hard | 143 (22.23%) | ||
| 75–79 | 39 (6.02%) | Very hard | 63 (9.90%) | ||
| >80 | 21 (3.32%) | None | 398 (61.90%) | ||
| Income | <2000 (~USD300) | 173 (26.90%) | Hearing Devices | Cochlear implants | 15 (2.33%) |
| 2000–4000 (~USD300–600) | 203 (31.57%) | Bone-anchored hearing aids | 21 (3.27%) | ||
| 4000–6000 (~USD600–900) | 186 (28.93%) | Air-conduction hearing aids | 177 (27.52%) | ||
| >6000 (~USD900) | 81 (12.60%) | Other | 32 (4.98%) |
| Construct | Item | Mean | SD |
|---|---|---|---|
| Social Isolation | SI1 | 4.918 | 1.596 |
| SI2 | 4.792 | 1.540 | |
| SI3 | 5.056 | 1.602 | |
| Psychosocial Loss | PL1 | 4.900 | 1.601 |
| PL2 | 4.899 | 1.538 | |
| PL3 | 4.844 | 1.613 | |
| PL4 | 4.975 | 1.646 | |
| PL5 | 4.846 | 1.515 | |
| PL6 | 4.967 | 1.634 | |
| Self-Efficacy | SE1 | 5.003 | 1.554 |
| SE2 | 4.928 | 1.584 | |
| SE3 | 5.008 | 1.516 | |
| SE4 | 5.042 | 1.508 | |
| SE5 | 4.997 | 1.506 | |
| SE6 | 4.997 | 1.520 | |
| SE7 | 5.033 | 1.582 | |
| SE8 | 5.036 | 1.584 | |
| SE9 | 4.942 | 1.590 | |
| SE10 | 4.952 | 1.476 | |
| Social Network Size | SNS1 | 5.025 | 1.590 |
| SNS2 | 4.935 | 1.600 | |
| SNS3 | 4.988 | 1.678 | |
| SNS4 | 4.843 | 1.680 | |
| Social Support | SS1 | 4.866 | 1.508 |
| SS2 | 4.827 | 1.563 | |
| SS3 | 4.759 | 1.633 | |
| SS4 | 5.002 | 1.583 | |
| SS5 | 4.966 | 1.564 | |
| Social Media Use | SMU1 | 4.918 | 1.613 |
| SMU2 | 4.946 | 1.616 | |
| SMU3 | 4.751 | 1.517 | |
| SMU4 | 4.988 | 1.523 | |
| Depressive Symptoms | DS1 | 4.986 | 1.591 |
| DS2 | 4.894 | 1.527 | |
| DS3 | 4.946 | 1.675 | |
| DS4 | 4.933 | 1.639 | |
| DS5 | 4.863 | 1.581 |
| Construct | Item | Loading | Cronbach’s Alpha | Rho_A | CR | AVE |
|---|---|---|---|---|---|---|
| Social Isolation | SI1 | 0.826 | 0.765 | 0.770 | 0.865 | 0.680 |
| SI2 | 0.800 | |||||
| SI3 | 0.848 | |||||
| Psychosocial Loss | PL1 | 0.765 | 0.855 | 0.857 | 0.892 | 0.579 |
| PL2 | 0.766 | |||||
| PL3 | 0.756 | |||||
| PL4 | 0.760 | |||||
| PL5 | 0.759 | |||||
| PL6 | 0.758 | |||||
| Self-Efficacy | SE1 | 0.730 | 0.900 | 0.922 | 0.916 | 0.523 |
| SE2 | 0.764 | |||||
| SE3 | 0.726 | |||||
| SE4 | 0.709 | |||||
| SE5 | 0.703 | |||||
| SE6 | 0.720 | |||||
| SE7 | 0.712 | |||||
| SE8 | 0.727 | |||||
| SE9 | 0.714 | |||||
| SE10 | 0.735 | |||||
| Social Network Size | SNS1 | 0.763 | 0.822 | 0.859 | 0.880 | 0.648 |
| SNS2 | 0.853 | |||||
| SNS3 | 0.802 | |||||
| SNS4 | 0.800 | |||||
| Social Support | SS1 | 0.781 | 0.830 | 0.831 | 0.880 | 0.595 |
| SS2 | 0.766 | |||||
| SS3 | 0.763 | |||||
| SS4 | 0.786 | |||||
| SS5 | 0.763 | |||||
| Social Media Use | SMU1 | 0.783 | 0.824 | 0.886 | 0.879 | 0.644 |
| SMU2 | 0.773 | |||||
| SMU3 | 0.859 | |||||
| SMU4 | 0.793 | |||||
| Depressive Symptoms | DS1 | 0.785 | 0.839 | 0.841 | 0.886 | 0.609 |
| DS2 | 0.733 | |||||
| DS3 | 0.816 | |||||
| DS4 | 0.790 | |||||
| DS5 | 0.774 |
| DS | PL | SE | SI | SMU | SNS | SS | |
|---|---|---|---|---|---|---|---|
| DS | 0.780 | ||||||
| PL | 0.406 | 0.761 | |||||
| SE | 0.188 | 0.112 | 0.723 | ||||
| SI | 0.411 | 0.483 | 0.199 | 0.825 | |||
| SMU | 0.125 | 0.142 | 0.118 | 0.107 | 0.803 | ||
| SNS | 0.181 | 0.138 | 0.12 | 0.188 | 0.132 | 0.805 | |
| SS | 0.088 | 0.222 | 0.186 | 0.254 | 0.129 | 0.437 | 0.772 |
| Hypothetical Path | Path Coefficient | T Value | p Value | Conclusion |
|---|---|---|---|---|
| H1 SMU -> SNS | 0.132 | 3.444 | 0.001 | Support |
| H2 SMU -> SS | 0.129 | 2.950 | 0.003 | Support |
| H3 SMU -> SI | 0.107 | 2.505 | 0.013 | Support |
| H4 SNS -> PL | 0.007 | 0.182 | 0.856 | No support |
| H5 SS -> PL | 0.103 | 2.014 | 0.044 | Support |
| H6 SI -> PL | 0.456 | 10.458 | <0.001 | Support |
| H7 SMU -> SE | 0.096 | 2.249 | 0.025 | Support |
| H8 SS -> SE | 0.174 | 4.434 | <0.001 | Support |
| H9 PL -> DS | 0.268 | 6.307 | <0.001 | Support |
| H10 SE -> DS | 0.106 | 3.150 | 0.002 | Support |
| H11 SI -> DS | 0.260 | 6.036 | <0.001 | Support |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ma, Y.; Liang, C.; Yang, X.; Zhang, H.; Zhao, S.; Lu, L. The Effect of Social Media Use on Depressive Symptoms in Older Adults with Self-Reported Hearing Impairment: An Empirical Study. Healthcare 2021, 9, 1403. https://doi.org/10.3390/healthcare9111403
Ma Y, Liang C, Yang X, Zhang H, Zhao S, Lu L. The Effect of Social Media Use on Depressive Symptoms in Older Adults with Self-Reported Hearing Impairment: An Empirical Study. Healthcare. 2021; 9(11):1403. https://doi.org/10.3390/healthcare9111403
Chicago/Turabian StyleMa, Yiming, Changyong Liang, Xuejie Yang, Haitao Zhang, Shuping Zhao, and Liyan Lu. 2021. "The Effect of Social Media Use on Depressive Symptoms in Older Adults with Self-Reported Hearing Impairment: An Empirical Study" Healthcare 9, no. 11: 1403. https://doi.org/10.3390/healthcare9111403
APA StyleMa, Y., Liang, C., Yang, X., Zhang, H., Zhao, S., & Lu, L. (2021). The Effect of Social Media Use on Depressive Symptoms in Older Adults with Self-Reported Hearing Impairment: An Empirical Study. Healthcare, 9(11), 1403. https://doi.org/10.3390/healthcare9111403






