Effect of an Integrated Healthcare Program for Korean Rural Older Adults: A Quasi-Experimental Study
Abstract
1. Introduction
Purpose of the Study
2. Literature Review
2.1. Characteristics of Rural Older Adults
2.2. Health Care Programs for Older Adults
3. Materials and Methods
3.1. Study Design
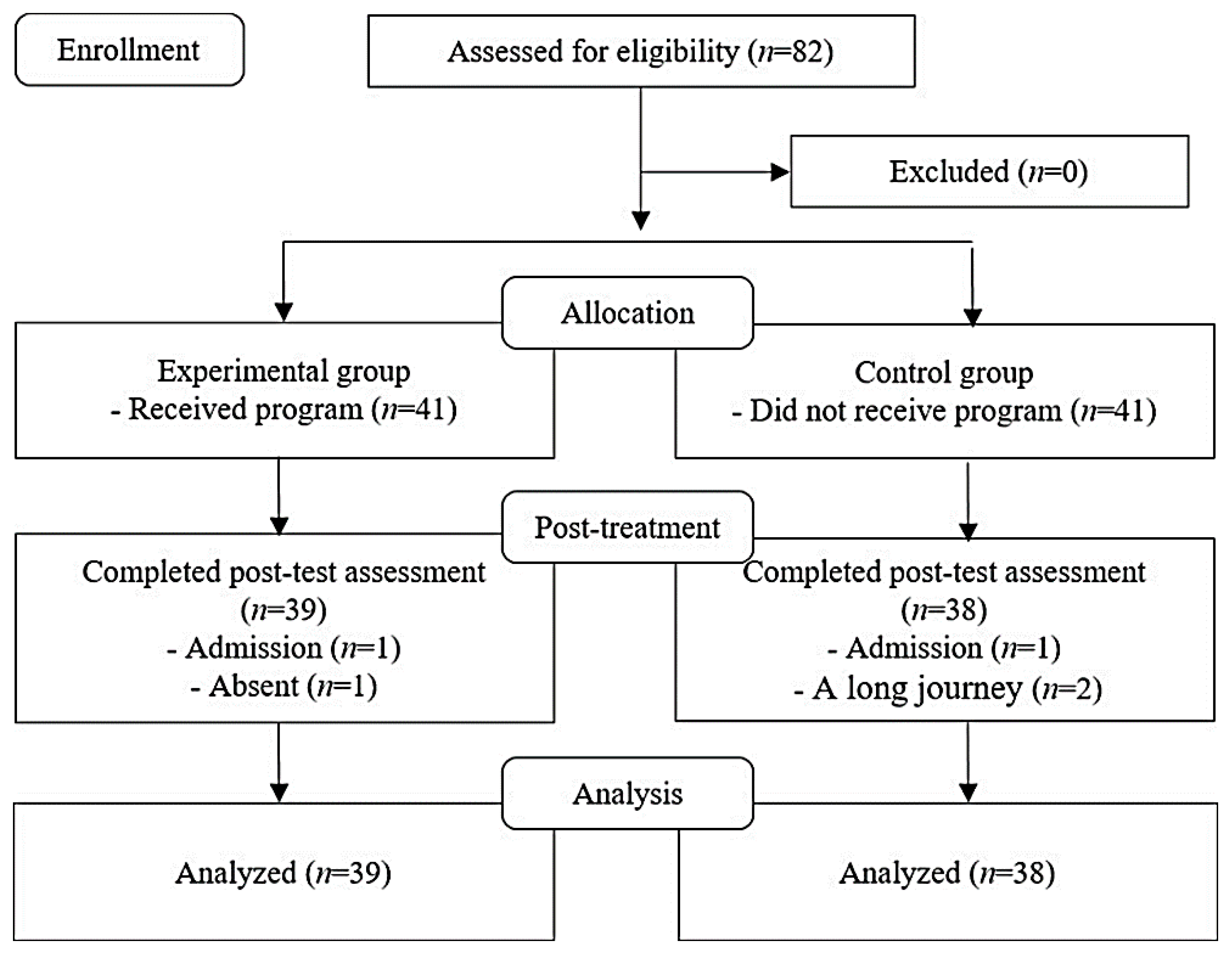
3.2. Participants and Setting
3.3. Procedure
3.3.1. Development of an Integrated Healthcare Program for the Rural Older Adults
3.3.2. Intervention
Pretest
Intervention
Posttest
3.4. Data Collection and Outcome Measures
3.5. Data Analysis
4. Results and Discussion
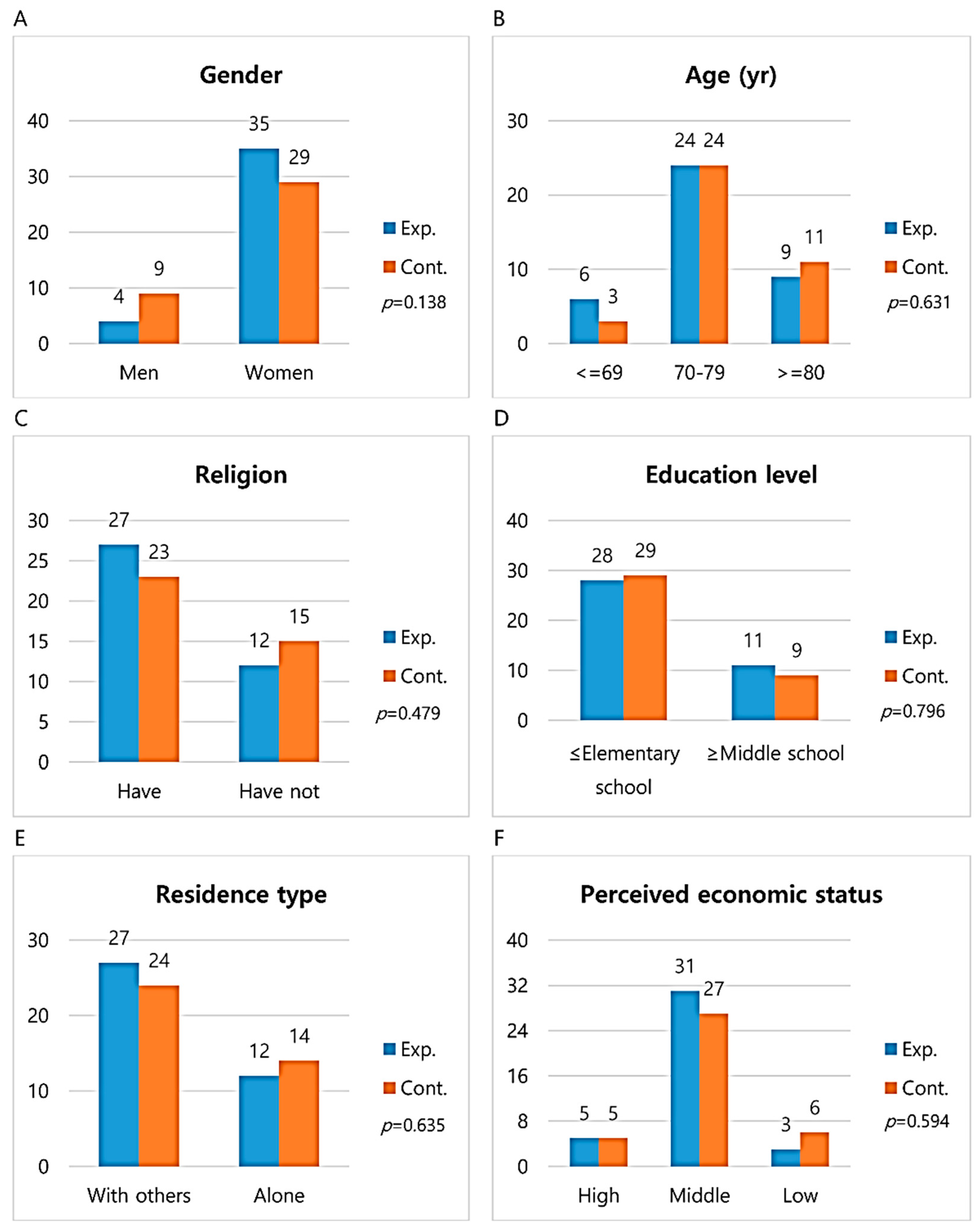
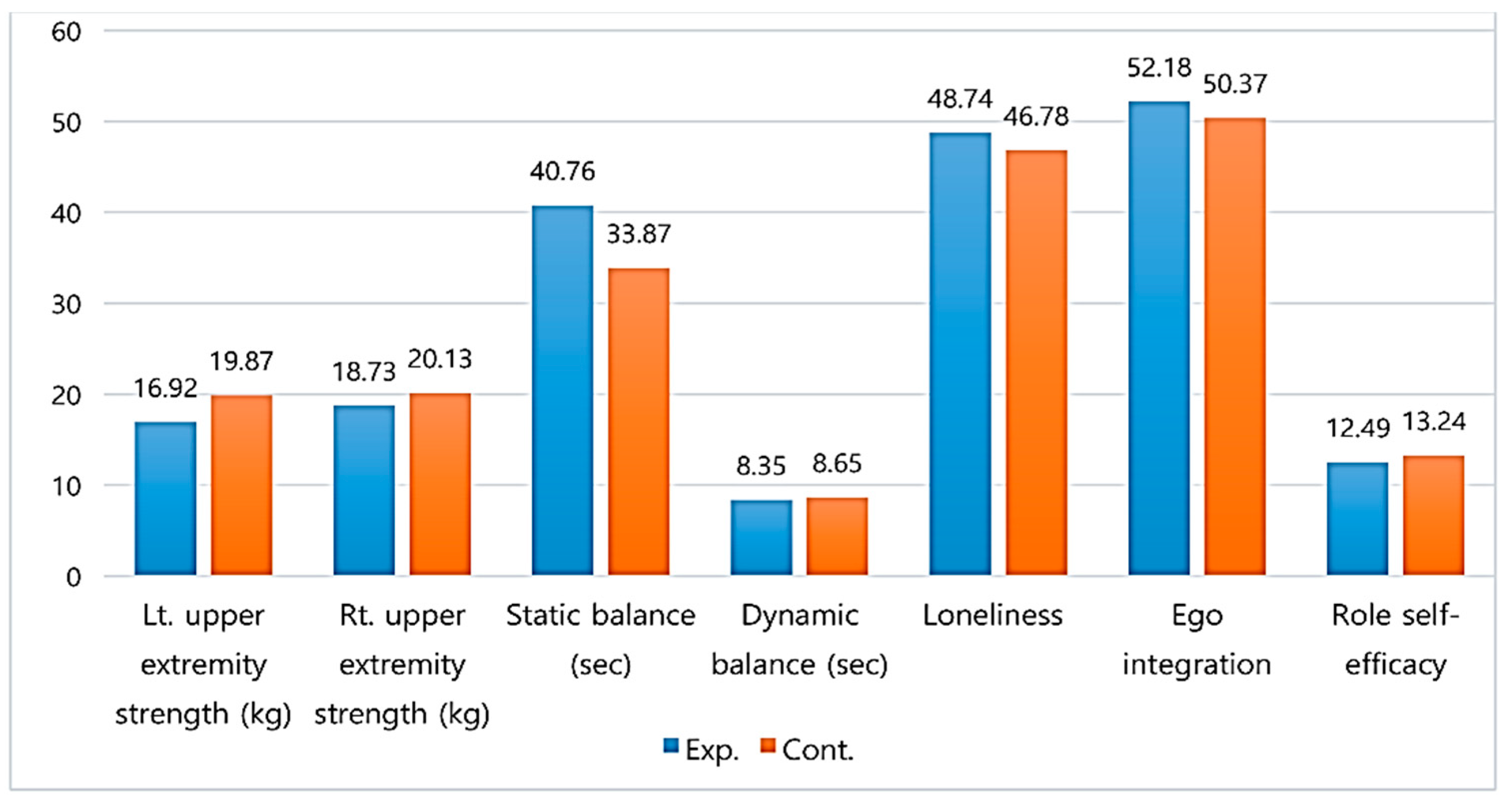
4.1. Homogeneity of Dependent Variables between Groups
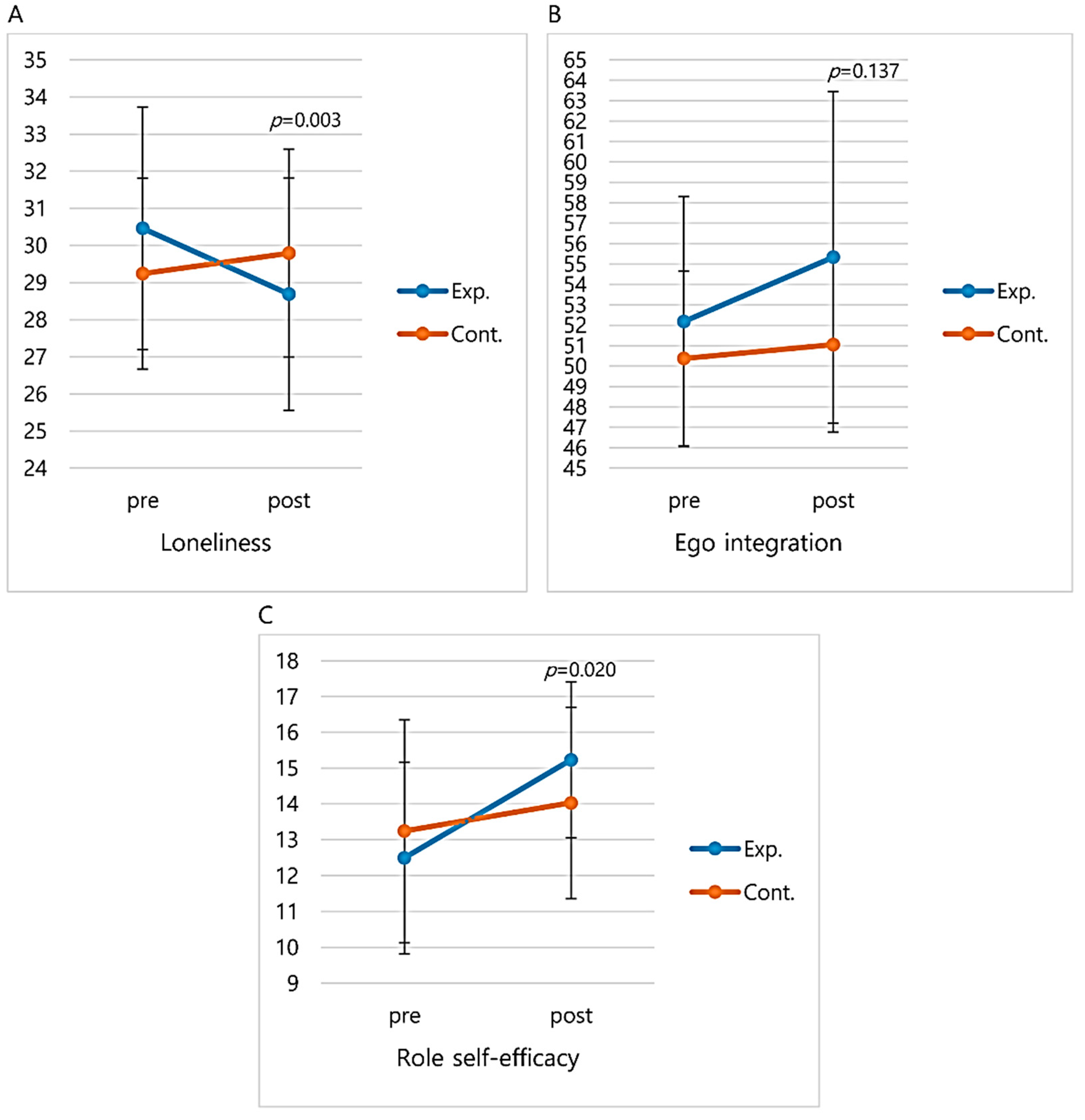
4.2. Effect of the Integrated Healthcare Program
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Future Demographic Estimates. Available online: http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1BPA001&conn_path=I2 (accessed on 12 June 2018).
- Kim, S.H.; Park, S. A meta-analysis of the correlates of successful aging in older adults. Res. Aging 2017, 39, 657–677. [Google Scholar] [CrossRef]
- Innes, K.E.; Selfe, T.K.; Khalsa, D.S.; Kandati, S. Effects of meditation versus music listening on perceived stress, mood, sleep, and quality of life in adults with early memory loss: A pilot randomized controlled trial. J. Alzheimers Dis. 2016, 52, 1277–1298. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.; Oh, H. Evaluating the comprehensive model of ego-integrity for senior patients in convalescent hospitals: Influence factors and outcome variables. Int. J. Bio. Sci. Bio. Technol. 2015, 7, 317–326. [Google Scholar] [CrossRef]
- Son, J.S.; Kang, D.; Yoon, D.H.; Kim, D.Y.; Kim, H.J.; Kim, J.H.; So, B.; Song, H.S.; Hwang, S.S.; Song, W. Effects of high-speed elastic band training on physical fitness and muscle function in rural community-dwelling elderly: A single-blinded randomized controlled trial. Korean. J. Health Promot. 2015, 15, 254–261. [Google Scholar] [CrossRef]
- Jung, H.W.; Kim, S.W.; Chin, H.J.; Kim, C.H.; Kim, K.I. Skeletal muscle mass as a predictor of mortality in the elderly population. Korean J. Med. 2013, 85, 167–173. [Google Scholar] [CrossRef]
- Lee, S.H.; Hong, G.R.; Kim, B.J.; Kim, E.H. Effects of aging process exercise program on walking ability and frailty of elderly women in rural. Korean J. Sports Sci. 2018, 27, 1115–1126. [Google Scholar] [CrossRef]
- Lee, M.G.; Quam, J.K. Comparing supports for LGBT aging in rural versus urban areas. J. Gerontol. Soc. Work 2013, 56, 112–126. [Google Scholar] [CrossRef]
- Roy, C. The Roy Adaptation Model, 3rd ed.; Pearson: Upper Saddle River, NJ, USA, 2009. [Google Scholar]
- Borzou, S.R.; Mohammadi, S.K.; Falahinia, G.H.; Mousavi, S.; Khalili, Z. Effects of Roy’s adaptation model in nursing practice on the quality of life in patients with type II diabetes. J. Nurs. Midwifery Sci. 2015, 2, 1–7. [Google Scholar]
- Hoogendijk, E.O. How effective is integrated care for community-dwelling frail older people? The case of the Netherlands. Age Ageing 2016, 45, 587–590. [Google Scholar] [CrossRef]
- Lee, H.-S.; Choi, G.-H.; Yoo, Y.-K.; Lm, S.I. Meta-analysis of study of the education and the effective treatment programs for the aged. Korean J. Gerontol. Soc. Welf. 2012, 56, 93–114. [Google Scholar] [CrossRef]
- Liu, L.; Gou, Z.; Zuo, J. Social support mediates loneliness and depression in elderly people. J. Health Psychol. 2016, 21, 750–758. [Google Scholar] [CrossRef]
- Park, G.S.; Park, Y.R.; Youm, Y.S. The effects of social participation on health related quality of life among rural elderly. Ment. Health Soc. Work 2015, 43, 200–227. [Google Scholar]
- Choi, M.Y.; Lee, S.E.; Park, H.S. The effect of elderly’s social exclusion on elderly depression: Focusing on the mediating role of working. Korean J. Gerontol. Soc. Welf. 2015, 69, 9–30. [Google Scholar]
- Park, S.; Park, Y.H. Predictors of physical activity in Korean older adults: Distinction between urban and rural areas. J. Korean Acad. Nurs. 2010, 40, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Wilcox, S.; Bopp, M.; Oberrecht, L.; Kammermann, S.K.; McElmurray, C.T. Psychosocial and perceived environmental correlates of physical activity in rural and older African American and white women. J. Gerontol. B Psychol. Sci. Soc. Sci. 2003, 58, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Nishiguchi, S.; Yamada, M.; Tanigawa, T.; Sekiyama, K.; Kawagoe, T.; Suzuki, M.; Tsuboyama, T. A 12-week physical and cognitive exercise program can improve cognitive function and neural efficiency in community-dwelling older adults: A randomized controlled trial. J. Am. Geriatr. Soc. 2015, 63, 1355–1363. [Google Scholar] [CrossRef]
- Ferretti, L.; McCallion, P.; McDonald, E.; Kye, H.; Herrera-Venson, A.P.; Firman, J. Assessing the effectiveness of the aging mastery program. Healthcare 2018, 6, 41. [Google Scholar] [CrossRef]
- Huang, T.T.; Liu, C.B.; Tsai, Y.H.; Chin, Y.F.; Wong, C.H. Physical fitness exercise versus cognitive behavior therapy on reducing the depressive symptoms among community-dwelling elderly adults: A randomized controlled trial. Int. J. Nurs. Stud. 2015, 52, 1542–1552. [Google Scholar] [CrossRef]
- Korea Institute of Sport Science. A Survey on Overseas Elderly Health Promotion Program for the Age of 100; Korea e-Work Association for the Disabled: Seoul, Korea, 2014. [Google Scholar]
- Oh, S.L.; Kim, H.J.; Woo, S.; Cho, B.L.; Song, M.; Park, Y.H.; Song, W. Effects of an integrated health education and elastic band resistance training program on physical function and muscle strength in community-dwelling elderly women: Healthy aging and happy aging II study. Geriatr. Gerontol. Int. 2017, 17, 825–833. [Google Scholar] [CrossRef]
- Marmeleira, J.; Galhardas, L.; Raimundo, A. Exercise merging physical and cognitive stimulation improves physical fitness and cognitive functioning in older nursing home residents: A pilot study. Geriatr. Nurs. 2018, 39, 303–309. [Google Scholar] [CrossRef]
- Im, M.L.; Lee, J.I. Effects of art and music therapy on depression and cognitive function of the elderly. Technol. Health Care. 2014, 22, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Rawtaer, I.; Mahendran, R.; Yu, J.; Fam, J.; Feng, L.; Kua, E.H. Psychosocial interventions with art, music, Tai Chi and mindfulness for subsyndromal depression and anxiety in older adults: A naturalistic study in Singapore. Asia Pac. Psychiatry 2015, 7, 240–250. [Google Scholar] [CrossRef]
- Ciasca, E.C.; Ferreira, R.C.; Santana, C.L.A.; Forlenza, O.V.; Dos Santos, G.D.; Brum, P.S.; Nunes, P.V. Art therapy as an adjuvant treatment for depression in elderly women: A randomized controlled trial. Braz. J. Psychiatry 2018, 40, 256–263. [Google Scholar] [CrossRef]
- Han, A.R.; Park, S.A.; Ahn, B.E. Reduced stress and improved physical functional ability in elderly with mental health problems following a horticultural therapy program. Complement. Ther. Med. 2018, 38, 19–23. [Google Scholar] [CrossRef]
- Yoshikawa, Y.; Ohmaki, E.; Kawahata, H.; Maekawa, Y.; Ogihara, T.; Morishita, R.; Aoki, M. Beneficial effect of laughter therapy on physiological and psychological function in elders. Nurs. Open 2019, 6, 93–99. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Senior Fitness Test Manual, 2nd ed.; Human Kinetics: New Zealand, Australia, 2013. [Google Scholar]
- Mathias, S.; Nayak, U.S.; Isaacs, B. Balance in elderly patients: The “get-up and go” test. Arch. Phys. Med. Rehabil. 1986, 67, 387–389. [Google Scholar]
- Russell, D.; Peplau, L.A.; Cutrona, C.E. The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. J. Personal. Soc. Psychol. 1980, 39, 472–480. [Google Scholar] [CrossRef]
- Kim, O.S. Korean version of the revised UCLA loneliness scale: Reliability and validity test. J. Korean Acad. Nurs. 1997, 27, 871–879. [Google Scholar] [CrossRef]
- Hong, Z.Y. Reminiscence Functions Predictors in the Elderly. Ph.D. Thesis, Ewha Women’s University, Seoul, Korea, 2016. [Google Scholar]
- Kim, M.H.; Shin, K.R. The study on the development of the “Successful Aging” scale for Korean elderly. J. Korean Geriatr. Soc. 2005, 25, 35–52. [Google Scholar]
- Wongcharoen, S.; Sungkarat, S.; Munkhetvit, P.; Lugade, V.; Silsupadol, P. Home-based interventions improve trained, but not novel, dual-task balance performance in older adults: A randomized controlled trial. Gait. Posture 2017, 52, 147–152. [Google Scholar] [CrossRef]
- Oliveira Gonçalves, I.; Bandeira, A.N.; Coelho-Júnior, H.J.; Silva Aguiar, S.; Minucci Camargo, S.; Yukio Asano, R.; Batista Júnior, M.L. Multicomponent exercise on physical function, cognition and hemodynamic parameters of community-dwelling older adults: A quasi-experimental study. Int. J. Environ. Res. Public Health 2019, 16, 2184. [Google Scholar] [CrossRef]
- Frank, J.S.; Patla, A.E. Balance and mobility challenges in older adults: Implications for preserving community mobility. Am. J. Prev. Med. 2003, 25, 157–163. [Google Scholar] [CrossRef]
- Jo, H.; Song, E. The effect of reminiscence therapy on depression, quality of life, ego-integrity, social behavior function, and activities of daily living in elderly patients with mild dementia. Educ. Gerontol. 2014, 41, 1–13. [Google Scholar] [CrossRef]
- Imamura, H.; Nakamura, H.; Nishiwaki, Y. Relationship between the well-being of elderly men and cohabiting with women who have had experience as a health promotion volunteer in Japan: A cross-sectional study. Int. J. Environ. Res. Public Health 2018, 16, 65. [Google Scholar] [CrossRef]
- Battaglia, G.; Bellafiore, M.; Alesi, M.; Paoli, A.; Bianco, A.; Palma, A. Effects of an adapted physical activity program on psychophysical health in elderly women. Clin. Interv. Aging 2016, 11, 1009–1015. [Google Scholar] [CrossRef]
- Birkenes, T.S.; Myklebust, H.; Kramer-Johansen, J. Time delays and capability of elderly to activate speaker function for continuous telephone CPR. Scand. J. Trauma Resusc. Emerg. Med. 2013, 21, 1–6. [Google Scholar] [CrossRef]
- Goelitz, D.; Trenkamp, C.; Paulus, P. Leisure activities in care homes: How do they relate to the well-being of the elderly? In Leisure, Health and Well-Being: A Holistic Approach; Benkő, Z., Modi, I., Tarkó, K., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 73–77. [Google Scholar]
- Chruściel, P.; Dobrowolska, B. The correlation between social support and quality of life of seniors without cognitive disorders from an institutional environment—A descriptive cross-sectional survey. Healthcare 2020, 8, 212. [Google Scholar] [CrossRef]
- Li, C.; Jiang, S.; Li, N.; Zhang, Q. Influence of social participation on life satisfaction and depression among Chinese elderly: Social support as a mediator. J. Community Psychol. 2018, 46, 345–355. [Google Scholar] [CrossRef]
- Rogers, C.; Keller, C. Roy’s adaptation model to promote physical activity among sedentary older adults. Geriatr. Nurs. 2009, 30, 21–26. [Google Scholar] [CrossRef]
- Chatters, L.M.; Taylor, H.O.; Nicklett, E.J.; Taylor, R.J. Correlates of objective social isolation from family and friends among older adults. Healthcare 2018, 6, 24. [Google Scholar] [CrossRef]

| Session | Contents | Rationale Based on Roy Adaptation Model | Time(min) |
|---|---|---|---|
| 1 |
| 30 10 80 | |
| 2 |
|
| 30 20 70 |
| 3 |
|
| 90 30 |
| 4 |
|
| 30 20 70 |
| 5 |
|
| 50 20 50 |
| 6 |
|
| 100 20 |
| 7 |
|
| 50 20 50 |
| 8 |
|
| 60 60 |
| 9 |
|
| 30 20 70 |
| 10 |
|
| 30 20 70 |
| 11 |
|
| 30 20 70 |
| 12 |
|
| 30 20 70 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.J.; Kim, H.Y.; Yang, Y.; Ko, E. Effect of an Integrated Healthcare Program for Korean Rural Older Adults: A Quasi-Experimental Study. Healthcare 2020, 8, 244. https://doi.org/10.3390/healthcare8030244
Kim HJ, Kim HY, Yang Y, Ko E. Effect of an Integrated Healthcare Program for Korean Rural Older Adults: A Quasi-Experimental Study. Healthcare. 2020; 8(3):244. https://doi.org/10.3390/healthcare8030244
Chicago/Turabian StyleKim, Hyuk Joon, Hye Young Kim, Youngran Yang, and Eun Ko. 2020. "Effect of an Integrated Healthcare Program for Korean Rural Older Adults: A Quasi-Experimental Study" Healthcare 8, no. 3: 244. https://doi.org/10.3390/healthcare8030244
APA StyleKim, H. J., Kim, H. Y., Yang, Y., & Ko, E. (2020). Effect of an Integrated Healthcare Program for Korean Rural Older Adults: A Quasi-Experimental Study. Healthcare, 8(3), 244. https://doi.org/10.3390/healthcare8030244





