Connecting the World of Healthcare Virtually: A Scoping Review on Virtual Care Delivery
Abstract
:1. Introduction
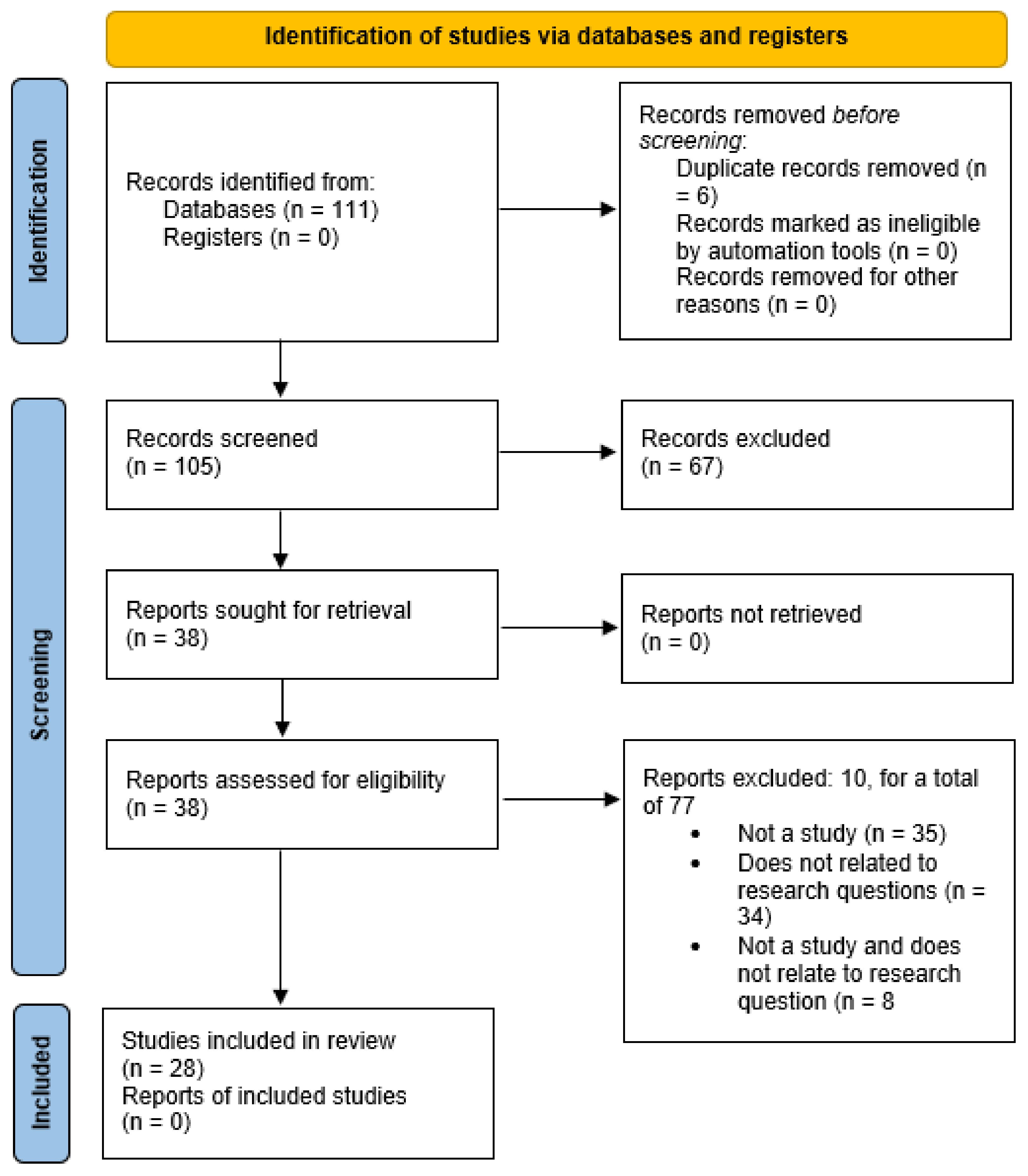
2. Materials and Methods
2.1. Identifying Research Questions
- How is virtual care defined?
- How has virtual care influenced the healthcare industry?
- How is virtual care being expanded to complement the existing healthcare system?
- What are the outcomes of virtual care for patients’ and caregivers’ perspectives?
2.2. Identifying Relevant Studies
2.3. Selecting Studies
2.4. Data Charting
2.5. Dissemination of Results
3. Results
3.1. Definition of Virtual Care
3.2. Influence of Virtual Care on the Healthcare Industry
3.2.1. Pain and Anxiety Management
3.2.2. Virtual Consultations and Follow-Up Visits
3.2.3. Rehabilitation and Therapy Services
3.2.4. Outpatient Care
- 98/107 (91.6%) patients in the virtual outpatient clinic group were successfully contacted.
- 83/102 (81.4%) patients in the outpatient clinic group were successfully contacted.
- 10 patients in the virtual outpatient clinic group reported ongoing issues.
- 6 patients in the outpatient clinic group reported ongoing issues.
- 78/82 (95%) of patients in the virtual outpatient clinic group were happy with their overall experience.
- 34/61 (56%) of patients in the outpatient clinic group were happy with their overall experience.
- 68/81 (83%) of patients in the virtual outpatient clinic group preferred a virtual outpatient clinic appointment in the future.
- 41/61 (67%) of patients in the outpatient clinic group preferred a virtual outpatient clinic appointment in the future.
3.2.5. Emergency Services
3.3. Expansion of Virtual Care to Complement the Existing Healthcare System
3.3.1. Online Training Platforms
3.3.2. Virtual Reality
3.3.3. Virtual Patients
3.4. Consumer Perspectives on Virtual Care
3.4.1. Patient Perspectives
3.4.2. Provider Perspectives
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Article# (In Order of Which it Was Processed in Covidence®) | Article Name and Author | Exclusion Reason |
|---|---|---|
| 108 | Ackerman 2017 Ackerman, Mary Lou; Virani, Tazim; Billings, Barry Digital Mental Health—Innovations in Consumer-Driven Care Nursing Leadership (1910-622X) 2017;30(3):63–72 2017 | Does not discuss application of virtual care tool |
| 6 | Adams 2011 Adams, E. C.; Rodgers, C. J.; Harrington, R.; Young, M. D. B.; Sieber, V. K. How we created virtual patient cases for primary care-based learning Medical Teacher 2011;33(4):273–278 2011 | Is not a study |
| 104 | Agnola 2018 Agnola, Danny Transforming digital health services in Australia Journal of Pharmacy Practice & Research 2018;48(3):283–286 2018 | Only provides high-level overview of digital health strategy in Australia and not virtual care |
| 46 | Anderson 2001 Anderson DG; Stenzel C Internet patient care applications in ambulatory care Journal of Ambulatory Care Management 2001;24(4):1–38 2001 | Does not relate to research questions |
| 40 | Arndt 2018 Arndt, Rachel Z. Providing virtual care from the other side of the globe Modern Healthcare 2018;48(32):0030–0030 2018 | Is not a study |
| 100 | Arndt 2018 Arndt, Rachel Z. Physical therapy and rehab go virtual Modern Healthcare 2018;48(26/27):0030–0030 2018 | Is not a study |
| 39 | Bashford 2011 Bashford, Curt POINT OF VIEW. Virtual Care: How telemedicine is transforming the delivery of emergency medical services in the field EMS World 2011;40(10):31–35 2011 | Is not a study |
| 78 | Bhattacharyya 2017 Bhattacharyya, Rahul; Jayaram, Prem Ruben; Holliday, Robin; Jenkins, Paul; Anthony, Iain; Rymaszewski, Lech The virtual fracture clinic: Reducing unnecessary review of clavicle fractures Injury 2017;48(3):720–723 2017 | Does not relate to research questions |
| 11 | Butler 2014 Butler, Anneliese; Canamucio, Anne; Macpherson, David; Skoko, Jennifer; True, Gala Primary care staff perspectives on a virtual learning collaborative to support medical home implementation JGIM: Journal of General Internal Medicine 2014;29(2):579–588 2014 | Is not a study |
| 92 | Carolan-Rees 2015 Carolan-Rees, G; Ray, Af The ScanTrainer obstetrics and gynaecology ultrasound virtual reality training simulator: A cost model to determine the cost viability of replacing clinical training with simulation training Ultrasound 2015;23(2):110–115 2015 | Does not relate to research questions |
| 105 | Charalambous 2019 Charalambous, Andreas Utilizing the Advances in Digital Health Solutions to Manage Care in Cancer Patients Asia Pac J Oncol Nurs 2019;6(3):234–237 2019 | Does not relate to virtual care |
| 86 | Chen 2019 Chen, Hang; Wang, Xianfeng Sharp Reilly-type inequalities for a class of elliptic operators on submanifolds Differential Geometry and its Applications 2019;63:1–29 2019 | Does not relate to virtual care |
| 64 | Crabb 2019 Crabb, Stephanie Digital Health: Promise, Perils, and Perspective Journal of AHIMA 2019;90(5):32–35 2019 | Is not a study |
| 4 | Dorn 2019 Dorn, Spencer D. Gastroenterologists Without Borders: Using Virtual Care to Reach Beyond the Clinic Walls Gastroenterology 2019; 157(2): 2019 | Is not a study |
| 62 | DupuitsFMH 2002 Dupuits FMH The effects of the Internet on pharmaceutical consumers and providers Disease Management & Health Outcomes 2002;10(11):679–691 2002 | Does not relate to virtual care |
| 24 | Ferenc 2015 Ferenc, Jeff Virtual care center connects worlds of technology and nature Health Facilities Management 2015;28(12):6–6 2015 | Is not a study |
| 48 | Ferenc 2016 Ferenc, Jeff Spreading telehealth know-how to other hospitals H&HN: Hospitals & Health Networks 2016;90(8):20–20 2016 | Is not a study |
| 61 | Fotsch 1998 Fotsch E Internet. Medical intranets create virtual healthcare malls hfm (Healthcare Financial Management) 1998;52(1):26–26 1998 | Is not a study |
| 58 | Fowler 2014 Fowler, Christianne; Haney, Tina; Rutledge, Carolyn M. An Interprofessional Virtual Healthcare Neighborhood for Caregivers of Elderly With Dementia Journal for Nurse Practitioners 2014;10(10):829–834 2014 | Is not a study |
| 33 | Fronczek 2019 Fronczek, Ann E. Nursing Theory in Virtual Care Nursing Science Quarterly 2019;32(1):35–38 2019 | Only talks about theory |
| 2 | Gavarkovs 2019 Gavarkovs, Adam G. Behavioral Counseling Training for Primary Care Providers: Immersive Virtual Simulation as a Training Tool Front. Public Health 2019;9(7):116 2019 | Does not relate to research questions |
| 59 | Grube 2015 Grube, Mark E Making the Case for Virtual Healthcare. What CEOs and trustees need to know about this emerging field Healthcare Executive 2015;30(2):68–68 2015 | Is not a study |
| 35 | Hafner-Fogarty 2018 Hafner-Fogarty, Rebecca mHEALTH UPDATE. THE NEED GROWS TO INCREASE ACCESS TO VIRTUAL CARE For the Record (Great Valley Publishing Company, Inc.) 2018;30(10):33–33 2018 | Is not a study |
| 87 | Hilton 2017 Hilton, Lisette Create a virtual HS clinic Dermatology Times 2017;38(6):23–43 2017 | Does not relate to research questions |
| 47 | Hogan 2018 Hogan, Timothy P.; Luger, Tana M.; Volkman, Julie E.; Rocheleau, Mary; Mueller, Nora; Barker, Anna M.; Nazi, Kim M.; Houston, Thomas K.; Bokhour, Barbara G. Patient Centeredness in Electronic Communication: Evaluation of Patient-to-Health Care Team Secure Messaging Journal of Medical Internet Research 2018;20(3):26–26 2018 | Does not relate to virtual care |
| 81 | Jelliman 2016 Jelliman, Pauline; Downes, Bob; Mannix, Tracy; Foote, Liz; Chaponda, Mas HIV community virtual clinic: an innovative service development to ensure the needs those who cannot attend hospital HIV clinics are effectively met HIV Nursing 2016;16(2):58–58 2016 | Is not a study |
| 15 | Jennings 2017 Jennings, Terry ‘Virtual clinics’ a success story for BOP renal service Kai Tiaki Nursing New Zealand 2017;23(9):22–24 2017 | Is not a study |
| 1 | Johnston 2016 Johnston, Barb; Yellowlees, Peter Telepsychiatry Consultations in Primary Care Coordinated by Virtual Care Navigators PS 2016;67(1):142–142 2016 | Is not a study |
| 45 | Kehoe 2016 Kehoe, Bob Health network advances virtual care visits for chronic diseases Health Facilities Management 2016;29(5):7–7 2016 | Is not a study |
| 69 | Ketchell 2018 Ketchell, Robert Ian Telemedicine is the way forward for the management of cystic fibrosis—the case in favour Paediatric Respiratory Reviews 2018; 26:19–21 2018 | Does not relate to research questions |
| 34 | Kulkarni 2019 Kulkarni, Ameya Navigating Loneliness in the Era of Virtual Care New England Journal of Medicine 2019;380(4):307–309 2019 | Does not relate to research questions |
| 107 | Landi 2018 Landi, Heather Digital Health Leaders, Cardiologists Ponder the Launch of Apple’s New ECG Device Healthcare Informatics 2018 2018 | Does not relate to virtual care |
| 37 | Litwin 2019 Litwin, Sasha; Canning, Matthew; Clemens, Julia; Danukarjanto, Claire; Vandenbergh, Nancy; Wallace, Emma; Ostrow, Olivia 114 Virtual care as a quality improvement intervention to reduce low-acuity return visits to the paediatric emergency department... 96th Annual Conference of the Canadian Paediatric Society, June 6–8 2019, Toronto, Canada Paediatrics & Child Health (1205–7088) 2019;24(): e43–e44 2019 | Is not a study |
| 94 | Lougheed 2019 Lougheed, Tim Time to embrace the promise of virtual health care CMAJ: Canadian Medical Association Journal 2019;191(11): E320–E321 2019 | Does not relate to research questions |
| 74 | Lowery 2014 Lowery, Bobby; Corbett, Robin Webb; King, Carol Ann; Brown, Sylvia T.; Faser, Jr., Karl E. Virtual Clinic—Opening the Clinic Door to Interprofessional Education and Practice Journal for Nurse Practitioners 2014;10(10): e69–e76 2014 | Does not relate to research questions |
| 12 | Mace 2015 Mace, Scott The reality of virtual care Healthcare Leadership Review 2015;25(7):1–8 2015 | Is not a study |
| 44 | Mace 2015 Mace, Scott Diversification and Virtual Care Services HealthLeaders Magazine 2015;18(3):22–23 2015 | Does not relate to research questions |
| 106 | MacLeod 2018 MacLeod, Janice Digital Health Technology in Diabetes Care: It’s transforming the way people with diabetes communicate with personal health care teams and treat and manage their disease Today’s Dietitian 2018;20(8):40–43 2018 | Does not relate to research questions |
| 95 | McLaughlin 2016 McLaughlin, Kelly Virtual psychology clinic helps the hard to reach Journal of Physiotherapy 2016;62(2):120 2016 | Is not a study |
| 67 | Montayre 2018 Montayre, Jed Nursing the future: Braving possibilities, challenges and dilemmas Nursing Praxis in New Zealand 2018;34(1):5–6 2018 | Does not relate to virtual care |
| 109 | Nunn 2016 Nunn, Sandra Watson Joins the Digital Health Record Mix Radiology Today 2016;17(12):22–25 2016 | Is not a study Does not relate to virtual care |
| 60 | Pallarito 1996 Pallarito K Virtual healthcare—linking firms to form all-star teams Modern Healthcare 1996;26(12):42–47 1996 | Does not relate to research questions |
| 43 | Palmer 2018 Palmer, Sarah Jane Virtual care: smartphone apps launched for atrial fibrillation British Journal of Cardiac Nursing 2018;13(1):40–41 2018 | Is not a study |
| 42 | Pearson 2018 Pearson, John F.; Rodriguez, Jorge A.; Safran, Charles Virtual Care as a Specialty JAMA: Journal of the American Medical Association 2018;319(24):2559–2560 2018 | Is not a study |
| 56 | Real 2017 Real, Francis J.; DeBlasio, Dominick; Samaan, Zeina; Beck, Andrew F.; Klein, Melissa D.; McLinden, Daniel; Ollberding, Nicholas J.; Davis, David; Cruse, Bradley A Virtual Reality Curriculum for Pediatric Residents Decreases Rates of Influenza Vaccine Refusal Academic Pediatrics 2017;17(4):431–435 2017 | Does not relate to research questions |
| 85 | Roberts 2015 Roberts, Simon; Spain, Brian; Hicks, Chelsea; London, James; Tay, Stanley Telemedicine in the Northern Territory: An assessment of patient perceptions in the preoperative anaesthetic clinic Australian Journal of Rural Health 2015;23(3):136–141 2015 | Does not relate to virtual care |
| 13 | Roth 2019 Roth, Mandy Virtual care is no longer optional: What’s now, what’s next, and how to get there Healthcare Leadership Review 2019;38(2):1–5 2019 | Is not a study |
| 17 | Rothschild 2003 Rothschild SK; Lapidos S Virtual integrated practice: integrating teams and technology to manage chronic disease in primary care Journal of Medical Systems 2003;27(1):85–93 2003 | Does not relate to research questions |
| 63 | Russell 2018 Russell, Amy; Spence, Brian Virtual Simulation in Radiologic Science Education Radiologic Technology 2018;90(2):169–171 2018 | Does not relate to research questions Does not relate to virtual care |
| 77 | Sechi 2016 Sechi, A.; Sawyer, E.; Ng, W.; Connor, S. Proving cost-effectiveness through implementation of a nurse-led inflammatory bowel disease (IBD) patient advice line and virtual clinic (CHEAP) J. GENCA 2016;26(2):4–6 2016 | Is not a study Does not relate to research questions |
| 66 | Shah 2013 Shah, B; Campbell, P; Ford, C; Goyal, S; Lim, K S Re: The Portsmouth-based refinement scheme: a role for virtual clinics in the future? Eye (Lond). 2012 Oct;26(10):1288–94 Eye 2013;27(7):892–893 2013 | Is not a study Does not relate to research questions |
| 14 | Shaw 2018 Shaw, James; Jamieson, Trevor; Agarwal, Payal; Griffin, Bailey; Wong, Ivy; Bhatia, R. Sacha Virtual care policy recommendations for patient-centred primary care: findings of a consensus policy dialogue using a nominal group technique J Telemed Telecare 2018;24(9):608–615 2018 | Does not relate to research questions |
| 55 | SilvadosSantos 2017 Silva dos Santos, Gabriela; de Melo Tavares, Cláudia Mara; de Faria Pereira, Cosme Sueli; Eleutério Ferreira, Rejane Reflective Analysis Article Reflections on the Use of Virtual Social Networks in Care for Persons with Chronic Disease Journal of Nursing UFPE/Revista de Enfermagem UFPE 2017;11(2):724–730 2017 | Does not relate to virtual care Does not relate to research questions |
| 83 | Succar 2013 Succar, T; Zebington, G; Billson, F; Byth, K; Barrie, S; McCluskey, P; Grigg, J The impact of the Virtual Ophthalmology Clinic on medical students’ learning: a randomised controlled trial Eye 2013;27(10):1151–1157 2013 | Does not relate to virtual care |
| 52 | TuaniCandidodeOliveiraSalvador 2018 Tuani Candido de Oliveira Salvador, Pétala; dos Santos Mariz, Camila Maria; Fortes Vítor, Allyne; Ferreira Júnior, Marcos Antônio; Domingues Fernandes, Maria Isabel; Amado Martins, José Carlos; Pereira Santos, Viviane Euzébia Validation of virtual learning object to support the teaching of nursing care systematization Revista Brasileira de Enfermagem 2018;71(1):11–19 2018 | Does not relate to research questions Does not relate to virtual care |
| 51 | Yeun-SimJeong 2019 Yeun-Sim Jeong, Sarah; Kwang-Ok Lee The Emergence of Virtual Reality Simulation and Its Implications for Nursing Profession Korean Journal of Women Health Nursing 2019;25(2):125–128 2019 | Is not a study |
| 32 | Zhu 2019 Zhu, Xi; Tu, Shin-Ping; Sewell, Daniel; Yao, Nengliang (Aaron); Mishra, Vimal; Dow, Alan; Banas, Colin Measuring electronic communication networks in virtual care teams using electronic health records access-log data International Journal of Medical Informatics 2019;128(): 46–52 2019 | Does not relate to research questions Does not relate to virtual care |
| 102 | The virtual hypertension clinic | Ovid ;(): | Is not a study Does not relate to research questions |
| 38 | Research Shows Virtual Care’s Impact on Patient Acquisition For the Record (Great Valley Publishing Company, Inc.) 2018;30(5):27–27 2018 | Is not a study |
| 10 | Patients embrace virtual care more than physicians Healthcare Leadership Review 2018;37(8):12–12 2018 | Is not a study |
| 57 | NHS doctors train using virtual reality to improve care for people with diabetes Operating Theatre Journal 2019;(345):4–4 2019 | Is not a study Does not relate to research questions |
| 93 | Jeffrey S. Gurock. The Jews of Harlem: The Rise, Decline, and Revival of a Jewish Community. | The American Historical Review | Oxford Academic 2018;123(2): 598-599 | Does not relate to research questions Does not relate to virtual care |
| 7 | Humana health plan centered on virtual primary care Healthcare Leadership Review 2019;38(5):13–13 2019 | Is not a study |
| 99 | Health Care Technology Today PT in Motion 2018;10(2):32–41 2018 | Does not relate to research questions Does not relate to virtual care |
| 98 | Establishing the reliability and concurrent validity of physical performance tests using virtual reality equipment for community-dwelling healthy elders: Disability and Rehabilitation 2015; 37(12): 1097-101. | Does not relate to research questions |
| 36 | AAFP, Zipnosis team for virtual care Healthcare Leadership Review 2018;37(5):18–18. | Is not a study Does not relate to research questions |
| 82 | A Chance to Wait Is a Chance to Educate: Exploring Virtual Technology for the Delivery of Patient Health and Wellness Information at Mayo Clinic in Arizona: Journal of Hospital Librarianship 2012; 12(4): 317-326. | Does not relate to research questions |
Appendix B
| Author | Wilson Pecci, A. | Glennon, C. |
|---|---|---|
| Date | 2017 | 2018 |
| Title | Innovative digital health tools offer “seamless” patient experience | Use of Virtual Reality to Distract From Pain and Anxiety |
| Publication | Healthcare Leadership Review | Oncology Nursing Forum |
| Method | Measure app usage | Quasi-experimental study. T tests and Chi square tests |
| Setting | Nemuors Children’s Health System | Outpatient cancer center |
| Subjects | Clinicians creating asthma plans | 97 adults |
| Results | Clinicians thought they were going to be overwhelmed, but the volume was very reasonable, and it was a good way to answer questions | Experimental and control groups showed a decrease in pain and anxiety from pre to post procedure |
| Limitations | Older patients might not be suitable for this app | Similarities between experimental and control groups. Small sample size |
| Themes (edu, using, intro, consumer/doc pers)? | Clinician perspectives | Using virtual care |
| Notes | App for healthcare plan | VR can be considered a type of virtual care intervention |
| Author | Abbott, D. | Birnie, K. |
| Date | 2018 | 2018 |
| Title | Financial and Temporal Advantages of Virtual Consultation in Veterans Requiring Specialty care | Usability Testing of an Interactive Virtual Reality Distraction Intervention to Reduce Procedural Pain in Children and Adolescents with Cancer |
| Publication | Military Medicine | Journal of Pediatric Oncology Nursing |
| Method | Virtual consultation compared with in-person consultations over 6 months | Three iterative cycles of mixed method usability testing with semi-structured interviews |
| Setting | Veteran Affairs, Thoracic surgery outpatient clinic | Pediatric care center |
| Subjects | 157 veterans | 17 children and adolescents |
| Results | Overall cost was decreased to 64% per veteran encounter with virtual consults | 94% would like to use VR in subsequent needle procedures. No adverse events were reported |
| Limitations | Virtual consult is influenced by referring provider bias. Generalizability of virtual consult cost savings is more easily shown with a fixed budget such as that of the VA, which may not be the case for other facilities. No collection of patient outcomes | Small sample from a single tertiary pediatric care center. Lacked participants undergoing IVAD access for the first time, and participants reported low levels of preprocedural stress |
| Themes (edu, using, intro, consumer/doc pers)? | Using virtual care | Using virtual care |
| Notes | Benefits and potential cost savings of virtual care | VR can be considered a type of virtual care intervention |
| Author | Schneider, S.M. | Cornejo-Palma, D. |
| Date | 2007 | 2019 |
| Title | Virtual reality: A distinction intervention for chemotherapy | Virtual postoperative clinic: Can we push virtual postoperative care further upstream? |
| Publication | Oncology Nursing Forum | BMJ Quality & Safety |
| Method | Crossover design where participants served as their own control | Randomized controlled trial comparing telephone-based virtual outpatient with an actual outpatient clinic for follow up of general surgery patients 6–8 weeks after discharge from hospital |
| Setting | Cancer treatment center | Outpatient clinic |
| Subjects | 123 chemotherapy patients | 107 subjects randomized to virtual follow up 102 subjects randomized to conventional clinic follow up |
| Results | Patients state that using VR made treatment seem shorter, and chemo treatments with VR are better. Positive experiences did not result in a decrease in symptom distress | 92% of 107 subjects successfully contacted by phone, of which 10% had postoperative issues, and three of whom attended a conventional clinic for follow up. 81% of 102 subjects attended the appointment, of which 16% had postoperative concerns. Most patients in both groups expressed a preference for virtual follow up in the future |
| Limitations | Single study site and lack of standardized measures to capture satisfaction with use of VR during chemo. Intervention was only used once with each patient | N/A |
| Themes (edu, using, intro, consumer/doc pers)? | Using virtual care Consumer perspectives | Using virtual care Consumer perspective |
| Notes | VR is a good tool for virtual care as a distractor | Consumer preference for virtual care |
| Author | Gandolfi, M. | De Jong, J. |
| Date | 2017 | 2018 |
| Title | Telerehabilitation for Postural Instability in Parkinson’s Disease: A Multicenter, Single-Blind, Randomized Controlled Trial | A Cloud-Based Virtual Outpatient Clinic for Patient-Centered Care: Proof of Concept Study |
| Publication | BioMed Research International | Journal of Medical Internet Research |
| Method | Multicenter study. 76 patients were randomly assigned to either receive VR telerehabilitation or in-clinic SIBT | Six digital tools that support self-monitoring. Assessed the feasibility, usage stats, technical issues, adherence, and conducted qualitative interviews with all participants |
| Setting | Patient homes | Outpatient clinic |
| Subjects | 76 Parkinson’s disease patients | 20 participants from Internal Medicine and Dermatology departments |
| Results | VR is a feasible alternative to in-clinic SIBT for reducing postural instability in PD patients having a caregiver | Qualitative data showed that performance and effort expectancy scored high among participants, indicating that using the VOC is convenient and time saving |
| Limitations | Lack of instrumental evaluation to assess balance performance, postural reactions, and changing muscle strength and lean body mass | Nonrandomized convenience sample, as participants with interest in technology and digitalization are more likely to participate in this study. Short study period |
| Themes (edu, using, intro, consumer/doc pers)? | Using virtual care | Using virtual care |
| Notes | VR as a type of virtual care intervention | Tools that support remote monitoring |
| Author | Diaz-Hennessey, S. | Gordon, A. |
| Date | 2019 | 2017 |
| Title | Virtual Reality: Augmenting the Acute Pain Experience in Children | Virtual Visits for Acute, Nonurgent Care: A Claims Analysis of Episode-Level Utilization |
| Publication | Pediatric Nursing | Journal of Medical Internet Research |
| Method | Randomized sample. Control group received standard ED treatment, intervention group received VR. Pain assessed using Numerical Rating Scale | Cross-sectional, retrospective analysis of claims from a large commercial health insurer was performed to compare care and cost of patients receiving care via virtual visits for a condition of interest |
| Setting | Acute care pediatric emergency department | Varied depending on the type of care |
| Subjects | 15 participants aged 8–17 | Patient less than 65 years of age without serious chronic conditions |
| Results | Pain scores reported by patients were not significantly lower when using VR than those receiving standard treatment. Average length of stay was shorter for patients in the intervention group. Self-reported pain scores did not vary significantly, but observed pain scores had a significant difference. | 59,945 visits were included (4635 virtual, 55310 nonvirtual). Lab rates for virtual visits were lower than in-person locations, and imaging rates for virtual visits were lower than in-person locations. RHC, UCC, ED, and PCP were $36, $153, $1735 and $162 more expensive than virtual visits, respectively |
| Limitations | Small sample size and researcher bias. Length of stay could have been increased for a number of other factors that do not relate to patient’s pain | Accuracy of diagnosis in claims may be a concern for virtual visits, as there is no physical examination. Claims do not provide complete information on the reasons patients chose a specific site of care. |
| Themes (edu, using, intro, consumer/doc pers)? | Using virtual care | Using virtual care |
| Notes | VR as a tool for virtual care | Cost savings of virtual care |
| Author | Healy, P. | Klein, B. |
| Date | 2019 | 2011 |
| Title | Virtual outpatient clinic as an alternative to an actual clinic visit after surgical discharge: A randomised controlled trial | Anxiety online a virtual clinic: Preliminary outcomes following completion of the five fully automated treatment programs for anxiety disorders and symptoms |
| Publication | BMJ Quality & Safety | Journal of Medical Internet Research |
| Method | All patients admitted under one general surgical service over the study period were assessed. If eligible for inclusion, randomization and follow-up methods were explained to receive either a VIRTUAL OUTPATIENT CLINIC or an OPC appointment | Naturalistic participant choice, quasi-experimental design to evaluate each of the 5 anxiety online fully automated self-help e-therapy programs |
| Setting | Outpatient clinic | Anxiety e-therapy programs online |
| Subjects | 209 patients included | 225 participants. Participants needed to have at least subclinical levels of one of the anxiety disorders to be offered the e-therapy program |
| Results | 91.6% in VIRTUAL OUTPATIENT CLINIC group successfully contacted, 81.4% in OPC group were successfully contacted. 95% of VIRTUAL OUTPATIENT CLINIC patients were very happy with their overall experience compared with 56% in the OPC group. 83% in VIRTUAL OUTPATIENT CLINIC and 67% in OPC preferred VIRTUAL OUTPATIENT CLINIC appointment in the future | Significant improvements were found on 21/25 measures across the five fully automated self-help programs. Reductions on all five anxiety disorder/clinical disorder severity ratings, increased confidence in managing one’s own mental healthcare, and decreases in the total number of clinical diagnoses |
| Limitations | Follow-up questionnaire was devised to assess the outcomes of interest in this study, as it has not been previously validated, unlike the patient satisfaction questionnaire which has been validated | Open-access, participant choice, naturalistic trial, so the lack of a control group makes it impossible to conclude whether the improvements are a result of the active e-therapy programs |
| Themes (edu, using, intro, consumer/doc pers)? | Using virtual care Consumer perspective | Using virtual care Consumer perspectives |
| Notes | Consumer preference for virtual care | e-therapy |
| Author | Roth, S. | Scapin, S. |
| Date | 2014 | 2017 |
| Title | Clinical Experience Using a 5-Week Treadmill Training Program with Virtual Reality to Enhance Gait in an Ambulatory Physical Therapy Service | Use of virtual reality for treating burned children: Case reports. |
| Publication | Physical Therapy | Revista Brasileira de Enfermagem |
| Method | Retrospective data analysis | Case report on the use of VR in pain intensity during dressing change of two burned children |
| Setting | Ambulatory clinic | Burn Treatment Center |
| Subjects | 60 patients | 2 burned children |
| Results | Treadmill training with VR appears to be an effective and practical tool that can be applied in an outpatient physical therapy clinic. May also augment cognitive and functional aspects | VR can become an important non pharmacological method for treating pain in burned children |
| Limitations | Use of retrospective analysis with no control group and lack of objective cognitive assessment | Small sample size. Only based on case reports; hence, results cannot be generalized |
| Themes (edu, using, intro, consumer/doc pers)? | Using virtual care | Using virtual care |
| Notes | VR as a tool for virtual care | VR can be considered a type of virtual care intervention |
| Author | Tejera, S. | Ventola, C.L. |
| Date | 2016 | 2019 |
| Title | A New Form of Communication Between Rheumatology and Primary Care: The Virtual Consultation | Virtual Reality in Pharmacy: Opportunities for Clinical, Research and Educational Applications |
| Publication | Reumatologia Clinica | P&T: A Peer-Reviewed Journal for Managed Care & Formulary Management |
| Method | Observational and retrospective study Virtual practices were made through a computerized program, DRAGO | Clinical studies on applications of VR for pharmacotherapy in pain management, anxiety and other disorders, drug discovery, education/training, and patient counseling |
| Setting | Three healthcare centers | Inpatient and outpatient therapeutic purposes |
| Subjects | 44 primary care physicians with a reference population of 70,693 inhabitants | Subjects from clinical studies |
| Results | Closer contact with primary care, rapid resolution of doubts about rheumatic disease in patients, improvement of training in rheumatic disorders, prioritizing patients requiring early assessment by a rheumatologist | In spite of increasing awareness regarding VR in the medical and pharmacy community, how or whether to apply this technology in clinical practice remains unclear. As technology improves, VR’s influence can be increased in clinical, research, educational, and patient counseling practices in pharmacy |
| Limitations | No patient satisfaction surveys | Technical capabilities; inability to incorporate data from wearables, EHRs, patient portals or biosensors, unrealistic avatars interfere with VR immersion, potential inefficacy of less advanced VR systems |
| Themes (edu, using, intro, consumer/doc pers)? | Using virtual care | Using virtual care |
| Notes | Virtual consultation for rheumatology can reduce unnecessary visits | Trends for VR in pharmacy |
| Author | Weissman, S. | White, T. |
| Date | 2018 | 2019 |
| Title | Implementing a Virtual Health Telemedicine Program in a Community Setting | Virtual Postoperative Visits for New Ostomates |
| Publication | Journal of Genetic Counseling | CIN: Computers, Informatics, Nursing |
| Method | Recruited genetic counselors for virtual health clinical workflows | Survey data analyses, content analysis described video interactions |
| Setting | Nine prenatal and cancer clinics | Patient homes |
| Subjects | Patients in the nine clinics, unclear of sample size | 10 postoperative patients |
| Results | Decreased wait times, allowed patients to be seen in a clinic closer to their homes, ability for one GC to staff geographically disparate clinics on the same day | All patients successfully complete two virtual visits from their homes. 90% felt these helped with ostomy management and all felt comfortable with a virtual format. |
| Limitations | Not formally studied, have not addressed the issue of billing | Sample size was small and recruited from a single facility, limiting the generalizability of findings. Limited scope did not allow exploring into issues with technology |
| Themes (edu, using, intro, consumer/doc pers)? | Using virtual care | Using virtual care Consumer perspectives |
| Notes | Virtual care solving recruitment issues | Video conferencing for follow-up visits |
| Author | Tong, X. | Yen, C. |
| Date | 2016 | 2011 |
| Title | Usability Comparisons of Head-Mounted vs. Stereoscopic Desktop Displays in a Virtual Reality Environment with Pain Patients | Effects of Virtual Reality-Augmented Balance Training on Sensory Organization and Attentional Demand for Postural Control in People with Parkinson Disease: A Randomized Controlled Trial...including Invited Commentary with Author Response |
| Publication | Studies in Health Technology & Informatics | Physical Therapy |
| Method | Repeated-measured experiment | Longitudinal, randomized controlled trial |
| Setting | Clinical setting | Intervention was conducted in the clinic, assessment was performed in a research lab |
| Subjects | 20 chronic pain patients | 42 people with PD |
| Results | Participants experienced higher levels of simulator sickness with Oculus Rift HMD. Results may help clinicians and researchers to choose the most appropriate VR displays for chronic pain patients and to enhance VR displays for long-term pain management interventions | Both VR and CB training improved sensory integration for postural control in people with PD. Attentional demand for postural control was not changed after either VR or CB training. |
| Limitations | Did not measure the use of either display over longer periods of time, or with repeated frequency | Functional significance of the improvement in equilibrium scores in the SOTs was not known, and the sample size was small |
| Themes (edu, using, intro, consumer/doc pers)? | Using virtual care | Using virtual care |
| Notes | VR tools and selecting the best VR tool on the market for pain management | VR as a tool for augmented training for PD patients |
| Author | Papadopoulos, L. | Dyer, E. |
| Date | 2013 | 2018 |
| Title | Design and evaluation of a simulation for pediatric dentistry in virtual worlds | Using virtual reality in medical education to teach empathy |
| Publication | Journal of Medical Internet Research | Journal of Medical Library Association |
| Method | Child virtual patient used. Evaluation of simulation completed | VR immersion training |
| Setting | Pediatric dentistry | University of New England library |
| Subjects | 103 dental students | Health professions students |
| Results | 69% of the simulation group expressed their preference for using this module as an additional teaching tool | Successfully introduced an innovative new teaching modality to the medical physician assistant, physical therapy and nursing curricula. VR enhanced students’ understanding of age-related health problems and increased their empathy for older adults with vision and hearing loss or Alzheimer’s disease. |
| Limitations | Did not include measures of changes in students’ skills on behavior management. | Staff time and pace issues. |
| Themes (edu, using, intro, consumer/doc pers)? | Using virtual care for education | Virtual tools for education |
| Notes | Virtual education for dental students | VR for educating empathy in medical students |
| Author | Salminen, H. | Tong, V.T |
| Date | 2014 | 2012 |
| Title | Virtual patients in primary care: Developing a reusable model that fosters reflective practice and clinical reasoning | Smoking Cessation for Pregnancy and Beyond: A Virtual Clinic |
| Publication | Journal of Medical Internet Research | Journal of Women’s Health |
| Method | Content analysis of student’s opinions on a virtual patient | Interactive patient simulations |
| Setting | Medical curriculum at Karolinska Institute, Sweden | Dartmouth College interactive Media Laboratory, ACOG and Centers for Disease Control and Prevention |
| Subjects | 10 primary care physicians and 14 medical students | Healthcare professionals |
| Results | Good acceptance by students, supporting self-directed learning and reflective thinking | Web-based training programs can help providers enhance their skills in helping pregnant women quit smoking and remain smoke-free post-partum |
| Limitations | n/a | n/a |
| Themes (edu, using, intro, consumer/doc pers)? | Using virtual care for education | Education at a distance |
| Notes | Virtual patients for educating medical students | Patient simulations for education |
| Author | Shumaher Frutuoso, I. | Naverlo, S. |
| Date | 2019 | 2016 |
| Title | Creation of a Virtual Learning Environment in Intensive Care | Patient Perceptions of a Virtual Health Room Installation in Rural Sweden |
| Publication | Journal of Nursing UFPE | Rural & Remote Health |
| Method | Mixed, descriptive, cross-sectional study | Evaluation of patient perceptions through survey (patient activation measure) |
| Setting | Intensive Care Unit | Center for Rural Medicine |
| Subjects | 70 professionals from the nursing team | 19 users of the virtual health room |
| Results | Virtual learning environment is important for continuing education | Older patients were less likely to value the contribution of VHR. No relationships between level of education and distance traveled and perceptions of VHR |
| Limitations | Lack of published materials related to virtual learning environments in hospitals, which may intimidate creation initiatives in the nursing area | Limited regarding depth of information relative to sample size |
| Themes (edu, using, intro, consumer/doc pers)? | Using virtual care for education | Consumer perspectives |
| Notes | Nursing education | Virtual Health Room |
| Author | Mammen, J. | Pflugeisen, B. |
| Date | 2017 | 2017 |
| Title | Patient and Physician Perceptions of Virtual Visits for Parkinson’s Disease: A Qualitative Study | Patient Satisfaction with Virtual Obstetric Care |
| Publication | Telemed J E Health | Maternal & Child Health Journal |
| Method | Qualitative survey | Four-domain satisfaction questionnaire, Dillman method. Chi-square tests, t-tests, logistic regression, ANOVA models |
| Setting | Home | Antenatal visits |
| Subjects | Parkinson’s disease patients and treating physicians | 378 participants using virtual care, 795 using traditional care for obstetric services |
| Results | Patients and providers mostly favor telemedicine, which higher satisfaction in patients compared to providers | Overall satisfaction was significantly higher in the virtual care cohort. Virtual care model was selected by significantly more women who already have children than those experiencing pregnancy for the first time |
| Limitations | Experiences of subjects varied depending on their comfort level or issues encountered with technology | Implicit bias present in retrospective, voluntary response survey studies and low response rates. |
| Themes (edu, using, intro, consumer/doc pers)? | Consumer perspectives | Consumer perspectives |
| Notes | Virtual care for obstetric services |
References
- HIPAA Journal. What is PII, PHI, and IIHA? 2017. Available online: https://www.hipaajournal.com/what-is-considered-phi/ (accessed on 15 June 2018).
- Rouse, M. Health Insurance Portability and Accountability Act. 2017. Available online: https://searchhealthit.techtarget.com/definition/HIPAA (accessed on 15 June 2018).
- Office of the Information and Privacy Commissioner. PIPEDA in Brief. 2019. Available online: https://www.priv.gc.ca/en/privacy-topics/privacy-laws-in-canada/the-personal-information-protection-and-electronic-documents-act-pipeda/pipeda_brief/ (accessed on 15 June 2018).
- Kassam, I.; Nagle, L.; Strudwick, G. Informatics Competencies for Leaders: Protocol for a Scoping Review. 2017. Available online: https://www-ncbi-nlm-nih-gov.ezproxy.library.uvic.ca/pubmed/29247108 (accessed on 10 August 2018).
- De Jong, J.M.; Ogink, P.A.; van Bunningen, C.G.; Driessen, R.J.; Engelen, L.J.; Heeren, B.; Bredie, S.J.; van de Belt, T.H. A Cloud-Based Virtual Outpatient Clinic for Patient-Centered Care: Proof-of-Concept Study. J. Med. Internet Res. 2018, 20, 64. [Google Scholar] [CrossRef]
- Gordon, A.S.; Adamson, W.C.; DeVries, A.R. Virtual Visits for Acute, Nonurgent Care: A Claims Analysis of Episode-Level Utilization. J. Med. Internet Res. 2017, 19, e35. [Google Scholar] [CrossRef]
- Glennon, C.; McElroy, S.F.; Connelly, L.M.; Lawson, L.M.; Bretches, A.M.; Gard, A.R.; Newcomer, L.R. Use of Virtual Reality to Distract From Pain and Anxiety. Oncol. Nurs. Forum 2018, 45, 545–552. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Birnie, K.A.; Kulandaivelu, Y.; Jibb, L.; Hroch, P.; Positano, K.; Robertson, S.; Campbell, F.; Abla, O.; Stinson, J. Usability Testing of an Interactive Virtual Reality Distraction Intervention to Reduce Procedural Pain in Children and Adolescents with Cancer. J. Pediatr. Oncol. Nurs. 2018, 35, 406–416. [Google Scholar] [CrossRef]
- Scapin, S.Q.; Echevarría-Guanilo, M.E.; Boeira Fuculo Junior, P.R.; Martins, J.C.; da Ventura Barbosa, M.; Pereima, M.J.L. Use of virtual reality for treating burned children: Case reports. Rev. Bras. Enferm. 2017, 70, 1291–1295. [Google Scholar] [CrossRef] [Green Version]
- Schneider, S.M.; Hood, L.E. Virtual reality: A distraction intervention for chemotherapy. Oncol. Nurs. Forum 2007, 34, 39–46. [Google Scholar] [CrossRef] [Green Version]
- Abbott, D.E.; Macke, R.A.; Kurtz, J.; Safdar, N.; Greenberg, C.C.; Weber, S.M.; Voils, C.I.; Fisher, D.A.; Maloney, J.D. Financial and Temporal Advantages of Virtual Consultation in Veterans Requiring Specialty Care. Mil. Med. 2018, 183, e71–e76. [Google Scholar] [CrossRef] [Green Version]
- Cornejo-Palma, D.; Urbach, D.R. Virtual postoperative clinic: Can we push virtual postoperative care further upstream? BMJ Qual. Saf. 2019, 28, 7–9. [Google Scholar] [CrossRef] [Green Version]
- Gandolfi, M.; Geroin, C.; Dimitrova, E.; Boldrini, P.; Waldner, A.; Bonadiman, S.; Picelli, A.; Regazzo, S.; Stirbu, E.; Primon, D.; et al. Virtual Reality Telerehabilitation for Postural Instability in Parkinson’s Disease: A Multicenter, Single-Blind, Randomized, Controlled Trial. BioMed Res. Int. 2017, 2017, 7962826. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yen, C.-Y.; Lin, K.-H.; Hu, M.-H.; Wu, R.-M.; Lu, T.-W.; Lin, C.-H.; Deutsch, J.E.; Mirelman, A.; Hausdorff, J.M. Effects of Virtual Reality-Augmented Balance Training on Sensory Organization and Attentional Demand for Postural Control in People With Parkinson Disease: A Randomized Controlled Trial... including Invited Commentary with Author Response. Phys. Ther. 2011, 91, 862–878. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roth Shema, S.; Brozgol, M.; Dorfman, M.; Maidan, I.; Sharaby-Yeshayahu, L.; Malik-Kozuch, H.; Mirelman, A. Clinical Experience Using a 5-Week Treadmill Training Program With Virtual Reality to Enhance Gait in an Ambulatory Physical Therapy Service. Phys. Ther. 2014, 94, 1319–1326. [Google Scholar] [CrossRef] [Green Version]
- Healy, P.; McCrone, L.; Tully, R.; Flannery, E.; Flynn, A.; Cahir, C.; Arumugasamy, M.; Walsh, T. Virtual outpatient clinic as an alternative to an actual clinic visit after surgical discharge: A randomised controlled trial. BMJ Qual. Saf. 2019, 28, 24–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diaz-Hennessey, S.; O’Shea, E.R. Virtual Reality: Augmenting the Acute Pain Experience in Children. Pediatr. Nurs. 2019, 45, 122–127. [Google Scholar]
- Klein, B.; Meyer, D.; Austin, D.W.; Kyrios, M. Anxiety online-a virtual clinic: Preliminary outcomes following completion of five fully automated treatment programs for anxiety disorders and symptoms. J. Med. Internet Res. 2011, 13, e89. [Google Scholar] [CrossRef] [Green Version]
- Tong, V.T.; Dietz, P.M.; England, L.J. “Smoking Cessation for Pregnancy and Beyond: A Virtual Clinic,” an Innovative Web-Based Training for Healthcare Professionals. J. Women’s Health 2012, 21, 1014–1017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ventola, C.L. Virtual Reality in Pharmacy: Opportunities for Clinical, Research, and Educational Applications. P T Peer-Rev. J. Manag. Care Formul. Manag. 2019, 44, 267–276. [Google Scholar]
- Dyer, E.; Swartzlander, B.J.; Gugliucci, M.R. Using virtual reality in medical education to teach empathy. J. Med. Libr. Assoc. 2018, 106, 498–500. [Google Scholar] [CrossRef] [Green Version]
- Papadopoulos, L.; Pentzou, A.-E.; Louloudiadis, K.; Tsiatsos, T.-K. Design and evaluation of a simulation for pediatric dentistry in virtual worlds. J. Med. Internet Res. 2013, 15, e240. [Google Scholar] [CrossRef]
- Salminen, H.; Zary, N.; Björklund, K.; Toth-Pal, E.; Leanderson, C. Virtual patients in primary care: Developing a reusable model that fosters reflective practice and clinical reasoning. J. Med. Internet Res. 2014, 16, e2616. [Google Scholar] [CrossRef]
- Pflugeisen, B.; Mou, J. Patient Satisfaction with Virtual Obstetric Care. Matern. Child Health J. 2017, 21, 1544–1551. [Google Scholar] [CrossRef]
- Näverlo, S.; Carson, D.B.; Edin-Liljegren, A.; Ekstedt, M. Patient perceptions of a Virtual Health Room installation in rural Sweden. Rural. Remote Health 2016, 16, 1–8. [Google Scholar]
- White, T.; Watts, P.; Morris, M.; Moss, J. Virtual Postoperative Visits for New Ostomates. CIN Comput. Inform. Nurs. 2019, 37, 73–79. [Google Scholar] [CrossRef]
- Wilson Pecci, A. Innovative digital health tools offer “seamless” patient experience. Healthc. Leadersh. Rev. 2017, 36, 8–12. [Google Scholar]
- Mammen, J.; Elson, M.; Java, J.; Beck, C.; Beran, D.; Biglan, K.; Boyd, C.; Schmidt, P.; Simone, R.; Willis, A.; et al. Patient and Physician Perceptions of Virtual Visits for Parkinsons’s Disease: A Qualitative Study. Telemed. e-Health 2018, 24, 255–267. [Google Scholar] [CrossRef]
- Shumaher Frutuoso, I.; Antônio Doimo, T.M.; Marqui, R.; Contrin, L.M.; de Cássia Helu Mendonça Ribeiro, R.; Werneck, A.L. Creation of a Virtual Learning Environment in Intensive Care. J. Nurs. UFPE/Revista de Enfermagem UFPE 2019, 13, 1278–1287. [Google Scholar] [CrossRef]
- Vimarlund, V.; Borycki, E.M.; Kushniruk, A.W.; Avenberg, K. Ambient Assisted Living: Identifying New Challenges and Needs for Digital Technologies and Service Innovation. Yearb. Med. Inform. 2021, 30, 141–149. [Google Scholar] [CrossRef]
- Borycki, E.M.; Kushniruk, A.W.; Kletke, R.; Vimarlund, V.; Senathirajah, Y.; Quintana, Y. Enhancing Safety During a Pandemic Using Virtual Care Remote Monitoring Technologies and UML Modeling. Yearb. Med. Inform. 2021, 30, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Kushniruk, A.; Lau, F.; Borycki, E.; Protti, D. The School of Health Information Science at the University of Victoria: Towards an integrative model for health informatics education and research. Yearb. Med. Inform. 2006, 15, 159–165. [Google Scholar]
- Li, C.Z.; Borycki, E.M. Smart Homes for Healthcare. Stud. Health Technol. Inform. 2019, 257, 283–287. [Google Scholar] [PubMed]
- Paquette, S.; Lin, J.C. Outpatient Telemedicine Program in Vascular Surgery Reduces Patient Travel Time, Cost, and Environmental Pollutant Emissions. Ann. Vasc. Surg. 2019, 59, 167–172. [Google Scholar] [CrossRef]
| Virtual Care | Online Care | Mobile Doctor | Devices | Telehealth |
|---|---|---|---|---|
| Video Conference | Monitoring | Virtual Clinics | WebRTC | Distance |
| Telemedicine | Technology | Digital Health | Virtual Visits | Application |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, C.; Borycki, E.M.; Kushniruk, A.W. Connecting the World of Healthcare Virtually: A Scoping Review on Virtual Care Delivery. Healthcare 2021, 9, 1325. https://doi.org/10.3390/healthcare9101325
Li C, Borycki EM, Kushniruk AW. Connecting the World of Healthcare Virtually: A Scoping Review on Virtual Care Delivery. Healthcare. 2021; 9(10):1325. https://doi.org/10.3390/healthcare9101325
Chicago/Turabian StyleLi, Cindy (Zhirui), Elizabeth M. Borycki, and Andre W. Kushniruk. 2021. "Connecting the World of Healthcare Virtually: A Scoping Review on Virtual Care Delivery" Healthcare 9, no. 10: 1325. https://doi.org/10.3390/healthcare9101325
APA StyleLi, C., Borycki, E. M., & Kushniruk, A. W. (2021). Connecting the World of Healthcare Virtually: A Scoping Review on Virtual Care Delivery. Healthcare, 9(10), 1325. https://doi.org/10.3390/healthcare9101325








