Effect of Four Weeks of Home-Based Balance Training on the Performance in Individuals with Functional Ankle Instability: A Remote Online Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.1.1. Inclusion Criteria
- I.
- At least one severe ankle sprain in the past;
- II.
- The first sprain must have happened at least 12 months before enrolling in the trial;
- III.
- The initial sprain has to be accompanied by inflammatory signs (i.e., pain, edema and so on); at least 1 day of targeted physical activity must have been disrupted by the first injury;
- IV.
- The most recent injury must have occurred at least 3 months before enrolling in the study;
- V.
- Previous ankle joint injury with giving way, recurrent sprain or feelings of instability;
- VI.
- In the 6 months leading up to study enrolment, participants must report at least two occurrences of giving way;
- VII.
- Experiencing a recurring sprain, which is defined as two or more sprains on the same ankle;
- VIII.
- Instability in the ankle joint;
- IX.
- Cumberland Ankle Instability Tool 41: <24 confirmed self-reported ankle instability.
2.1.2. Exclusion Criteria
- I.
- A history of past musculoskeletal surgery in either lower extremity limb;
- II.
- A history of a fracture in one of the lower extremity limbs that necessitated a realignment;
- III.
- Acute damage to the musculoskeletal structures of other joints in the lower extremity in the past 3 months that resulted in at least 1 day of missed physical activity;
- IV.
- Ankle anterior drawer test was positive;
- V.
- Only one training session was missed.
2.2. Sample Power
2.3. Tools and Measurements
2.4. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gribble, P.A.; Robinson, R.H. Alterations in knee kinematics and dynamic stability associated with chronic ankle instability. J. Athl. Train. 2009, 44, 350–355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al Adal, S.; Mackey, M.; Pourkazemi, F.; Hiller, C.E. The relationship between pain and associated characteristics of chronic ankle instability: A retrospective study. J. Sport Health Sci. 2020, 9, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Fu, S.N.; Hui-Chan, C. Modulation of prelanding lower-limb muscle responses in athletes with multiple ankle sprains. Med. Sci. Sports Exerc. 2007, 39, 1774–1783. [Google Scholar] [CrossRef] [PubMed]
- Delahunt, E. Neuromuscular contributions to functional instability of the ankle joint. J. Bodyw. Mov. Ther. 2007, 11, 203–213. [Google Scholar] [CrossRef]
- Marsh, D.W.; Richard, L.A.; Williams, L.A.; Lynch, K.J. The relationship between balance and pitching error in college baseball pitchers. J. Strength Cond. Res. 2004, 18, 441–446. [Google Scholar] [PubMed]
- Gerber, J.P.; Williams, G.N.; Scoville, C.R.; Arciero, R.A.; Taylor, D.C. Persistent disability associated with ankle sprains: A prospective examination of an athletic population. Foot Ankle Int. 1998, 19, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Anandacoomarasamy, A.; Barnsley, L. Long term outcomes of inversion ankle injuries. Br. J. Sports Med. 2005, 39, e14. [Google Scholar] [CrossRef] [Green Version]
- Hubbard, T.J.; Wikstrom, E.A. Ankle sprain: Pathophysiology, predisposing factors, and management strategies. Open Access J. Sports Med. 2010, 1, 115. [Google Scholar] [CrossRef] [Green Version]
- Cruz, A.; Oliveira, R.; Silva, A. Functional ankle instability prevalence and associated risk factors in male football players. Open J. Orthop. 2020, 10, 77. [Google Scholar] [CrossRef] [Green Version]
- Lee, A.J.; Lin, W.-H. Twelve-week biomechanical ankle platform system training on postural stability and ankle proprioception in subjects with unilateral functional ankle instability. Clin. Biomech. 2008, 23, 1065–1072. [Google Scholar] [CrossRef]
- Freeman, M.; Dean, M.; Hanham, I. The etiology and prevention of functional instability of the foot. J Bone Jt. Surg. Br. 1965, 47, 678–685. [Google Scholar] [CrossRef]
- Giza, E.; Fuller, C.; Junge, A.; Dvorak, J. Mechanisms of foot and ankle injuries in soccer. Am. J. Sports Med. 2003, 31, 550–554. [Google Scholar] [CrossRef]
- Hertel, J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J. Athl. Train. 2002, 37, 364. [Google Scholar]
- Santos, M.J.; Liu, H.; Liu, W. Unloading reactions in functional ankle instability. Gait Posture 2008, 27, 589–594. [Google Scholar] [CrossRef]
- Geerinck, A.; Beaudart, C.; Salvan, Q.; Van Beveren, J.; D’Hooghe, P.; Bruyère, O.; Kaux, J.-F. French translation and validation of the Cumberland Ankle Instability Tool, an instrument for measuring functional ankle instability. Foot Ankle Surg. 2020, 26, 391–397. [Google Scholar] [CrossRef]
- Martin, R.L.; Irrgang, J.J.; Burdett, R.G.; Conti, S.F.; Van Swearingen, J.M. Evidence of validity for the Foot and Ankle Ability Measure (FAAM). Foot Ankle Int. 2005, 26, 968–983. [Google Scholar] [CrossRef]
- Clark, V.M.; Burden, A.M. A 4-week wobble board exercise programme improved muscle onset latency and perceived stability in individuals with a functionally unstable ankle. Phys. Ther. Sport 2005, 6, 181–187. [Google Scholar] [CrossRef]
- Mckeon, P.; Ingersoll, C.; Kerrigan, D.C.; Saliba, E.; Bennett, B.; Hertel, J. Balance training improves function and postural control in those with chronic ankle instability. Med. Sci. Sports Exerc. 2008, 40, 1810. [Google Scholar] [CrossRef] [PubMed]
- Hale, S.A.; Hertel, J. Reliability and Sensitivity of the Foot and Ankle Disability Index in Subjects With Chronic Ankle Instability. J. Athl. Train. 2005, 40, 35–40. [Google Scholar]
- Ghram, A.; Briki, W.; Mansoor, H.; Al-Mohannadi, A.S.; Lavie, C.J.; Chamari, K. Home-based exercise can be beneficial for counteracting sedentary behavior and physical inactivity during the COVID-19 pandemic in older adults. Postgrad. Med. 2020, 133, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Vahedian-Azimi, A.; Miller, A.C.; Hajiesmaieli, M.; Kangasniemi, M.; Alhani, F.; Jelvehmoghaddam, H.; Fathi, M.; Farzanegan, B.; Ardehali, S.H.; Hatamian, S. Cardiac rehabilitation using the Family-Centered Empowerment Model versus home-based cardiac rehabilitation in patients with myocardial infarction: A randomised controlled trial. Open Heart 2016, 3, e000349. [Google Scholar] [CrossRef] [Green Version]
- Chindhy, S.; Taub, P.R.; Lavie, C.J.; Shen, J. Current challenges in cardiac rehabilitation: Strategies to overcome social factors and attendance barriers. Expert Rev. Cardiovasc. Ther. 2020, 18, 777–789. [Google Scholar] [CrossRef]
- De Ridder, R.; Willems, T.; Vanrenterghem, J.; Roosen, P. Effect of a home-based balance training protocol on dynamic postural control in subjects with chronic ankle instability. Int. J. Sports Med. 2015, 36, 596–602. [Google Scholar] [CrossRef] [PubMed]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, Ed000142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gribble, P.A.; Delahunt, E.; Bleakley, C.M.; Caulfield, B.; Docherty, C.L.; Fong, D.T.-P.; Fourchet, F.; Hertel, J.; Hiller, C.E.; Kaminski, T.W.; et al. Selection Criteria for Patients With Chronic Ankle Instability in Controlled Research: A Position Statement of the International Ankle Consortium. J. Athl. Train. 2014, 49, 121. [Google Scholar] [CrossRef] [Green Version]
- Hiller, C.E.; Refshauge, K.M.; Bundy, A.C.; Herbert, R.D.; Kilbreath, S.L. The Cumberland ankle instability tool: A report of validity and reliability testing. Arch. Phys. Med. Rehabil. 2006, 87, 1235–1241. [Google Scholar] [CrossRef] [PubMed]
- Hiller, C.E.; Kilbreath, S.L.; Refshauge, K.M. Chronic ankle instability: Evolution of the model. J. Athl. Train. 2011, 46, 133–141. [Google Scholar] [CrossRef] [Green Version]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Rahmat, A.J.; Arsalan, D.; Bahman, M.; Hadi, N. Anthropometrical profile and bio-motor abilities of young elite wrestlers. Phys. Educ. Stud. 2016, 20, 63–69. [Google Scholar] [CrossRef] [Green Version]
- Arazi, H.; Mirzaei, B.; Nobari, H. Anthropometric profile, body composition and somatotyping of national Iranian cross-country runners. Turk. J. Sport Exerc. 2015, 17, 35–41. [Google Scholar] [CrossRef]
- Mazaheri, M.; Salavati, M.; Negahban, H.; Sohani, S.; Taghizadeh, F.; Feizi, A.; Karimi, A.; Parnianpour, M. Reliability and validity of the Persian version of Foot and Ankle Ability Measure (FAAM) to measure functional limitations in patients with foot and ankle disorders. Osteoarthr. Cartil. 2010, 18, 755–759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mattacola, C.G.; Dwyer, M.K. Rehabilitation of the ankle after acute sprain or chronic instability. J. Athl. Train. 2002, 37, 413. [Google Scholar] [PubMed]
- Hale, S.A.; Hertel, J.; Olmsted-Kramer, L.C. The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. J. Orthop. Sports Phys. Ther. 2007, 37, 303–311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hupperets, M.D.; Verhagen, E.A.; Van Mechelen, W. Effect of unsupervised home based proprioceptive training on recurrences of ankle sprain: Randomised controlled trial. BMJ 2009, 339, b2684. [Google Scholar] [CrossRef] [Green Version]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1998. [Google Scholar]
- DeSoto, K.A.; Schweinsberg, M. Replication data collection highlights value in diversity of replication attempts. Sci. Data 2017, 4, 170028. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hunter, P. The reproducibility “crisis”: Reaction to replication crisis should not stifle innovation. EMBO Rep. 2017, 18, 1493–1496. [Google Scholar] [CrossRef] [PubMed]
- Coiera, E.; Ammenwerth, E.; Georgiou, A.; Magrabi, F. Does health informatics have a replication crisis? J. Am. Med. Inform. Assoc. JAMIA 2018, 25, 963–968. [Google Scholar] [CrossRef] [Green Version]
- Lederman, E. Neuromuscular Rehabilitation in Manual and Physical Therapies: Principles to Practice; Elsevier Health Sciences: Amsterdam, The Netherlands, 2010. [Google Scholar]

| Group | n | Age (Years) | p | Weight (kg) | p | Height (cm) | p |
|---|---|---|---|---|---|---|---|
| HBBT | 15 | 23.7 ± 1.4 | 0.704 | 81.1 ± 3.7 | 0.238 | 183.2 ± 5.4 | 0.357 |
| CG | 15 | 23.3 ± 1.2 | 78.6 ± 2.6 | 181.7 ± 4.9 |
| Exercise | Se 1 | Se 2 | Se 3 | Se 4 | Se 5–6 | Se 7–8 | Se 9–10 | Se 11–12 |
|---|---|---|---|---|---|---|---|---|
| A | 1 (3 × 10 s) | 2 (3 × 15 s) | 3 (3 × 15 s) | 3 + 4 (2 × 15 s) | 3 + 4 (2 × 20 s) | 4 + 5 (2 × 15 s) | 5 + 6 (2 × 20 s) | v3 + 6 (2 × 20 s) |
| B | 1 (3 × 10 s) | 1 (3 × 15 s) | 2 (3 × 15 s) | 2 (3 × 20 s) | 3 (3 × 20 s) | 3 (3 × 25 s) | 4 (3 × 20 s) | 4 (3 × 25 s) |
| C | 1 (3 × 5 rp) | 1 (3 × 7 rp) | 2 (3 × 5 rp) | 2 (3 × 7 rp) | 3 (3 × 6 rp) | 3 (3 × 8 rp) | 4 (3 × 5 rp) | 4 (3 × 7 rp) |
| D | 1(3 × 15 rp) | 1 (3 × 15 rp) | 1 (3 × 20 rp) | 1 (3 × 20 rp) | 2 (3 × 10rp) | 2(3 × 12 rp) | 2 (3 × 15 rp) | 2 (3 × 15 rp) |
| E | 1 (3 × 10 rp) | 2 (3 × 10 rp) | 2 (3 × 12 rp) | 3 (3 × 10 rp) | 3 (3 × 12 rp) | 4 (3 × 10 rp) | 4 (3 × 12 rp) |
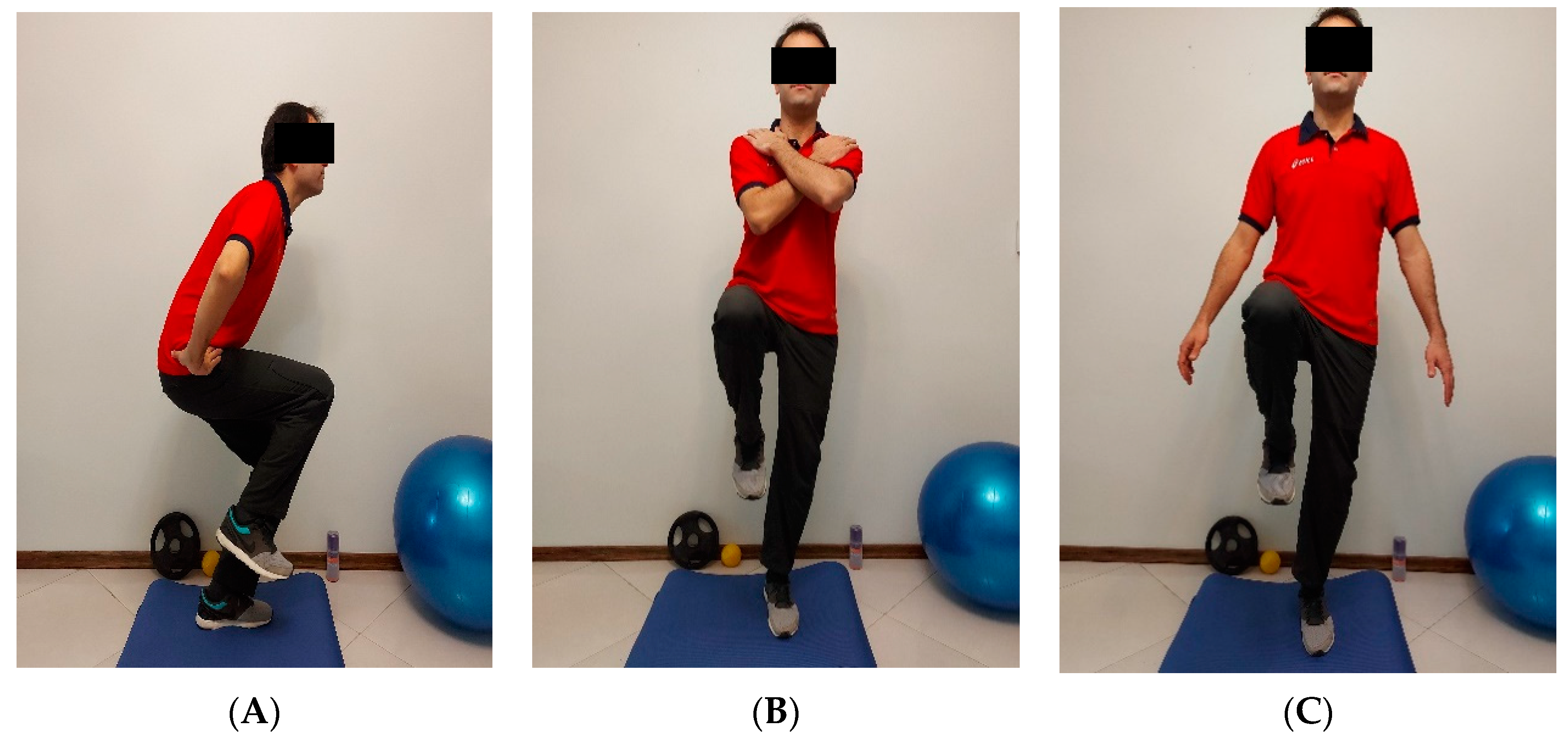
| Movements Training | |
|---|---|
| A. Single leg stance: 1. Firm surface, arms crossed with EO; 2. Firm surface, arms free with EC; 3. Firm surface, arms crossed with EC; 4. Airex, arms crossed with EO; 5. Airex, arms free with EC; 6. Airex, arms crossed with EC. | C. Single leg squat: 1. Firm surface, hands on the hips with EO; 2. Firm surface, hands on the hips with EC; 3. Airex, hands on the hips with EO; 4. Airex, hands on the hips with EC. |
| D. Heel raise: | |
| 1. Firm surface, bilateral with EO; | |
| 2. Firm surface, unilateral with EO. | |
| B. Crossed leg sway: 1. Firm surface, hands on the hips with EO; 2. Airex, hands on the hips with EO; 3. Airex, arms free with EC; 4. Airex, hands on the hips with EC. | E. Lunge/jump exercise: |
| 1. Firm surface, 45 cm to the front with EO; 2. Firm surface, 45 cm to the front and sidelong with EO; 3. Firm surface, 70 cm to the front and sidelong with EO; 4. Airex, 45 cm to the front and sidelong with EO. |
| Questionnaires | Groups | Pre-Training | Post-Training | CI95% for Difference | Hedge’s g (95% CI) |
|---|---|---|---|---|---|
| Values [Lower–Upper] | Values [Lower–Upper] | ||||
| FAAM-daily | HBBT | 6.8 ± 79.7 | 3.5 *# ± 91.9 | 12.3 [8.3 to 16.3] | 2.1 [1.2 to 3.0] |
| CG | 7.7 ± 78.1 | 4.9 ± 81.8 | 3.8 [−1.1 to 8.6] | 0.5 [−0.2 to 1.3] | |
| FAAM-sport | HBBT | 5.9 ± 62.9 | 4.5 *# ± 88.2 | 25.3 [21.4 to 29.2] | 4.5 [3.1 to 5.8] |
| CG | 4.2 ± 61.0 | 5.4 ± 61.9 | 1.0 [−2.7 to 4.6] | 0.2 [−0.5 to 0.9] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seyedi, M.; Nobari, H.; Abbasi, H.; Khezri, D.; Oliveira, R.; Pérez-Gómez, J.; Badicu, G.; Afonso, J. Effect of Four Weeks of Home-Based Balance Training on the Performance in Individuals with Functional Ankle Instability: A Remote Online Study. Healthcare 2021, 9, 1428. https://doi.org/10.3390/healthcare9111428
Seyedi M, Nobari H, Abbasi H, Khezri D, Oliveira R, Pérez-Gómez J, Badicu G, Afonso J. Effect of Four Weeks of Home-Based Balance Training on the Performance in Individuals with Functional Ankle Instability: A Remote Online Study. Healthcare. 2021; 9(11):1428. https://doi.org/10.3390/healthcare9111428
Chicago/Turabian StyleSeyedi, Mohammadreza, Hadi Nobari, Hamed Abbasi, Davood Khezri, Rafael Oliveira, Jorge Pérez-Gómez, Georgian Badicu, and José Afonso. 2021. "Effect of Four Weeks of Home-Based Balance Training on the Performance in Individuals with Functional Ankle Instability: A Remote Online Study" Healthcare 9, no. 11: 1428. https://doi.org/10.3390/healthcare9111428
APA StyleSeyedi, M., Nobari, H., Abbasi, H., Khezri, D., Oliveira, R., Pérez-Gómez, J., Badicu, G., & Afonso, J. (2021). Effect of Four Weeks of Home-Based Balance Training on the Performance in Individuals with Functional Ankle Instability: A Remote Online Study. Healthcare, 9(11), 1428. https://doi.org/10.3390/healthcare9111428












