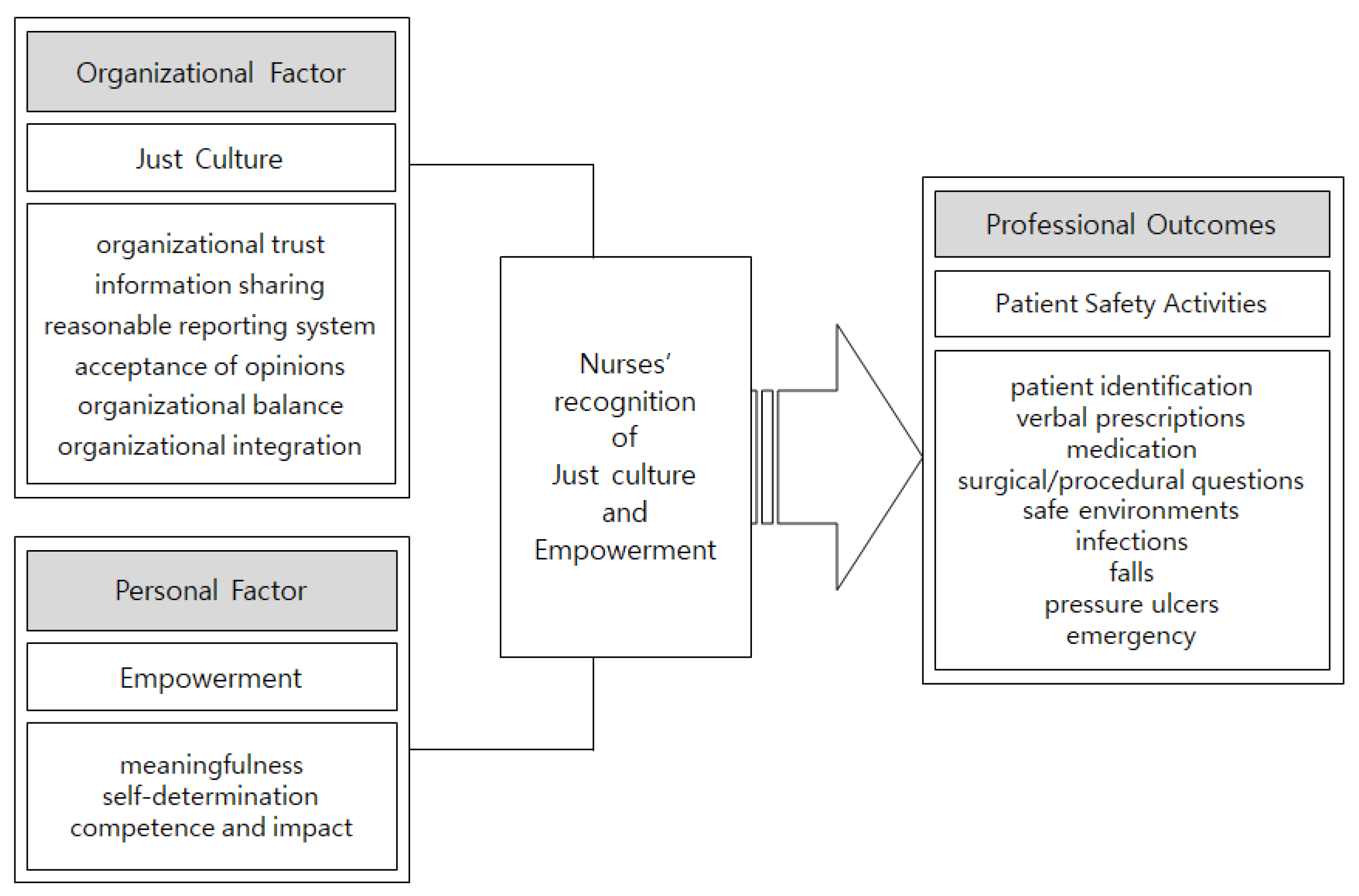
Effects of Just Culture and Empowerment on Patient Safety Activities of Hospital Nurses
Abstract
:1. Introduction
2. Methods
2.1. Study Setting
2.2. Data Collection
2.3. Measures
2.3.1. Just Culture
2.3.2. Empowerment
2.3.3. Patient Safety Activities
2.4. Data Analysis
3. Results
3.1. Participants’ General Characteristics
3.2. Just Culture, Empowerment, and Patient Safety Activities of Participants
3.3. Correlations among Nurses’ Perceived Just Culture, Empowerment, and Patient Safety Activities
3.4. Factors Influencing Patient Safety Activities
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Makary, M.A.; Daniel, M. Medical error—the third leading cause of death in the US. BMJ 2016, 353, i2139. [Google Scholar] [CrossRef]
- Yang, Y.; Liu, H. The effect of patient safety culture on nurses’ near-miss reporting intention: The moderating role of perceived severity of near misses. J. Res. Nurs. 2021, 26, 6–16. [Google Scholar] [CrossRef]
- Edmondson, A.C. The Fearless Organization: Creating Psychological Safety in the Workplace for Learning, Innovation, and Growth; John Wiley and Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Edmondson, A.C. Psychological safety and learning behavior in work teams. Adm. Sci. Q. 1999, 44, 350–383. [Google Scholar] [CrossRef] [Green Version]
- Nina, P.B.; Susan, S.S. Just culture in healthcare: An integrative review. Nurs. Forum 2021, 56, 103–111. [Google Scholar]
- Marx, D. Patient Safety and the Just Culture. Obstet. Gynecol. Clin. North Am. 2019, 46, 239–245. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Available online: https://www.who.int/patientsafety/en/ (accessed on 22 April 2021).
- Vaismoradi, M.; Tella, S.; Logan, P.A.; Khakurel, J.; Vizcaya-Moreno, F. Nurses’ Adherence to Patient Safety Principles: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 2028. [Google Scholar] [CrossRef] [Green Version]
- Amiri, M.; Khademian, Z.; Nikandish, R. The effect of nurse empowerment educational program on patient safety culture: A randomized controlled trial. BMC Med. Educ. 2018, 18, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Metwally, F.G. Relationship between Structural Empowerment, Magnet Hospital Characteristics and Patient Safety Climate among Nurses Working in Intensive Care Units. Zagazig Nurs. J. 2015, 11, 219–232. [Google Scholar] [CrossRef]
- Heo, J.I.; Moon, H. Moderating Effect of Empowerment of Perioperative Nurses in the Relationship between Their Patient Safety Culture Awareness and Safety Management Activities. Nurs. Health Issues 2019, 24, 89–95. [Google Scholar] [CrossRef]
- Richardson, A.; Storr, J. Patient safety: A literature review on the impact of nursing empowerment, leadership and collaboration. Int Nurs. Rev. 2010, 57, 12–21. [Google Scholar] [CrossRef]
- Petschonek, S. Developing the Just Culture Assessment Tool: A Method for Measuring Individual Cultural Perceptions in a Healthcare Setting. Ph.D. Thesis, The University of Memphis, Tennessee, TN, USA, December 2011. [Google Scholar]
- Lee, K.E.; Lee, J.I.; Sohn, Y.W.; Ha, Y.J. A Validation Study of the Korean Just Culture Assessment Tool: A Study of Korean Air Force Pilots. Korean J. Bus. Adm. 2013, 26, 3235–3255. [Google Scholar]
- Spreitzer, G.M. Psychological empowerment in the workplace: Dimensions, measurement, and validation. Acad. Manag. J. 1995, 38, 1442–1465. [Google Scholar] [CrossRef]
- Choo, J.Y. The Effect of Organizational Culture and Organizational Justice on Organizational Effectiveness: Focusing on the Mediating Effect of Organizational Communication and Empowerment. Ph.D. Thesis, Hanyang University, Seoul, Korea, 2017. [Google Scholar]
- Lee, G.O. The study on nurse manager leadership and patient safety-related nursing activities. Master’s Thesis, Kyung Hee University, Seoul, Korea, 2009. [Google Scholar]
- Lee, Y.J. Patient Safety Culture and Management Activities Perceived by Hospital Nurses. Master’s Thesis, Eulji University, Seoul, Korea, 2011. [Google Scholar]
- Lee, G.S.; Park, J.Y. Impact of Nursing Work Environment on Nurses’ Perception of Just Culture. Korean J. Health Promot. 2021, 21, 37–43. [Google Scholar]
- Do, E.S.; Kim, M.Y. Comparison of internal marketing, job satisfaction and customer orientation of nurses by size of medical care institution; small-medium hospitals and general hospitals. J. Korean Acad. Nurs. Adm. 2012, 18, 56–66. [Google Scholar] [CrossRef] [Green Version]
- Ko, Y.K.; Jeong, S.H.; Yu, S. Job autonomy, perceptions of organizational policy, and the safety performance of nurses. Int. J. Nurs. Pr. 2018, 24, e12696. [Google Scholar] [CrossRef] [PubMed]
- Malone, G.; Darcy, C. Perceptions of ‘Just Culture’–The Case of Aircraft Maintenance. J. Strat. Innov. Sustain. 2019, 14. [Google Scholar] [CrossRef]
- Walker, D.; Altmiller, G.; Barkell, N.; Hromadik, L.; Toothaker, R. Development and Validation of the Just Culture Assessment Tool for Nursing Education. Nurse Educ. 2019, 44, 261–264. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Kim, E.K.; Kim, S.Y. Effects of Empowerment and Job Satisfaction on Nursing Performance of Clinical Nurses. J. Korean Acad. Nurs. Adm. 2014, 20, 426–436. [Google Scholar] [CrossRef] [Green Version]
- Paradiso, L.; Sweeney, N. Just culture: It’s more than policy. Nurs. Manag. 2019, 50, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Westat, R.; Sorra, J.; Famolaro, T.; Dyer, M.N.; Khanna, K.; Nelson, D. Hospital Survey on Patient Safety Culture: 2018 User Database Report; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2018.
- Dekker, S.W.A.; Breakey, H. ‘Just culture’: Improving safety by achieving substantive, procedural and restorative justice. Saf. Sci. 2016, 85, 187–193. [Google Scholar] [CrossRef]
- Klein, C.A.; Klein, A.B. Alternative dispute resolution: An overview. Nurse Pr. 2007, 32, 15–16. [Google Scholar] [CrossRef] [PubMed]
| Variables | Mean ± SD | Range | |
|---|---|---|---|
| Min. | Max. | ||
| Just Culture | 2.95 ± 0.25 | 1 | 5 |
| Empowerment | 3.59 ± 0.51 | 1 | 5 |
| Patient Safety Activities | 4.22 ± 0.43 | 1 | 5 |
| Characteristics | Category | n | Just Culture | Empowerment | Patient Safety Activities | |||
|---|---|---|---|---|---|---|---|---|
| M ± SD | t or F (p) Scheffé | M ± SD | t or F (p) Scheffé | M ± SD | t or F (p) Scheffé | |||
| Gender | Male | 10 | 2.99 ± 0.28 | 0.40 (0.456) | 3.91 ± 0.70 | 1.98 (0.083) | 4.5 ± 0.08 | 3.13 (0.044) |
| Female | 179 | 2.95 ± 0.24 | 3.58 ± 0.49 | 4.20 ± 0.03 | ||||
| Age (years) | 20–29 a | 113 | 2.88 ± 0.23 | 11.547 (<0.001) c > a | 3.57 ± 0.50 | 3.398 (0.091) | 4.23 ± 0.42 | 0.897 (0.444) - |
| 30–39 b | 60 | 3.04 ± 0.23 | 3.55 ± 0.51 | 4.16 ± 0.42 | ||||
| 40–49 c | 10 | 3.20 ± 0.18 | 3.89 ± 0.42 | 4.39 ± 0.48 | ||||
| ≥40 d | 6 | 3.13 ± 0.20 | 4.10 ± 0.57 | 4.23 ± 0.57 | ||||
| Education | Diploma a | 20 | 2.89 ± 0.26 | 5.347 (0.001) | 3.69 ± 0.41 | 0.899 (0.443) | 4.07 ± 0.44 | 0.952 (0.417) |
| Bachelor b | 135 | 2.93 ± 0.24 | 3.56 ± 0.54 | 4.23 ± 0.43 | ||||
| Master c | 33 | 3.10 ± 0.23 | 3.69 ± 0.43 | 4.27 ± 0.43 | ||||
| PhD d | 1 | 3.27 | 3.75 | 4.12 | ||||
| Marital status | Single | 147 | 2.90 ± 0.23 | −6.597 (0.403) | 3.53 ± 0.47 | −3.242 (0.149) | 4.20 ± 0.42 | −0.810 (0.152) |
| Married | 42 | 3.16 ± 0.21 | 3.82 ± 0.57 | 4.26 ± 0.47 | ||||
| Position | Staff nurse a | 107 | 2.91 ± 0.22 | 12.390 (<0.001) c > a, b | 3.57 ± 0.54 | 4.818 (0.009) c > a, b | 4.23 ± 0.42 | 0.552 (0.577) - |
| Charge nurse b | 72 | 2.98 ± 0.26 | 3.56 ± 0.55 | 4.18 ± 0.43 | ||||
| Unit manager c | 10 | 3.28 ± 0.16 | 4.08 ± 0.47 | 4.33 ± 0.54 | ||||
| Department | Ward a | 79 | 2.88 ± 0.25 | 6.753 (<0.001) e > a, c | 3.58 ± 0.55 | 1.082 (0.367) | 4.19 ± 0.41 | 1.692 (0.154) |
| ICU b | 49 | 2.91 ± 0.20 | 3.54 ± 0.39 | 4.14 ± 0.46 | ||||
| ER c | 45 | 3.06 ± 0.22 | 3.68 ± 0.56 | 4.35 ± 0.39 | ||||
| OPD d | 6 | 3.21 ± 0.28 | 3.35 ± 0.37 | 4.16 ± 0.55 | ||||
| others | 10 | 3.07 ± 0.23 | 3.77 ± 0.53 | 4.27 ± 0.44 | ||||
| Clinical experience (years) | 1–≤ 3 a | 66 | 2.87 ± 0.20 | 9.911 (<0.001) d > a, b | 3.54 ± 053. | 2.210 (0.088) | 4.25 ± 0.38 | 0.621 (0.602) |
| 3–≤ 6 b | 51 | 2.90 ± 0.21 | 3.56 ± 0.51 | 4.16 ± 0.49 | ||||
| 6–10 c | 31 | 3.02 ± 0.22 | 3.53 ± 0.50 | 4.19 ± 0.39 | ||||
| ≥10 d | 41 | 3.11 ± 0.29 | 3.78 ± 0.46 | 4.25 ± 0.44 | ||||
| Current department experience | 1–≤ 3 a | 21 | 2.98 ± 0.29 | 4.413 (0.005) d > b | 3.70 ± 066. | 1.075 (0.361) | 4.19 ± 0.49 | 0.606 (0.612) |
| 3–≤ 6 b | 69 | 2.90 ± 0.22 | 3.55 ± 0.52 | 4.26 ± 0.40 | ||||
| 6–10 c | 55 | 2.93 ± 0.20 | 3.54 ± 0.45 | 4.16 ± 0.46 | ||||
| ≥10 d | 44 | 3.06 ± 0.29 | 3.68 ± 0.49 | 4.23 ± 0.40 | ||||
| Overtime days per week | 0–1 a | 83 | 2.99 ± 0.21 | 2.282 (0.081) | 3.61 ± 049 | 0.172 (0.915) | 4.26 ± 0.44 | 0.759 (0.518) |
| 2–3 b | 60 | 2.92 ± 0.28 | 3.56 ± 0.55 | 4.16 ± 0.42 | ||||
| 3–4 c | 26 | 2.88 ± 0.23 | 3.58 ± 0.45 | 4.23 ± 0.46 | ||||
| Everyday d | 20 | 3.01 ± 0.28 | 3.64 ± 0.58 | 4.17 ± 0.34 | ||||
| Variables | Just Culture (p) | Empowerment (p) | Patient Safety Activities (p) |
|---|---|---|---|
| Just Culture | 1 | ||
| Empowerment | 0.427 (< 0.000) | 1 | |
| Patient Safety Activities | 0.369 (< 0.000) | 0.380 (< 0.000) | 1 |
| Variables | B | SE | β | t | p |
|---|---|---|---|---|---|
| (Constant) | 2.345 | 0.367 | 6.384 | 0.000 | |
| Gender | −0.209 | 0.127 | −0.108 | −1.638 | 0.103 |
| Just Culture | 0.442 | 0.124 | 0.257 | 3.547 | 0.000 |
| Empowerment | 0.213 | 0.061 | 0.254 | 3.477 | 0.001 |
| F-value | 16.170 | ||||
| p | < 0.001 | ||||
| R2 | 0.208 | ||||
| Adj R2 | 0.195 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, B.B.; Yu, S. Effects of Just Culture and Empowerment on Patient Safety Activities of Hospital Nurses. Healthcare 2021, 9, 1324. https://doi.org/10.3390/healthcare9101324
Kim BB, Yu S. Effects of Just Culture and Empowerment on Patient Safety Activities of Hospital Nurses. Healthcare. 2021; 9(10):1324. https://doi.org/10.3390/healthcare9101324
Chicago/Turabian StyleKim, Bo Bae, and Soyoung Yu. 2021. "Effects of Just Culture and Empowerment on Patient Safety Activities of Hospital Nurses" Healthcare 9, no. 10: 1324. https://doi.org/10.3390/healthcare9101324
APA StyleKim, B. B., & Yu, S. (2021). Effects of Just Culture and Empowerment on Patient Safety Activities of Hospital Nurses. Healthcare, 9(10), 1324. https://doi.org/10.3390/healthcare9101324





