A Systematic Review of WTA-WTP Disparity for Dental Interventions and Implications for Cost-Effectiveness Analysis
Abstract
1. Introduction
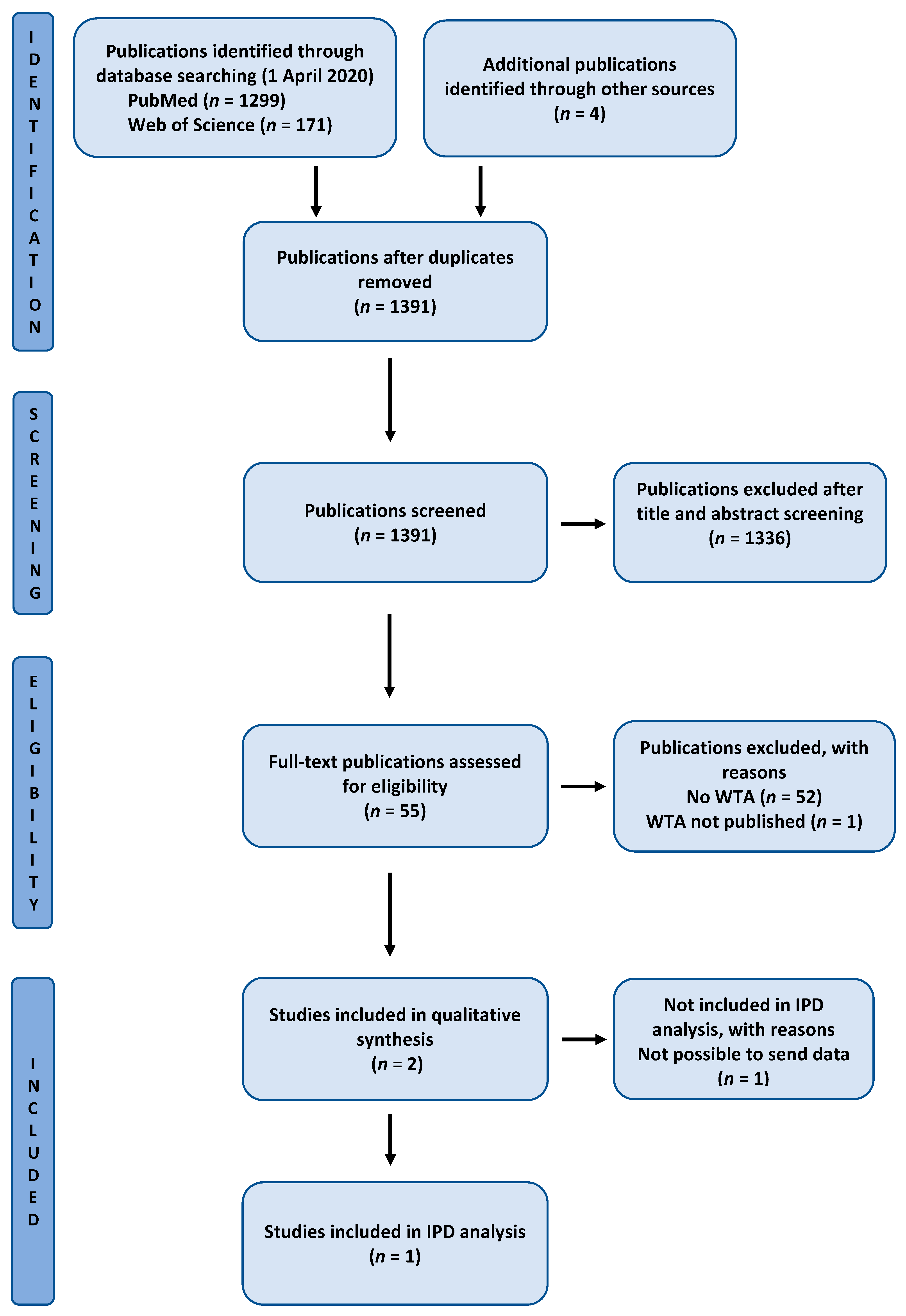
2. Methods
2.1. Systematic Review
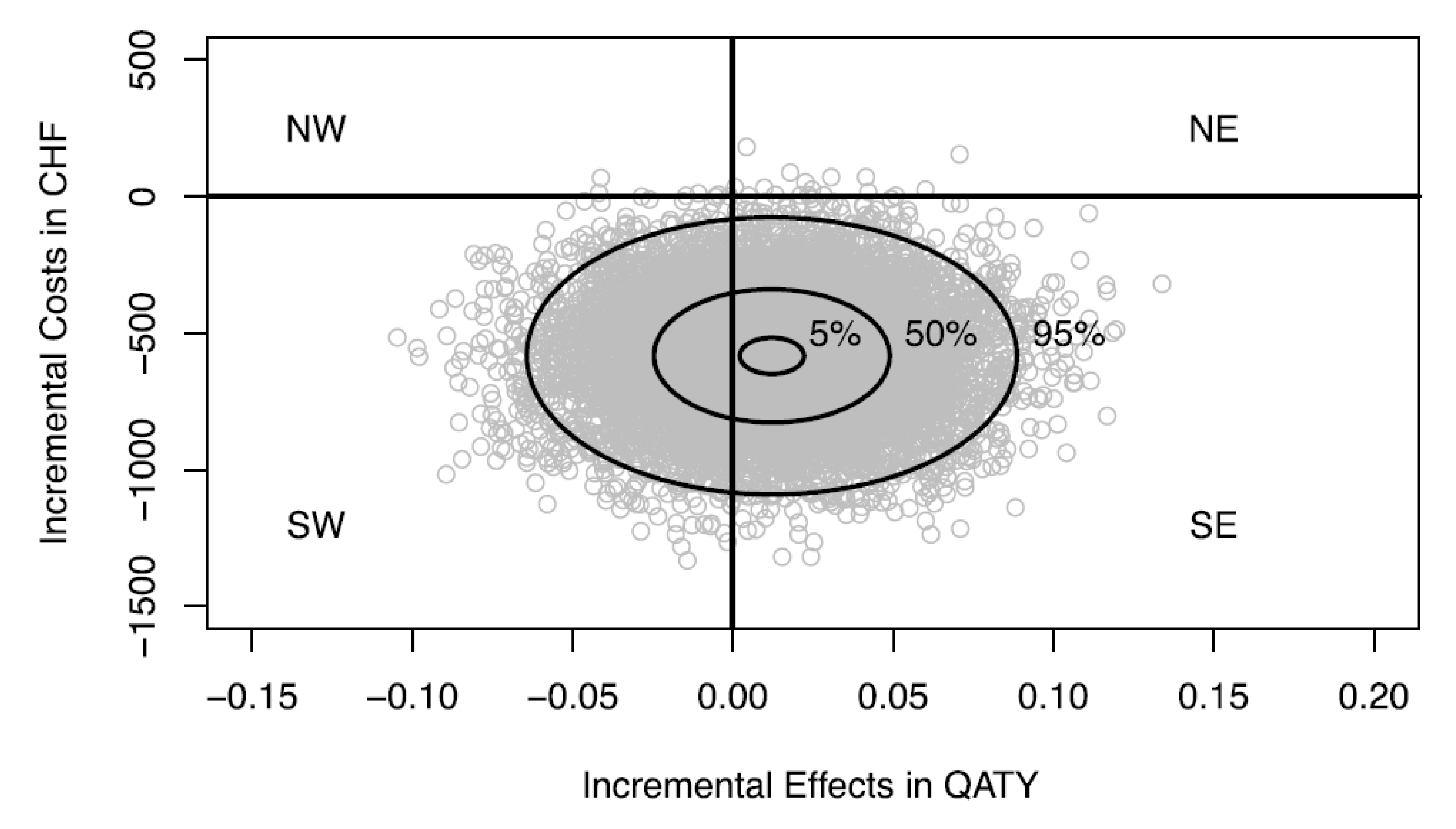
2.2. Analysis of Patient-Level Data
3. Results
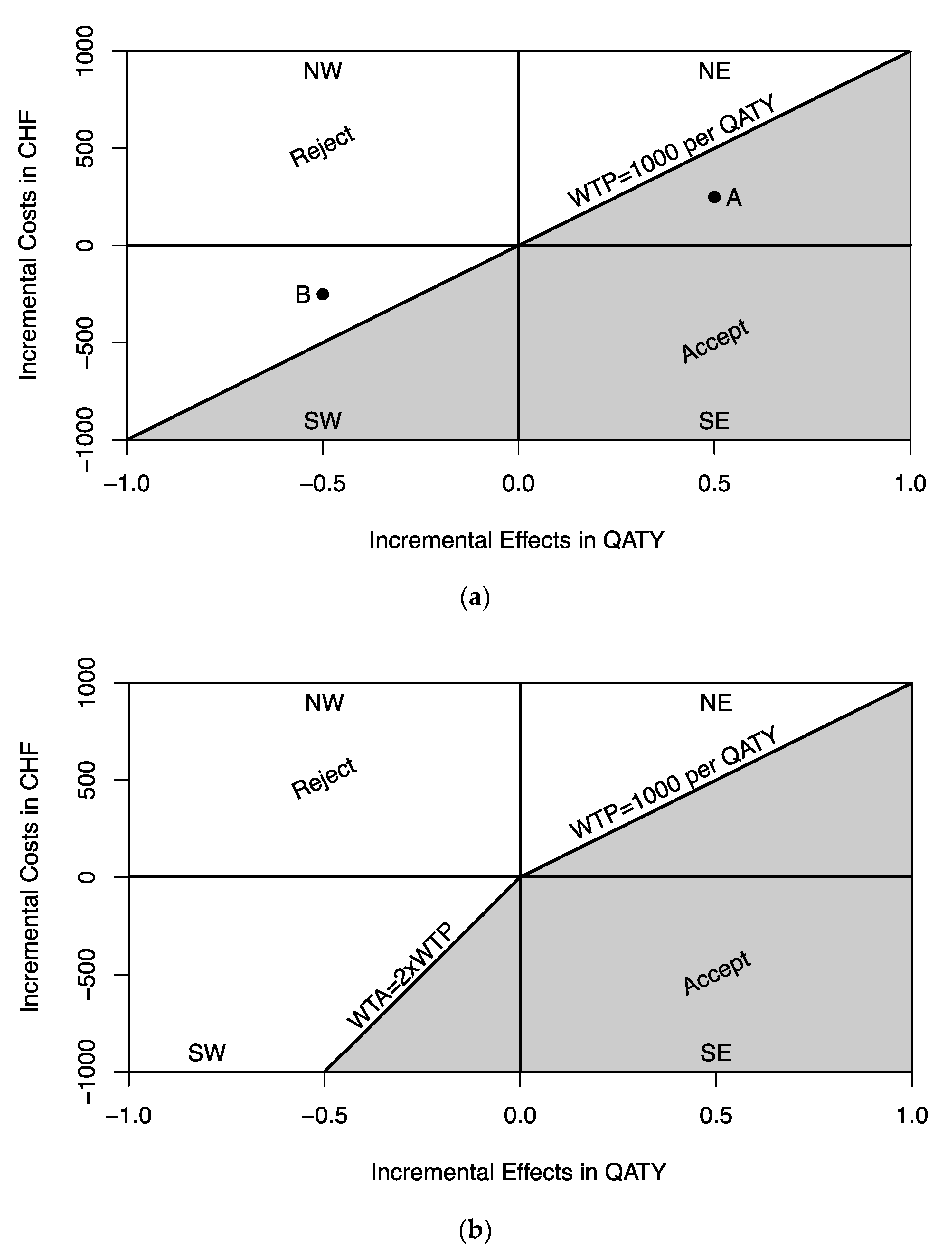
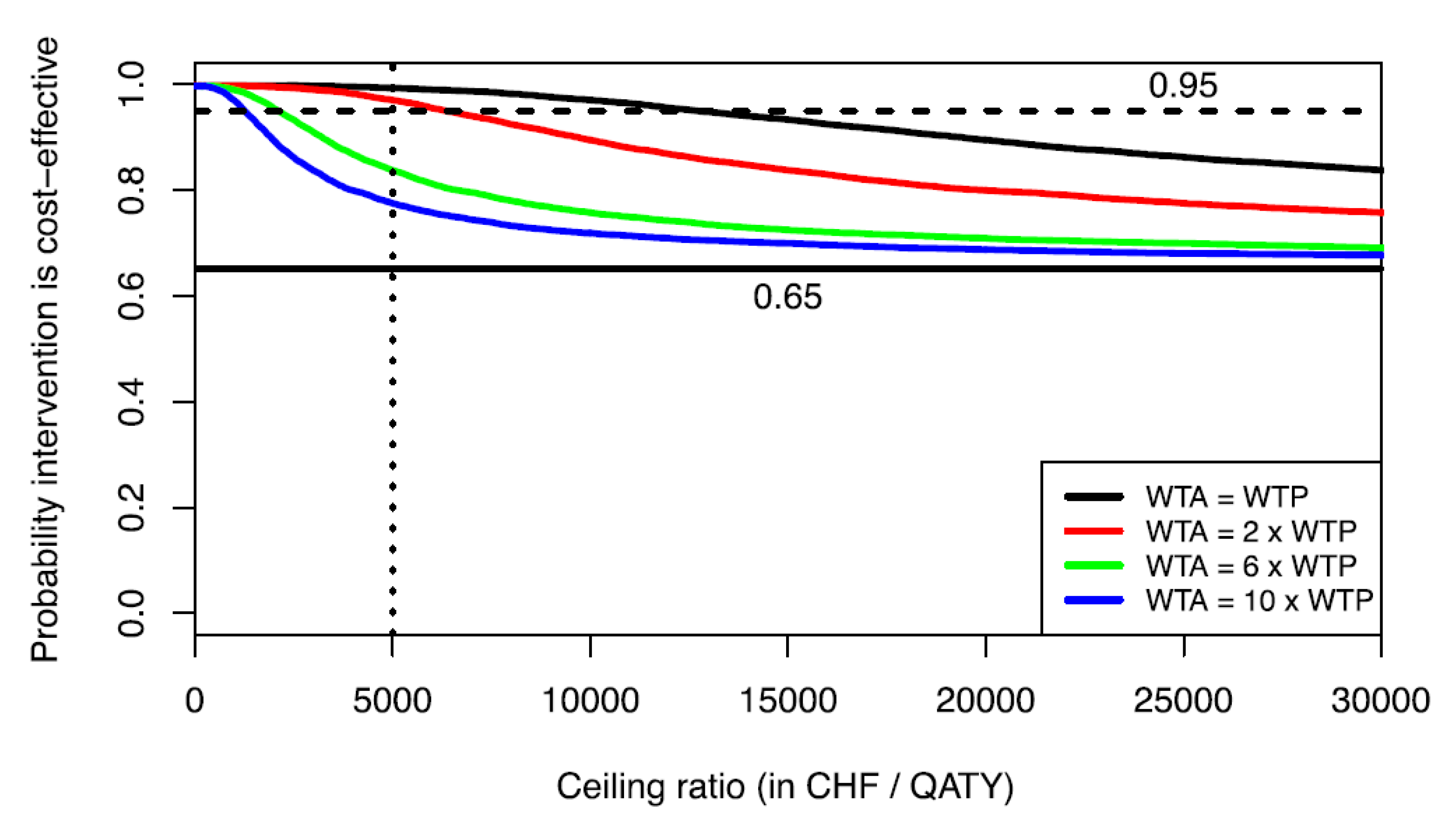
4. Implications for Cost-Effectiveness Analysis
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Weinstein, M.C.; Stason, W.B. Foundations of cost-effectiveness analysis for health and medical practices. N. Engl. J. Med. 1977, 296, 716–721. [Google Scholar] [CrossRef] [PubMed]
- Tonmukayakul, U.; Calache, H.; Clark, R.; Wasiak, J.; Faggion, C.M. Systematic review and quality appraisal of economic evaluation publications in dentistry. J. Dent. Res. 2015, 94, 1348–1354. [Google Scholar] [CrossRef] [PubMed]
- Hettiarachchi, R.M.; Kularatna, S.; Downes, M.J.; Byrnes, J.; Kroon, J.; Lalloo, R.; Johnson, N.W.; Scuffham, P.A. The cost-effectiveness of oral health interventions: A systematic review of cost-utility analyses. Community Dent. Oral Epidemiol. 2018, 46, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, M.; Zeckhauser, R. Critical ratios and efficient allocation. J. Public Econ. 1973, 2, 147–157. [Google Scholar] [CrossRef]
- Johannesson, M. The relationship between cost-effectiveness analysis and cost-benefit analysis. Soc. Sci. Med. 1995, 41, 483–489. [Google Scholar] [CrossRef]
- Bobinac, A.; van Exel, N.J.A.; Rutten, F.F.H.; Brouwer, W.B.F. Willingness to pay for a quality-adjusted life-year: The individual perspective. Value Health 2010, 13, 1046–1055. [Google Scholar] [CrossRef]
- O’Brien, B.J.; Gertsen, K.; Willan, A.R.; Faulkner, L.A. Is there a kink in consumers’ threshold value for cost-effectiveness in health care? Health Econ. 2002, 11, 175–180. [Google Scholar] [CrossRef]
- Van Hout, B.A.; Al, M.J.; Gordon, G.S.; Rutten, F.F. Costs, effects and C/E-ratios alongside a clinical trial. Health Econ. 1994, 3, 309–319. [Google Scholar] [CrossRef]
- Stinnett, A.A.; Mullahy, J. Net health benefits: A new framework for the analysis of uncertainty in cost-effectiveness analysis. Med. Decis. Making 1998, 18, S68–S80. [Google Scholar] [CrossRef]
- Fenwick, E.; Claxton, K.; Sculpher, M. Representing uncertainty: The role of cost-effectiveness acceptability curves. Health Econ. 2001, 10, 779–787. [Google Scholar] [CrossRef]
- Sendi, P.P.; Briggs, A.H. Affordability and cost-effectiveness: Decision-making on the cost-effectiveness plane. Health Econ. 2001, 10, 675–680. [Google Scholar] [CrossRef] [PubMed]
- Sendi, P.; Gafni, A.; Birch, S. Opportunity costs and uncertainty in the economic evaluation of health care interventions. Health Econ. 2002, 11, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Sendi, P.; Al, M.J.; Zimmermann, H. A risk-adjusted approach to comparing the return on investment in health care programs. Int. J. Health Care Finance Econ. 2004, 4, 199–210. [Google Scholar] [CrossRef]
- Tambour, M.; Zethraeus, N.; Johannesson, M. A note on confidence intervals in cost-effectiveness analysis. Int. J. Technol. Assess. Health Care 1998, 14, 467–471. [Google Scholar] [CrossRef] [PubMed]
- Al, M.J. Cost-effectiveness acceptability curves revisited. Pharmacoeconomics 2013, 31, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Severens, J.L.; Brunenberg, D.E.M.; Fenwick, E.A.L.; O’Brien, B.; Joore, M.A. Cost-effectiveness acceptability curves and a reluctance to lose. Pharmacoeconomics 2005, 23, 1207–1214. [Google Scholar] [CrossRef]
- Tunçel, T.; Hammitt, J.K. A new meta-analysis on the WTP/WTA disparity. J. Environ. Econ. Manag. 2014, 68, 175–187. [Google Scholar] [CrossRef]
- Horowitz, J.K.; McConnell, K.E. A review of WTA/WTP studies. J. Environ. Econ. Manag. 2002, 44, 426–447. [Google Scholar] [CrossRef]
- Rotteveel, A.H.; Lambooij, M.S.; Zuithoff, N.P.A.; van Exel, J.; Moons, K.G.M.; de Wit, G.A. Valuing healthcare goods and services: A systematic review and meta-analysis on the WTA-WTP disparity. Pharmacoeconomics 2020, 38, 443–458. [Google Scholar] [CrossRef]
- Tan, S.H.X.; Vernazza, C.R.; Nair, R. Critical review of willingness to pay for clinical oral health interventions. J. Dent. 2017, 64, 1–12. [Google Scholar] [CrossRef]
- Whynes, D.K.; Sach, T.H. WTP and WTA: Do people think differently? Soc. Sci. Med. 2007, 65, 946–957. [Google Scholar] [CrossRef] [PubMed]
- Azur, M.J.; Stuart, E.A.; Frangakis, C.; Leaf, P.J. Multiple imputation by chained equations: What is it and how does it work? Int. J. Methods Psychiatr. Res. 2011, 20, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Barnard, J.; Rubin, D.B. Small-sample degrees of freedom with multiple imputation. Biometrika 1999, 86, 948–955. [Google Scholar] [CrossRef]
- Sendi, P.; Bertschinger, N.; Brand, C.; Marinello, C.P.; Bucher, H.C.; Bornstein, M.M. Measuring the monetary value of dental implants for denture retention: A willingness to pay approach. Open Dent. J. 2017, 11, 498–502. [Google Scholar] [CrossRef]
- Dixon, S.; Shackley, P. Estimating the benefits of community water fluoridation using the willingness-to-pay technique: Results of a pilot study. Community Dent. Oral Epidemiol. 1999, 27, 124–129. [Google Scholar] [CrossRef]
- Black, W.C. The CE plane: A graphic representation of cost-effectiveness. Med. Decis. Making 1990, 10, 212–214. [Google Scholar] [CrossRef]
- Sendi, P.; Gafni, A.; Birch, S. Ethical economics and cost-effectiveness analysis: Is it ethical to ignore opportunity costs? Expert Rev. Pharmacoecon. Outcomes Res. 2005, 5, 661–665. [Google Scholar] [CrossRef]
- Zitzmann, N.U.; Krastl, G.; Weiger, R.; Kühl, S.; Sendi, P. Cost-effectiveness of anterior implants versus fixed dental prostheses. J. Dent. Res. 2013, 92, S183–S188. [Google Scholar] [CrossRef]
- Briggs, A.H. A Bayesian approach to stochastic cost-effectiveness analysis. Health Econ. 1999, 8, 257–261. [Google Scholar] [CrossRef]
- Löthgren, M.; Zethraeus, N. Definition, interpretation and calculation of cost-effectiveness acceptability curves. Health Econ. 2000, 9, 623–630. [Google Scholar] [CrossRef]
- Chilton, S.; Jones-Lee, M.; McDonald, R.; Metcalf, H. Does the WTA/WTP ratio diminish as the severity of a health complaint is reduced? Testing for smoothness of the underlying utility of wealth function. J. Risk Uncertain. 2012, 45, 1–24. [Google Scholar] [CrossRef]
- Randall, A.; Stoll, J. Consumer’s Surplus in Commodity Space. Am. Econ. Rev. 1980, 70, 449–455. [Google Scholar]
- Hanemann, W. Willingness to pay and willingness to accept: How much can they differ? Am. Econ. Rev. 1991, 81, 635–647. [Google Scholar] [CrossRef]
- Brown, T.C. Loss aversion without the endowment effect, and other explanations for the WTA-WTP disparity. J. Econ. Behav. Organ. 2005, 57, 367–379. [Google Scholar] [CrossRef]
- Grutters, J.P.C.; Kessels, A.G.H.; Dirksen, C.D.; van Helvoort-Postulart, D.; Anteunis, L.J.C.; Joore, M.A. Willingness to accept versus willingness to pay in a discrete choice experiment. Value Health 2008, 11, 1110–1119. [Google Scholar] [CrossRef]
- Diener, A.; O’Brien, B.; Gafni, A. Health care contingent valuation studies: A review and classification of the literature. Health Econ. 1998, 7, 313–326. [Google Scholar] [CrossRef]
| Publication | Sendi et al., 2017 [24] | Dixon and Shackley, 1999 [25] |
|---|---|---|
| Intervention | Mandibular implant overdentures | Discontinuing water fluoridation |
| Country | Switzerland | United Kingdom |
| Study design | Contingent valuation | Contingent valuation |
| Elicitation method | Iterative bidding (WTP) Open-ended (WTA) | Payment cards |
| Comparison group | Within subject design | Within subject design |
| Mean WTP | 4606 CHF (95% CI: 3547–6560) 1 (n = 15) | 29.38 GBP (n = 8) |
| Mean WTA | 33,500 CHF (95% CI: 9000–72,000) 1 (n = 5) | 76.00 GBP (n = 5) |
| Mean WTA/WTP ratio | 5.31 (95% CI: 2.34–8.20) 1 (n = 5) | N.A. |
| WTA/WTP ratio (ratio of means) | 7.27 | 2.58 |
| Mean WTA/WTP ratio (mean ratio using MICE) 2 | 5.12 (95% CI: 2.61–7.62) | N.A. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sendi, P.; Ramadani, A.; Zitzmann, N.U.; Bornstein, M.M. A Systematic Review of WTA-WTP Disparity for Dental Interventions and Implications for Cost-Effectiveness Analysis. Healthcare 2020, 8, 301. https://doi.org/10.3390/healthcare8030301
Sendi P, Ramadani A, Zitzmann NU, Bornstein MM. A Systematic Review of WTA-WTP Disparity for Dental Interventions and Implications for Cost-Effectiveness Analysis. Healthcare. 2020; 8(3):301. https://doi.org/10.3390/healthcare8030301
Chicago/Turabian StyleSendi, Pedram, Arta Ramadani, Nicola U. Zitzmann, and Michael M. Bornstein. 2020. "A Systematic Review of WTA-WTP Disparity for Dental Interventions and Implications for Cost-Effectiveness Analysis" Healthcare 8, no. 3: 301. https://doi.org/10.3390/healthcare8030301
APA StyleSendi, P., Ramadani, A., Zitzmann, N. U., & Bornstein, M. M. (2020). A Systematic Review of WTA-WTP Disparity for Dental Interventions and Implications for Cost-Effectiveness Analysis. Healthcare, 8(3), 301. https://doi.org/10.3390/healthcare8030301






