Assessment of Equity in Access to Percutaneous Coronary Intervention (PCI) Centres in Poland
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lumme, S.; Manderbacka, K.; Keskimaki, I. Trends of relative and absolute socioeconomic equity in access to coronary revascularisations in 1995–2010 in Finland: A register study. Int. J. Equity Health 2017, 16, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kirchberger, I.; Meisinger, C.; Goluke, H.; Heier, M.; Kuch, B.; Peters, A.; Quinones, P.A.; von Scheidt, W.; Mielck, A. Long-term survival among older patients with myocardial infarction differs by educational level: Results from the MONICA/KORA myocardial infarction registry. Int. J. Equity Health 2014, 13, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef] [PubMed]
- Roffi, M.; Patrono, C.; Collet, J.P.; Mueller, C.; Valgimigli, M.; Andreotti, F.; Bax, J.J.; Borger, M.A.; Brotons, C.; Chew, D.P.; et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2016, 37, 267–315. [Google Scholar] [CrossRef]
- Katritsis, D.G.; Siontis, G.C.M.; Kastrati, A.; van’t Hof, A.W.J.; Neumann, F.J.; Siontis, K.C.M.; Ioannidis, J.P.A. Optimal timing of coronary angiography and potential intervention in non-ST-elevation acute coronary syndromes. Eur. Heart J. 2011, 32, 32–40. [Google Scholar] [CrossRef]
- Pinto, D.S.; Kirtane, A.J.; Nallamothu, B.K.; Murphy, S.A.; Cohen, D.J.; Laham, R.J.; Cutlip, D.E.; Bates, E.R.; Frederick, P.D.; Miller, D.P.; et al. Hospital delays in reperfusion for ST-Elevation myocardial infarction implications when selecting a reperfusion strategy. Circulation 2006, 114, 2019–2025. [Google Scholar] [CrossRef]
- Terkelsen, C.J.; Sørensen, J.T.; Maeng, M.; Jensen, L.O.; Tilsted, H.H.; Trautner, S.; Vach, W.; Johnsen, S.P.; Thuesen, L.; Lassen, J.F. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA 2010, 304, 763–771. [Google Scholar] [CrossRef] [PubMed]
- Henry, T.D.; Sharkey, S.W.; Burke, M.N.; Chavez, I.J.; Graham, K.J.; Henry, C.R.; Lips, D.L.; Madison, J.D.; Menssen, K.M.; Mooney, M.R.; et al. A Regional System to Provide Timely Access to Percutaneous Coronary Intervention for ST-Elevation Myocardial Infarction. Circulation 2007, 116, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Le May, M.R.; So, D.Y.; Dionne, R.; Glover, C.A.; Froeschl, M.P.; Wells, G.A.; Davies, R.F.; Sherrard, H.L.; Maloney, J.; Marquis, J.F.; et al. A Citywide Protocol for Primary PCI in ST-Segment Elevation Myocardial Infarction. N. Engl. J. Med. 2008, 358, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Nallamothu, B.K.; Krumholz, H.M.; Ko, D.T.; LaBresh, K.A.; Rathore, S.; Roe, M.T.; Schwamm, L. Development of Systems of Care for ST-Elevation Myocardial Infarction Patients. Gaps, Barriers, and Implications. Circulation 2007, 116, e68–e72. [Google Scholar] [CrossRef] [PubMed]
- Poloński, L.; Gasior, M.; Gierlotka, M.; Kalarus, Z.; Cieśliński, A.; Dubiel, J.S.; Gil, R.J.; Ruzyłło, W.; Trusz-Gluza, M.; Zembala, M.; et al. Polish Registry of Acute Coronary Syndromes (PL-ACS). Characteristics, treatments and outcomes of patients with acute coronary syndromes in Poland. Kardiol. Pol. 2007, 65, 861–872. [Google Scholar]
- Sowada, C.; Sagan, A.; Kowalska-Bobko, I. Health System Review 2019; WHO: Geneva, Switzerland; Regional Office for Europe: Copenhagen, Denmark, 2019. [Google Scholar]
- Jaworzynńska, M. A Comparative Analysis of the Health System Financing in Poland and Selected Countries. Econ. Sociol. 2016, 9, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Rój, J. Relationship between Funding Mechanism and Service Effectiveness of Hospital. In The Economics of Health Reforms; Yfantopoulos, J.N., Ed.; ATINER: Athens, Greece, 2004; pp. 507–518. [Google Scholar]
- Rój, J. The Cost Efficiency of Hospitals in Poland. In Themes on Health Care: Challenges and Future Actions; Boutsioli, Z., Ed.; ATINER: Athens, Greece, 2009; pp. 306–320. [Google Scholar]
- Rój, J. Znaczenie Czynnika Finansowego w Rozwoju Technologii Medycznych w Klinice Uniwersyteckiej (The Importance of the Financial Factor in the Development of Health Technologies in the University Clinic); Wydawnictwo UEP: Poznań, Poland, 2011. [Google Scholar]
- Mossialos, E. Health Systems in Transition, Poland. Health System Review. European Observatory on Health Systems and Policies. Volume 13 No. 8. Available online: http://www.euro.who.int/__data/assets/pdf_file/0018/163053/e96443.pdf (accessed on 10 December 2018).
- Balańzs, N. Improving the Allocation of Health Care Resources in Poland. 2015. Available online: http://www.euro.who.int/__data/assets/pdf_file/0011/273863/ImprovingAllocationHealthCareresourcesPoland.pdf?ua=1 (accessed on 10 December 2018).
- Constitution of the World Health Organization; World Health Organization: Geneva, Switzerland, 1948.
- The Constitution of the Republic of Poland of 2nd April; Dziennik Ustaw No 78, item 483: Warszawa, Poland, 1997.
- National Health Program. Ministry of Health. Available online: https://www.gov.pl/web/zdrowie (accessed on 10 December 2018).
- Polkard. Program Polityki Zdrowotnej. In Program Profilaktyki i Leczenia Chorób Układu Sercowo-Naczyniowego POLKARD na lata 2017-2020; Minister Zdrowia: Warszawa, Poland, 2019. [Google Scholar]
- Wojtyniak, B.; Goryński, P. Sytuacja Zdrowotna Ludności Polski i jej Uwarunkowania. (The Health Situation of the Polish Population and Its Determinants); NIZP-PZH: Warszawa, Poland, 2016. [Google Scholar]
- Raport NIK. Informacja o wynikach kontroli. Realizacja świadczeń zdrowotnych z zakresu kardiologii przez publiczne i niepubliczne podmioty lecznicze. (Information about the Results of the Inspection. Implementation of Health Services in the Field of Cardiology by Public and Non-Public Entities); LKA-4101-039/2014 Nr ewid. 1/2016/P/14078/LKA; NIK: Warszawa, Poland, 2016. [Google Scholar]
- OECD/EU. Health at a Glance: Europe 2018: State of Health in the EU Cycle; OECD Publishing: Paris, France, 2018. [Google Scholar]
- AISN. Available online: http://www.aisn.pl/pracownie/baza_pracowni (accessed on 10 May 2019).
- Statistics Poland. Polish Statistical Yearbook. Available online: https://stat.gov.pl/obszary-tematyczne/ludnosc/powierzchnia-i-ludnosc-w-przekroju-terytorialnym-w-2018-roku,7,15.html (accessed on 10 May 2019).
- NFZ. Available online: https://statystyki.nfz.gov.pl/ (accessed on 1 August 2019).
- Druckman, A.; Jackson, T. Measuring resource inequalities: The concepts and methodology for an area-based gini coefficient. Ecol. Econ. 2008, 65, 242–252. [Google Scholar] [CrossRef]
- Gini, C. Variabilita e mutabilita 1912 reprinted. In Memorie di Metodologica Statistica; Pizetti, E., Salvemini, T., Eds.; Libreria Eredi Virgilio Veschi: Rome, Italy, 1955. [Google Scholar]
- Gini, C. On the measurement of concentration and variability of characters. Metron Int. J. Stat. 2005, LXIII, 1–38. [Google Scholar]
- Zhang, T.; Xu, Y.; Ren, J.; Sun, L.; Liu, C. Inequlity in the distribution of health resources and health services in China: Hospitals versus primary care institutions. Int. J. Equity Health 2017, 16, 1–8. [Google Scholar] [CrossRef]
- Jin, J.; Wang, J.; Ma, X.; Wang, Y.; Li, R. Equality of Medical Health Resource Allocation in China Based on the Gini Coefficient Method. Iran. J. Public Health 2015, 44, 445–457. [Google Scholar]
- Frankfort-Nachmias, C.; Nachmias, D. Metody Badawcze w Naukach Społecznych (Research Methods in Social Sciences); Wydawnictwo Zysk i S-ka: Poznań, Poland, 2001. [Google Scholar]
- Aczel, A.D. Statystyka w Zarządzaniu (Statistics in Management); Wydawnictwo Naukowe PWN: Warszawa, Poland, 2000. [Google Scholar]
- Rashid, S.; Simms, A.; Batin, P.; Kurian, J.; Gale, C.P. Inequalities in care in patients with acute myocardial infarction. World J. Cardiol. 2015, 7, 895–901. [Google Scholar] [CrossRef]
- Joensen, A.M.; Joergensen, T.; Lundbye-Christensen, S.; Johansen, M.B.; Guzman-Castillo, M.; Bandosz, P.; Hallas, J.; Prescott, E.I.B.; Capewell, S.; O’Flaherty, M. Explaining trends in coronary healrt disease mortality in different socioeconomic groups in Denmark 1991–2007 using the IMPACTSECmodel. PLoS ONE 2018, 13, e0194793. [Google Scholar] [CrossRef]
- Nicholas, O.; Gale, C.P.; Ludman, P.; de Belder, M.A.; Timmis, A.; Fox, K.A.A.; Simpson, I.A.; Redwood, S.; Ray, A.G. Total Center Percutaneous Coronary Intervention Volume and 30-Day Mortality. Circ. Cardiovasc. Qual. Outcomes 2017, 10, 1–11. [Google Scholar]
- Artaiz, M.; Salterain, N.; Fernandez Montero, A.; Hernandez-Hernandez, A.; Canepa Leite, J.P.; Calabuig-Nogues, J. Percutaneous coronary intervention in Navarre. Outcomes of a low volume centre. An. Del Sist. Sanit. De Navar. 2016, 39, 87–97. [Google Scholar]
- Jankowiak, M. Konwergencja ochrony zdrowia w państwach Unii Europejskiej (Convergence of Health Care in European Union Member States). Polityka Społeczna 2010, 7, 6–10. [Google Scholar]
- Jankowiak, M. Convergence of Health Care Systems in European Union Countries in The Light of Quantitative Statistical Evaluations; Working Papers in Management, Finance and Economics; MBA Poznań-Atlanta: Poznań, Poland, 2010; p. 1. [Google Scholar]
- Wojtyniak, B.; Jankowski, K.; Zdrojewski, T.; Opolski, G. Regional differences in determining cardiovascular diseases as the cause of death in Poland: Time for change. Kardiol. Pol. 2012, 70, 695–701. [Google Scholar] [PubMed]
- Gierlotka, M.; Wojtyniak, B.; Zdrojewski, T.; Gasior, M.; Polonski, L.; Wierucki, L.; Zembala, M.; Kalarus, Z.; Wysocki, M.; Opolski, G. Age and gender differences in place and causes of deaths of acute myocardial infarction in-patients in a 3-year observation after discharge. Eur. Heart J. 2015, 36, 163–508. [Google Scholar]
- Marek, M.; Chłoń-Domińczak, A.; Kaleta, D.; Mazur, J.; Miśkiewicz, P.; Poznańska, D.; Stokwiszewski, J.; Wotyniak, B.; Zdrojewski, T. Social Inequalities in Health in Poland; World Health Organization: Copenhagen, Denmark, 2012. [Google Scholar]
- Baeten, R.; Spasova, S.; Vanhercke, B.; Coster, S. Inequalities in Access to Healthcare. A Study of National Policies; European Social Policy Network (ESPN), European Commission: Brussels, Belgium, 2018. [Google Scholar]
- Regions and Cities at a Glance 2018 – POLAND. Available online: http://oecd.org/cfe/POLAND-Regions-and-Cities-2018.pdf (accessed on 31 January 2020).
- GUS. Regions of Poland 2019; GUS: Warszawa, Poland, 2019. [Google Scholar]
| District (Voivodeship) | Area in Squar km a | Population a | Number of PCI Centres b | Hospit. due to Coronarographies c | Hospit. due to PCI Procedures c |
|---|---|---|---|---|---|
| Lower Silesian | 19,947 | 2,901,225 | 12 | 978 | 4828 |
| Kuyavian-Pomeranian | 17,972 | 2,077,775 | 10 | 786 | 3557 |
| Lubelskie | 25,122 | 2,117,619 | 7 | 512 | 3115 |
| Lubuskie | 13,988 | 1,014,548 | 4 | 810 | 2216 |
| Łódź | 18,219 | 2,466,322 | 13 | 773 | 4556 |
| Lesser Poland | 15,183 | 3,400,577 | 11 | 830 | 4402 |
| Masovian | 35,558 | 5,403,412 | 20 | 1794 | 7373 |
| Opole | 9412 | 986,506 | 4 | 294 | 1430 |
| Podkarpackie | 17,846 | 2,129,015 | 7 | 493 | 2860 |
| Podlaskie | 20,187 | 1,181,533 | 5 | 316 | 1394 |
| Pomeranian | 18,310 | 2,333,523 | 10 | 745 | 3465 |
| Silesian | 12,333 | 4,533,565 | 16 | 1331 | 7498 |
| Świętokrzyskie | 11,711 | 1,241,546 | 8 | 570 | 2136 |
| Warmian-Masurian | 24,173 | 1,428,983 | 4 | 465 | 1965 |
| Wielkopolska | 29,826 | 3,493,969 | 14 | 1130 | 5060 |
| Zachodniopomorskie | 22,892 | 1,701,030 | 4 | 311 | 2314 |
| Total - Poland | 312,679 | 38,411,148 | 149 | 12,138 | 58,17 |
| PCI Centres | Mean | Median | Max. | Min. | Std. Dev. * | Variance |
|---|---|---|---|---|---|---|
| Per 1000 km2 | 0.51 | 0.51 | 1.30 | 0.17 | 0.28 | 0.08 |
| Per 100000 people | 0.40 | 0.40 | 0.64 | 0.23 | 0.10 | 0.01 |
| Statistics | Hospitalisations per 100,000 Population due to: | ||
|---|---|---|---|
| Coronarographies and PCIs | Coronarographies Only | PCIs Only | |
| Mean value | 186.87 | 33.41 | 153.46 |
| Median | 175.96 | 31.63 | 146.03 |
| Maximum value | 298.26 | 79.84 | 218.42 |
| Minimum value | 144.73 | 18.28 | 117.98 |
| Standard deviation | 37.28 | 13.94 | 25.07 |
| Coefficient of variation | 19.9% | 41.7% | 16.3% |
| PCI Centres | Gini Coefficient |
|---|---|
| Per 1000 km2 | 28.02% |
| Per 100,000 population | 12.87% |
| Number of PCI Centres: | Hospitalisations Per 100,000 Population due to: | ||
|---|---|---|---|
| Coronarographies and PCIs | Coronarographies Only | PCIs Only | |
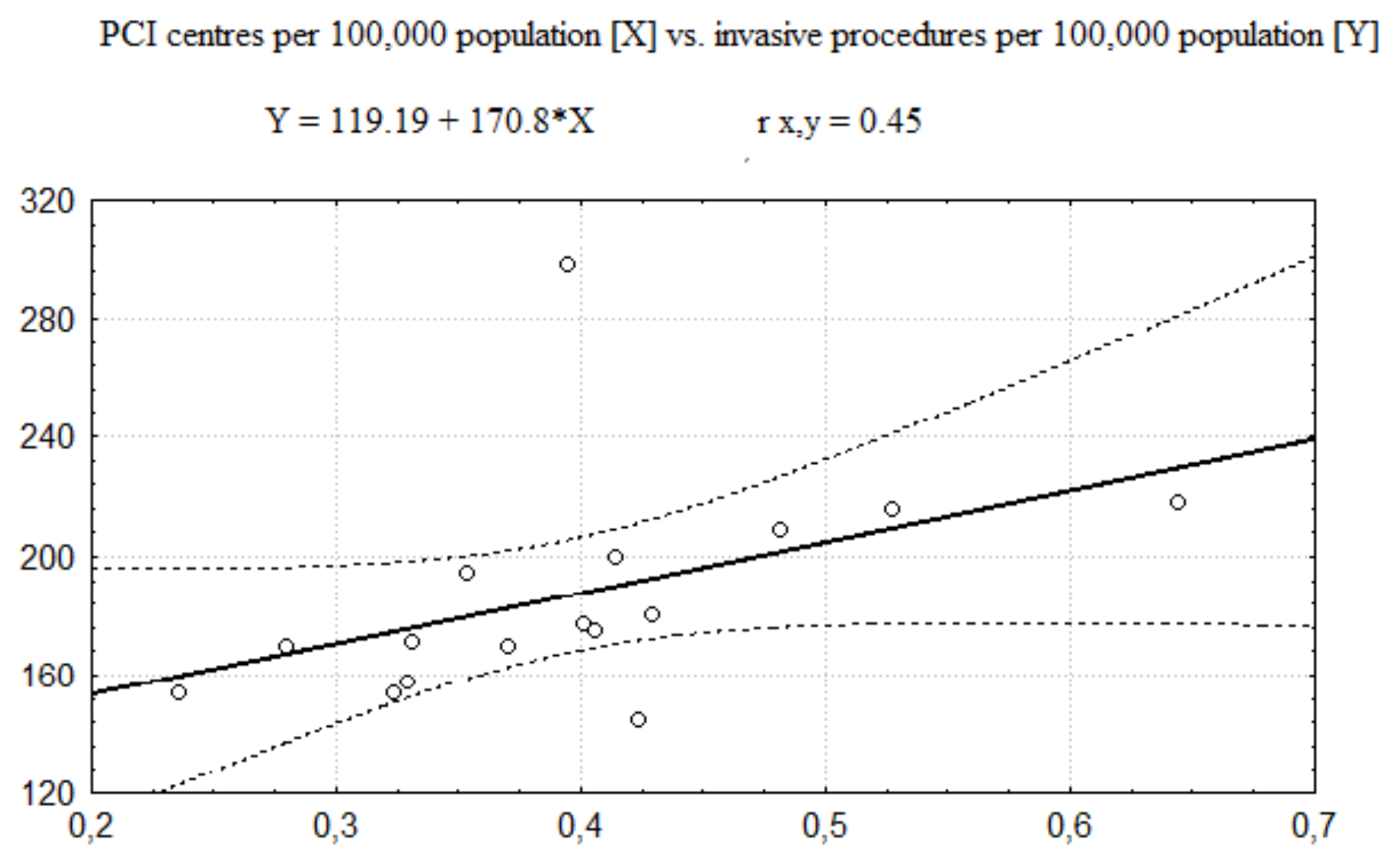
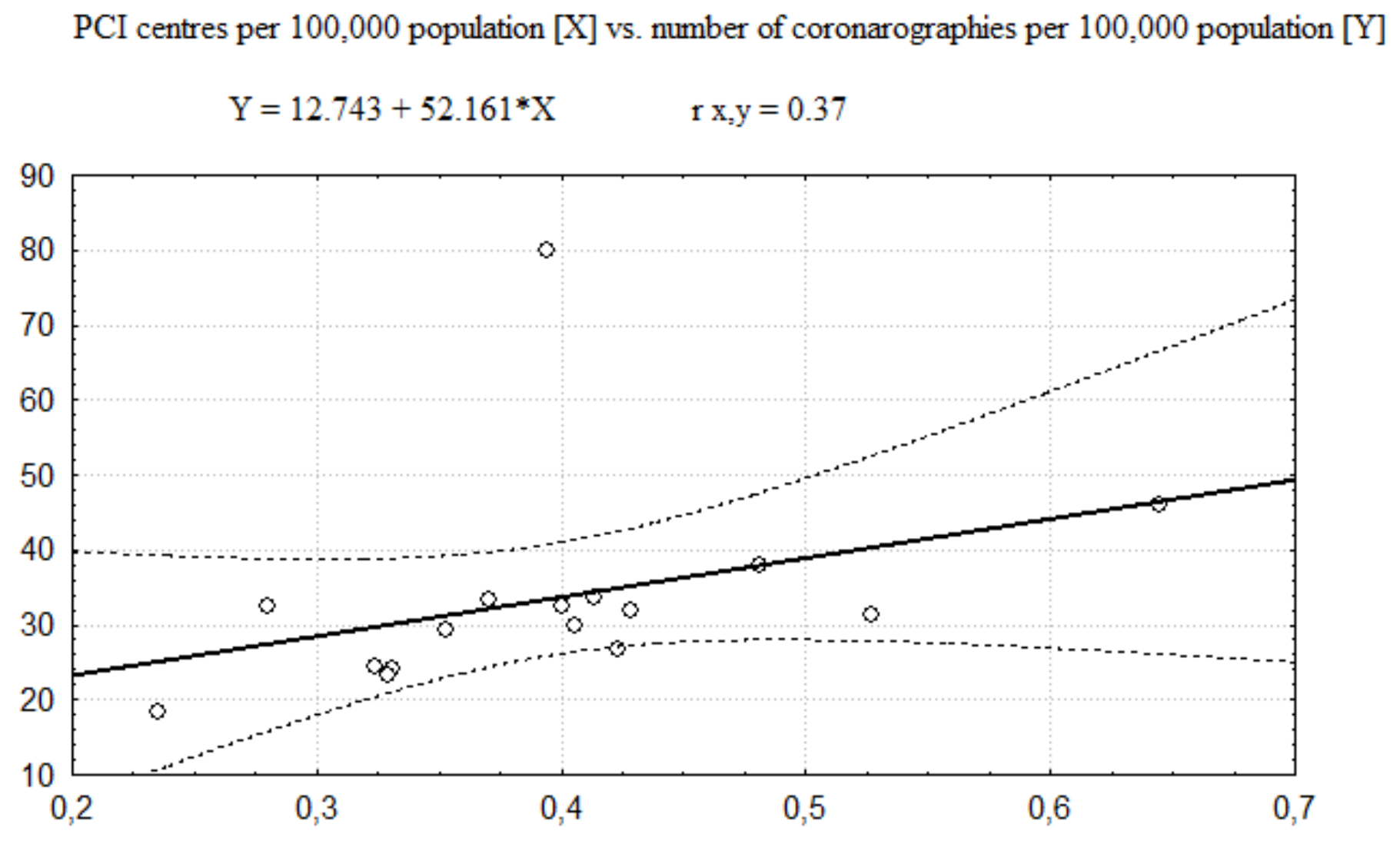
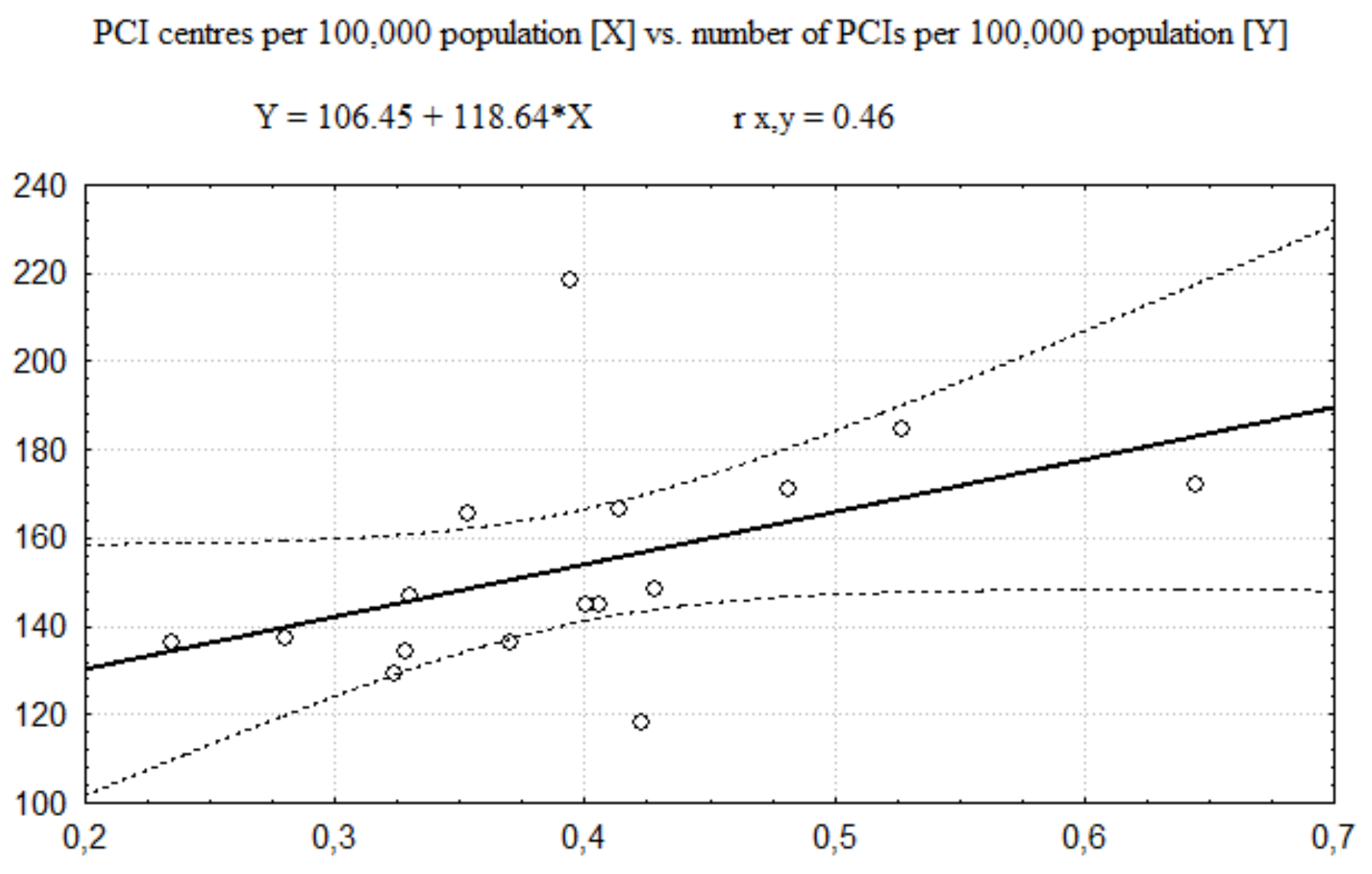
| Per 100,000 population | rX,Y = 0.45 | rX,Y = 0.37 | rX,Y = 0.46 |
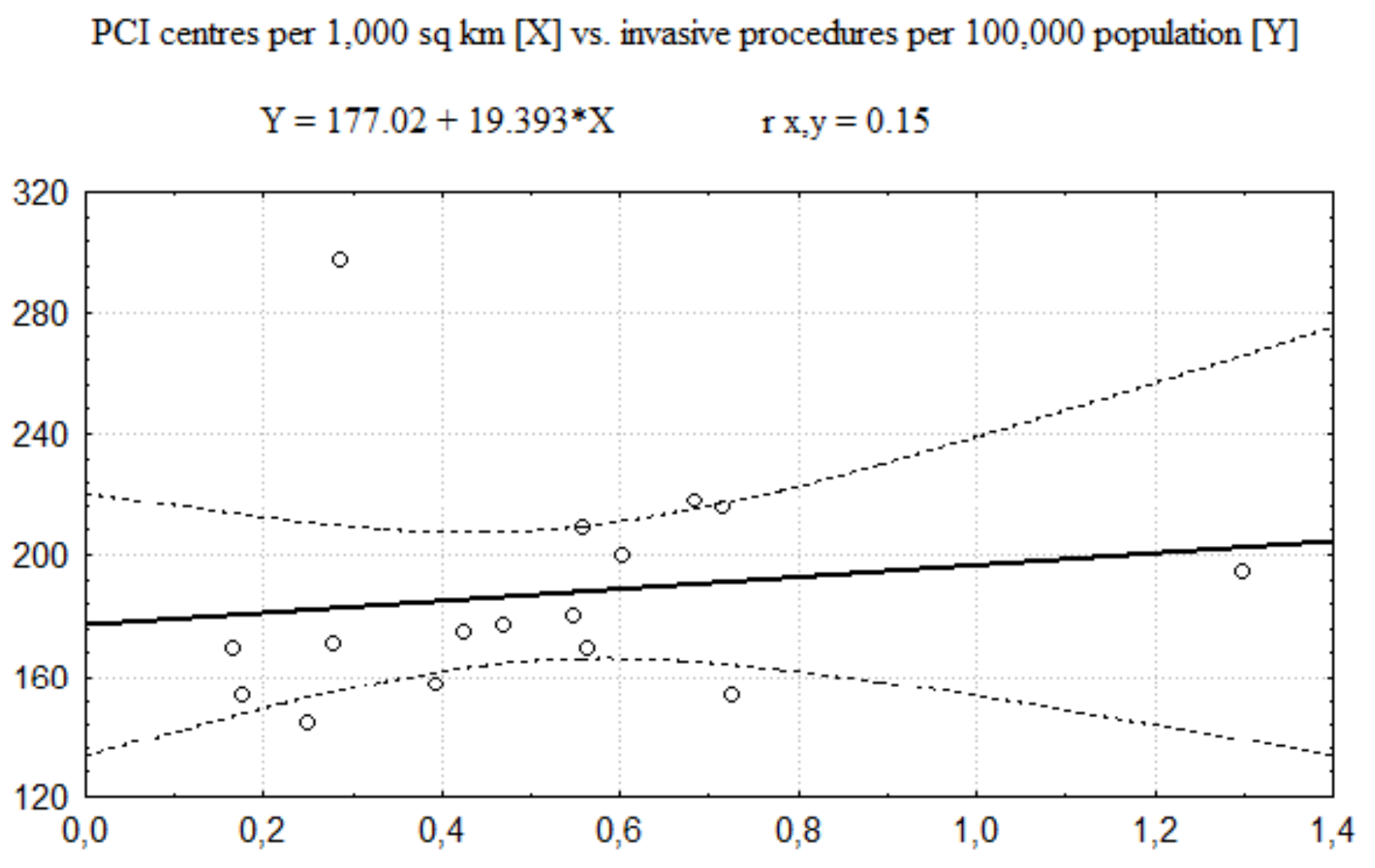
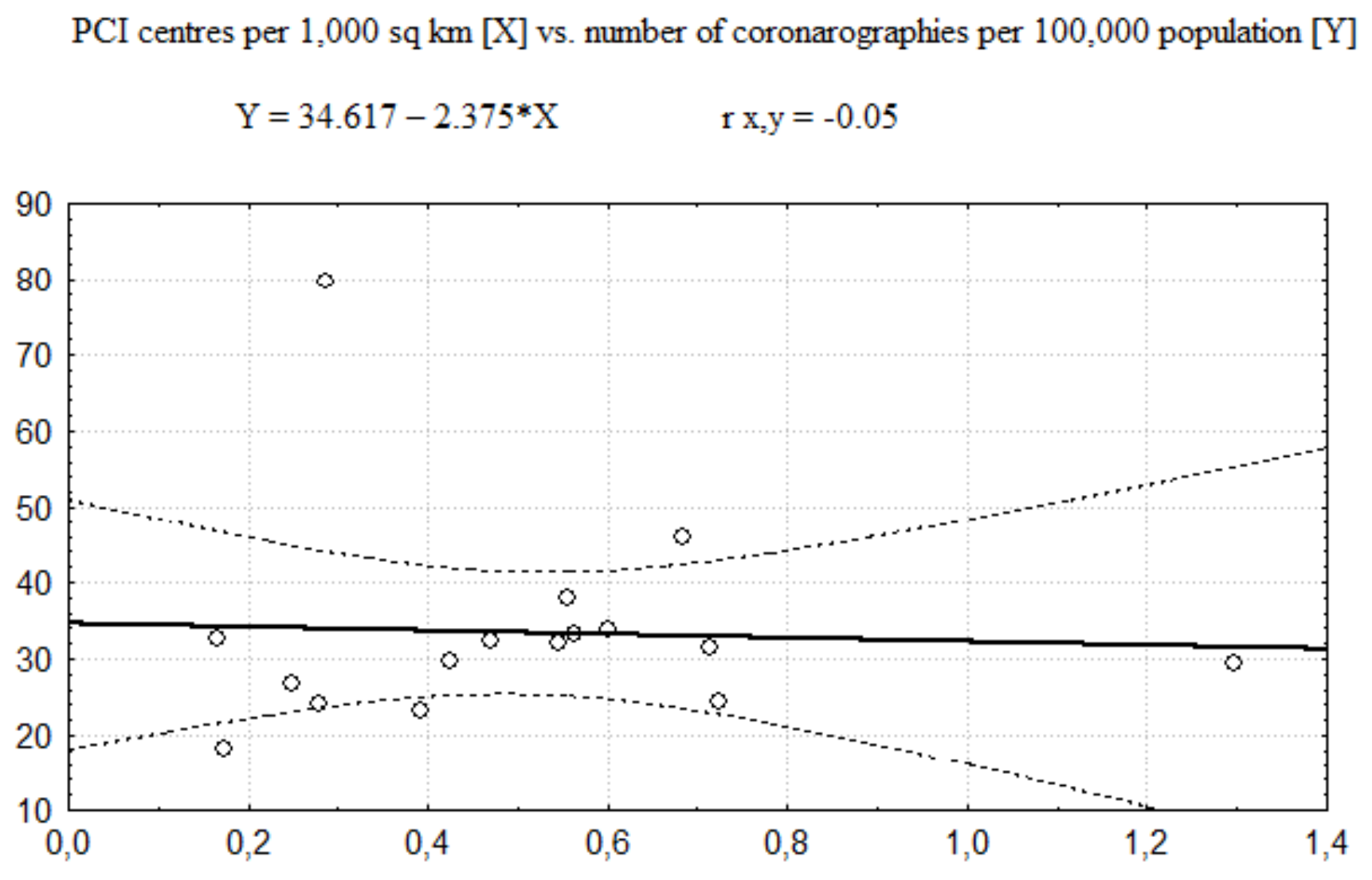
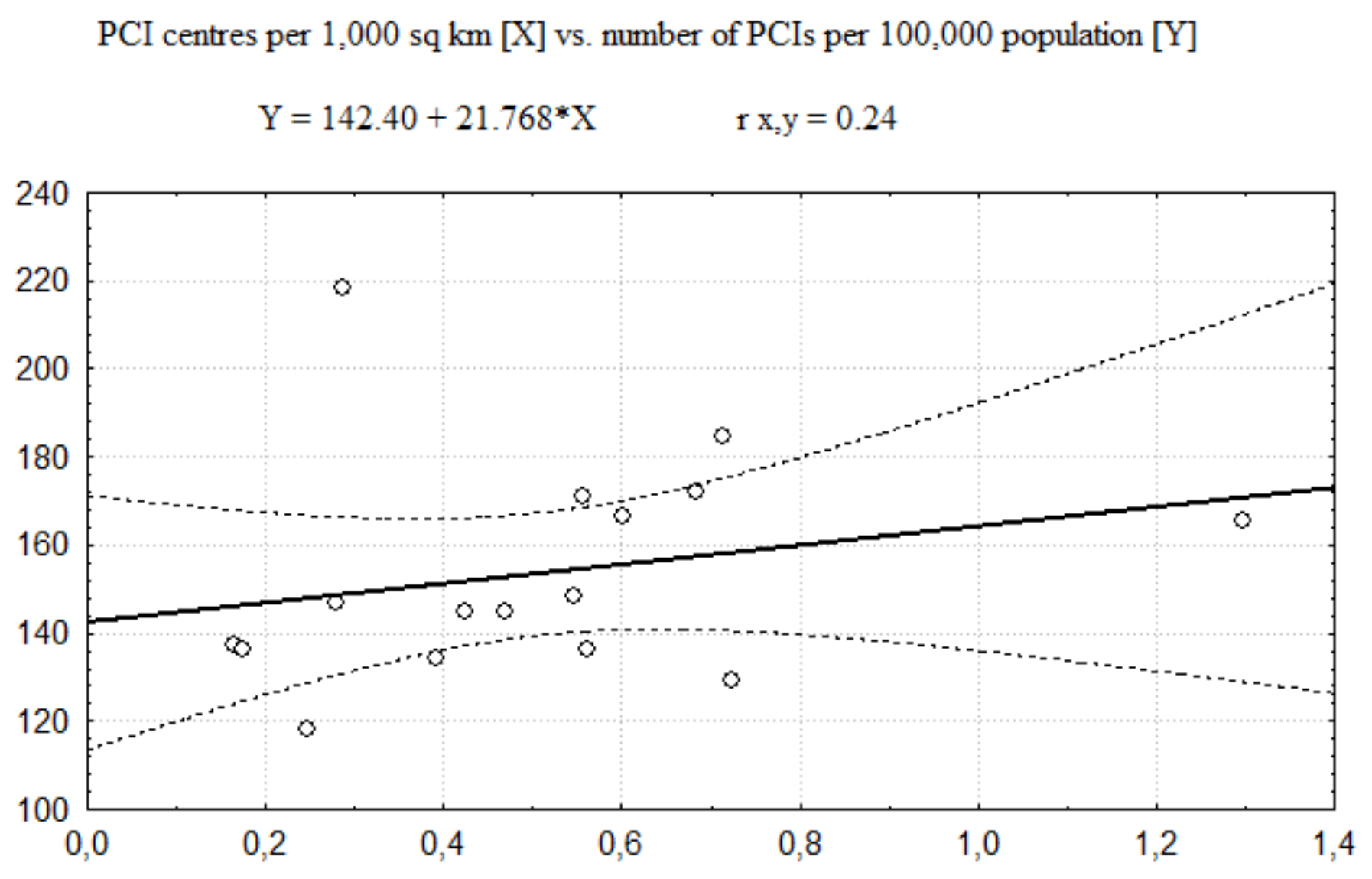
| Per 1000 km2 | rX,Y = 0.15 | rX,Y = −0.05 | rX,Y = 0.24 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rój, J.; Jankowiak, M. Assessment of Equity in Access to Percutaneous Coronary Intervention (PCI) Centres in Poland. Healthcare 2020, 8, 71. https://doi.org/10.3390/healthcare8020071
Rój J, Jankowiak M. Assessment of Equity in Access to Percutaneous Coronary Intervention (PCI) Centres in Poland. Healthcare. 2020; 8(2):71. https://doi.org/10.3390/healthcare8020071
Chicago/Turabian StyleRój, Justyna, and Maciej Jankowiak. 2020. "Assessment of Equity in Access to Percutaneous Coronary Intervention (PCI) Centres in Poland" Healthcare 8, no. 2: 71. https://doi.org/10.3390/healthcare8020071
APA StyleRój, J., & Jankowiak, M. (2020). Assessment of Equity in Access to Percutaneous Coronary Intervention (PCI) Centres in Poland. Healthcare, 8(2), 71. https://doi.org/10.3390/healthcare8020071






